Abstract
Background
Late presentation of breast carcinoma is common in resource-limited countries with attendant poor outcome.
Objective
To describe the pattern of clinical presentation and challenges of treating patients presenting with metastatic breast carcinoma in a Nigerian hospital.
Method
Clinical records of all patients who presented with metastatic breast carcinoma between January 1991 and December 2005 at the Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Nigeria were reviewed.
Results
More than half of all histologically confirmed breast cancer patients seen within the study period presented with metastatic disease. Their ages ranged between 20–81years with a mean age of 45.9 years. Only 3% (6 of 202) were males. Two-thirds had more than one secondary site on initial evaluation and the commonest sites were liver (63%), lung parenchyma (51%), pleura (26%) and contralateral breast in 25%. On immunohistochemistry, basal like tumours were found in 46.1%. Mastectomy was done in 37 patients with fungating breast masses while only one third of those referred to a nearby center for radiotherapy had it done. One year survival rate was 27%.
Conclusion
Metastatic disease is common in Nigeria and treatment is limited due to resource limitations. Improved awareness of the disease is advocated to reduce late presentation.
Keywords: breast cancer, metastasis, developing country
Introduction
Metastatic breast carcinoma is associated with low survival in most patients across the world1,2. In such patients, the aim of treatment therefore is usually palliative with specific objectives of improving quality of life, ensuring symptom control and prolonging survival3. To achieve and improve upon these objectives, various modalities and options of treatment have evolved over the past few decades. In particular, chemotherapeutic options and combinations have continued to change with introduction of newer drugs for first, second and subsequent lines of chemotherapy in metastatic disease4,5. Improved knowledge of the biology of the disease has also led to the introduction of biological agents targeted at specific growth modulators6. Clinical trials with some of these newer drugs across Europe and North America have shown improvement in both the disease free and overall survival among selected patients while many others have not really shown any benefit4,7,8. The cost of many of these new agents are however prohibitive with limited use in resource-constrained economies.
In Nigeria, as indeed in many developing countries, a combination of poor health education, poverty and a high patronage of non-orthodox healing practices among the populace contribute to late presentation of breast cancer in many hospitals with attendant high number of metastatic disease and poor disease survival9. This is worsened by the commonly encountered non-adherence to treatment schedule among the patients. The burden of caring for these large numbers of patients in a low resource country is enormous.
We hypothesize that a large number of metastatic breast cancer will present to Nigerian tertiary hospitals and many challenges will attend their management. This study therefore reviews the presentation, management and outcome of the patients aiming to highlight the magnitude of metastatic breast cancer and the challenges encountered in management of the patients in a tertiary hospital in Nigeria.
Methods
The clinical records of all patients who were treated for breast cancer at the Ife Hospital Unit of the Obafemi Awolowo University Teaching Hospitals Complex, (OAUTHC), Ile-Ife, South- West Nigeria over a fifteen year period of January 1991 to December 2005 were reviewed. All patients with histopathologically confirmed breast cancer had initial clinical evaluation for metastasis. Plain Chest radiograph, and abdomino-pelvic ultrasound were routinely done in all patients at presentation. Due to resource limitations, only those presenting with complaints suggestive of distant spread had further investigations such as skeletal survey and cranial Computerized Axial Tomographic (CT) scan performed. Patients with metastatic disease detected at initial presentation were further studied. Data regarding mode of presentation, investigation findings, treatment modalities and adherence to medications as well as treatment outcome were extracted and further analyzed.
Results
More than 500 patients presented with breast cancer within the period of study but only 385 of them who had histopathological confirmation were further studied. Eleven (2.9%) of them were males. More than half of these patients (202 of 385; 52.5%) had metastatic disease on initial evaluation including 6 of the 11 (54.5%) male patients. Further study of the patients with metastatic disease showed an age range between 20–81years with a mean age of 45.9 years (SD=5.6). Five patients (2.5%) were in the third decade of life, and only 6 (3%) were more than 70 years in age as shown in Table 1.
Table 1.
Socio-demographic characteristics of the patients showing age and gender distribution
| Age Range(Yr) | n | Male | Female |
| 21–30 | 5 | - | 5 |
| 31–40 | 46 | - | 46 |
| 41–50 | 64 | - | 64 |
| 51–60 | 37 | 1 | 36 |
| 61–70 | 41 | 3 | 38 |
| >70 | 8 | 2 | 6 |
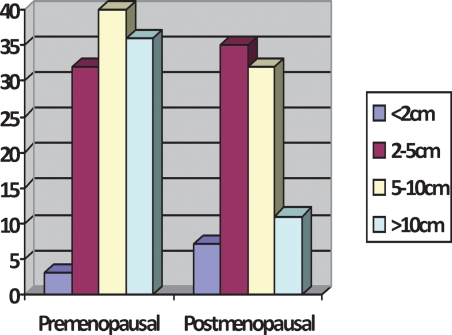
Majority (73.8%) of these patients had up to secondary or tertiary formal education. This however did not influence the duration of symptoms before presentation as only 70 of the 202 patients (34.7%) presented within 3 months of noticing a lump within the breast. Of the 196 women, 111 (56.7%) were premenopausal while the remaining 85 (43.4%) were postmenopausal as indicated in Figure 1. The primary tumour involved the left breast in 91 (45.7%) patients, the right breast in 86 (42.7%) patients, while 25 (12.3%) female patients had metastasis to the contralateral breast at initial presentation. The size of the primary tumour ranged from 1.5 to 28cm with a median of 8.5cm.
Figure 1.
Relating menopausal status of patients to their primary tumour size at presentation
Two-thirds of the patients had more than one site of metastasis on initial evaluation. The common sites were liver in 126 (62.6%) and lung parenchyma in 102 (50.7%) while pleural effusion occurred in 52 (25.9%) and contralateral breast and/or axillary secondaries were recorded in 50 (24.9%) patients as shown in Table 2. Sixty-five patients (32.2%) had palpably enlarged supraclavicular lymphadenopathy. Immunohistochemical studies were introduced in our pathology laboratory in the last few years of the period of this study and was performed on the specimen from 64 of these patient. Of these, 35.1% were positive for Oestrogen Receptor (ER), 26.7% for Progesterone Receptor (PR) and 48.3% for Human Epidermal Growth Factor (Her2neu). In combination, 39.1% were Luminal A, 10.1% were Luminal B while the Triple Negative (Basal-Like) tumours occurred in 46.1% as shown in Table 3.
Table 2.
Sites of breast cancer metastasis
| Sites of metastases | N (%) |
| Liver | 126 (62.6) |
| Lung Parenchyma | 102 (50.7) |
| Pleura | 52 (25.9) |
| Contralateral breast and/or axilla | 50 (24.9) |
| Long bone | 34 (16.9) |
| Brain | 22 (11.0) |
| Peritoneal | 16 (8.0) |
| Spine | 19 (9.4) |
| Others | 14 (7.0) |
Table 3.
Immunohistochemical characteristics of tumours of patients with metastatic disease (n = 64)
| Receptor Status | Percentage |
| ER+ | 35.1 |
| PR+ | 26.7 |
| Her2neu+ | 48.3 |
| Luminal A(ER+,PR+,Her2neu−) | 39.1 |
| Luminal B (ER/PR+Her2neu+) | 10.1 |
| Basal-like (Triple -ve) | 46.1 |
| ER-ve,PR-ve, Her2neu+ | 5.1 |
Anthracycline based chemotherapy combination was most commonly employed in the treatment of the patients and was used in 38% with the combination of Cyclophosphamide, Methotrexate and 5 Fluorouracil (CMF) used in 32%. Hormonal therapy with Tamoxifen was administered along with the chemotherapy in 46% of the patients but the routine use of Tamoxifen reduced drastically with the availability of immunohistochemistry in our laboratory. Taxane based combinations were recently introduced and used in 5 (2.5%) patients. Biological therapy with Transtuzumab was used in only 3 patients. In the course of chemotherapy, two-thirds of the patients defaulted from treatment schedule at one point in time or another. Eighteen (8.9%) patients however had no chemotherapy at all either due to poor clinical conditions at presentation or financial difficulties.
Seventy-eight patients had surgeries done including mastectomy in 69 patients, fixation of pathological bone fractures in 6 patients, metastectomy of brain secondaries in 3 patients. 73 patients were referred to a nearby center for radiotherapy but only 20 (27.4%) had it done, 32 (43.8%) could not due to a long waiting list, financial constraint and other difficulties encountered at the center while 21 (28.8%) patients were lost to follow up immediately after referral.
At one year of follow up, 54 (27.1%) of the patients were alive, 115 (57.1%) were dead and 32 (15.9%) were lost to follow-up. The 54 patients were followed up and at two years after initial presentation only 8(%) were still alive, 28 were confirmed dead and the remaining 18 were lost to follow up.
Discussion
Metastatic breast cancer is associated with a severe burden both to the patient and to the healthcare delivery system. This has led to increased efforts on routine screening towards early detection of the disease over the past two decades resulting in marked reduction in late presentation and the incidence of metastatic disease in many centers in Western communities10. In some countries, distant metastasis are now found in less than 10% of patients at initial presentation4. However in some developing countries such as Nigeria, routine screening for breast cancer is not yet commonly practiced and a large number of patients still present late. This is compounded by limitation of the resources necessary for the care of these patients.
There are few previous studies focusing on metastatic breast cancer in Africa. However in previous reports of breast cancer patients in Ibadan, Nigeria, Adebamowo et al had shown a rising hospital incidence of breast cancer in Nigeria with about two-thirds of the patients presenting with locally advanced or metastatic disease9. A previous study in South Africa has also shown that locally advanced and metastatic disease occurred in up to 77% of blacks compared to 30% in non-black patients11. This is in contrast to reports from South America where, about a decade ago, incidence of metastatic disease was shown to have reduced to between 10–16%12.
Different reasons may be adduced for the late presentation. Of major concern in Africa are socioeconomic factors which have been noted to influence the choice and outcome of treatment among women with late stages of breast cancer13,14. In our society, medical decision-making among these relatively young women is further compounded by the cultural influence of the husband and family members on their choice, acceptance and adherence to treatment options15,16.
The menace of breast cancer afflicting young women has been consistently reported among Africans including African Americans17–19. The mean age of 45.9 years of women with stage IV disease in this study further confirms the suspicion that a biologically aggressive form of breast cancer is predominant among African patients. Indeed, immunohistochemical studies carried out on 64 of these patients in the last two years of the period of this study found the Basal-like (Triple Negative) tumours which is associated with poor prognosis occurring in 46% of our patients compared to 12% reported among European patients20.
During the period of this study, immunohistochemistry findings similar to ours have were reported from other centers in Nigeria. Only 24% of patients were ER positive in a study conducted in Eastern Nigeria while 25% of those tested in a study from Northern Nigeria were ER positive21,22.In a similar report from East Africa, Nalwoga et al reported 34% Basal like tumours among breast cancer specimen23. The occurrence of these aggressive tumours in young women who also present after a rather long duration of symptoms (mean= 5.8months) may contribute significantly to high incidence of metastatic disease in our center and the generally poor outcome.
A major constraint in the management of the patients was the limitation of resources. Our patients bear the burden of paying for cancer treatment in a low resource country. Having a population of over 150million and a Gross Domestic Product of about 2000US Dollar per capita annually, Nigeria ranks among the poorest nations in the world24,25. With a Health Insurance Scheme that is still in its formative stage, paying for chemotherapy is an uphill task for the majority of patients. In an earlier study in our center, we found that up to 45% of the patients default from chemotherapy schedule due to financial difficulty26. This explains why second and subsequent lines of chemotherapy as well as new biological agents are infrequently used in our patients within the period of this study.
Long term survival in metastatic breast cancer has been reported among a small subset of patients including young patients with good performance status, those with isolated single lesions that are amenable to surgery or radiation and those with limited metastatic disease27–29. In our study, two thirds of the patients presented with more than one site of metastasis. Solid organ metastasis was also common with hepatic metastasis in 62%. It is not surprising therefore that the overall survival in this study was low with only about a quarter of the patients confirmed to be alive at one year. This is however confounded by the inadequate treatment received by a number of patients for various reasons. Radiation therapy is also limited across Nigeria. Throughout the period of this study, the facility was available in only three centers in the country with long patient waiting list and undue pressure on the centers. A number of patients referred for radiation end up not receiving the treatment while many others are lost to follow-up from the time of referral.
Our hospital serves both the urban and rural settings of South-Western Nigeria. The community-dwelling, largely agrarian indigenous population usually display a poor knowledge on health related matters. This may account for the high incidence of metastatic disease observed in this study. Being retrospective in nature, the study is also likely to have been affected by the poor record keeping in our setting as a number of patients were excluded due to incomplete records. Outcome analysis in our patients would have enabled us to identify specific factors that may influence the survival pattern observed. This was however limited due to the very high rate of loss to follow-up among the patients on treatment.
Conclusion
Present community based efforts in our locality by the Oncology Group in our hospital in collaboration with Non-Governmental Organizations is targeted at disseminating information on breast cancer and offering free breast cancer screening and subsidized cancer treatment. There is on-going campaign to sensitize the different tiers of government across Nigeria on the need to subsidize cancer treatment especially for the indigent patients. It is believed that these efforts will reduce the present high incidence of metastatic disease in the near future.
References
- 1.Gennari A, Conte P, Rosso R, Orlandini C, Bruzzi P. Survival of metastatic breast carcinoma patients over a 20-year period. Cancer. 2005;104:1742–1750. doi: 10.1002/cncr.21359. [DOI] [PubMed] [Google Scholar]
- 2.Falkson G, Holcroft C, Gelman R, Tormey D C, Wolter JM, Cummings FJ. Ten-year follow-up study of premenopausal women with metastatic breast cancer; an Eastern Cooperative Oncology Group study. J Clin Oncol. 1995;13:1453–1458. doi: 10.1200/JCO.1995.13.6.1453. [DOI] [PubMed] [Google Scholar]
- 3.Chung CT, Carlson RW. Goals and objectives in the management of metastatic breast cancer. The Oncologist. 2003;8:514–520. doi: 10.1634/theoncologist.8-6-514. [DOI] [PubMed] [Google Scholar]
- 4.Cardoso F, Di Leo A, Lohrisch C, Bernard C, Ferreira F, Piccart MJ. Second and subsequent lines of chemotherapy for metastatic breast cancer: what did we learn in the last two decades? Annals of Oncology. 2002;13:197–207. doi: 10.1093/annonc/mdf101. [DOI] [PubMed] [Google Scholar]
- 5.Bernard-Marty C, Cardoso F, Piccaart MJ. Facts and controversies in systemic treatment of metastatic breast cancer. The Oncologist. 2004;9:617–632. doi: 10.1634/theoncologist.9-6-617. [DOI] [PubMed] [Google Scholar]
- 6.Mouridsen HT, Rose C, Brodie AH, Smith IE. Challenges in the endocrine management of breast cancer. Breast. 2003 Dec;12(Suppl 2):S2–S19. doi: 10.1016/s0960-9776(03)80158-3. [DOI] [PubMed] [Google Scholar]
- 7.O'Shaughnessy J, Miles D, Vukelja S, Moiseyenko V, Ayoub JP, Cervantes G, et al. Superior survival with capecitabine plus docetaxel combination therapy in anthracycline-pretreated patients with advanced breast cancer; phase III trial results. J Clin Oncol. 2002;20:2812–2823. doi: 10.1200/JCO.2002.09.002. [DOI] [PubMed] [Google Scholar]
- 8.Mariani G, Petrelli F, Zambetti M, Moliterni A, Fasolo A, Marchiano A, et al. Capecitabine/Cyclophosphamide/Methotrexate for patients with metastatic breast cancer: a dose-finding, feasibility, and efficacy study. Clin Breast Cancer. 2006;7:321–325. doi: 10.3816/CBC.2006.n.044. [DOI] [PubMed] [Google Scholar]
- 9.Adebamowo CA, Ajayi OO. Breast cancer in Nigeria. West Afr J Med. 2000;19:179–191. [PubMed] [Google Scholar]
- 10.Blanks RG, Moss SM, McGahan CE, Quinn MJ, Babb PJ. Effect of NHS breast screening programme on mortality from breast cancer in England and Wales, 1990–8: comparison of observed with predicted mortality. BMJ. 2000;321:665–669. doi: 10.1136/bmj.321.7262.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vorobiof DA, Sitas F, Vorobiof G. Breast Cancer Incidence in South Africa. J Clin Oncol. 2001;19(18):125s–127s. [PubMed] [Google Scholar]
- 12.Schwartsmann Gilberto. Breast Cancer in South America: Challenges to Improve Early Detection and Medical Management of a Public Health Problem. J Clin Oncol. 19:118s–124s. [PubMed] [Google Scholar]
- 13.Bradley CJ, Given CW, Roberts C. Race, socioeconomic status, and breast cancer treatment and survival. J Natl Cancer Inst. 2002;94:490–496. doi: 10.1093/jnci/94.7.490. [DOI] [PubMed] [Google Scholar]
- 14.Adisa AO, Lawal OO, Adesunkanmi ARK. Paradox of wellness and nonadherence among Nigerian women on breast cancer chemotherapy. Journal of Cancer Research and Therapeutics. 2008 Jul-Sep;4(3):107–110. doi: 10.4103/0973-1482.42640. [DOI] [PubMed] [Google Scholar]
- 15.Nour A. Breast-conserving therapy in low-literacy patients in a developing country. Breast Journal. 2003;9(2):71–73. doi: 10.1046/j.1524-4741.2003.09202.x. [DOI] [PubMed] [Google Scholar]
- 16.Ajekigbe AT. Fear of Mastectomy: the most common factor responsible for late presentation of carcinoma of the breast in Nigeria. Clinical Oncology (Royal College of Radiologists.) 1991;3:78–80. doi: 10.1016/s0936-6555(05)81167-7. [DOI] [PubMed] [Google Scholar]
- 17.Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, et al. Race, breast cancer subtypes and survival in Carolina Breast Cancer Study. JAMA. 2006;295:2492–2502. doi: 10.1001/jama.295.21.2492. [DOI] [PubMed] [Google Scholar]
- 18.Digman JJ. Differences in breast cancer prognosis among African-American and Caucasian Women. CA Cancer J Clin. 2000;50:50–64. doi: 10.3322/canjclin.50.1.50. [DOI] [PubMed] [Google Scholar]
- 19.Okobia MN, Bunker CH. Epidemiological risk factors for breast cancer—a review. Niger J Clin Pract. 2005;8(9):35–42. [PubMed] [Google Scholar]
- 20.Kaplan HG, Malmgren JA. Impact of triple negative phenotype on breast cancer prognosis. The Breast Journal. 2008;14:456–463. doi: 10.1111/j.1524-4741.2008.00622.x. [DOI] [PubMed] [Google Scholar]
- 21.Ikpatt OF, Ndoma-Egba R. Oestrogen and progesterone receptors in Nigerian breast cancer: relationship to tumour histopathology and survival of patients. Cent Afr J Med. 2003;49(11–12):122–126. [PubMed] [Google Scholar]
- 22.Gukas ID, Jennings BA, Mandong BM, Igun GO, Girling AC, Manasseh AN, et al. Clinicopathological features and molecular markers of breast cancer in Jos, Nigeria. West Afr J Med. 2005;24(3):209–213. doi: 10.4314/wajm.v24i3.28220. [DOI] [PubMed] [Google Scholar]
- 23.Nalwoga H, Arnes JB, Wabinga H, Akslen LA. Frequency of the basal-like phenotype in African breast cancer. APMIS. 2007;115:1391–1399. doi: 10.1111/j.1600-0463.2007.00862.x. [DOI] [PubMed] [Google Scholar]
- 24.World Economic Outlook Database-October 2009. International Monetary Fund; [October 1, 2009]. [Google Scholar]
- 25.World Development Indicators database. World Bank; Data Released on 15 September 2009. [Google Scholar]
- 26.Adisa AO, Lawal OO, Adesunkanmi ARK. Evaluation of patients' adherence to chemotherapy for breast cancer. Afr J Health Sci. 2008;15:22–27. (2008) [Google Scholar]
- 27.Juan O, Lluch A, de Paz L, Prosper F, Azagra P, Marugan I, et al. Prognostic factors in patients with isolated recurrences of breast cancer (stage IV-NED) Breast Cancer Res Treat. 1999;53:105–112. doi: 10.1023/a:1006090319083. [DOI] [PubMed] [Google Scholar]
- 28.Hortobágyi GN. Can we cure limited metastatic breast cancer? J Clin Oncol. 2002;20:620–623. doi: 10.1200/JCO.2002.20.3.620. [DOI] [PubMed] [Google Scholar]
- 29.Diaz-Canton EA, Valero V, Rahman Z, Rodriguez-Monge E, Frye D, Smith T, et al. Clinical course of breast cancer patients with metastases confined to the lungs treated with chemotherapy. The University of Texa M.D. Anderson Cancer Center experience and review of the literature. Ann Oncol. 1998;9:413–418. doi: 10.1023/a:1008205522875. [DOI] [PubMed] [Google Scholar]