Abstract
Angiocentric glioma was recently recognized as a distinct clinicopathological entity in the 2007 World Health Organization classification of tumors of the central nervous system. Typically, it presents with seizure in children and young adults. However, our patient did not have a history of seizure. Seizure did not occur up to 6 months after operation. Although it usually does not have calcification brain magnetic resonance imaging in our patient showed T1-hyperintense and T2-hypointense signals with calcification.
Keywords: Angiocentric glioma, Glioma, Neuroepithelial tumors, Seizures, Pathologic Calcification
INTRODUCTION
Angiocentric glioma was recently codified as a new type of brain tumor in the 2007 World Health Organization (WHO) classification of tumors of the central nervous system1,3). It was first described in 2 independent reports in 20052,8). Until 2009, only 31 cases had been reported worldwide2,4-8). It is described as a slowly growing cerebral tumor that typically presents with seizure in children and young adults5). Pathologically, calcification is rarely observed in this tumor. However, in our case, seizure did not occur, and the lesion contained calcification. We report the case of a patient with unusual clinical and radiological features.
CASE REPORT
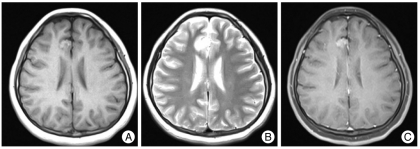
A 10-year-old girl presented at our clinic with 1-week history of dizziness. She complained of left otalgia and gaze nystagmus to the right side. Under the suspicion of left vestibular neuronitis or acute otitis media, she was treated at the otolaryngology department, but dizziness did not improve. Brain magnetic resonance (MR) imaging revealed a calcified mass at the right medial aspect of the frontal cortex (Fig. 1). It showed high signal intensity both in T1- and T2-weight images. Neurologic examination revealed nonspecific findings except nystagmus.
Fig. 1.
A : The T1-weighted magnetic resonance (MR) image shows a high signal intensity lesion in the right medial frontal cortex area. B : The T2-weighted MR image obtained at the same level shows a hyperintense tumor signal. C : Axial T1-weighted MR image with contrast shows the same lesion which is non-enhanced.
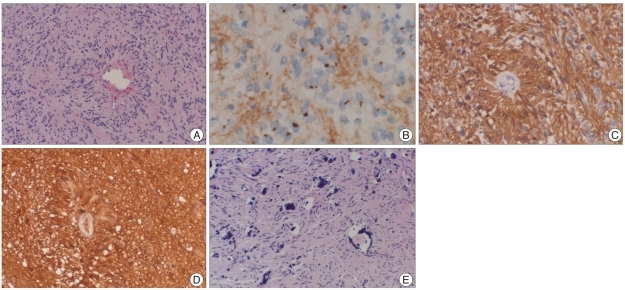
Under the general anesthesia, a bicoronal incision was made in the right frontal area. Bone flap was elevated just above the mass near the superior sagittal sinus. Using a surgical microscope, the interhemispheric space was separated, which disclosed a slightly firm and discolored mass with scattered calcified tissue in the cingulate gyrus. The tumor margin was not clean and similar in color as normal brain tissue. Under the microscopic guide, the tumor mass was totally removed. On the histopathological examination, elongated tumor cells occasionally forming perivascular pseudorosettes were observed by hematoxylin-eosin staining. The tumor cells were positive for GFAP and S-100 protein. The Ki-67 labelling index was less than 1%. EMA-positive "dot-like" structures corresponding to the microlumens were noted by DAB staining (Fig. 2). The perivascular orientation of tumor cells was compatible with angiocentric glioma WHO grade I.
Fig. 2.
A : Elongated tumor cells occasionally form perivascular pseudorosettes (H&E ×100). B : EMA-positive "dot-like" structures correspond to the microlumens (DAB ×400). C : Tumor cells in perivascular pseudorosettes express GFAP (DAB ×200). D : Tumor cells in perivascular pseudorosettes express S-100 (H&E ×200). E : Tumor consist of calcification (H&E ×100).
After 2 weeks, dizziness was much improved, and she showed no neurological deficits. At the 9-months follow-up, she presented no seizure or dizziness. Anticonvulsant was administered once, before operation, and for 1 week after operation.
DISCUSSION
In the 2007 WHO classification of tumors of the central nervous system, angiocentric glioma was grouped with astroblastoma and choroid glioma of the third ventricle in the category of 'other neuroepithelial tumors', which was previously designated as 'tumors of uncertain origin'3). It was assigned to WHO grade I due to its clinically benign behavior and feasibility of curative surgery. This new type of brain tumor was first described in 2 independent reports in 20052,8). Until 2009, only 31 cases had been reported in the United states (11 cases)6,8), France (10 cases)2), Austria/Germany (8 cases)5), New Zealand (1 case)4) and Japan(1 case)7). Our case is the second one in Asian countries.
Angiocentric glioma is described as a slowly growing cerebral tumor that typically presents with seizure in children and young adults3,5). Angiocentric glioma usually develops at the ages between 2 and 37 years2,4-8). The mean age of patients is 10.6 years. Our patient was 13 years old. The male to female ratio of angiocentric glioma is reported to be 17 : 142,4-8).
MR images of most angiocentric gliomas demonstrate a supratentorial, non-enhancing, T1-hypointense/T2-hyperintense lesion6). However, our case showed a T1-hyperintense signal. Calcified angiocentric glioma had been reported in only 2 among the 31 cases. Angiocentric glioma is a unique brain tumor that account for a considerable proportion of medically refractory epilepsy in children and young adults and that is amenable to neurosurgical intervention6). Only one among the 31 previously 2011reported cases did not have seizure as an initial symptom6). Our case is the second one. However, the relationship between calcification and seizure has not yet been determined. Our patient showed calcification without seizure unlike the previously reported patients.
Angiocentric glioma is histopathologically categorized as a unique entity, although its cytogenesis remains to be elucidated. It is characterized by monomorphous bipolar cells and an angiocentric growth pattern. It has a positive immunoreactivity for EMA, GFAP, S-100 protein or vimentin but not for neuronal antigens3). In this case, the specimens showed positive immunoreactivities for EMA, GFAP and S-100 protein. This low-grade neoplasm can originate from astrocytic and ependymal lineges8), or from radial glia or neuronal origin2). Despite frequent extension of angiocentric glioma to the ventricular wall and the presence of microscopic features suggestive of ependymal differentiation, predominant clinical symptoms, cortical location, architectural pattern and outcome are insufficient to designate this entity as an ependymoma variant. Therefore, angiocentric glioma was designated as astroblastoma and choroid glioma of the third ventricle in the category of 'other neuroepithelial tumors', which was previously designated as 'tumors of uncertain origin'3). It showed an excellent prognosis in all documented surgical cases of WHO grade I, regardless of its origin site2,4-8).
CONCLUSION
We reported a patient with angiocentric glioma who had unusual clinical and radiological findings. The former is no seizure history and the latter is intratumoral calcification.
References
- 1.Brat DJ, Scheithauer BW, Fuller GN, Tihan T. Newly codified glial neoplasms of the 2007 WHO classification of tumors of the central nervous system : angiocentric glioma, pilomyxoid astrocytoma and pituicytoma. Brain Pathol. 2007;17:319–324. doi: 10.1111/j.1750-3639.2007.00082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lellouch-Tubiana A, Boddaert N, Bourgeois M, Fohlen M, Jouvet A, Delalande O, et al. Angiocentric neuroepithelial tumor (ANET) : a new epilepsy-related clinicopathological entity with distinctive MRI. Brain Pathol. 2005;15:281–286. doi: 10.1111/j.1750-3639.2005.tb00112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97–109. doi: 10.1007/s00401-007-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lum DJ, Halliday W, Watson M, Smith A, Law A. Cortical ependymoma or monomorphous angiocentric glioma. Neuropathology. 2008;28:81–86. doi: 10.1111/j.1440-1789.2007.00831.x. [DOI] [PubMed] [Google Scholar]
- 5.Preusser M, Hoischen A, Novak K, Czech T, Prayer D, Hainfellner JA, et al. Angiocentric glioma report of clinico-pathologic and genetic findings in cases. Am J Surg Pathol. 2007;31:1709–1718. doi: 10.1097/PAS.0b013e31804a7ebb. [DOI] [PubMed] [Google Scholar]
- 6.Shakur SF, McGirt MJ, Johnson MW, Burger PC, Ahn E, Carson BS, et al. Angiocentric glioma : a case series. J Neurosurg Pediatr. 2009;3:197–202. doi: 10.3171/2008.11.PEDS0858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sugita Y, Ono T, Ohshima K, Niino D, Ito M, Toda K, et al. Brain surface spindle cell glioma in a patient with medically intractable partial epilepsy : a variant of monomorphous angiocentric glioma? Neuropathology. 2008;28:516–520. doi: 10.1111/j.1440-1789.2007.00849.x. [DOI] [PubMed] [Google Scholar]
- 8.Wang M, Tihan T, Rojiani AM, Bodhireddy SR, Prayson RA, Iacuone JJ, et al. Monomorphousangiocentric glioma : a distinctive epilptogenic neoplasm with features of infiltrating astrocytoma and ependymoma. J Neuropathol Exp Neurol. 2005;64:875–881. doi: 10.1097/01.jnen.0000182981.02355.10. [DOI] [PubMed] [Google Scholar]