Abstract
Objective
It is debatable whether an anterior oblique fracture orientation is really a contraindication to anterior odontoid screw fixation. The purpose of this study was to investigate the feasibility of anterior odontoid screw fixation of type II and rostral shallow type III fracture with an anterior oblique fracture orientation.
Methods
The authors evaluated 16 patients with type II and rostral shallow type III odontoid fracture with an anterior oblique fracture orientation. Of these 16 patients, 8 (group 1) were treated by anterior odontoid screw fixation, and 8 (group 2) by a posterior C1-2 arthrodesis.
Results
Of the 8 patients in group 1, seven patients achieved solid bone fusion (87.5%), and one experienced screw back-out of the C-2 body two months after anterior screw fixation. All patients treated by posterior C1-C2 fusion in group 2 achieved successful bone fusion. Mean fracture displacements and fracture gaps were not significantly different in two groups. (p=0.075 and 0.782). However, mean fracture orientation angles were 15.3±3.2 degrees in group 1, and 28.6+8.1 degrees in group 2 (p=0.002), and mean fragment angulations were 3.2±2.1 degrees in group 1, and 14.8±6.7 degrees in group 2 (p=0.001).
Conclusion
Even when the fracture lines of type II and rostral shallow type III fractures are oriented in an anterior oblique direction, anterior odontoid screw fixation can be feasible in carefully selected patients with a relatively small fracture orientation angle and relatively small fragment angulation.
Keywords: Fracture, Fracture orientation, Internal fixation, Odontoid process
INTRODUCTION
Various internal fixation methods using either the anterior or the posterior approach have been described for the treatment of acute type II and rostral type III odontoid fractures, and anterior screw fixation has become the most widely used procedure for the stabilization of type II and rostral shallow type III odontoid fractures. This method has several advantages over a posterior C1-2 arthrodesis, such as less surgically induced soft-tissue trauma, no requirement for bone grafting, a lower risk of injury to vertebral arteries, and the preservation of C1-2 rotational motion2,3,5,6,8,9,13,15,17-19,21). However, the utility of anterior screw fixation is limited by non-reducible fractures, fragment geometry or body habitus, such as a barrel-shaped chest, a short neck, and cervical or thoracic kyphosis, which may prevents proper trajectory for screw placement1,4,7). The major recognized anatomical contraindications include a comminuted fracture at the base of the dens and a disrupted transverse ligament1,8,14,17-19). In addition, some authors have reported that fracture line orientation also affected procedural success. Subach et al.19) concluded that sagittally oblique fractures should be considered a contraindication to anterior odontoid screw fixation. Recently, in a study of a modified classification of type II odontoid fractures, it was proposed that Subtype C fractures, where the fracture line passes from anterior inferior to posterior superior, and fractures with significant comminution are unsuitable for anterior screw fixation, so posterior atlantoaxial stabilization has been shown to yield good long-term results10). However, although several studies have reported successful fusion rates after anterior odontoid screw fixation of type II and rostral shallow type III fractures1,4,7,11,12), it remains debatable whether an anterior oblique fracture orientation is really a contraindication to anterior odontoid screw fixation.
Accordingly, we designed this preliminary retrospective study to investigate the feasibility of anterior odontoid screw fixation for type II and rostral shallow type III fracture with an anterior oblique fracture orientation.
MATERIALS AND METHODS
Patient population
After obtaining approval from the institutional review board of our institute, medical charts, imaging studies, and follow-up findings of all patients were retrospectively reviewed and analyzed. From January 2002 to December 2008, 55 consecutive patients with a diagnosis of a type II or a rostral shallow type III odontoid fracture were treated by surgical internal fixation at our institute. Of these 55 patients, we analyzed 16 patients with Anderson and D'Alonzo type II or a rostral shallow type III odontoid fracture with anterior oblique fracture orientation. Of these 16 patients, 8 (group 1) were treated by anterior odontoid screw fixation, and 8 (group 2) by posterior C1-2 arthrodesis. Clinical case summaries for the 16 study subjects are shown in Table 1. Surgical outcomes in these two treatment groups were retrospectively analyzed and compared. None of the 8 patients selected for anterior odontoid screw fixation had a major contraindication, such as, a barrel chest, a short neck, a ruptured transverse ligament or a substantial non-reducible fixed fragment.
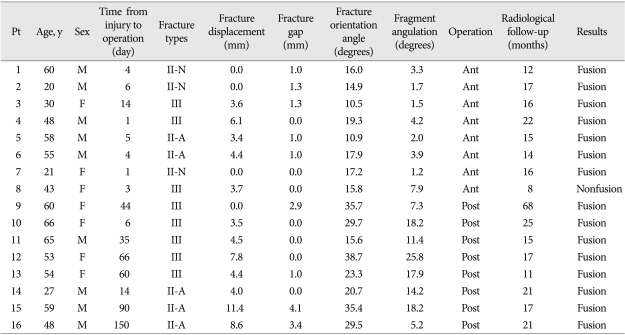
Table 1.
Clinical case summary of 16 patients of odontoid fractures type II and rostral type III with anterior oblique fracture orientation
Fracture types : II-A anteriorly displaced, II-P posteriorly displaced, II-N non-displaced. Pt : patient, Ant : anterior odontoid screw fixation, Post : posterior C1-C2 fusion
All fractures were preoperatively assessed using initial conventional anterior, open-mouth, and lateral radiographs, 3-dimensional computed tomographic (CT) scans, and magnetic resonace images.
Measurement of radiologic parameters
The preoperative analyses of radiologic parameters included degree of fracture displacement, fracture gap, fracture orientation angle, and fragment angulation. Fracture displacements were measured perpendicularly from a line through the posterior margin of the fracture, drawn parallel to the posterior wall of the vertebral body to the dorsal aspect of the dens. Fracture orientation angle and fragment angulations were measured in each case using sagittal reconstruded CT images using Cobb's method. (Fig. 1) Type II and rostral shallow type III fractures were classified as anteriorly displaced (Type II-A), posteriorly displaced (Type II-P), or non-displaced (Type II-N) based on evaluations of initial lateral cervical radiographs9). Fracture orientations were classified according to the antero-posterior direction of the fracture line as, anterior oblique, horizontal, or posterior oblique, as suggested by Apfelbaum et al.4) (Fig. 2).
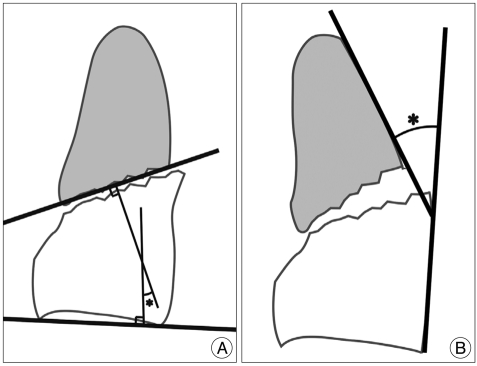
Fig. 1.
Diagram showing Cobb's method of measuring fracture orientation angles (A) and fragment angulation (B).
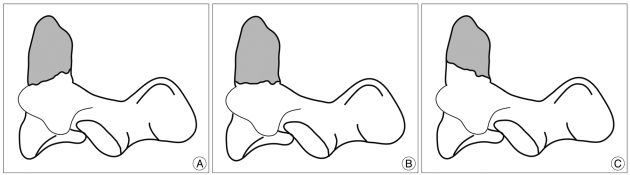
Fig. 2.
Classification of odontoid fractures by fracture orientation. Anterior oblique (A), horizontal (B), and posterior oblique (C). This classification system is based on the inferior direction of fracture slope, as demonstrated on lateral radiographs.
Operative techniques
All surgical procedures were performed by the senior author (J.K.S.). Choice of surgical approach depended on patient age, time from injury to operation, fracture displacement, fracture gap, fracture orientation angle, and fragment angulation. Eight patients with an acute type II or a rostral shallow type III fractures with a small fracture orientation angle or small fragment angulation underwent anterior screw fixation. The remaining eight patients, who had a large fracture orientation angle or a large fragment angulation, were treated by posterior C1-C2 fusion. The surgical technique used for anterior odontoid screw fixation has been previously described by the senior author (J.K.S.)14). Of the 8 patients treated by posterior C1-C2 fusion, two patients underwent posterior C1-2 transarticular screw fixation, and 6 underwent C1 lateral mass and C2 pedicular screw fixation.
Follow-Up and Evaluation of fusion
All patients underwent serial postoperative radiological examinations to verify screw position, fracture alignment, and fusion status. Follow-up studies included cervical spine radiographs (open mouth, flexion, and extension views) at 6 weeks and 3, 6, 12 months after surgery, and 3-D CT scans of the upper cervical spine at 6 or 12 months after surgery. Follow-ups were terminated when fractures were considered to be clinically and radiographically stable.
Strict radiographic criteria were used to assess fusion using dynamic radiographs (in flexion and extension views) and 3-D CT scans. Solid bone fusion was defined as the presence of a bony bridge and the definite continuity of cortical bone. Nonfusion was defined as a definite fracture gap with abnormal motion of the fractured dens on dynamic radiographs and on the 3-D CT scan.
Statistical analysis
The statistical analysis was performed using SPSS version 17 for Windows (SPSS, Inc., Chicago, IL, USA). All data are reported as mean±standard deviations. Significant differences were determined using the two sample t-test. Values not normally distributed were analyzed using the nonparametric Mann-Whitney U test. Two-sided probability testing was used, and a probability value ≤0.05 was considered statistically significant.
RESULTS
Patient Population
Baseline demographic and clinical characteristics of the 16 study subjects are summarized in Table 2. As outlined in Table 2, 8 (group 1) were treated by anterior odontoid screw fixation, and 8 (group 2) by posterior C1-2 arthrodesis. In group 1, there were 5 male and 3 female patients whose ages ranged from 20 to 60 years (mean age±standard deviation, 41.9±16.3 years). The causes of injuries were a traffic accident in 6, and a ground-level fall in 2. Follow-up ranged from 8 to 22 months (mean, 15.0±4.1 months). In group 2, there were 4 men and 4 women with ages ranging from 27 to 66 years (mean age 54.0±12.5 years). The causes of injuries were a traffic accident in 2, and a ground-level fall in 6. Follow-up ranged from 11 to 68 months (mean, 24.4±18.1 months). Mean age and mean follow-up were not significantly different in two groups. (p=0.117 and 0.102, respectively). However, mean times from injury to operation were significantly different (4.8±4.1 days in group 1, and 58.1±46.2 days in group 2).
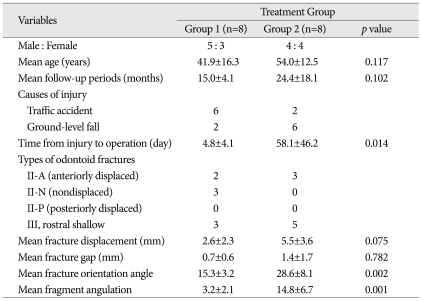
Table 2.
Baseline Demographic and Clinical Characteristics Obtained in 16 patients
Radiologic parameters
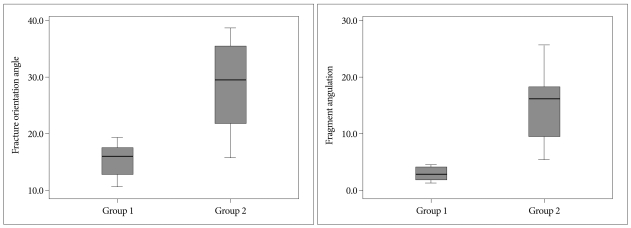
In group 1, fracture types were as follows; type II-A in 2 patients, II-N in 3, rostral shallow type III in 3 and, none with type II-P. In group 2, 3 patients had a type II-A fracture, and the other 5 patients had rostral and shallow type III fractures. Mean fracture displacements were 2.6±2.3 mm in group 1, and 5.5±3.6 mm in group 2, which were not significantly different (p=0.075), and similarly, mean fracture gap were also not significantly different (0.7±0.6 mm in group 1, and 1.4±1.7 mm in group 2). However, mean fracture orientation angles, and mean fragment angulations were significantly different; mean fracture orientation angles were 15.3±3.2 degrees in group 1, and 28.6±8.1 degrees in group 2 (p=0.002), and mean fragment angulations were 3.2±2.1 degrees in group 1, and 14.8±6.7 degrees in group 2 (p=0.001) (Fig. 3).
Fig. 3.
Box plots illustrating fracture orientation angles (A), and fragment angulations (B) in the two groups. Significant intergroup differences were found for these parameters (p=0.002 and 0.001, respectively).
Overall fusion rate and complication
No patient was lost during follow-up, and thus the follow-up data of all 16 study subjects were analyzed. There were no intraoperative complications, and no infection or hematoma was recorded. In all patients, successful screw positioning was verified by postoperative 3-D CT. In group 1, 7 patients achieved solid bone fusion (87.5%), but the remaining patient experienced screw back-out of the C-2 body two months after anterior odontoid screw fixation. The patient involved was a 43-year-old female with a type III fractures and associated fractures extending into the C-2 body and pedicle, which were recognized preoperatively, but were believed to afford an acceptable substrate for anterior odontoid screw fixation. This patient underwent additional posterior C1-C2 screw fixation. (Patient No. 8) All patients treated by posterior C1-C2 fusion in group 2 achieved successful bone fusion at last radiological follow-up. No patients in either groups manifested neurological impairment during follow-up. However, one patient in group 2 reported a transient occipital headache.
DISCUSSION
Operative stabilization is preferred by most authors over external immobilization for the treatment of type II and rostral shallow type III fractures of the odontoid process2,4,8,9,21). Although various internal fixation methods using either the anterior or the posterior approach have been described for the treatment of these fracture types, the optimal surgical methods remain controversial1,3-5,7,11,12,15,16,18,20). Since the reports issued by Nakanishi et al. and by Böhler, anterior screw fixation has become the most widely used procedure for the stabilization of type II and rostral shallow type III odontoid fractures3-5,7). This method has several advantages over posterior C1-2 fusion, namely, less surgical soft-tissue trauma, no requirement for bone grafting, a lower risk of injury to vertebral arteries, and the preservation of C1-2 rotational motion1,3-5,7,14). However, two requirements must be met for the patients to be considered an appropriate candidate for anterior odontoid screw fixation. The first is an intact transverse atlantal ligament, and the second requirement is the ability to adequately reduce the fracture and properly align the fragments1,4,7,14,19).
Recently, some authors have reported that fracture line orientation also affected procedural success. Subach et al.19) concluded that sagittally oblique fractures should be considered a contraindication to anterior odontoid screw fixation. In a study of modified classification of type II odontoid fractures, it has been proposed as the Subtype C fracture, in which fracture line pass from anterior inferior to posterior superior (i.e., anterior oblique direction) or fractures with significant comminution. These fracture patterns are not appropriate for anterior screw fixation, so posterior atlantoaxial stabilization has been shown to yield good long-term results10). However, it remains to be determined whether an anterior oblique fracture orientation is really a contraindication to anterior odontoid screw fixation, because few reports of clinical experiences and outcomes have been issued.
Although several studies have reported successful fusion rates after anterior odontoid screw fixation of type II and rostral shallow type III fractures, there are some controversies about risk factors of fusion failure after anterior odontoid screw fixation1,4,7,11,12). In the literature, some authors have regarded age, time delay from injury to operation, fracture displacement, and fracture gap as risk factors of fusion failure after anterior odontoid screw fixation1,3-5,7-9,11,13,17,19). At our institute, we evaluated the surgical results of 41 patients with a type II or a rostral shallow type III fracture treated by anterior odontoid screw fixation, and we found that a surgical delay of more than 1 week and a fracture gap of ≥2 mm were significant risk factors of fusion failure. However, patient age and fracture displacement were not found to be significantly associated with fusion failure (unpublished data). In our institute, all patients with a type II or a rostral shallow type III odontoid fracture, according to the Anderson and D'Alonzo classification system, were treated by anterior odontoid screw fixation, irrespective of the age of the patient. However, patients that presented for delayed treatment of odontoid fractures (subacute or chronic fractures) were treated by posterior C1-C2 fusion rather than anterior odontoid screw fixation. Thus, in the present study, the two study groups were significantly different with respect to mean time from injury to operation (4.8±4.1 days in group1, and 58.1±46.2 days in group 2).
In a study by Agrillo et al,1) 7 of 9 elderly patients with remote type II axis fractures developed solid bone fusion (77%), and one patient achieved non-anatomic bone fusion , even though the fracture line was oriented in a cranial-posterior to caudal-anterior direction (i.e., anterior oblique direction). However, in a recent study conducted by Lee et al.13) two reasons were given for sagittally oblique fractures considered a contraindication to anterior odontoid screw fixation. First, fractures that are oblique across the neck of the odontoid can become misaligned following screw placement, because of shearing forces generated by the lag screw. This misalignment increases the stress on the fixation. Second, the posterior aspect of the odontoid tip fragment has too little bone for the screw to hold, and thus any force applied to the construct in flexion-extension may cause failure by fracturing the posterior aspect of the odontoid tip or the anterior body of the axis.
In the largest series conducted on direct anterior screw fixation for recent and remote odontoid fractures by Apfelbaum et al.4) the effects of age, sex, fracture orientation, direction of odontoid displacement, and degree of odontoid displacement were evaluated on the rate of anatomical fusion of recent odontoid fractures, and the only variable found to be exerted a significant effect on anatomical bone union was the odontoid fracture orientation. In addition, in this large-scale study, a significantly (p<0.05) lower rate of anatomical bone fusion was found in 16 patients with an anterior oblique fracture orientation than in patients with a posterior oblique or horizontal fracture orientation.
In the present series, we describe our experiences of 16 patients with Anderson and D'Alonzo type II or rostral shallow type III odontoid fractures with an anterior oblique fracture orientation. Even though fracture lines were oriented in the anterior oblique direction, we carefully selected 8 patients with a relatively small fracture orientation angle and small fragment angulation for anterior odontoid screw fixation. Solid bone fusion was documented radiologically in 7 of 8 patients treated by anterior odontoid screw fixation in group 1 (87.5%). However, in cases with a relatively large fracture orientation angle and large fragment angulation, we believe that anterior oblique fracture orientation is a contraindication to anterior odontoid screw fixation. Thus, we performed posterior C1-C2 fusion rather than anterior odontoid screw fixation in the remaining 8 patients. As mentioned above, our two study groups differed significantly in terms of mean fracture orientation angle, (15.3±3.2 degrees vs. 28.6±8.1 degrees, group 1 vs. 2, respectively) and mean fragment angulation (3.2±2.1 degrees vs. 14.8±6.7 degrees, respectively) (p=0.002 and 0.001, respectively) However, no significant intergroup difference was found regarding patient age, fracture displacement, or fracture gap (p=0.117, 0.075, 0.782, respectively).
The major limitation of this study is that the 16 patients were not randomized. All patients were placed into the two groups according to our treatment algorithm that used anterior screw fixation in only the 8 who had the smallest fracture orientation and angulations. Our data does not provide information what would have occurred if patients were assigned to another group. And this study is limited by the relatively small number of the patients recruited, as it was based on a retrospective review conducted at a single institution. However, reports of clinical experiences and outcomes of anterior screw fixation of type II and rostral shallow type III fractures with an anterior oblique fracture orientation are sparse in the literature. Accordingly, we suggest that this topic needs further study.
CONCLUSION
Although the optimal treatment of type II and rostral shallow type III odontoid fractures with an anterior oblique fracture orientation remains controversial, we achieved successful bony fusion in 7 of 8 patients (87.5%) treated by anterior screw fixation in this retrospective study.
Even when the fracture lines of type II and rostral shallow type III fractures are oriented in an anterior oblique direction, anterior odontoid screw fixation can be feasible in carefully selected patients with a relatively small fracture orientation angle and relatively small fragment angulation.
References
- 1.Agrillo A, Russo N, Marotta N, Delfini R. Treatment of remote type II axis fractures in the elderly : feasibility of anterior odontoid screw fixation. Neurosurgery. 2008;63:1145–1150. doi: 10.1227/01.NEU.0000335780.87219.E9. discussion 1150-1151. [DOI] [PubMed] [Google Scholar]
- 2.Anderson LD, D'Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–1674. [PubMed] [Google Scholar]
- 3.Andersson S, Rodrigues M, Olerud C. Odontoid fractures : high complication rate associated with anterior screw fixation in the elderly. Eur Spine J. 2000;9:56–59. doi: 10.1007/s005860050009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Apfelbaum RI, Lonser RR, Veres R, Casey A. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg. 2000;93:227–236. doi: 10.3171/spi.2000.93.2.0227. [DOI] [PubMed] [Google Scholar]
- 5.Börm W, Kast E, Richter HP, Mohr K. Anterior screw fixation in type II odontoid fractures : is there a difference in outcome between age groups? Neurosurgery. 2003;52:1089–1092. discussion 1092-1094. [PubMed] [Google Scholar]
- 6.Dai LY, Yuan W, Ni B, Liu HK, Jia LS, Zhao DL, et al. Surgical treatment of nonunited fractures of the odontoid process, with special reference to occipitocervical fusion for unreducible atlantoaxial subluxation or instability. Eur Spine J. 2000;9:118–122. doi: 10.1007/s005860050221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dailey AT, Hart D, Finn MA, Schmidt MH, Apfelbaum RI. Anterior fixation of odontoid fractures in an elderly population. J Neurosurg Spine. 2010;12:1–8. doi: 10.3171/2009.7.SPINE08589. [DOI] [PubMed] [Google Scholar]
- 8.Fountas KN, Kapsalaki EZ, Karampelas I, Feltes CH, Dimopoulos VG, Machinis TG, et al. Results of long-term follow-up in patients undergoing anterior screw fixation for type II and rostral type III fractures. Spine. 2005;30:661–669. doi: 10.1097/01.brs.0000155415.89974.d3. [DOI] [PubMed] [Google Scholar]
- 9.Geisler FH, Cheng C, Poka A, Brumback RJ. Anterior screw fixation of posteriorly displaced type II odontoid fractures. Neurosurgery. 1989;25:30–37. doi: 10.1097/00006123-198907000-00006. discussion 37-38. [DOI] [PubMed] [Google Scholar]
- 10.Grauer JN, Shafi B, Hilibrand AS, Harrop JS, Kwon BK, Beiner JM, et al. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J. 2005;5:123–129. doi: 10.1016/j.spinee.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 11.Hadley MN, Dickman CA, Browner CM, Sonntag VK. Acute axis fractures: a review of 229 cases. J Neurosurg. 1989;71:642–647. doi: 10.3171/jns.1989.71.5.0642. [DOI] [PubMed] [Google Scholar]
- 12.Koivikko MP, Kiuru MJ, Koskinen SK, Myllynen P, Santavirta S, Kivisaari L. Factors associated with nonunion in conservatively-treated type-II fractures of the odontoid process. J Bone Joint Surg Br. 2004;86:1146–1151. doi: 10.1302/0301-620x.86b8.14839. [DOI] [PubMed] [Google Scholar]
- 13.Lee SC, Chen JF, Lee ST. Management of acute odontoid fractures with single anterior screw fixation. J Clin Neurosci. 2004;11:890–895. doi: 10.1016/j.jocn.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 14.Lee SH, Sung JK. Anterior odontoid fixation using a 4.5-mm Herbert screw : the first report of 20 consecutive cases with odontoid fracture. Surg Neurol. 2006;66:361–366. doi: 10.1016/j.surneu.2006.04.018. discussion 366. [DOI] [PubMed] [Google Scholar]
- 15.Lennarson PJ, Mostafavi H, Traynelis VC, Walters BC. Management of type II dens fractures : a case-control study. Spine. 2000;25:1234–1237. doi: 10.1097/00007632-200005150-00006. [DOI] [PubMed] [Google Scholar]
- 16.Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffl WG. Halo vest immobilization in the elderly : a death sentence? J Trauma. 2005;59:350–356. doi: 10.1097/01.ta.0000174671.07664.7c. discussion 356-358. [DOI] [PubMed] [Google Scholar]
- 17.Platzer P, Thalhammer G, Ostermann R, Wieland T, Vécsei V, Gaebler C. Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine. 2007;32:1714–1720. doi: 10.1097/BRS.0b013e3180dc9758. [DOI] [PubMed] [Google Scholar]
- 18.Sasso RC. C2 dens fractures : treatment options. J Spinal Disord. 2001;14:455–463. doi: 10.1097/00002517-200110000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Subach BR, Morone MA, Haid RW, Jr, McLaughlin MR, Rodts GR, Comey CH. Management of acute odontoid fractures with single-screw anterior fixation. Neurosurgery. 1999;45:812–819. doi: 10.1097/00006123-199910000-00015. discussion 819-820. [DOI] [PubMed] [Google Scholar]
- 20.Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006;60:199–203. doi: 10.1097/01.ta.0000197426.72261.17. [DOI] [PubMed] [Google Scholar]
- 21.Tun K, Kaptanoglu E, Cemil B, Yorubulut M, Karahan ST, Tekdemir I. Anatomical study of axis for odontoid screw thickness, length, and angle. Eur Spine J. 2009;18:271–275. doi: 10.1007/s00586-008-0814-7. [DOI] [PMC free article] [PubMed] [Google Scholar]