Abstract
In the past 20–30 years, the number of overweight children in the United States has doubled.1 Overweight children are acquiring conditions such as hypertension, type II diabetes, hypercholesterolemia, sleep apnea, and orthopedic problems. The purpose of this study was to explore the prevalence of and factors associated with at risk and overweight in children 2–10 years of age in a Health Maintenance Organization (HMO) in Hawai‘i. This quantitative, retrospective cross-sectional study included a stratified random sample of 554 children ages 2–10 years who received a well child health care exam at a HMO in 2003. The prevalence of at risk and overweight were examined including the relationship between ethnicity, socioeconomic status, place of residence, and a child being overweight. Thirteen percent were at risk for overweight (BMI 85–95%) and 19% (BMI >95%) were overweight. In the 6–10 year age group, 42 % were overweight or at risk for being overweight. Boys had a higher incidence of being overweight (54%) than the girls (46%). Pacific Islanders had the highest incidence of overweight (40%), followed by the Hawaiian/Part Hawaiians (19%) and Filipinos (19%). Ethnicity and place of residence were significantly associated with being at risk or overweight. Pacific Islanders were 4 times more likely to be overweight/at risk for overweight and those residing in the West O‘ahu, Honolulu, and Central O‘ahu/North Shore areas were 2–3 times more likely to be at risk for overweight when compared to children living in the Windward side. With increased age, the prevalence of overweight increased. Findings suggest that targeted obesity prevention strategies need to be initiated early in life and geared for ethnically and geographically diverse children and their families.
Introduction
Obesity is a major public health concern in pediatrics, both nationally and in Hawai‘i. Identifying overweight children is a priority of the United States Department of Health and Human Services. Monitoring the prevalence of overweight children is one of the ten leading health indicators in Healthy People 2010.2 Overweight in children has been associated with both physical and psychological risk factors such as hypertension, dyslipidemia, hyperinsulinemia, orthopedic problems, social rejection, and low self-esteem.2–6 The onset of these obesity-related morbidities in childhood predicts the presence of disease in adulthood. One out of six overweight children 6 years of age and older has been noted to have one or more heart disease risk factors.2
The prevalence of obesity in children and adolescents in the United States has been difficult to estimate because of a lack of consensus in the definition of obesity and lack of studies that focus on the pediatric population. Data on childhood obesity and different ethnic groups is minimal. More than one in seven children were overweight in the United States in 1999–2000; this is triple the 1960's rates.7 From 1999–2004, all ethnic/racial, gender, and age groups have increased in the percentage of children who are considered overweight.8
Nineteen percent of children ages 6–11 years and 17.4% of adolescents ages 12–19 years are overweight;8 this is an increase from previous data estimating 13% of children ages 6–11 years and 14% of adolescents ages 12–19 years.2 A study that estimated the prevalence of obesity in 2003–2006, found that 11.3% of 2–19 year olds were at or above the 97th percentile, 16.3 % were at or above the 95%, and 31.9% were at or above the 85th percentile.9
Socio-economic status may be a useful indicator of the potential environmental and family risk factors related to overweight. Studies have shown that children living in low income families were more apt to be overweight or at risk for overweight, however subgroups have differed.10–12 One study demonstrated the largest increases in overweight occurred among the 4–5 year old low income preschoolers.13
There is little literature on the prevalence and factors associated with overweight in Asian American, Hawaiian, and Pacific Island children. In a study done in Hawai‘i from 1992–1996 using data of 1,437 public school children, multiple anthropometric indicators suggest there might be more children of Hawaiian ancestry who are overweight. There were twice as many Hawaiian and Non-Hawaiian Ancestry boys and girls that were classified as obese compared to the statistics in the National Health and Nutrition Examination Surveys.14 An additional study of 20,000 children participating in the Women Infant and children supplemental food program noted large differences among the different ethnic groups in Hawai‘i.15 In a more recent Hawai‘i-based study using student health records, the prevalence of overweight was calculated based on Body Mass Index. Almost one third of children entering kindergarten in Hawai‘i public schools in 2002–2003 were overweight or at risk for overweight.16
There are several methods to determine adiposity that are very accurate but expensive and or invasive. The majority of health care providers use Body Mass Index (BMI).6 BMI has recently been recommended for both adults and pediatric populations. The revised 2000 CDC pediatric growth charts include gender-specific BMI for age percentile distribution for ages 2–20 years and are currently used across all racial and ethnic groups.17 When data was collected for this study, the standard measurement for “at risk for overweight” in children was 85–94% on the standard BMI percentile charts and “overweight” was considered at or above the 95%. The findings from this study will reflect these categories. Currently, the Expert Committee recommends using the terms overweight for 85%–94% and obese for 95% and greater.10 There are no BMI for age references for obesity in children less than 2 years.18
This article presents the findings of a retrospective, cross-sectional study using a stratified random sample of children ages 2–10 years who received a physical examination at the Health Maintenance Organization (HMO) on O‘ahu in 2003. This HMO is the second largest Health Insurance carrier for Hawai‘i, covering 20% of the population. The purpose of this study was to identify the prevalence and factors associated with overweight children. To achieve this aim, the following research questions were explored:
What is the prevalence of overweight /at risk for overweight in the 2 to 10 year old age groups?
Is there a significant difference between overweight/ at risk for being overweight by age?
Is there a significant association between overweight/ at risk for overweight children and ethnicity?
Is there a significant association between children who are overweight/at risk for overweight and their socioeconomic status and/or their residence?
Methods
This study was approved by the University of Hawai‘i at Manoa Institutional Review Board Committee on Human Studies and HMO's Institutional Review Board. A stratified random sample was selected from children with birthdates from 1993 to 2001 that accessed one of the 10 O‘ahu clinics for a physical examination in 2003 (N=9,768). Random samples were stratified by age groups (2–3 years, 4–5 years, and 6–10 years). The final sample consisted of 554 children ages 2 to 10 years, including 179 in the 2–3 year age group (N=2,766), 187 in the 4–5 year age group (N=2,929), and 188 in the 6–10 year age group (N=3,951). A power analysis was computed for this population at a confidence interval of 95%.
Data were obtained on all 554 subjects via a chart review and information was recorded on a data collection tool developed for this study. The age of the child at the time of the 2003 visit and BMI were calculated for that visit. Other variables included the child's gender, ethnicity, socioeconomic status, blood pressure, family health risk factors, zip code, and medical history. The child's ethnicity was determined by parental report in the child's medical record. Data were coded and then entered into SPSS 11.0, and audited for accuracy. Ethnicity was recoded from 8 to 6 categories collapsing the very small categories (Hispanics, Blacks and others) into one category for analysis.
The following definitions were used:
Body mass index (BMI) is the ratio of weight in kilograms divided by the square of height in meters. In children, BMI is age- and gender-specific and reported in percentiles.
Overweight was defined as a BMI ≥ 95th percentile for age and gender.
At risk for overweight was defined as a BMI ≥ 85th percentile but less than the 95th percentile for age and gender.
Socioeconomic Status (SES) was based on the child's health insurance plan. QUEST is the state Medicaid managed care program for family incomes of up to 200% of the federal poverty level. QUEST was considered the low SES group and the Health Plan was considered the non-low SES group.
Place of Residence was determined by the zip code of residence located in the medical record. Zip codes were recoded into 4 categories including West O‘ahu, Honolulu, Central O‘ahu/North Shore and Windward O‘ahu.
Data analysis included the calculation of percentages for nominal and ordinal data, and means and standard deviations for the interval level data. Calculations of percentages for prevalence of normal or underweight, at risk for overweight, and overweight categories were calculated for the entire sample and each age group. Cross tabulations, Chi-Square analysis, and Logistic regression were used for bivariate and multivariate analyses. A p<.05 value was considered as a significant value for this study.
Results
Fifty-four percent (n=300) of the subjects were boys and 46% (n=254) were girls. Table 1 provides a summary of the other demographic variables for this study. Nineteen percent (n=104) of children ages 2 to 10 years were overweight and another 13% were at risk for overweight. Overall, there was a significant difference in the prevalence of overweight status in boys (22%, n=66) compared to girls (15%, n=38); this trend continued with 15% (n=44) of boys and 10% (n=26) girls at risk for overweight in this age group (χ2 8.405, p< .015).
Table 1.
Demographic Characteristics of the Sample
| Variable | n | % | |
| Ethnicity | Hawaiian/Part Hawaiian | 236 | 42.6 |
| Pacific Island | 38 | 6.9 | |
| Asian/Part Asian | 104 | 18.8 | |
| Hispanic | 15 | 2.7 | |
| Filipino | 102 | 18.4 | |
| White | 42 | 7.6 | |
| Hispanics, Black & Other | 32 | 5.8 | |
| SES | Medicaid (Quest) | 160 | 28.9 |
| Non-Medicaid | 394 | 71.1 | |
| Residence | Honolulu/East Honolulu | 202 | 36.5 |
| Ewa/Waianae | 162 | 29.2 | |
| Central O‘ahu/North Shore | 73 | 13.2 | |
| Windward | 115 | 20.8 |
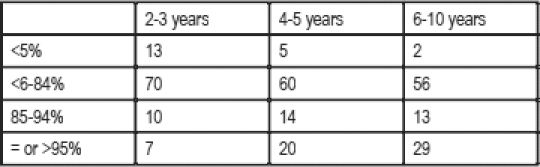
There was a significant association between age categories and overweight and at risk for overweight children (chi square 34.526, p=0.000). As the age categories increased, the prevalence of overweight increased. For the at risk group, the prevalence of at risk for overweight children increased between the youngest group (2–3 years) and the two older groups (4–5 years and 6–10 years) (Table 2).
Table 2.
Number & Percentage in Weight Categories by Ethnicity, SES, & Place of Residence
| Under- or Normal Weight (<85%) | At Risk (85–94%) | Overweight (= or >95%) | ||||
| n | % | n | % | n | % | |
| Ethnicity* | ||||||
| Hawaiian/Part Hawaiian | 164 | 70 | 27 | 11 | 45 | 19 |
| Pacific Island | 16 | 42 | 7 | 18 | 15 | 40 |
| Asian | 75 | 72 | 12 | 12 | 17 | 16 |
| Filipino | 72 | 70 | 11 | 11 | 19 | 19 |
| White | 29 | 69 | 9 | 21 | 4 | 10 |
| Hispanic, Black, Other | 24 | 75 | 4 | 12 | 4 | 13 |
| SES** | ||||||
| Medicaid (Quest) | 112 | 70 | 19 | 12 | 29 | 18 |
| Non-Medicaid | 268 | 68 | 51 | 13 | 75 | 19 |
| Residence^ | ||||||
| Honolulu/East Honolulu | 136 | 67 | 22 | 11 | 44 | 22 |
| Ewa/Waianae | 110 | 68 | 17 | 10 | 35 | 22 |
| Cental O‘ahu/North Shore | 44 | 60 | 18 | 25 | 11 | 15 |
| Windward | 89 | 78 | 13 | 11 | 13 | 11 |
x2 20.172, p = 0.028;
x2 0.218, p = 0.897;
x2 17.288, p=0.008
The highest prevalence of overweight children ages 2–10 years was in the Pacific Island children with 40% “overweight” and 18% “at risk” for overweight. Nineteen percent of Hawaiian/Part Hawaiian children and 19% of Filipino children were overweight. Caucasian children had the lowest percentage of overweight children; however they had the highest percentage of at risk for overweight children (21%). (Table 2).
In the bivariate analysis, there was a significant association between ethnic groups and weight categories (χ2 20.172, p=0.028) and in overweight and at risk for overweight and place of residence (χ2 17.288, p=0.008). The Windward O‘ahu location had the highest percentage of children who were underweight or normal weight. There was no association between SES and weight categories in this study (Table 2).
The variables (Ethnicity/Race, SES, and Residence) were entered into a binary logistic regression model. The dependent variables for this analysis were under/normal weight, and at risk for overweight and overweight (BMI ≥85%). The model demonstrated a non-significant Hosmer & Lemeshow test (p=.648), indicating the data fit the model.19 This model was able to classify 12% of the children who were at risk for overweight/overweight and almost all (97%) of those who were not; the overall model was able to classify 70% correctly. Pacific Island children were 3.6 times more likely to be at risk for or overweight. In addition, children living in Honolulu and West O‘ahu were 2 times as likely and those living in Central O‘ahu/North Shore were 3 times as likely to be at risk for or overweight when compared to children living in Windward O‘ahu. (Table 3).
Table 3.
Logistic Regression Model for Ethnicity, SES, Residence & at risk for overweight/overweight
| Variable | b | Wald Chi Square | p | Odds ratio | 95% CI for Odds Ratio | |
| Lower | Upper | |||||
| Ethnicity | ||||||
| Asian | 14.565 | .012 | ||||
| White | .162 | .161 | .689 | 1.2 | .532 | 2.6 |
| Filipino | .034 | .012 | .913 | 1.0 | .556 | 1.928 |
| Pacific Island | .203 | .560 | .454 | 1.2 | .719 | 2.088 |
| Hawaiian/Part Hawaiian | 1.380 | 11.801 | .001 | 4.0 | 1.809 | 8.741 |
| Hispanic, Black, Other | −.152 | .105 | .746 | 0.9 | .341 | 2.160 |
| SES | ||||||
| Non-Medicaid | .162 | .581 | .446 | 1.2 | .776 | 1.781 |
| Residence | ||||||
| Honolulu/East Honolulu | 8.838 | .032 | ||||
| Ewa/Waianae | −.035 | .022 | .883 | 1.0 | .610 | 1.530 |
| Central O‘ahu/North Shore | .393 | 1.872 | .171 | 1.5 | .844 | 2.604 |
| Windward | −.597 | 4.497 | .034 | 0.5 | .317 | .956 |
| Constant | −1.036 | 12.688 | .000 | 0.4 | ||
Note: All ethnicity categories are compared to Asian/Part Asian category, SES was compared to Medicaid (Quest) category and Residence was compared to Honolulu/East Honolulu category.
To further understand the subtle differences in childhood overweight that may occur within the ethnicity/race, socioeconomic status, and place of residence categories, a multinominal logistic regression using with 3 dependent variables (normal/underweight, at risk for overweight (BMI 85–94%), and overweight (BMI ≥ 95%)), was conducted. Children living in the Central O‘ahu/North Shore area (p=.006) were significantly more likely to be at risk for overweight and children living in the West O‘ahu area were more likely to be overweight (p=.018) In addition, Pacific Island children were 6 times more likely to be overweight (p = .005).
Discussion
The study findings indicated a high prevalence rate of overweight and at risk of being overweight (overall 32%) in children who received a physical exam at the HMO on O‘ahu. As the age groups increased, the prevalence for overweight increased. This data is similar to the prevalence of high BMI for similar age categories reported among US children from the 2003–2006.9 This study supports similar findings from childhood obesity studies in Hawai‘i. Almost one third of children entering kindergarten in Hawai‘i public schools during the 2002–2003 were overweight or at risk for overweight.16
Initially in the 2–3 year age category, the “at risk for overweight” was higher than the “overweight” percentage, but as the age category increased the “overweight” percentage was greater than the “at risk for overweight” group. Several studies note a strong relationship between a child's weight status and adult obesity.20,21 The older the child is when they are overweight, the more likely they will continue to be overweight or obese adults. Ritchie et al2 noted that this trend starts as early as age 6 to 9 years. Sixty percent of children who were overweight during preschool and 80% of children who were overweight at 7 to 11 years of age were overweight at 12 years of age.22 A study by Whitaker et al tracking BMI from childhood to adulthood notes that 75% of those with a BMI for age above the 85th percentile were obese as adults.23 Adolescence has been cited as a critical period for the development of obesity-related co-morbidities. Studies demonstrate that up to 80% of overweight adolescents will become obese adults.24,25 It has been suggested that the rising trend if continued will result in the next generation of children being more obese and less physically active than this generation.26,27
The study findings demonstrated a significant association between ethnicity and being overweight. Fifty eight percent of the Pacific Island children were overweight or at risk for being overweight. In the Hawaiian /Part Hawaiian group, 31 % were either overweight or at risk for being overweight. Each ethnic group had variations in the percentages that were “at risk” and “overweight”. When these two weight categories were combined, the difference among the ethnic/racial groups was less apparent (Filipino 29%; Asian 28%; Caucasian 31%). Caucasian children had the highest “at risk” percentage (21 %). Other studies with children living in Hawai‘i have noted similar results.14,15,28 Data indicates that Pacific Islanders (Native Hawaiians included) have some of the highest prevalence of obesity and type 2 diabetes.28
There was no association between the socioeconomic status (SES) of children in this study and being “overweight” or “at risk” for being overweight. This was a consistent finding observed with non-white females and Mexican American children.30 For this study, SES was determined by a child's type of medical insurance. Other methods for determining SES, including parental or family income, parent's occupation, or education level may have yielded different findings. There was a significant difference noted in the child's place of residence and being “overweight’ or ‘at risk” for being overweight. One could argue that place of residence is not an independent variable but rather a proxy measure for SES based on the economic or ethnic/racial homogeneity within a specific area. In this study, when all these variables were put into a regression model, Central O‘ahu children were more likely to be at risk and West O‘ahu children were more likely to be overweight. The BMI in childhood may correlate with body fatness and overall health outcomes of a population, but the ethnic and other socio-demographic factors such as place of residence may influence these relationships. Peer and family social support, neighborhood opportunities and physical environment, and schools are important determinants for a child's physical activity level and overall well-being.31
There were limitations in this study. First, in any retrospective cross-sectional study design, the reliability of the data present is a limitation. The existing data did not always include the information that were needed or it may have been inaccurate. Documentation was handwritten and completed by a various health practitioners. A second limitation is that the study included children on the island of O‘ahu in 2003 who received a well child examination. Neighbor island children may have experienced different environmental factors that may influence their weight status. Therefore, this study may not be representative of all children in the 2–10 year age group of Hawai‘i. Furthermore, the SES indicator of “QUEST”/“Health Plan” used in this study may not be an accurate measure for SES. Finally, this study used BMI as a measure for weight categories. Chai and colleagues have suggested using multiple anthropometric indicators rather than a single one may be more accurate and appropriate for determining overweight in this population.14 The relevance of the BMI must be considered in the context of the medical history, physical exam, and presence of co-morbidities. The validity of the BMI still remains an issue but its use is recommended as a trigger for assessment and intervention.10 Tyrell et al stated that even though the BMI cutoff-points for children may need to be ethnic specific, this should not justify the use of different BMI percentiles.29
Recommendations
Findings from this study are the first to document the prevalence of “at risk for overweight” and “overweight” in a population of 2–10 year olds at a HMO in Hawai‘i. The rate of overweight and obesity in the HMO population is consistent with both recent Hawai‘i State and National Prevalence estimates. HMOs focus on keeping people well and invest in health promotion and disease prevention. This study contributes significantly to the understanding of the prevalence of childhood obesity and opportunities to intervene with prevention at the earliest possible time in a child's life, before they become overweight or obese.
Study findings support the aggressive implementation of Expert National recommendations for screening, monitoring, and stepwise intervention guidelines in the prevention of childhood obesity.10,32,33 The calculation of BMI and anticipatory guidance at all well child care visits is the first step at obesity prevention. Pediatric obesity has become a major focus as the new morbidity that threatens the health status of children and has implications into adult life. Public health interventions for children who are overweight needs to be directed at the primary prevention level. The difficulty in treating adult obesity has been documented and the potential future health care costs associated with children who are obese and its co-morbidities are overwhelming.
Interventions need to be initiated early in a child's life. Cook and colleagues report that clinicians diagnosed obesity in less than 1% of all visits.34 Health Care Providers must target interventions that are developmentally age appropriate. Strategies should include nutrition and physical activity counseling that takes into consideration lifestyles of communities in Hawai‘i, cultural aspects of parenting practices, and environmental influences. This study was conducted prior to the implementation of the electronic medical record (EMR). EMR systems can be instrumental in collecting accurate and complete health data, reporting prevalence data, and providing reminder cues for Health Care Providers.
The study's findings suggest there is a significant prevalence of overweight and at risk for overweight among this HMO population on O‘ahu. Further studies should be directed at examining other age groups, including the under 2 year and over 10 year groups. It is vital for the health care providers to take the lead in prevention and early identification of overweight children. Understanding the prevalence in children is the initial step in instituting a primary prevention approach to obesity.
Figure 1.
Percentage on BMI Growth Charts in Age Groups
Disclosure Statement
The authors have no financial relationships relevant to this article to disclose. This research was partially funded by a seed grant from the Office of Faculty Research, University of Hawai‘i at Manoa School of Nursing and Dental Hygiene.
References
- 1.Bartlett T, Lancaster R, New N. Pediatric obesity: Use a team approach. The Clinical Advisor. 2005:22–31. [Google Scholar]
- 2.Ritchie L, Ivey S, Masch M, Woodward-Lopez G, Ikeda J, Crawford P. Pediatric overweight: A review of the literature. Center for Weight and Health, U. C. Berkeley; 2001. pp. 1–16. [Google Scholar]
- 3.Barlow S, Dietz W. Obesity evaluation and treatment: Expert committee recommendations. Pediatrics. 1998;102(3):1–11. doi: 10.1542/peds.102.3.e29. [DOI] [PubMed] [Google Scholar]
- 4.Freedman DS, Dietz WH, Srinivasan SR, Brenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103:1175–1182. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics, author. Policy Statement. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112(2):424–430. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 6.Hodges E. A primer on early childhood obesity and parental influence. Pediatr Nurs. 2003;29(1):13–16. [PubMed] [Google Scholar]
- 7.Child Trends Data Bank. 2003. [On-Line]. http//www.childtrendsdatabank.org.
- 8.Ogden C, Carroll M, Curtin L, McDowell M, Tabak C, Flegal K. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 9.Ogden C, Carroll M, Flegal K. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 10.Barlow SE The Expert Committee, author. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary Report. 2007. Pediatrics. 2007;120:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 11.Gordon_Larson P, Adair L, Popkin B. The relationship of ethnicity, socioeconomic factors, and overweight in US adolescents. Obesity Research. 2003;11:121–129. doi: 10.1038/oby.2003.20. [DOI] [PubMed] [Google Scholar]
- 12.Strauss R, Knight J. Influence of the home environment on the development of obesity in children. Pediatrics. 1999;6:103. doi: 10.1542/peds.103.6.e85. [DOI] [PubMed] [Google Scholar]
- 13.Ogden C, Flegal K, Carroll M, Johnson C. Prevalence and trends in overweight among US children and adolescents. JAMA. 2002;288:14,1728–14,1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 14.Chai D, Kaluhiokalani N, Little J, Hetzler R, Zhang S, Mikami J, Ho K. Childhood overweight problem in a selected school district in Hawaii. American Journal of Human Biology. 2003 doi: 10.1002/ajhb.10134. [DOI] [PubMed] [Google Scholar]
- 15.Baruffi G, Hardy C, Waslien C, Uyehara S, Kruptitsky D. Ethnic differences in the prevalence of overweight among young children in Hawaii. Journal of the American Dietetic Association. 2004:1701–1707. doi: 10.1016/j.jada.2004.08.027. [DOI] [PubMed] [Google Scholar]
- 16.Pobutsky A, Hirokawa R, Zou L, Huang T, Rosen L, Wood B. Overweight and at-risk for overweight among Hawai'i public school students entering kindergarten, 2002–2003. 2006:283–287. [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention, author. 2000 CDC growth charts; United States. 2000. [OnLine]. Available: http://www.cdc.gov/growthcharts.
- 18.Institute of Medicine. Committee on scientific evaluation WIC nutrition risk criteria food and nutrition board, author. Summary of WIC nutrition risk criteria; A scientific assessment. J Am Diet Assoc. 1996;96(9):925–930. [PubMed] [Google Scholar]
- 19.Munro BH. Statistical methods for health care research. Lippincott: Williams and Wilkens, Philadelphia; 2005. [Google Scholar]
- 20.Guo SS, Chumela WC. Tracking of body mass index in children in relation to overweight in adulthood. A. J Clin Nutr. 1999;70(suppl):145S. doi: 10.1093/ajcn/70.1.145s. [DOI] [PubMed] [Google Scholar]
- 21.Berensen GS. Obesity-a critical issue in preventive cardiology: The Bogalusa Heart Study. Prev Cardiol. 2005;8:234–241. doi: 10.1111/j.0197-3118.2005.04485.x. [DOI] [PubMed] [Google Scholar]
- 22.Nader P, O'Brien M, Houts R, Bradley R, Belsky J, Crosone R, Friedman S, Mei Z, Susman E. The National Institute of Child Health and Human Development Early Child Care Research Network. Pediatrics. 2006;118:594–601. [Google Scholar]
- 23.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 24.Morrison JA, Sprecher DL, Barton BA, Waclawiw MA, Daniels SR. Overweight, fat patterning, and cardiovascular disease risk factors in black and white girls: The National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr. 1999;135:4,409–4,410. doi: 10.1016/s0022-3476(99)70168-x. [DOI] [PubMed] [Google Scholar]
- 25.Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S, Robinson TN, Scott BJ, St Jeor S, Williams CL. Overweight children and adolescents. Pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111:1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- 26.Straus RS. Childhood obesity. Pediatric Clinics of North America. 2002;49:1,175–1,201. doi: 10.1016/s0031-3955(03)00114-7. [DOI] [PubMed] [Google Scholar]
- 27.Shilbli R, Rubin L, Akons H, Shaoul R. Morbidity of overweight (≥85 Percentile) in the first 2 years of life. Pediatrics. 2008;122:2,267–2,272. doi: 10.1542/peds.2007-2867. [DOI] [PubMed] [Google Scholar]
- 28.Okihiro M, Davis J, White L, Beckham S, Derauf DC. Childhood overweight in a population of Pacific Island children. He Huliau-A turning point eliminating health disparities in native Hawaiians and Pacific peoples: Obesity 2005; Conference sponsored by the Hawaii Consortium for Continuing Medical Education, a joint venture between the Hawaii Medical Association and the John A. Burns School of Medicine, University of Hawaii.2005. [Google Scholar]
- 29.Tyrell VJ, Richards GE, Hofman P, Gillies GF, Robinson E, Cutfield WS. Obesity in Auckland school children: A comparison of the body mass index and percentage body fat as the diagnostic criterion. Int J Obes Relat Metab Disord. 2001;25(2):164–169. doi: 10.1038/sj.ijo.0801532. [DOI] [PubMed] [Google Scholar]
- 30.Wang Y, Zang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am J Clin Nutr. 2006;84:707–716. doi: 10.1093/ajcn/84.4.707. [DOI] [PubMed] [Google Scholar]
- 31.Davis MM, Gance-Cleveland B, Hassink S, Johnson R, Paradis G, Resnicow K. Recommendations for prevention of childhood obesity. Pediatrics. 2007;120:S229–S253. doi: 10.1542/peds.2007-2329E. [DOI] [PubMed] [Google Scholar]
- 32.Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120:S193–S228. doi: 10.1542/peds.2007-329D. [DOI] [PubMed] [Google Scholar]
- 33.Gee S, Rogers V, Liu L, McGrath J. An implementation guide from NICHQ's Childhood Obesity Action Network. NICHQ, Childhood Obesity Action Network; 2008. [Google Scholar]
- 34.Cook S, Weitzman M, Auinger P, Barlow SE. Screening and counseling associated with obesity diagnosis in a national survey of ambulatory pediatric visits. Pediatrics. 2005;116:1,112–1,116. doi: 10.1542/peds.2004-1517. [DOI] [PubMed] [Google Scholar]


