Abstract
The authors present a case of a 42-year-old lady who visited her gynaecologist with dysuria and a sensation of incomplete voiding for 2 weeks. Urine culture grew Escherichia coli and blood studies were normal. Pelvic ultrasound revealed a smooth well-defined mass arising from the bladder wall. She was referred to the urologist who requested CT and MRI for further evaluation. These modalities confirmed an intramural bladder mass with normal overlying mucosa. The mass was deemed contributory to her symptoms and a decision was made to excise the mass surgically. Via a transurethral approach, cystoscopy revealed a smooth well-circumscribed intramural mass. This was partially excised. The mass was found to be a leiomyoma. Except for an uncomplicated urinary tract infection, her postoperative course has been uneventful.
Background
Leiomyomas are most frequently encountered in the uterus. A bladder leiomyoma is uncommon, this being the first documented case in our radiology department and the third in our department of pathology, to the best of our knowledge. This case serves to highlight the clinical presentation, imaging findings and surgical management of this unusual bladder neoplasm.
Case presentation
A 42-year-old woman presented to her gynaecologist with a 2-week history of dysuria and a sensation of incomplete voiding. There were no other symptoms and physical examination was unremarkable. She had no contributory medical, surgical, family, drug or social history.
Urine culture detected growth of Escherichia coli. Blood studies including a complete blood count, urea and electrolytes were normal. A pelvic ultrasound was revealed a 4 cm mass impressing on the bladder lumen. The patient was referred to the urologist. Culture-directed antibiotics were commenced and repeat culture was sterile.
CT and MRI of the pelvis were requested by the urologist. These confirmed the bladder mass and assisted in the surgical plan for excising the mass.
Operative management in the form of cystoscopy and transurethral resection of bladder tumour was performed. The mass was partially excised.
Histopathological examination revealed fragmented portions of a tumour composed of whorls and interlacing fascicles of spindle shaped cells that were immunoreactive for smooth muscle actin and desmin. There was no evidence of cytological atypia, mitotic activity or necrosis. The pathological diagnosis was that of leiomyoma. Focally attached portions of urinary bladder mucosa showed chronic inflammation.
The patient’s immediate postoperative course was uneventful but she has since had a recurrent urinary tract infection. Complete excision is planned at her convenience.
Investigations
A multidetector row CT scan was performed using GE, Lightspeed VCT (General Electric, Milwaukee, WI, USA), 5 mm axial sections were obtained. MRI was subsequently performed using GE Signa LX 1.5 Tesla unit (General Electric, Milwaukee, WI, USA). T2-weighted sequences in all three planes were performed together with axial T1W pre and postcontrast images. Both modalities revealed a 3.8 cm smooth well-circumscribed mass arising on the left lateral wall. The mass was hypodense to muscle on CT (figure 1).On MRI, the mass appeared intramural with an intact bladder mucosa. On both T1 and T2W images, the mass was iso-intense to muscle (figures 2–4). There was no extension through the wall, perivesical fat obliteration or adjacent organ involvement. There was no compression of the left vesicoureteric junction and no hydronephrosis.
Figure 1.

Axial postcontrast CT pelvis.
Figure 2.
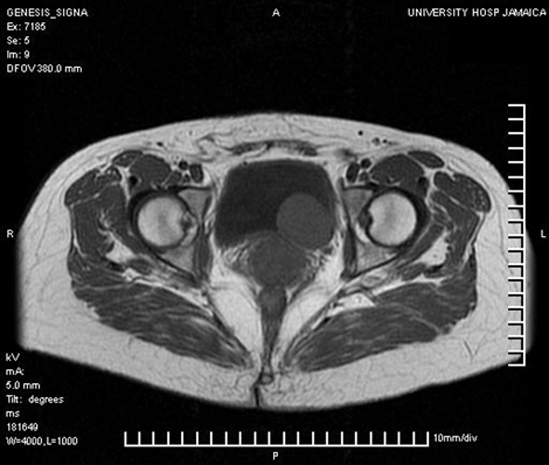
Axial T1-weighted MRI of pelvis.
Figure 4.

Coronal T2-weighted MRI of pelvis.
Figure 3.
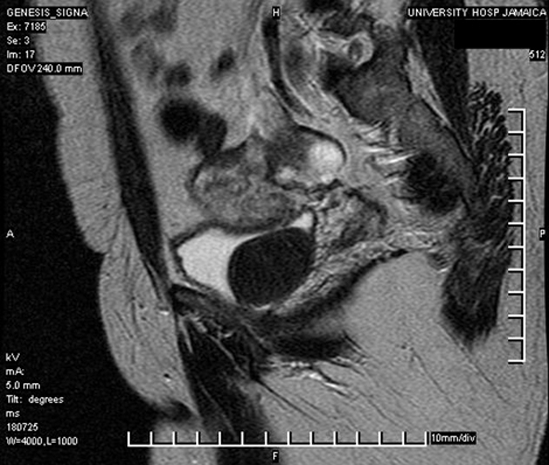
Sagittal T2-weighted MRI of pelvis.
Differential diagnosis
-
▶
Leiomyosarcoma
-
▶
Bladder carcinoma
-
▶
Benign fibrous tumour.
Treatment
At cystoscopy under general anaesthesia, a smooth intramural mass with unremarkable overlying urothelium was noted in the left lower lateral wall of the bladder. The left ureteric orifice was displaced superiorly but easily identified and catheterised. The mass was resected to the level of the bladder wall but a significant remaining portion was evident. This seemed to likely extend the full thickness of the bladder wall. Her immediate postoperative course was uneventful.
Outcome and follow-up
Complete surgical excision is generally reported to be curative. In the case of incomplete resection, surveillance is recommended. As these are generally slow-growing neoplasms, yearly follow-up is being considered.
Discussion
Leiomyomas are benign smooth muscle tumours. They are commonly found in the uterus, but rare sites of occurrence such as the bladder have been recorded.1 Despite the bladder being a rare site for leiomyoma, it is the most common benign bladder tumour (35%).2 The single largest series of smooth muscle bladder tumours (leiomyoma and leiomyosarcoma) had 51 cases3 and the largest series of bladder leiomyomas had 90 cases.4 However, only 1–5% of bladder tumours are benign.
Bladder leiomyomas are predominantly found in women. This finding may reflect the tumour’s expression of oestrogen receptors5 The most common presenting symptoms result from obstruction or irritation.6 7 There have also been cases of leiomyoma that have presented with haematuria and a case that presented as a pelvic mass.8
Gross examination of a bladder leiomyoma reveals a firm tan-coloured tumour mass which may be endovesical, intramural or extravesical. They are characterised microscopically by low cellularity and show interlacing fascicles of smooth muscle cells, which do not display atypia or any significant mitotic activity.
The differential diagnoses of spindle cell lesions of the bladder include leiomyosarcoma, postoperative spindle cell nodule and inflammatory pseudotumour. While both leiomyomas and leiomyosarcomas are immunoreactive for smooth muscle actin and desmin, they are distinguished morphologically by the circumscription, low cellularity and lack of cytologic atypia and mitotic activity in the former. Leiomyosarcomas, by contrast, show an infiltrative growth pattern, high cellularity, cytologic atypia and increased mitotic activity.9 10 Postoperative spindle cell nodules also show marked cellularity and high mitotic activity, but lack the pleomorphism exhibited by leiomyosarcomas, and unlike leiomyosarcomas, are immunoreactive for low molecular weight cytokeratin.9 10 In addition, patients with postoperative spindle cell nodule will have a history of a recent surgical procedure.10 Inflammatory pseudotumours are highly cellular and exhibit pleomorphism, but are distinguished from sarcomas by their highly myxoid and inflammatory background.11
Ninety-five per cent of bladder neoplasms arise from the epithelium; the most common being urothelial carcinoma, which accounts for 90% of cases.12 It typically occurs in men aged 50–70 years and may be related to smoking or occupational exposure to carcinogens such as aromatic dyes.13 Other carcinoma include squamous cell carcinoma (2–15%) and adenocarcinoma (<2%), which tend to occur in the setting of chronic bladder infection/irritation. Rare mesenchymal tumours include paraganglioma, lymphoma and solitary fibrous tumour. Although imaging findings are not specific for these tumours, patterns of growth and tumour characteristics may allow differentiation.
There are three main modalities that can be employed in the demonstration of bladder leiomyomata. These are ultrasound, CT and MRI. On all three imaging modalities, leiomyomas appear smooth, well-circumscribed and ovoid.14
Ultrasound is often the first procedure done for urinary tract and pelvic evaluation in the female patient owing to its affordability and availability. It also provides a good overview of the kidneys, bladder, uterus and ovaries without gonadal irradiation. The features of bladder leiomyoma on ultrasound have been documented and include a soft tissue mass which is typically iso to hypoechoic to bladder wall.15 16 They may show Doppler flow.17 At CT, the mass is isodense to muscle and may show mild enhancement. For accurate staging, MRI is the modality of choice.18 At MRI, the normal bladder wall is of intermediate signal intensity on the T1-weighted image, while there is an intermediate signal outer band and a low signal inner band on the T2-weighted image. On both T1- and T2-weighted images, non-degenerative leiomyomas are usually visualised as low intensity nodules with smooth surfaces. The submucosal location with intact mucosa is a characteristic feature of urinary bladder leiomyoma, and resembles uterine leiomyoma. By contrast, the more common transitional cell carcinoma affects the mucosa.
There is no known medical treatment that may induce involution of bladder leiomyomata. As malignant conversion of these tumours has not been documented, observation of asymptomatic lesions can be considered once the pathology is certain. Options for resection include laparoscopic,19 robotic assisted20 transurethral21 22 and open surgery.
Learning points.
-
▶
Though uncommon, bladder leiomyoma is the most common benign bladder tumour.
-
▶
It may be responsible for obstructive or irritative bladder symptoms.
-
▶
Ultrasound should be a primary consideration in patients with bladder symptoms and can satisfactorily depict a bladder leiomyoma.
-
▶
MRI is the best tool for establishing the diagnosis of leiomyoma and in preoperative planning.
-
▶
Treatments are surgical, with transurethral endoscopic removal providing a safe and effective means of treatment.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Fasih N, Prasad Shanbhogue AK, Macdonald DB, et al. Leiomyomas beyond the uterus: unusual locations, rare manifestations. Radiographics 2008;28:1931–48 [DOI] [PubMed] [Google Scholar]
- 2.Campbell EW, Gislason GJ. Benign mesothelial tumors of the urinary bladder: review of literature and a report of a case of leiomyoma. J Urol 1953;70:733–41 [DOI] [PubMed] [Google Scholar]
- 3.Lee TK, Miyamoto H, Osunkoya AO, et al. Smooth muscle neoplasms of the urinary bladder: a clinicopathologic study of 51 cases. Am J Surg Pathol 2010;34:502–9 [DOI] [PubMed] [Google Scholar]
- 4.Silva-Ramos M, Massó P, Versos R, et al. Leiomyoma of the bladder. Analysis of a collection of 90 cases. Actas Urol Esp 2003;27:581–6 [DOI] [PubMed] [Google Scholar]
- 5.Furuhashi M, Suganuma N. Recurrent bladder leiomyoma with ovarian steroid hormone receptors. J Urol 2002;167:1399–400 [PubMed] [Google Scholar]
- 6.Saunders SE, Conjeski JM, Zaslau S, et al. Leiomyoma of the urinary bladder presenting as urinary retention in the female. Can J Urol 2009;16:4762–4 [PubMed] [Google Scholar]
- 7.Lin HC, Wu WJ, Ke HL, et al. Bladder leiomyoma presenting as voiding dysfunction: a case report. Kaohsiung J Med Sci 2006;22:154–7 [DOI] [PubMed] [Google Scholar]
- 8.Erdemoglu E, Kamaci M. Giant bladder leiomyoma presenting as a pelvic mass: a case report. Eur J Gynaecol Oncol 2007;28:509–10 [PubMed] [Google Scholar]
- 9.Cheville J. Leiomyoma. In: Elbe JN, Sauter G, Epstein JI, Sesterhenn IA, eds. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Urinary System and Male Genital Organs. Lyon, France: IARC Press; 2004:144 [Google Scholar]
- 10.Rosai J. (ed.). Rosai and Ackerman’s Surgical Pathology. Ninth edition Philadelphia, PA: Mosby; 2004 [Google Scholar]
- 11.Cruz Guerra NA, Fradejas Rodríguez A, del Valle Manteca A, et al. Bladder leiomyosarcoma: case report. Arch Esp Urol 2006;59:198–201 [DOI] [PubMed] [Google Scholar]
- 12.Wong-You-Cheong JJ, Woodward PJ, Manning MA, et al. From the Archives of the AFIP: neoplasms of the urinary bladder: radiologic-pathologic correlation. Radiographics 2006;26:553–80 [DOI] [PubMed] [Google Scholar]
- 13.Borchini R, Bonzini M, Veronesi G, et al. Validation of a screening method for occupational bladder cancer. Med Lav 2009;100:438–47 [PubMed] [Google Scholar]
- 14.Zhang LY, Dai JR. Imaging features of nonepithelial tumors of the bladder. Zhonghua Zhong Liu Za Zhi 2009;31:384–7 [PubMed] [Google Scholar]
- 15.John NK, Fuad SF, James DN. Leiomyoma of bladder. Report of 2 cases and demonstration of ultrasonic appearance. Urology 1990;35:210–12 [DOI] [PubMed] [Google Scholar]
- 16.Fernandez A, Mayayo DT. Leiomyoma of the urinary bladder floor: diagnosis by transvaginal ultrasound. Urol Int 1992;48:99–101 [DOI] [PubMed] [Google Scholar]
- 17.Sherer DM, Gorelick C, Gabbur N, et al. Color Doppler imaging and 3-dimensional sonographic findings of urinary bladder leiomyoma. J Ultrasound Med 2007;26:667–70 [DOI] [PubMed] [Google Scholar]
- 18.Maya MM, Slywotzky C. Urinary bladder leiomyoma resonance imaging findings. Urol Radiol 1992;14:197–9 [DOI] [PubMed] [Google Scholar]
- 19.Hong SY, Lee TS, Kim JH. Laparoscopic enucleation of a bladder leiomyoma. J Minim Invasive Gynecol 2009;16:772–4 [DOI] [PubMed] [Google Scholar]
- 20.Thiel DD, Williams BF, Krishna M, et al. Robot-assisted laparoscopic excision of bladder wall leiomyoma. J Endourol 2009;23:579–82 [DOI] [PubMed] [Google Scholar]
- 21.Sugimoto K, Yamamoto Y, Hashimoto K, et al. Leiomyoma of the urinary bladder treated by transurethral resection: a case report. Hinyokika Kiyo 2007;53:251–3 [PubMed] [Google Scholar]
- 22.Khallouk A, Wallerand H, Kleinclauss F, et al. Bladder leiomyoma treated by transurethral endoscopic resection. Prog Urol 2005;15:1135–7 [PubMed] [Google Scholar]


