Summary
Abdominal pregnancy is a rare form of ectopic pregnancy with very high morbidity and mortality for both the mother and the foetus. Diagnosis and management can pose some difficulties especially in low-resource centres. High index of suspicion is vital in making prompt diagnosis in such situations. A case of abdominal pregnancy that resulted in a live healthy newborn at a Regional Hospital in Ghana is presented.
Keywords: abdominal pregnancy, live baby, ectopic, placenta
Introduction
Ectopic pregnancy represents about 1–2% of all pregnancies with 95% occurring in the fallopian tube. Abdominal pregnancies represent just about 1% of ectopic pregnancies.1 The incidence of abdominal pregnancy differs in various publications and ranges between 1: 10000 pregnancies and 1:30,000 pregnancies.1,2 It was reported for the first time in 1708 as an autopsy finding and numerous cases have been reported worldwide ever since. In most of these cases, the diagnosis is made on the basis of the ensuing complications such as hemorrhage and abdominal pain. Maternal mortality and morbidity are also very high especially if the condition is not diagnosed and managed appropriately. These pregnancies generally do not get to 37 weeks (term gestation) and usually the end result is the extraction of a dead fetus. Another challenge for babies from abdominal pregnancy is the very high incidence of congenital malformations.
Abdominal pregnancy at term with a healthy viable fetus is therefore an extremely rare condition and very few of such cases have been published during the last ten years. We present a case of abdominal pregnancy that resulted in a term live baby without malformations.
Case Report
A 31- year- old woman, Gravida 3 Para 1, was referred from a District Hospital on 17th June 2008 at 8:00am. Her principal complaint on arrival was severe abdominal pain. She had irregular menstrual cycles prior to her pregnancy and was not sure of her last date of menstruation. The patient suffered from severe abdominal pain and vaginal bleeding which kept her out of work during the first trimester but the second trimester was incident free. She was, however, again kept out of work during the third trimester with abdominal pain. Her antenatal card indicated nine visits and a gestational age of 38 weeks at the time of referral.
On examination, she looked generally stable. She was not pale; vital signs were within normal parameters. Cardiovascular and respiratory systems did not reveal any abnormalities. The abdominal examination revealed symphysio-fundal height of 33cm, transverse lie, foetal heart rate of 136 beats per minute and no uterine contractions.
Vaginal examination revealed posterior located cervix measuring 2cm long without dilatation. There was no vaginal bleeding. She had five ultrasound scan examination with the last two within seven days of presentation indicating intrauterine gestation with transverse lie. The rest of her investigations were normal. The haemoglobin level was 10.9g/dl and blood group was O Rhesus positive. She was booked for emergency caesarean section on account of transverse lie at term.
At laparotomy the following findings were made: Abdominal pregnancy with a live female baby weighing 2.3 kilograms and meconium stained liquor. The placenta was extensively adherent to segments of large bowel, omentum and left cornual region of the uterus (Figure1).
Figure1.
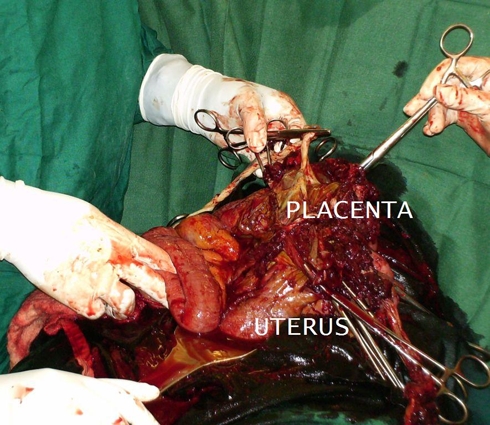
Normal sized uterus and placenta implanted on segment of bowel
The uterus, right tube and both ovaries were normal but the left tube was not identified. Other abdominal organs were normal.
There was significant bleeding from some detached portions of the placenta, which prompted removal of the detached placenta tissue to facilitate haemostasis. The rest of the placenta was left in situ. Haemostasis was secured. Total estimated trans-operative bleeding was one litre.
A unit of compatible blood was transfused intraoperatively. The patient progressed well and was discharged on the fifth postoperative day. She was followed up weekly for four weeks. Abdominal ultrasound after six weeks showed normal size uterus and ovaries and the portion of placenta that was left in situ was not identified. Beta human chorionic gonadotropin (BhCG) was negative at the same period. All investigations by the neonatologist and the general paediatrician did not show any abnormality on the baby. The patient was finally discharged home.
Discussions
Advanced abdominal pregnancy is extremely rare. In a review at the Komfo Anokye Teaching Hospital, Opare-Addo et al reported an incidence of 1:1320 deliveries3 whilst Amirtha et al cited 1:25000 deliveries.4 Most of the cases of abdominal pregnancies are secondary from aborted or ruptured tubal pregnancy. 4 In this case it was obvious that the abdominal implantation was secondary to undiagnosed ruptured left tubal ectopic pregnancy. Clinical diagnosis can be very difficult and ultrasound is very helpful during the early stages of gestation but can also be disappointing in the later stages.
Other radiological studies such as MRI and CT scan are helpful in the later stages.5 Teng et al reported an interesting case in which MRI played a decisive role in the diagnosis6, unfortunately these advanced imaging technologies are not available in most parts of the third world. Our patient had five ultrasound scan examinations and none of these suggested the possibility of abdominal pregnancy. In poorly resourced centres, high index of suspicion is key for prompt diagnosis and timely intervention to prevent life-threatening complications.
In our opinion, bleeding from placental implantation site is the most life-threatening complication during laparotomy. The decision to remove the placenta or not can be a determining factor for the survival or otherwise of the woman and this decision is subject to the surgeon's expertise and the particular case in question. It is generally recommended to leave the placenta in situ and make a follow up with human chorionic gonadotropin levels.7 In this case there was significant bleeding from some detached portions of the placenta that prompted removal of these portions to secure haemostasis. The patient was transfused with one unit of blood during the operation and that was enough. For the newborn, it is very important to rule out congenital malformations. There are reports of foetal malformations as high as 40% associated with abdominal pregnancies and only 50% of these babies survive up to one week post delivery.8,9
In his extensive review, Stevens found some varying degrees of deformations and malformations in 21.4% of these infants. In this case that has been presented; no malformation has been found on the child after ten months.
Conclusions
Abdominal pregnancy with resultant healthy newborn is very rare. Diagnosis of the condition can be difficult especially if the pregnancy is advanced. High level of suspicion, careful clinical and ultrasound examinations are the routine means of diagnosis though C T scan and MRI can be useful. Bleeding is the single most important life-threatening complication for the mother whilst fetal malformation is one of the numerous challenges that can confront the newborn.
Acknowledgement
We wish to acknowledge the kind comments and guidance of Dr R.M.K Adanu on this case report.
References
- 1.Nwobodo EI. Abdominal pregnancy. A case report. Ann Afr Med. 2004;3(4):195–196. doi: 10.4103/1596-3519.55653. [DOI] [PubMed] [Google Scholar]
- 2.Badria L, Amarin Z, Jaradat A, Zahawi H, Gharaibeh A. Full-term viable abdominal pregnancy. A case report and review. Arch Gynaecol Obstet. 2003;268(4):340–342. doi: 10.1007/s00404-002-0363-y. [DOI] [PubMed] [Google Scholar]
- 3.Opare-Addo HS, Daganus S. Advanced abdominal pregnancy: a study of 13 consecutive cases seen in 1993 and 1994 at Komfo Anokye Teaching Hospital, Kumasi, Ghana. Afr J Reproductive Health. 2000;4(1):28–39. [PubMed] [Google Scholar]
- 4.Amritha B, Sumangali T, Priya B, Deepak S, Rai S. A rare case of term viable secondary abdominal pregnancy following rupture of a rudimentary horn. A case report. J Med case reports. 2009;3:38. doi: 10.1186/1752-1947-3-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karat LS. Viable Abdominal Pregnancy. J Obstet Gynecol India. 2007;57(2):169–170. [Google Scholar]
- 6.Cunningham F, Gant N, Leveno K, et al. Williams Obstetrics. 21. Mcgraw-Hill; 2001. Ectopic Pregnancy; pp. 899–902. [Google Scholar]
- 7.Jianping Z, Fen L, Qiu S. Full-Term Abdominal Pregnancy. A Case Report and Review of the Literature. Gynecol Obstet Invest. 2008;65(2):139–141. doi: 10.1159/000110015. [DOI] [PubMed] [Google Scholar]
- 8.Teng H, Kumar G, Ramli N. A viable secondary intra-abdominal pregnancy resulting from rupture of uterine scar: role of MRI. Br J Radiol. 2007;80:134–136. doi: 10.1259/bjr/67136731. [DOI] [PubMed] [Google Scholar]
- 9.Kun K, Wong P, Ho M, Tai C. Abdominal pregnancy presenting as a missed abortion at 16 weeks gestation. Hong Kong Med J. 2000;6(4):425–427. [PubMed] [Google Scholar]
- 10.Stevens CA. Malformations and deformations in abdominal pregnancy. Am J Med Genet. 1993;47(8):1189–1195. doi: 10.1002/ajmg.1320470812. [DOI] [PubMed] [Google Scholar]


