Abstract
Context
Borderline personality disorder (BPD) is traditionally considered chronic and intractable.
Objective
To compare the course of BPD’s psychopathology and social function with that of other personality disorders and with major depressive disorder (MDD) over 10 years.
Design
A collaborative study of treatment-seeking, 18-to 45-year-old patients followed up with standardized, reliable, and repeated measures of diagnostic remission and relapse and of both global social functioning and subtypes of social functioning.
Setting
Nineteen clinical settings (hospital and outpatient) in 4 northeastern US cities.
Participants
Three study groups, including 175 patients with BPD, 312 with cluster C personality disorders, and 95 with MDD but no personality disorder.
Main Outcome Measures
The Diagnostic Interview for DSM-IV Personality Disorders and its follow-along version (the Diagnostic Interview for DSM-IV Personality Disorders–Follow-Along Version) were used to diagnose personality disorders and assess changes in them. The Structured Clinical Interview for DSM-IV Axis I Disorders and the Longitudinal Interval Follow-up Evaluation were used to diagnose MDD and assess changes in MDD and in social function.
Results
Eighty-five percent of patients with BPD remitted. Remission of BPD was slower than for MDD (P<.001) and minimally slower than for other personality disorders (P<.03). Twelve percent of patients with BPD relapsed, a rate less frequent and slower than for patients with MDD (P<.001) and other personality disorders (P=.008). All BPD criteria declined at similar rates. Social function scores showed severe impairment with only modest albeit statistically significant improvement; patients with BPD remained persistently more dysfunctional than the other 2 groups (P<.001). Reductions in criteria predicted subsequent improvements in DSM-IV Axis V Global Assessment of Functioning scores (P<.001).
Conclusions
The 10-year course of BPD is characterized by high rates of remission, low rates of relapse, and severe and persistent impairment in social functioning. These results inform expectations of patients, families, and clinicians and document the severe public health burden of this disorder.
Prior research on the longitudinal course of borderline personality disorder (BPD) has included many short-term prospective studies complemented by a few seminal long-term retrospective studies.1 These studies, largely completed in the decade from 1985 to 1995, indicated that BPD is unstable and that many patients get better, thereby challenging the widely held view of BPD as an unremittingly chronic condition. Still, the methodological and design limitations that characterized this prior literature diminished its impact, and a firmly entrenched pessimism about the prognosis of patients with BPD has persisted. Moreover, these limitations have kept open the question about whether the course of BPD is sufficiently distinct to fulfill the standards of diagnostic validation set by Robins and Guze.2 Both the Collaborative Longitudinal Personality Disorders Study (CLPS)3 and a concurrent long-term prospective study, the McLean Study of Adult Development (MSAD),4,5 were undertaken to address these limitations in scientific and clinical credibility.
This report extends prior CLPS accounts of the course of BPD6–11 by using the perspective of the study’s full 10-year follow-up and by concurrently examining both changes in psychopathology (remission and relapse) and social functioning. Psychopathology is the primary focus of clinical interventions, whereas the associated social dysfunction, via direct costs and effects on others, is the primary public health concern. By examining both, this report allows us to examine how these 2 domains interact.
METHODS
DESIGN
The CLPS is a multisite, naturalistic, repeated-measures, longitudinal study of individuals with 4 personality disorders, BPD, schizotypal personality disorder, avoidant personality disorder (AVPD), and obsessive-compulsive personality disorder (OCPD), and a comparison group of patients with major depressive disorder (MDD) without personality disorder.
SAMPLE
The CLPS was approved by the institutional review boards at all participating sites. All patients gave written informed consent after procedures were fully explained. Each of the 4 sites (Brown University, Columbia University, Harvard University, and Yale University) recruited consecutive eligible patients from multiple clinical subsites (N=19 subsites).3 The resulting samples were most frequently ascertained from psychiatric outpatient clinics (43%) and from psychiatric hospitals (12%). All participants were aged 18 to 45 years, an age range that would best generalize to clinical samples and would allow follow-up through the most relevant stage of life. Our personality disorder samples were identified by semistructured interview (Diagnostic Interview for DSM-IV Personality Disorders, see later) with confirmation of the diagnosis (cell assignment) from self-report measures and/or by independent clinical judgment.3 Because the cell-assigned diagnoses are informed by clinical judgment and ensure that our samples are mutually exclusive, this narrower definition of our personality disorder samples was used. While the CLPS also includes subjects with schizotypal personality disorder, that diagnostic group was excluded from this report because their follow-up data involved ratings from in vivo observations that were progressively more difficult to obtain as more assessments were conducted via telephone. Their omission increased the homogeneity of the comparison group with other personality disorders (OPD) by combining the 2 cluster C personality disorders, ie, AVPD and OCPD. Thus, the study’s 3 study groups were patients with BPD (n=175), patients with cluster C OPD (n=312, including 158 with AVPD and 154 with OCPD), and patients with MDD (n=95).3 Our MDD study group was notable for having been selected to exclude any comorbid personality disorder. The 3 diagnostic study groups shared similar age and socioeconomic status; there were, however, more women (75%) in the BPD group than in the OPD (64%) or MDD (60%) cells (P=.01).3
Sixty-six percent of the patients who entered the study completed the full 10 years of follow-up. This report includes 111 patients with BPD (63% of those with BPD who entered), 211 with OPD (including 97 with AVPD [61%] and 114 with OCPD [74%]), and 62 with MDD (65%). Differences in attrition by study cell, age, and sex were not statistically significant.
ASSESSMENTS
The CLPS used repeated comprehensive assessments of the course of personality disorders, of Axis I disorders, and of functional impairment. Personality disorder criteria were assessed with the Diagnostic Interview for DSM-IV Personality Disorders12 at baseline, 6 months, 12 months, and 2, 4, 6, 8, and 10 years. The respective interrater and test-retest κ values at baseline were 0.68 and 0.69 for BPD, 0.68 and 0.73 for AVPD, and 0.71 and 0.74 for OCPD.13 A standardized regression analysis examining how these levels of reliability might affect subsequent criterion counts found that observed rates of remission over time were only minimally affected, ie, changes of 0.003% for BPD, 0.035% for AVPD, and 0.020% for OCPD. The course of personality disorders was also assessed with a non–blindly administered follow-along version of the Diagnostic Interview for DSM-IV Personality Disorders.14 This instrument rates each personality disorder criterion on a scale of 0 (absent or clinically insignificant), 1 (present but of uncertain clinical significance), or 2 (present and clinically significant) points for each month during the time interval queried. Reliability on the Diagnostic Interview for DSM-IV Personality Disorders–Follow-Along Version based on ratings of 2 overlapping time points (month 6 was rated twice for 453 cases) resulted in good κ coefficients: 0.70 for BPD, 0.73 for AVPD, and 0.68 for OCPD.9
Both MDD and the DSM-IV Axis V Global Assessment of Functioning (GAF) score were assessed at baseline using the Structured Clinical Interview for DSM-IV.15 Baseline interrater reliability for MDD was a κ of 0.80, with a test-retest κ of 0.64.13 Follow-along assessments of weekly changes in MDD criteria and yearly changes in GAF score were assessed by the non–blindly administered Longitudinal Interval Follow-up Evaluation (LIFE).16 The LIFE also included monthly ratings (retrospective to the time of previous assessment) of functional impairment with established reliabilities.9,17 The Global Social Adjustment (GSA) scale (social and occupational functioning without contribution from symptoms) was used, with subscales rating functional impairment in relationships (with parents, spouse/partner, and friends), recreation, employment, and satisfaction. Each subscale rates impairment on a scale from 1 to 5 (1 indicating none; 2, satisfactory or good; 3, mild or fair; 4, moderate or poor; and 5, severe or very poor).
ANALYSES
Cumulative Kaplan-Meier survival analyses assessed rates of remission and relapse with a Wilcoxon χ2 test for group equality. Remission was defined as meeting 2 or fewer criteria for BPD. In comparing BPD rates of remission with those of OPD, we used 12-month durations at 2 or fewer criteria for greater clinical significance, whereas in comparing rates of remission of the BPD study group with those of MDD, we used what has become the MDD standard (a Psychiatric Status Rating ≤2, reflecting minimal or no symptoms) of a 2-month duration. Remission from OPD was defined as remaining at 2 or fewer AVPD criteria for patients in the AVPD cell and remaining at 2 or fewer OCPD criteria for those in the OCPD cell. Relapse for BPD was defined as returning to 5 or more criteria (the DSM-IV threshold) for 2 or more months after having remitted. For OPD, relapse was defined as returning to 4 or more criteria (the DSM-IV thresholds) for 2 or more months for AVPD and OCPD cells separately.
Point prevalence analyses were used to assess changes in mean scores for number of BPD criteria and for each individual BPD criterion, for GAF and GSA scores, and for scores on 6 LIFE subscales (and their total). This examination offers an alternative way to document change that is perhaps more clinically recognizable than survival analyses. To characterize individual patterns of improvement, using only those participants who provided at least 5 years of data, we analyzed individual change in GAF scores across follow-up. First, we tabulated how many participants improved their baseline GAF scores by at least 10 points at some time during follow-up as well as the amount of improvement. We then calculated how many consecutive years these persons stayed at a GAF score no more than 5 points worse than their best GAF score. Finally, we noted the lowest postpeak GAF score. These analyses together depict the maximum amount of improvement and how long that improvement was sustained. We contrasted the BPD and OPD groups on these measures using t tests for continuous measures and χ2 tests for dichotomous measures.
Hierarchical linear modeling (HLM)18 analyses were used to test for between-group differences in functioning for the GAF score, the GSA score, and the continuous measures listed in Table 1. The HLM analyses included main effects for BPD vs OPD vs MDD, a term for linear change over time, and interaction terms for time × BPD vs OPD and time × BPD vs MDD. For more detailed examination of dichotomized variables over time, ie, employment (full time vs not) and marital status (married or cohabiting vs not), generalized estimating equation analyses with a logistic link function were used. Both the HLM and generalized estimating equation analyses covaried for age, education, and sex. In all of these analyses, we used multiple imputation19 to accommodate missing data. For each separate dependent variable, 25 imputed samples were generated using PROC MI in SAS version 9.2 statistical software (SAS Institute, Inc, Cary, North Carolina); results were aggregated across imputations using PROC MIANALYZE. It should be noted that the effective df for tests aggregated by multiple imputation are computed as a function of the actual sample size and missingness20; thus, estimated df will vary from test to test.
Table 1.
Social Functioning as Measured by Longitudinal Interval Follow-up Evaluation Subscalesa
| Subscale | Baseline | 2 y | 4 y | 6 y | 8 y | 10 y | Significant Covariatesb |
|---|---|---|---|---|---|---|---|
| Employment | Age (3), education (−) | ||||||
| BPD | |||||||
| Score, mean (SD) | 2.82 (2.18) | 2.34 (1.40) | 2.28 (1.27) | 2.25 (1.30) | 2.04 (1.24) | 2.13 (1.13) | |
| No. | 145 | 99 | 100 | 84 | 75 | 64 | |
| OPD | |||||||
| Score, mean (SD) | 2.05 (1.13) | 1.93 (1.07) | 1.99 (1.07) | 1.92 (1.06) | 1.91 (1.01) | 1.84 (0.93) | |
| No. | 216 | 216 | 206 | 184 | 172 | 151 | |
| MDD | |||||||
| Score, mean (SD) | 2.14 (1.18) | 1.70 (0.96) | 1.86 (1.13) | 1.69 (0.79) | 1.76 (0.80) | 2.05 (0.94) | |
| No. | 78 | 63 | 63 | 61 | 54 | 42 | |
| Spouse role | Age (3), education (−) | ||||||
| BPD | |||||||
| Score, mean (SD) | 3.20 (1.29) | 2.51 (1.29) | 2.29 (1.15) | 2.13 (1.21) | 2.26 (1.10) | 2.24 (1.16) | |
| No. | 87 | 45 | 48 | 52 | 46 | 49 | |
| OPD | |||||||
| Score, mean (SD) | 2.58 (1.21) | 2.12 (1.00) | 2.16 (1.07) | 2.00 (1.12) | 2.11 (1.03) | 2.17 (1.01) | |
| No. | 158 | 92 | 92 | 101 | 102 | 101 | |
| MDD | |||||||
| Score, mean (SD) | 3.03 (1.38) | 1.92 (1.15) | 1.93 (0.81) | 1.83 (0.87) | 1.88 (1.07) | 1.86 (0.97) | |
| No. | 34 | 25 | 28 | 24 | 26 | 28 | |
| Parent role | Education (−) | ||||||
| BPD | |||||||
| Score, mean (SD) | 3.13 (1.31) | 2.59 (1.11) | 2.40 (1.00) | 2.33 (1.07) | 2.35 (1.08) | 2.48 (1.15) | |
| No. | 166 | 144 | 134 | 123 | 107 | 93 | |
| OPD | |||||||
| Score, mean (SD) | 2.55 (1.18) | 2.33 (0.99) | 2.30 (1.01) | 2.09 (0.98) | 2.17 (1.01) | 2.13 (0.96) | |
| No. | 291 | 266 | 252 | 230 | 203 | 184 | |
| MDD | |||||||
| Score, mean (SD) | 2.26 (1.06) | 2.20 (1.05) | 2.13 (0.97) | 2.10 (1.01) | 1.93 (1.01) | 1.90 (0.93) | |
| No. | 91 | 82 | 78 | 70 | 58 | 52 | |
| Friend role | Age (3), education (−) | ||||||
| BPD | |||||||
| Score, mean (SD) | 3.17 (1.22) | 2.62 (1.12) | 2.56 (1.20) | 2.53 (1.26) | 2.53 (1.18) | 2.69 (1.16) | |
| No. | 175 | 157 | 146 | 139 | 124 | 111 | |
| OPD | |||||||
| Score, mean (SD) | 2.79 (1.24) | 2.46 (1.13) | 2.44 (1.12) | 2.34 (1.15) | 2.42 (1.23) | 2.61 (1.25) | |
| No. | 312 | 287 | 277 | 259 | 233 | 211 | |
| MDD | |||||||
| Score, mean (SD) | 2.44 (1.03) | 1.80 (0.87) | 1.95 (1.02) | 2.00 (0.94) | 2.03 (0.98) | 2.29 (1.11) | |
| No. | 95 | 87 | 84 | 78 | 68 | 62 | |
| Recreation | Age (3), education (−) | ||||||
| BPD | |||||||
| Score, mean (SD) | 3.46 (1.18) | 2.76 (1.29) | 2.73 (1.21) | 2.87 (1.17) | 2.60 (1.04) | 2.60 (1.08) | |
| No. | 175 | 156 | 146 | 139 | 124 | 111 | |
| OPD | |||||||
| Score, mean (SD) | 2.72 (1.18) | 2.38 (1.11) | 2.52 (1.12) | 2.46 (1.08) | 2.42 (1.10) | 2.48 (1.10) | |
| No. | 312 | 287 | 277 | 259 | 233 | 211 | |
| MDD | |||||||
| Score, mean (SD) | 2.94 (1.07) | 2.07 (1.09) | 2.18 (1.10) | 2.08 (0.92) | 2.15 (0.98) | 2.34 (1.13) | |
| No. | 95 | 87 | 84 | 78 | 68 | 62 | |
| Satisfactionc | Age (3), education (−) | ||||||
| BPD | |||||||
| Score, mean (SD) | 3.57 (0.95) | 3.01 (1.10) | 2.91 (1.12) | 2.90 (1.16) | … | … | |
| No. | 175 | 157 | 146 | 139 | … | … | |
| OPD | |||||||
| Score, mean (SD) | 3.06 (0.89) | 2.65 (0.99) | 2.64 (1.01) | 2.58 (1.08) | … | … | |
| No. | 312 | 286 | 277 | 257 | … | … | |
| MDD | |||||||
| Score, mean (SD) | 3.23 (0.84) | 2.35 (0.90) | 2.39 (1.05) | 2.27 (1.03) | … | … | |
| No. | 95 | 86 | 84 | 78 | … | … | |
Abbreviations: BPD, borderline personality disorder; MDD, major depressive disorder; OPD, other personality disorders; ellipses, not applicable.
Reported means use nonmissing data; hierarchical linear modeling analyses were based on multiple imputation. Scores were measured on a scale of 1 to 5, with 1 indicating no impairment; 2, satisfactory or good; 3, mild or fair; 4, moderate or poor; and 5, severe or very poor. All 3 diagnostic cells improved significantly on every measure of social impairment, with P < .001.
For covariates, + indicates that higher covariate scores go with higher (worse) scale scores; − indicates the converse.
Data were not gathered at years 8 and 10.
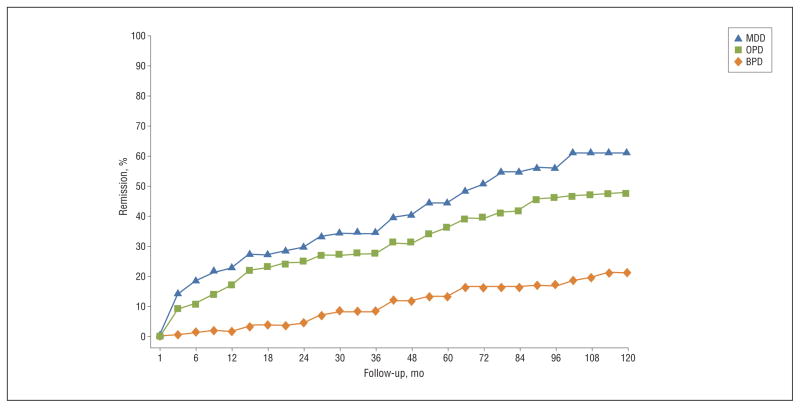
Kaplan-Meier survival analyses examined changes over time on the subgroups whose level of function was considered good based on GAF scores higher than 70.
Lagged HLM analyses with number of BPD criteria and GAF score as time-varying predictors were used to test our hypotheses regarding which predictors would predict subsequent (the next year’s) scores in the other domain. Thus, in 1 analysis, year 2 BPD criteria were used to predict year 3 GAF scores, year 3 BPD criteria were used to predict year 4 GAF scores, and so on. In a separate analysis, the roles of GAF score and BPD criteria were reversed. These analyses also included tests for age, sex, and education as covariates, a main effect for study year, and a year × time-varying predictor interaction. These analyses used multiple imputations for missing data as described earlier.
RESULTS
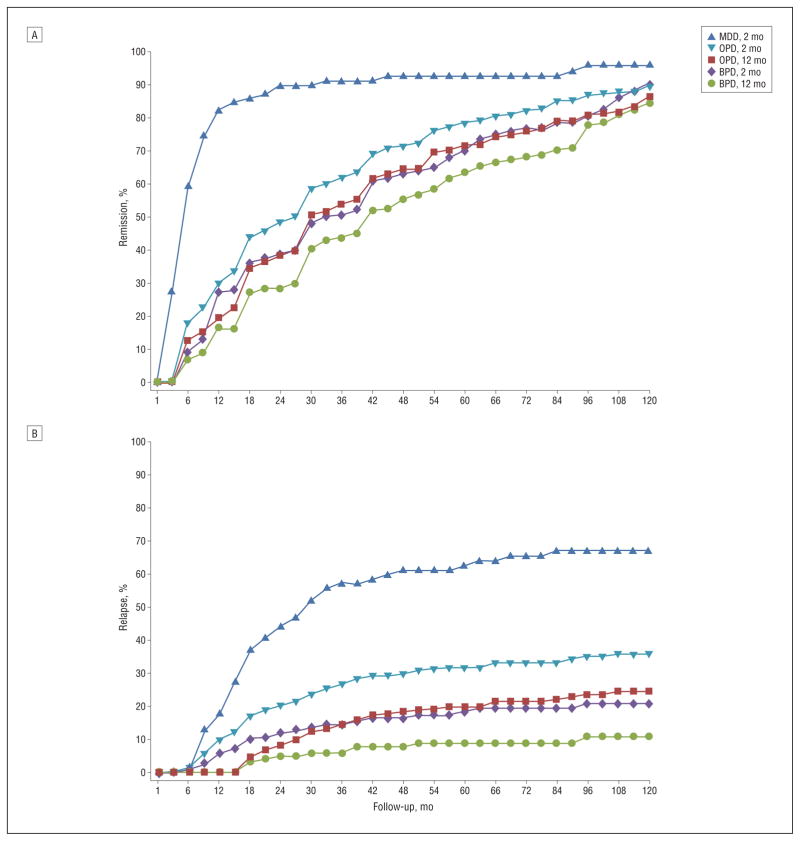
Figure 1A shows that the cumulative rates of remission for BPD over 10 years were 91% (95% confidence interval [CI], 86–96) using the 2-month definition of remission and 85% (95% CI, 78–91) using the 12-month definition, with the greatest rate of change occurring in the earlier years. While the overall rates of remission at 10 years were high for all 3 diagnostic study groups, the time to remission for BPD was significantly longer than for MDD ( ; P<.001) (using the 2-month standard for MDD) but only minimally longer than for cluster C OPD ( ; P=.03) (using the 12-month definition).
Figure 1.
Diagnostic remission (A) and diagnostic relapse (B) of major depressive disorder (MDD), other personality disorders (OPD; either avoidant personality disorder [AVPD] or obsessive-compulsive personality disorder [OCPD]), and borderline personality disorder (BPD). Remission of MDD was based on a Psychiatric Status Rating of less than 2 for 2 consecutive months, and MDD relapse was based on a Psychiatric Status Rating of 5 or 6 for 2 consecutive months. Remission of OPD was defined as either fewer than 2 AVPD criteria for AVPD cases or fewer than 2 OCPD criteria for OCPD cases for 2 or 12 consecutive months, and OPD relapse was defined as returning to more than 4 criteria for 2 months or for either AVPD or OCPD cases separately. Remission of BPD was defined as fewer than 2 criteria for 2 or 12 consecutive months, and BPD relapse was defined as returning to more than 5 criteria for 2 months. Analyses were based on lifetest survival estimates.
Figure 1B shows the cumulative relapse rates for patients with BPD who had remitted using both the 2- and 12-month definitions and how these compare with the MDD and OPD cells. The 10-year relapse rate for BPD was 11% (95% CI, 4–17) for the more clinically significant 12-month definition of remission—a rate that rose to 21% (95% CI, 13–29) using the 2-month definition. Relapses largely occurred in the first 4 years before leveling off. Using the 12-month definition of remission, the relapse rate for the OPD study group at 10 years was 25% (95% CI, 18–31), significantly higher than for BPD ( ; P =.008). The relapse rate for the MDD study group, using a 2-month definition, was significantly higher: 67% (95% CI, 57–78) in the MDD group relapsed by 10 years compared with 21% (95% CI, 13–29) for BPD ( ; P <.001).
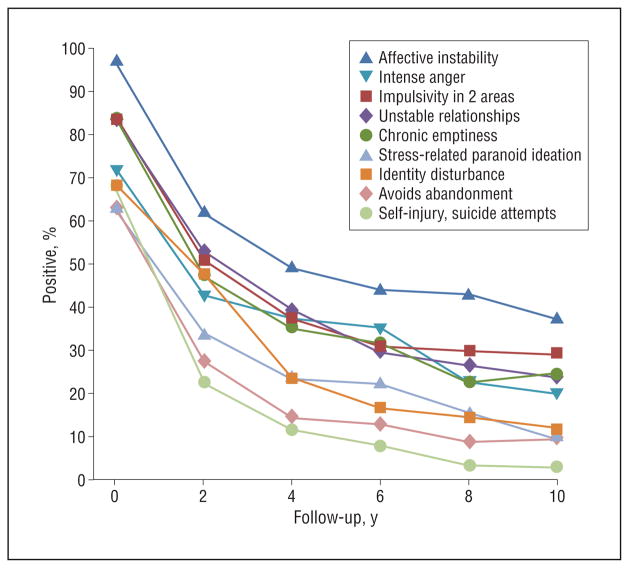
The mean number of criteria met for BPD decreased from 6.7 to 4.3 in the first year and thereafter steadily decreased at a rate of 0.29 criteria per year to a low of 1.7 at 10 years. Only 9% of the patients with BPD remained stably disordered (≥5 criteria) at 10 years. As Figure 2 illustrates, the rates of decline for each of the 9 DSM-IV BPD criteria were similar, with those that were most prevalent at baseline remaining most prevalent after 10 years.
Figure 2.
Prevalence of borderline personality disorder criteria. Positive indicates the cases with a score of 2 (definitely present and clinically significant) for each of the 9 borderline personality disorder criteria on the Diagnostic Interview for DSM-IV Personality Disorders, assessed for the 2 years prior to the follow-up point.
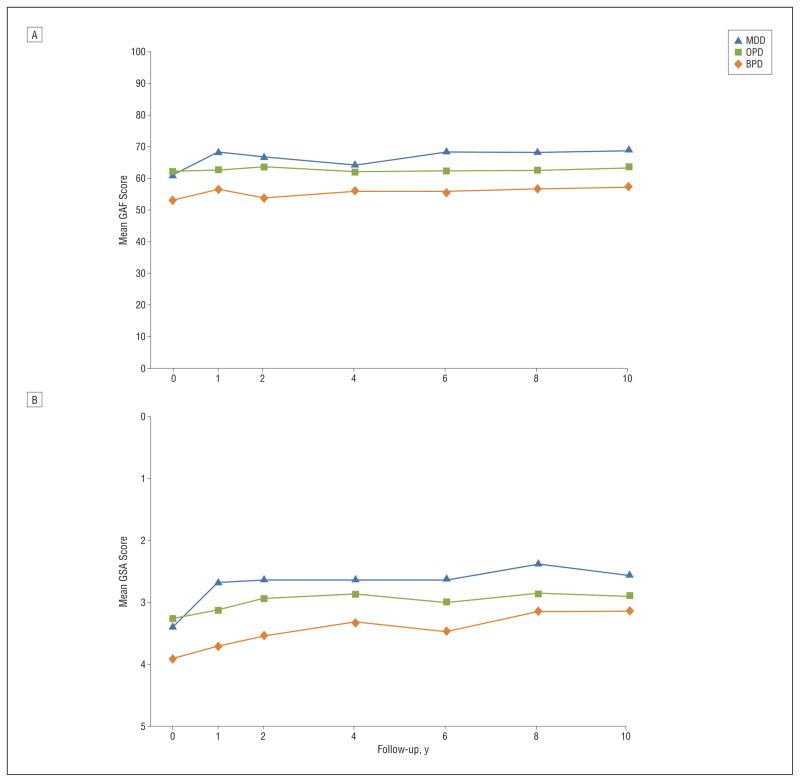
Figure 3A shows change in GAF scores over time. The clinically modest levels of functional improvement for BPD (mean GAF scores increased from 53 to 57), OPD (mean GAF scores increased from 62 to 64), and MDD (mean GAF scores increased from 61 to 69) were each, nonetheless, statistically significant over time (F1,467=26.36; P <.001). Across follow-up, 66% of subjects with BPD and 53% of subjects with OPD had at least 1 year when their GAF score was at least 10 points better than at intake. This difference is statistically significant ( ; P =.01). Of those who improved 10 points or more, the mean (SE) improvement was 12.21 (0.54) points and the mean (SE) number of years of sustained improvement was 2.00 (0.05) years; these measures did not differ between BPD and OPD. Improvements typically were not sustained. The worst GAF score following the best year was a mean (SE) of 16.45 (0.57) points lower; the size of decrement in GAF score did not differ for BPD vs OPD.
Figure 3.
Scores on the Global Assessment of Functioning (GAF) (A) and the Global Social Adjustment (GSA) scale (B). A, A score of 100 represents the best level of overall functioning, and a score of 0 represents the lowest level. B, A score of 0 represents the highest level of social functioning, and a score of 5 represents the lowest level. MDD indicates major depressive disorder; OPD, other personality disorders; and BPD, borderline personality disorder.
An HLM examination of the averaged mean GAF scores over time covaried for age, education, and sex showed that the averaged GAF score for BPD (GAF score 56) was significantly worse than for OPD (GAF score 62) (b=−1.137; t437=−2.29; P =.02), although the difference narrowed over time (b=0.519; t258=3.21; P =.002). A similar pattern holds when BPD was compared with MDD (GAF score 65) (b=−3.804; t411=−5.77; P <.001), although with a smaller change in the difference over time (b=−0.430; t264=−2.01; P =.04). Significant covariates were age (b =−0.276; t462 =−6.53; P < .001) and education (b=1.669; t483=8.76; P <.001). We next looked at subgroups with good (GAF score >70), fair (GAF score 61–70), and poor (GAF score <61) functioning. The fractions of both subjects with OPD and subjects with MDD who scored either good or poor uniformly ranged between 20% and 40%. A much higher fraction of the subjects with BPD rated poor (range, 61%–81%; mean, 69%) and a much lower percentage rated good (range, 3%–14%; mean, 9%). A more focused examination of the attainment of good functioning (GAF score >70) by survival analysis showed that at baseline no subjects of the BPD sample had good functioning and that by 10 years only 21% achieved this (Figure 4). This fraction for the BPD sample was much lower than the frequency of good functioning attained in either the OPD sample (48%) or MDD sample (61%) ( ; P <.001).
Figure 4.
Functional remission, defined as a Global Assessment of Functioning score greater than 70 sustained for 2 months. Analyses were conducted using lifetest survival estimates. MDD indicates major depressive disorder; OPD, other personality disorders; and BPD, borderline personality disorder.
The LIFE ratings of GSA scores (Figure 3B) fell uniformly in the range from poor to mild impairment. The GSA scores mirrored the relatively low levels of change found with the GAF, although again all 3 diagnostic cells showed statistically significant improvement (b=0.474; t401=8.43; P<.001). An HLM examination covarying for age, sex, and education showed that the averaged GSA score over time for BPD (mean GSA score 3.42, poor to fair) was initially worse than for OPD, although the difference decreased over time (b=−0.045; t237=−3.14; P=.002) (mean GSA score 3.06, fair), and for MDD (mean GSA score 2.83, fair to mild) (b=0.245; t449=4.89; P <.001). Significant covariates were age (older age predictive of poorer functioning, P<.001) and education (more education predictive of better functioning, P<.001).
The LIFE functioning changes over time are shown in Table 1. The HLM analyses using multiple imputation for missing data are reported in Table 2. In these analyses, overall improvement from baseline to follow-up was observed for all subscales (P<.001). The differences between BPD and OPD at baseline diminished over time, and even though the mean score for BPD was higher (worse), there were no statistically significant main effects for BPD vs OPD. For the satisfaction and recreation subscales, there were time × BPD vs OPD interactions in which the BPD-OPD difference was significant early on but decreased later. For BPD vs MDD comparisons, however, there were statistically significant main effects for all scales except spouse/partner. For the satisfaction scale, there was a time × BPD vs MDD interaction in which the participants with MDD improved more over time than the participants with BPD. As indicated in Table 1, younger age and more education were significant covariates, ie, they were associated with better functioning for all scales except the parent role, where only education was significant.
Table 2.
Results of Hierarchical Linear Modeling Analyses of Longitudinal Interval Follow-up Evaluation Functioning
| Dependent Variable | Main Effect
|
BPD vs OPD or MDD × Time Interaction
|
||||||
|---|---|---|---|---|---|---|---|---|
| β | t | df | P Value | β | t | df | P Value | |
| BPD vs OPD | ||||||||
| Satisfaction | 0.001 | 0.02 | 400 | .98 | −0.064 | −2.45 | 404 | .01 |
| Recreation | 0.041 | 0.98 | 437 | .33 | −0.039 | −2.40 | 325 | .02 |
| Friend role | −0.096 | −1.90 | 409 | .06 | 0.009 | 0.51 | 212 | .61 |
| Spouse role | 0.002 | 0.03 | 245 | .98 | −0.038 | −1.17 | 117 | .25 |
| Parent role | 0.045 | 0.90 | 466 | .37 | −0.003 | −0.22 | 230 | .83 |
| Employment | 0.034 | 0.66 | 292 | .51 | 0.010 | 0.46 | 216 | .65 |
| BPD vs MDD | ||||||||
| Satisfaction | 0.268 | 3.88 | 422 | <.001 | 0.070 | 2.06 | 428 | .04 |
| Recreation | 0.196 | 3.60 | 449 | <.001 | −0.007 | −0.35 | 378 | .73 |
| Friend role | 0.305 | 4.63 | 416 | <.001 | −0.043 | −1.87 | 218 | .06 |
| Spouse role | 0.096 | 0.98 | 228 | .33 | 0.016 | 0.34 | 91 | .73 |
| Parent role | 0.158 | 2.36 | 430 | .02 | −0.033 | −1.48 | 172 | .14 |
| Employment | 0.139 | 2.01 | 276 | .045 | −0.053 | −1.76 | 182 | .08 |
Abbreviations: BPD, borderline personality disorder; MDD, major depressive disorder; OPD, other personality disorders.
Data on full-time employment status and marital status for the 3 diagnostic study groups appear in Table 3. Generalized estimating equation analyses indicate that even though there was significant improvement over time for all 3 groups (t255=3.06; P =.002), the BPD sample was significantly less apt to have full-time employment than were the other 2 samples (BPD vs OPD: t431=2.55; P =.01; BPD vs MDD: t438=2.26; P =.02). Being younger, female, and more educated were associated with greater likelihood of attaining full-time employment. As shown in Table 3, 23% of the BPD sample was married or cohabiting at baseline, and this increased to 41% at 10 years; indeed, in all 3 groups, the percentage of participants who were married or cohabiting increased over time (t325=3.35; P<.001). The BPD sample’s rates of being married or cohabiting were not significantly different from those of the other 2 groups at any period. These analyses corroborated our finding that the mean level of the BPD sample’s spouse/partner role functioning did not significantly differ from either the OPD or the MDD samples. More education, but not age or sex, predicted greater likelihood of being married or cohabiting.
Table 3.
Comparison of Full-Time Employment and Marital Status by Diagnostic Cella
| Diagnostic Cell | Baseline | 1 y | 2 y | 4 y | 6 y | 8 y | 10 y |
|---|---|---|---|---|---|---|---|
| Full-time employment, %b | |||||||
| BPD | 19 | 32 | 33 | 38 | 37 | 34 | 36 |
| OPD | 35 | 45 | 49 | 54 | 48 | 51 | 52 |
| MDD | 21 | 38 | 47 | 50 | 55 | 58 | 50 |
| Married or cohabiting, %c | |||||||
| BPD | 23 | 28 | 26 | 31 | 38 | 39 | 41 |
| OPD | 26 | 28 | 30 | 31 | 36 | 40 | 46 |
| MDD | 23 | 24 | 26 | 30 | 31 | 31 | 42 |
Abbreviations: BPD, borderline personality disorder; MDD, major depressive disorder; OPD, other personality disorders.
Reported frequencies are based on nonmissing data; generalized estimating equation analyses used multiple imputation.
For BPD vs OPD, P = .01 for main effect and P = .73 for interaction with time. For BPD vs MDD, P = .02 for main effect and P = .90 for interaction with time. Significant covariates are age (P < .001), sex (P = .001), education (P < .001), and time (P = .002).
For BPD vs OPD, P = .54 for main effect and P = .37 for interaction with time. For BPD vs MDD, P = .51 for main effect and P = .86 for interaction with time. Significant covariates are education (P = .001) and time (P < .001).
Our hypothesis that the number of BPD criteria present at each assessment would inversely predict subsequent GAF scores was confirmed in a repeated-measures HLM with BPD criteria as a time-varying predictor (t155=−3.10; P =.002); each additional criterion predicted a decrease of 0.47 point on the following year’s GAF. There was an interaction between study year and number of criteria. Notably, the number of BPD criteria in early years predicted subsequent GAF scores less well than in subsequent years. Age and education also significantly predicted GAF scores (P<.001 for both): every 10 years of added age predicted a decrease of 3.22 GAF points, whereas every additional year of education predicted an increase of 1.71 GAF points.
In a parallel HLM analysis with GAF score as the time-varying predictor, GAF scores did not predict number of BPD criteria for the next year (t193=−1.01; P =.31). There was no year × GAF score interaction. Education was a significant covariate (t378=−5.39; P <.001), but age and sex were not. As noted earlier (Figure 1), there was a significant decline over time in number of BPD criteria (t295=−10.06; P <.001).
COMMENT
This report is written at a time when, despite the high prevalence of BPD in psychiatric facilities, attention to BPD remains woefully low relative to that paid to other major psychiatric disorders.21 Indeed the diagnosis is underused22,23 and most mental health care professionals avoid or actively dislike patients with BPD.24 This context helps frame the significance of this study. Its results correlate with those of the only other 10-year prospective study of BPD4,5 to demonstrate that BPD psychopathology improves more than generally expected but that psychosocial functioning often remains impaired.
The remission rates found for BPD, very similar to those found in the MSAD,4,25 exceed what might have been predicted from usual clinical assumptions as well as from prior long-term retrospective studies.26–28 Notably, this pattern of remission, occurring in the absence of sustained or BPD-specific treatments,29–31 is consistent with the theory that if patients with BPD can achieve stable supports and avoid interpersonal stressors they will remit clinically.32,33 The relapse data, again mirroring what was found in the MSAD follow-up,4,34 are equally striking. Only 11% of those who remitted subsequently relapsed. The low relapse rate suggests that during the remission process, the patients changed either psychologically, perhaps having acquired more resiliency or new adaptive skills, or situationally by attaining more supports or less stress.
The rates of BPD remission found here resemble those observed in 10-year follow-up studies that used similar follow-up methods for MDD,35 bipolar disorder,36 and panic disorders37 but far exceed those for social phobia.37 The rates of BPD relapse found here are dramatically lower than for all of these disorders.35–38 These comparisons underscore the clinically significant and distinct BPD pattern in which BPD remitted significantly more slowly than MDD but only minimally more slowly than OPD and relapsed significantly less often than MDD and OPD. Insofar as 80% of our BPD sample had lifetime MDD,39 the dramatically faster rate to remission of our MDD sample (80% by 1 year) compared with BPD (30% by 1 year) underscores how negatively BPD influences the course of MDD. Similarly, the fact that the rate of relapse found in our MDD sample was lower than in other MDD samples presumably reflects our sample’s lack of personality disorder comorbidity. What is evident appears clinically counterintuitive: patients with BPD improve symptomatically more often, more quickly, and more dramatically than expected and, once better, maintain improvements more enduring than for many other major psychiatric disorders.
The relative stability of BPD criteria reported here extends our prior reports after 2 years of follow-up.9,40 The earlier reports from CLPS, like the 10-year data from the MSAD,25 suggested a hybrid model with more stable criteria being traitlike (eg, affective instability, unstable relationships) and with less stable criteria being more symptomlike or statelike (eg, self-injurious behavior, stress/paranoia). In contrast, these 10-year data failed to confirm this division: all 9 criteria had similar rates and levels (about 50%) of decline with a similar rank ordering of prevalence at all times. Our finding is clinically instructive: criteria that we had previously predicted9,40 would remain intransigently stable traits proved just as likely to diminish over time as those that we expected would prove more episodic and transient. This finding also is notable for failing to show that any of BPD’s 3 major phenotypes, ie, affective, behavioral, or interpersonal, show a distinctive pattern of stability. This perhaps affirms the overriding single-factor unity of the BPD construct.41,42 In any event, the apparent between-study differences are not well understood. They can be partially explained by our use of prevalence rates based on our entire sample in contrast to the MSAD’s use of time-to-remission analyses that apply only to the subjects who had the criteria at baseline, but they may also be related to differences in the samples and the assessment instruments. This issue requires more research.
Despite statistically significant overall improvement in functioning, the magnitude of these improvements was far less dramatic and far less clinically significant than the improvements found on measures of psychopathology. The fact that the patients with BPD improved more than those in the comparison groups reflected their having lower baseline functioning. The initially more severe level of the BPD sample’s functional impairment tended to converge toward the levels of both comparison groups over time. As measured by mean GSA scores at 10 years, BPD’s social adjustment (3.1) lagged considerably below that found for MDD (2.7), bipolar I disorder (2.9), and bipolar II disorder (2.8) after 14 to 15 years.43 As measured by GAF score (ie, mid 50s), our BPD sample was less functional than observed after long-term retrospective follow-up of other BPD samples27,28 (ie, the mid to high 60s) but resembles the MSAD sample.5,44 Why the 2 prospective studies evidenced more dysfunction than the retrospective studies is unclear. Although it could relate to severity of BPD in the samples or to less effective intervening therapies, it seems more likely that the use of rigorous—presumably more valid—assessment methods for diagnosis and functioning established a better estimate.
Our results show that the improvements in the BPD sample’s functioning evident during the first 2 years11 continued to progress, albeit more slowly. The BPD sample’s improvement in specific areas usually moved them from the poor to the satisfactory range of function. Moreover, the analyses of individual change indicate that while average levels of functioning change slowly, subgroups of patients with BPD (and OPD) episodically experienced substantial fluctuations at the individual level; change in function was more the norm than was stability. Thus, with respect to psychosocial function, the traditional pessimism about this disorder’s prognosis seems partially justified. Younger age, consistent with 2 prior reports,45,46 and more education consistently predicted better function, whereas sex had no effect.
Improvement on the employment subscale of the GSA merits a special note insofar as lost productivity accounts for most of the indirect public health care costs for mental illnesses.47 The BPD sample improved from mild or fair (mean score, 2.8) to satisfactory or good (mean score, 2.1). Much of this modest improvement took place in the first 2 years, and the BPD sample’s overall level of employment remained consistently and significantly poorer than for either the OPD or MDD sample. After 10 years, only about one-third had full-time employment—a rate approximating that found in the MSAD for full-time work or school.5 Still, our BPD sample’s mean employment score at 10 years (2.1) appeared somewhat better than that found in prospective 14- to 15-year follow-up of patients with MDD (2.5), bipolar I disorder (2.8), or bipolar II disorder (2.6).43 Of note, while more education did not affect the quantity and quality of overall employment for patients with BPD, it was associated with more likelihood to achieve full-time employment. Also of note, our MDD sample’s level of employment at 10 years (mean score, 2.1) fell inexplicably lower than earlier in the study but remained better than the Collaborative Depression Study sample’s score of 2.5—presumably reflecting their MDD sample’s enrollment from inpatient hospital units and extensive comorbidity with personality disorders, unlike our MDD sample.
The relative severity and persistence of BPD’s social dysfunction and its contrasting levels of improvement in psychopathology echo findings reported in our 2-year follow-up report,11 findings from MSAD,5,48 and the conclusion that McGlashan reached in his earlier study.49 The patterns of improved psychopathology and persisting social dysfunction have been noted for other disorders.43,50,51 However, the finding of a course marked by gradually attained, frequent, and persistent remission is distinctive for BPD. Given that the other prospective 10-year follow-up study4 identified a very similar course, there now exists a strong empirically based prognostic portrait of BPD that can inform clinicians, families, and patients. By virtue of its distinctiveness, this course offers strong validation for the DSM-IV BPD diagnosis. This validation joins the hard-earned validation of DSM-IV BPD that has come from descriptive and familiality or heritability research and from disorder-specific therapies.21,52 Because, as reported here, the DSM-IV definition of BPD—like DSM-IV definitions of other major psychiatric disorders—identifies a disorder whose course is disjunctive with social disability, it invites the hope that a revised characterization of BPD might more closely correspond to the disorder’s dysfunction and perhaps with its underlying genotype. While current proposals to redefine BPD for DSM-5 (http://www.dsm5.org and the article by Gunderson53) might fulfill this hope, they should proceed with due recognition that the existing definition already has difficult-to-attain validation and conveys clinically essential information about course.
That psychopathology would predict dysfunction is consistent with the MSAD findings that symptomatic improvement was associated with better function44 and is also consistent with the idea that sustained periods of active illness can interfere with developmental tasks and leave patients with BPD with “scars” that obstruct satisfactory community-based activities.54 After the first few years, however, the level of psychopathology proved to only weakly predict long-term functional improvement, ie, patients with BPD who failed to remit tended to remain chronically impaired. Although the psychopathology initially reflected in the BPD criteria may be a cause of social disability, if its reduction was slow, it then proved to be only weakly associated with the development of satisfactory and productive lives. Surprisingly, improvement in social function was not significantly associated with subsequent reductions in psychopathology.
An implication of this study is that the enthusiasm generated by the successes reported for psychosocial therapies of patients with BPD55–62 needs to be qualified by the recognition that these treatments have rarely demonstrated that the patients achieve better functional capacities. Clearly, future studies of therapeutic outcome need to assess functional gain, but more importantly, future BPD therapies need to address functional impairment, ie, to incorporate social learning and rehabilitation strategies. The need for rehabilitative strategies has already been recognized with other major mental illnesses.63,64 From a public health viewpoint, it is critical that therapies demonstrate their effectiveness in helping patients with BPD attain and maintain work roles.
The methods and design of this study as well as the confirmatory results from the MSAD permit a much higher level of confidence in our findings than from prior studies. Still, the completion of the study invites reminders of its limitations. The effort to attain a representative clinical urban sample precludes generalization of our findings to nonclinical or rural populations. As with all longitudinal studies, the repeated contacts with research staff may have affected the outcomes. Other limitations include our reliance on the participants as informants (when outside informants may have augmented assessment validity)65 and our reliance on a measure of employment that did not include homemaking. Finally, we are aware of the many related issues that we did not examine, issues such as predictors of change or the isolation of subgroups based on good or poor outcomes, comorbidity, or sex.
In summary, the 10-year outcome of patients with BPD in the CLPS demonstrates a distinctive, clinically useful, and diagnostically validating course characterized by remissions more enduring and by functional impairment more severe than many other major psychiatric disorders. This pattern highlights the potential therapeutic rewards of treating patients with BPD, while challenging the next generation of therapies to help them become more effective by improving functional outcomes. It also highlights the imposing public health issue these patients represent and the embarrassingly disproportionate lack of attention the disorder has received.18
Acknowledgments
Funding/Support: This work was supported by grants R01 MH 080221, R01 MH 01654, R01 MH 50837, R01 MH 50838, R01 MH 50839, R01 MH 50840, R01 MH 50850, R01 MH 69904, and R01 MH 73708 from the National Institute of Mental Health.
Footnotes
Financial Disclosure: None reported.
Additional Contributions: The manuscript was reviewed and approved for submission by the Publications Committee of the Collaborative Longitudinal Personality Disorders Study.
References
- 1.Grilo CM, McGlashan TH, Oldham JM. Course and stability of personality disorders. J Pract Psychiatry Behav Health. 1998;1(4):61–75. [Google Scholar]
- 2.Robins E, Guze SB. Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry. 1970;126(7):983–987. doi: 10.1176/ajp.126.7.983. [DOI] [PubMed] [Google Scholar]
- 3.Gunderson JG, Shea MT, Skodol AE, McGlashan TH, Morey LC, Stout RL, Zanarini MC, Grilo CM, Oldham JM, Keller MB. The Collaborative Longitudinal Personality Disorders Study: development, aims, design, and sample characteristics. J Pers Disord. 2000;14(4):300–315. doi: 10.1521/pedi.2000.14.4.300. [DOI] [PubMed] [Google Scholar]
- 4.Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Time to attainment of recovery from borderline personality disorder and stability of recovery: a 10-year prospective follow-up study. Am J Psychiatry. 2010;167(6):663–667. doi: 10.1176/appi.ajp.2009.09081130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. The 10-year course of psychosocial functioning among patients with borderline personality disorder and axis II comparison subjects. Acta Psychiatr Scand. 2010;122(2):103–109. doi: 10.1111/j.1600-0447.2010.01543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grilo CM, Sanislow CA, Gunderson JG, Pagano ME, Yen S, Zanarini MC, Shea MT, Skodol AE, Stout RL, Morey LC, McGlashan TH. Two-year stability and change of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. J Consult Clin Psychol. 2004;72(5):767–775. doi: 10.1037/0022-006X.72.5.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gunderson JG, Morey LC, Stout RL, Skodol AE, Shea MT, McGlashan TH, Zanarini MC, Grilo CM, Sanislow CA, Yen S, Daversa MT, Bender DS. Major depressive disorder and borderline personality disorder revisited: longitudinal interactions. J Clin Psychiatry. 2004;65(8):1049–1056. doi: 10.4088/jcp.v65n0804. [DOI] [PubMed] [Google Scholar]
- 8.Gunderson JG, Daversa MT, Grilo CM, McGlashan TH, Zanarini MC, Shea MT, Skodol AE, Yen S, Sanislow CA, Bender DS, Dyck IR, Morey LC, Stout RL. Predictors of 2-year outcome for patients with borderline personality disorder. Am J Psychiatry. 2006;163(5):822–826. doi: 10.1176/ajp.2006.163.5.822. [DOI] [PubMed] [Google Scholar]
- 9.McGlashan TH, Grilo CM, Sanislow CA, Ralevski E, Morey LC, Gunderson JG, Skodol AE, Shea MT, Zanarini MC, Bender DS, Stout RL, Yen S, Pagano ME. Two-year prevalence and stability of individual DSM-IV criteria for schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders: toward a hybrid model of axis II disorders. Am J Psychiatry. 2005;162(5):883–889. doi: 10.1176/appi.ajp.162.5.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shea MT, Stout RL, Gunderson JG, Morey LC, Grilo CM, McGlashan TH, Skodol AE, Dolan-Sewell RT, Dyck IR, Zanarini MC, Keller MB. Short-term diagnostic stability of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. Am J Psychiatry. 2002;159(12):2036–2041. doi: 10.1176/appi.ajp.159.12.2036. [DOI] [PubMed] [Google Scholar]
- 11.Skodol AE, Pagano ME, Bender DS, Shea MT, Gunderson JG, Yen S, Stout RL, Morey LC, Sanislow CA, Grilo CM, Zanarini MC, McGlashan TH. Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder over two years. Psychol Med. 2005;35(3):443–451. doi: 10.1017/s003329170400354x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zanarini MC, Frankenburg FR, Sickel AE, Yong L. The Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV) Belmont, MA: McLean Hospital; 1996. [Google Scholar]
- 13.Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, Morey LC, Grilo CM, Shea MT, McGlashan TH, Gunderson JG. The Collaborative Longitudinal Personality Disorders Study: reliability of axis I and II diagnoses. J Pers Disord. 2000;14(4):291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]
- 14.Zanarini MC, Shea MT. The Diagnostic Interview for DSM-IV Personality Disorders–Follow-Along Version (DIPD-FA) Belmont, MA: McLean Hospital; 1996. [Google Scholar]
- 15.First MB, Gibbon M, Spitzer RL, William JBW. Structured Clinical Interview for DSM-IV Axis I Disorders–Patient Version (SCID-I/P) New York: Biometrics Research Dept, New York State Psychiatric Institute; 1996. [Google Scholar]
- 16.Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, An-dreasen NC. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44(6):540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 17.Warshaw MG, Keller MB, Stout RL. Reliability and validity of the Longitudinal Interval Follow-up Evaluation for assessing outcome of anxiety disorders. J Psychiatr Res. 1994;28(6):531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- 18.Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 19.Little RJA, Rubin DB. Statistical Analysis With Missing Data. 2. New York, NY: John Wiley & Sons; 2002. [Google Scholar]
- 20.Barnard J, Rubin DB. Small-sample degrees of freedom with multiple imputation. Biometrika. 1999;86(4):948–955. doi: 10.1093/biomet/86.4.948. [DOI] [Google Scholar]
- 21.Gunderson JG. Borderline personality disorder: ontogeny of a diagnosis. Am J Psychiatry. 2009;166(5):530–539. doi: 10.1176/appi.ajp.2009.08121825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zimmerman M, Mattia JI. Differences between clinical and research practices in diagnosing borderline personality disorder. Am J Psychiatry. 1999;156(10):1570–1574. doi: 10.1176/ajp.156.10.1570. [DOI] [PubMed] [Google Scholar]
- 23.Zimmerman M, Galione J. Psychiatrists’ and nonpsychiatrist physicians’ reported use of the DSM-IV criteria for major depressive disorder. J Clin Psychiatry. 2010;71(3):235–238. doi: 10.4088/JCP.08m04940blu. [DOI] [PubMed] [Google Scholar]
- 24.Shanks C, Pfohl B, Blum N, Black DW. Can negative attitudes toward patients with borderline personality disorder be changed? the effect of attending a STEPPES workshop. J Pers Disord. doi: 10.1521/pedi.2011.25.6.806. In press. [DOI] [PubMed] [Google Scholar]
- 25.Zanarini MC, Frankenburg FR, Reich DB, Silk KR, Hudson JI, McSweeney LB. The subsyndromal phenomenology of borderline personality disorder: a 10-year follow-up study. Am J Psychiatry. 2007;164(6):929–935. doi: 10.1176/ajp.2007.164.6.929. [DOI] [PubMed] [Google Scholar]
- 26.McGlashan TH. The Chestnut Lodge follow-up study, III: long-term outcome of borderline personalities. Arch Gen Psychiatry. 1986;43(1):20–30. doi: 10.1001/archpsyc.1986.01800010022003. [DOI] [PubMed] [Google Scholar]
- 27.Plakun EM, Burkhardt PE, Muller JP. 14-year follow-up of borderline and schizotypal personality disorders. Compr Psychiatry. 1985;26(5):448–455. doi: 10.1016/0010-440x(85)90081-1. [DOI] [PubMed] [Google Scholar]
- 28.Stone MH, Hurt SW, Stone DK. The PI 500: long-term follow-up of borderline inpatients meeting DSM-III criteria, I: global outcome. J Pers Disord. 1987;1(4):291–298. doi: 10.1521/pedi.1987.1.4.291. [DOI] [Google Scholar]
- 29.Bender DS, Dolan RT, Skodol AE, Sanislow CA, Dyck IR, McGlashan TH, Shea MT, Zanarini MC, Oldham JM, Gunderson JG. Treatment utilization by patients with personality disorders. Am J Psychiatry. 2001;158(2):295–302. doi: 10.1176/appi.ajp.158.2.295. [DOI] [PubMed] [Google Scholar]
- 30.Bender DS, Skodol AE, Pagano ME, Dyck IR, Grilo CM, Shea MT, Sanislow CA, Zanarini MC, Yen S, McGlashan TH, Gunderson JG. Prospective assessment of treatment use by patients with personality disorders. Psychiatr Serv. 2006;57(2):254–257. doi: 10.1176/appi.ps.57.2.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bender DS, Skodol AE, Dyck IR, Markowitz JC, Shea MT, Yen S, Sanislow CA, Pinto A, Zanarini MC, McGlashan TH, Gunderson JG, Daversa MT, Grilo CM. Ethnicity and mental health treatment utilization by patients with personality disorders. J Consult Clin Psychol. 2007;75(6):992–999. doi: 10.1037/0022-006X.75.6.992. [DOI] [PubMed] [Google Scholar]
- 32.Gunderson JG, Bender D, Sanislow C, Yen S, Rettew JB, Dolan-Sewell R, Dyck I, Morey LC, McGlashan TH, Shea MT, Skodol AE. Plausibility and possible determinants of sudden “remissions” in borderline patients. Psychiatry. 2003;66(2):111–119. doi: 10.1521/psyc.66.2.111.20614. [DOI] [PubMed] [Google Scholar]
- 33.Gunderson JG. Disturbed relationships as a phenotype for borderline personality disorder. Am J Psychiatry. 2007;164(11):1637–1640. doi: 10.1176/appi.ajp.2007.07071125. [DOI] [PubMed] [Google Scholar]
- 34.Zanarini MC, Frankenburg FR, Hennen J, Silk KR. The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. Am J Psychiatry. 2003;160(2):274–283. doi: 10.1176/appi.ajp.160.2.274. [DOI] [PubMed] [Google Scholar]
- 35.Mueller TI, Leon AC, Keller MB, Solomon DA, Endicott J, Coryell W, Warshaw M, Maser JD. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. Am J Psychiatry. 1999;156(7):1000–1006. doi: 10.1176/ajp.156.7.1000. [DOI] [PubMed] [Google Scholar]
- 36.Winokur G, Coryell W, Akiskal HS, Endicott J, Keller M, Mueller T. Manic-depressive (bipolar) disorder: the course in light of a prospective ten-year follow-up of 131 patients. Acta Psychiatr Scand. 1994;89(2):102–110. doi: 10.1111/j.1600-0447.1994.tb01495.x. [DOI] [PubMed] [Google Scholar]
- 37.Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano M, Shea MT, Keller MB. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. Am J Psychiatry. 2005;162(6):1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Keller MB, Lavori PW, Coryell W, Endicott J, Mueller TI. Bipolar I: a five-year prospective follow-up. J Nerv Ment Dis. 1993;181(4):238–245. doi: 10.1097/00005053-199304000-00005. [DOI] [PubMed] [Google Scholar]
- 39.McGlashan TH, Grilo CM, Skodol AE, Gunderson JG, Shea MT, Morey LC, Zanarini MC, Stout RL. The Collaborative Longitudinal Personality Disorders Study: baseline axis I/II and II/II diagnostic co-occurrence. Acta Psychiatr Scand. 2000;102(4):256–264. doi: 10.1034/j.1600-0447.2000.102004256.x. [DOI] [PubMed] [Google Scholar]
- 40.Grilo CM, Sanislow CA, Skodol AE, Gunderson JG, Stout RL, Bender DS, Yen S, Shea MT, Morey LC, Zanarini MC, McGlashan TH. Longitudinal diagnostic efficiency of DSM-IV criteria for borderline personality disorder: a 2-year prospective study. Can J Psychiatry. 2007;52(6):357–362. doi: 10.1177/070674370705200604. [DOI] [PubMed] [Google Scholar]
- 41.Clifton A, Pilkonis PA. Evidence for a single latent class of Diagnostic and Statistical Manual of Mental Disorders borderline personality pathology. Compr Psychiatry. 2007;48(1):70–78. doi: 10.1016/j.comppsych.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 42.Fossati A, Maffei C, Bagnato M, Donati D, Namia C, Novella L. Latent structure analysis of DSM-IV borderline personality disorder criteria. Compr Psychiatry. 1999;40(1):72–79. doi: 10.1016/s0010-440x(99)90080-9. [DOI] [PubMed] [Google Scholar]
- 43.Judd LL, Schettler PJ, Solomon DA, Maser JD, Coryell W, Endicott J, Akiskal HS. Psychosocial disability and work role function compared across the long-term course of bipolar I, bipolar II and unipolar major depressive disorders. J Affect Disord. 2008;108(1–2):49–58. doi: 10.1016/j.jad.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 44.Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. The McLean Study of Adult Development (MSAD): overview and implications of the first six years of prospective follow-up. J Pers Disord. 2005;19(5):505–523. doi: 10.1521/pedi.2005.19.5.505. [DOI] [PubMed] [Google Scholar]
- 45.Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Prediction of the 10-year course of borderline personality disorder. Am J Psychiatry. 2006;163 (5):827–832. doi: 10.1176/ajp.2006.163.5.827. [DOI] [PubMed] [Google Scholar]
- 46.Tracie Shea M, Edelen MO, Pinto A, Yen S, Gunderson JG, Skodol AE, Markowitz JC, Sanislow CA, Grilo CM, Ansell E, Daversa MT, Zanarini MC, McGlashan TH, Morey LC. Improvement in borderline personality disorder in relationship to age. Acta Psychiatr Scand. 2009;119(2):143–148. doi: 10.1111/j.1600-0447.2008.01274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marcotte DE, Wilcox-Gök V. Estimating the employment and earnings costs of mental illness: recent developments in the United States. Soc Sci Med. 2001;53(1):21–27. doi: 10.1016/s0277-9536(00)00312-9. [DOI] [PubMed] [Google Scholar]
- 48.Zanarini MC, Jacoby RJ, Frankenburg FR, Reich DB, Fitzmaurice G. The 10-year course of social security disability income reported by patients with borderline personality disorder and axis II comparison subjects. J Pers Disord. 2009;23(4):346–356. doi: 10.1521/pedi.2009.23.4.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McGlashan TH. Implications of outcome research for the treatment of borderline personality disorder. In: Paris J, editor. BPD: Etiology and Treatment. Washington, DC: American Psychiatric Press; 1993. pp. 235–259. [Google Scholar]
- 50.Coryell W, Scheftner W, Keller M, Endicott J, Maser J, Klerman GL. The enduring psychosocial consequences of mania and depression. Am J Psychiatry. 1993;150(5):720–727. doi: 10.1176/ajp.150.5.720. [DOI] [PubMed] [Google Scholar]
- 51.Stout RL, Dolan R, Dyck I, Eisen J, Keller MB. Course of social functioning after remission from panic disorder. Compr Psychiatry. 2001;42(6):441–447. doi: 10.1053/comp.2001.27894. [DOI] [PubMed] [Google Scholar]
- 52.New AS, Triebwasser J, Charney DS. The case for shifting borderline personality disorder to Axis I. Biol Psychiatry. 2008;64(8):653–659. doi: 10.1016/j.biopsych.2008.04.020. [DOI] [PubMed] [Google Scholar]
- 53.Gunderson JG. Revising the borderline diagnosis for DSM-V: an alternative proposal. J Pers Disord. 2010;24(6):694–708. doi: 10.1521/pedi.2010.24.6.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Prisciandaro JJ, Roberts JE. A taxometric investigation of unipolar depression in the National Comorbidity Survey. J Abnorm Psychol. 2005;114(4):718–728. doi: 10.1037/0021-843X.114.4.718. [DOI] [PubMed] [Google Scholar]
- 55.McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L, Streiner DL. A randomized trial of dialectical behavior therapy vs general psychiatric management for borderline personality disorder. Am J Psychiatry. 2009;166(12):1365–1374. doi: 10.1176/appi.ajp.2009.09010039. [DOI] [PubMed] [Google Scholar]
- 56.Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1991;48(12):1060–1064. doi: 10.1001/archpsyc.1991.01810360024003. [DOI] [PubMed] [Google Scholar]
- 57.Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, Korslund KE, Tutek DA, Reynolds SK, Lindenboim N. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry. 2006;63(7):757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- 58.Giesen-Bloo J, van Dyck R, Spinhoven P, van Tilburg W, Dirksen C, van Asselt T, Kremers I, Nadort M, Arntz A. Outpatient psychotherapy for borderline personality disorder: randomized trial of schema-focused therapy vs transference-focused psychotherapy. Arch Gen Psychiatry. 2006;63(6):649–658. doi: 10.1001/archpsyc.63.6.649. [DOI] [PubMed] [Google Scholar]
- 59.Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: a multiwave study. Am J Psychiatry. 2007;164(6):922–928. doi: 10.1176/ajp.2007.164.6.922. [DOI] [PubMed] [Google Scholar]
- 60.Bateman A, Fonagy P. Effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. Am J Psychiatry. 1999;156(10):1563–1569. doi: 10.1176/ajp.156.10.1563. [DOI] [PubMed] [Google Scholar]
- 61.Davidson K, Norrie J, Tyrer P, Gumley A, Tata P, Murray H, Palmer S. The effectiveness of cognitive behavior therapy for borderline personality disorder: results from the Borderline Personality Disorder Study of Cognitive Therapy (BOSCOT) trial. J Pers Disord. 2006;20(5):450–465. doi: 10.1521/pedi.2006.20.5.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Blum N, St John D, Pfohl B, Stuart S, McCormick B, Allen J, Arndt S, Black DW. Systems Training for Emotional Predictability and Problem Solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. Am J Psychiatry. 2008;165(4):468–478. doi: 10.1176/appi.ajp.2007.07071079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kopelowicz A, Liberman RP. Integrating treatment with rehabilitation for persons with major mental illness. Psychiatr Serv. 2003;54(11):1491–1498. doi: 10.1176/appi.ps.54.11.1491. [DOI] [PubMed] [Google Scholar]
- 64.Drake RE, Bond GR. The future of supported employment for people with severe mental illness. Psychiatr Rehabil J. 2008;31(4):367–376. doi: 10.2975/31.4.2008.367.376. [DOI] [PubMed] [Google Scholar]
- 65.Zimmerman M, Pfohl B, Stangl D, Corenthal C. Assessment of DSM-III personality disorders: the importance of interviewing an informant. J Clin Psychiatry. 1986;47(5):261–263. [PubMed] [Google Scholar]