Abstract
Background: Obstructive Sleep Apnoea Syndrome (OSAS) is a condition of obstruction, apneas and arousals while sleeping. It has been suggested that OSAS independently influences glucose metabolism. The main treatment for OSAS is continuous positive airways pressure (CPAP).
Objectives: To assess the effects of CPAP on insulin resistance and glucose metabolism.
Search strategy: We searched Medline, Embase and the Cochrane Controlled Trial Register (January 2010).
Selection criteria: We included randomised and non-randomised trials comparing CPAP with inactive control or placebo CPAP in adults with OSAS.
Data collection and analysis: Two authors independently assessed trial quality and extracted data. Parallel and crossover group trials were analysed separately. A meta-analysis was carried out.
Results: Three parallel group and two cross-over randomised trials and one controlled trial were included investigating 296 participants. Sample sizes ranged from n=13 to n=102 participants, age was 18 to 75 years, mean body mass index (BMI) 27.2 kg/m² to 37.1 kg/m², mean apnoe hypopnoe index (AHI) 29.7 to 39.7 events per hour, mean dips >4% in arterial oxygen saturation per hour of sleep 1 to 42.7 events. The studies’ methodological quality varied. Follow-up ranged from 4 to 12 weeks. Various endpoints were investigated. CPAP did neither influence plasma insulin levels nor HOMA-index, adiponectin levels or HbA1c value. One study reported a significant positive effect on the insulin sensitivity index (1.68%/min, 95% CI 0.3 to 3.06).
Conclusion: This systematic review does not support the hypothesis that OSAS independently influences glucose metabolism. Sufficiently powered, long-term randomised controlled trials defining changes of insulin resistance as primary endpoint are needed.
Keywords: Insulin resistance, continuous positive airway pressure, obstructive sleep apnea, diabetes mellitus type 2, meta-analysis
Abstract
Hintergrund: Das Obstruktive Schlafapnoe-Syndrom (OSAS) ist durch wiederholte Apnoen mit nachfolgenden Weckreaktionen während des Schlafes gekennzeichnet. Es wird vermutet, dass obstruktive Schlafapnoen einen unabhängigen Einfluss auf den Glukosestoffwechsel haben. Leitlinien empfehlen die kontinuierliche Überdruckbeatmung (CPAP) zur Behandlung des OSAS.
Ziel: Systematische Sichtung und kritische Beurteilung klinischer Studien zu den Effekten einer CPAP-Beatmung auf Marker der Insulinresistenz und des Glukosestoffwechsels.
Suchstrategie: Die Suche erfolgte in den Datenbanken Medline, Embase und dem Cochrane Controlled Trial Register. Der Suchzeitraum erstreckte sich bis Januar 2010.
Ein- und Ausschlusskriterien: Eingeschlossen wurden randomisiert-kontrollierte und klinische kontrollierte Interventionsstudien, die eine CPAP-Therapie mit einer Placebo CPAP-Therapie oder einer nicht behandelten Kontrollgruppe bei Patienten mit OSAS verglichen hatten.
Datensammlung und Analyse: Zwei Autoren extrahierten die Daten unabhängig voneinander und beurteilten das Risiko für methodische Verzerrungen der eingeschlossenen Studien. In der Metaanalyse wurden Parallelgruppen- und Crossover-Studien getrennt voneinander analysiert.
Ergebnisse: Sechs Studien mit insgesamt 296 Probanden konnten eingeschlossen werden. Die Studien untersuchen 13 bis 102 Teilnehmer im Alter von 18 bis 75 Jahren. Der mittlere Body-Mass-Index (BMI) der Studienteilnehmer beträgt 27,2 kg/m² bis 37,1 kg/m², der mittlere Apnoe-Hypopnoe-Index (AHI) 29,7 bis 39,7 Ereignisse/Stunde, der mittlere Abfall der arteriellen Sauerstoffsättigung >4% pro Stunde beträgt 1 bis 42,7 Ereignisse. Die Nachbeobachtungszeit der Studien umfasst vier bis zwölf Wochen. Die methodische Qualität der Studien ist unterschiedlich. Vier der fünf randomisiert-kontrollierten Studien verwendeten ein doppelblindes Design; eine verdeckte Zuteilung zur jeweiligen Behandlungsgruppe ist lediglich in zwei Studien beschrieben. Eine Poweranalyse zur Fallzahlenkalkulation sowie ein Intention-to-Treat-Analyse zur adäquaten Nachbeobachtung wurde in drei der fünf Studien durchgeführt.
Das Poolen der Daten zeigte, dass eine CPAP-Therapie weder die Plasmainsulinspiegel, noch den Homaindex, die Adiponektinspiegel oder die HbA1c-Werte beeinflusst. Eine Studie berichtete über einen signifikant positiven Effekt der CPAP-Therapie auf den Insulinsensitivitätsindex (1,68%/min, 95% CI 0,3–3,06).
Schlussfolgerung: Das vorliegende systematische Review unterstützt nicht die Hypothese, dass die CPAP-Therapie einen unabhängigen Einfluss auf den Glukosestoffwechsel hat. Qualitativ hochwertige Studien mit primärem Endpunkt Insulinresistenz, ausreichend langer Nachbeobachtungszeit und adäquater Stichprobe stehen aus.
Introduction
Obstructive Sleep Apnoea Syndrome (OSAS) is deemed to be the most important respiratory dysfunction while sleeping. OSAS is defined by the coexistence of an obstructive sleep hypopnoe or apnoea and excessive sleepiness during the day [1]. Its symptoms result from intermittent hypoxia and sleep fragmentation caused by obstructive sleep apnoea [2]. OSAS is found in approximately 4% of middle-aged (30 to 60 years) men and 2% of women [3], [4].
Continuous positive airway pressure (CPAP) is used as first line treatment if symptoms and disease are severe. The effectiveness of CPAP regarding elimination of obstructive sleep apnoea has been proven by a number of randomised controlled studies [5], [6], [7], [8]. CPAP-therapy is likely to increase quality of life and to decrease fatigue during daytime in patients with intermediate and severe OSAS [9].
The association between OSAS and diabetes mellitus has been discussed controversially. In 2008, an international taskforce of the International Diabetes Federation (IDF) requested that doctors, health care policy and persons concerned should be alerted to the potential link between these diseases and asked to intensify research in this area [10]. Existing data suggest a higher OSAS prevalence amongst patients with diabetes mellitus [11], [12], [13], [14]. It remains unclear whether this is a causal relationship or due to coexistence of the two phenomena, because both diseases are commonly associated with obesity.
Several possibilities regarding the postulated relation of these two diseases are conceivable.
Intermittent hypoxia and arousals result in the activation of the sympathetic nervous system followed by the release of contra-insulin hormones like adrenaline and noradrenaline. Moreover, proteins known to induce insulin-resistance like interleukin 6 and tumor necrosis factor alpha are more frequently expressed [15], [16]. The accumulation of oxidative stress causing or boosting an insulin-resistance is also a matter of discussion [17], as well as a possible relevant shift in the concentration of the adipokines leptin, resistin and adiponectin. Finally, it is assumed that OSAS induced disturbance of the physiological sleep profile itself can cause an impaired glucose tolerance [18].
It is not clear whether eliminating of the factors mentioned above by the employment of CPAP-therapy would lead to a reduced insulin-resistance or an improved metabolic status for people diagnosed with diabetes type 2. Studies with OSAS patients which have investigated the impact of CPAP-therapy regarding insulin-sensitivity and glucose metabolism have shown heterogeneous results [19], [20], [21] [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39]. One of the reasons might be the difference in length of follow up.
Available reviews on this subject are non-systematic [10], [40], [41], [42], neither defining inclusion criteria nor critically appraising primary studies.
We therefore conducted a systematic review and a meta-analysis following current methodological approaches [43] aimed to assess the effects of CPAP-therapy on markers of insulin-resistance and glucose metabolism.
Methods
Search strategy
A systematic literature search was performed using the databases Medline (via PubMed), Embase, and the Cochrane Controlled Trial Register. Abstract books of the annual meetings of the German Diabetes Society (Deutsche Diabetes Gesellschaft) covering 1999 to 2009 were screened. The search strategy followed the recommendation of the Cochrane Handbook for Systematic Reviews of Interventions 5.0.2 [43]. The overall search strategy combined search terms for population (adults with OSAS), therapy (CPAP, nasal CPAP (nCPAP), automated positve airway pressure (APAP)), and endpoints (marker of insulin-resistance and glucose metabolism, respectively). Results were limited to clinical controlled studies (see Appendix for a detailed search strategy).
Selection of studies
Titles and abstracts or full texts of identified studies were screened based on pre-defined inclusion criteria:
Randomised and non-randomised controlled intervention study comparing CPAP, nCPAP or APAP (auto CPAP) therapy with either placebo CPAP therapy or a non treated control group
OSAS was diagnosed by respiratory polysomnography, age ≥18 years
Primary or secondary endpoint defined as marker for insulin-resistance (HOMA-index, plasma insulin level, adiponectin, Hyperinsulinemic Euglycemic Glucose Clamp trial) or glucose metabolism (HbA1c)
Exclusion criteria were:
No control group
Observational study (cohort study, case-control study), review or duplicate
Study having examined children and adolescents
Study having examined patients with a central sleep apnoea
Study that solely relied on blood glucose levels in order to determine insulin-resistance and glucose metabolism
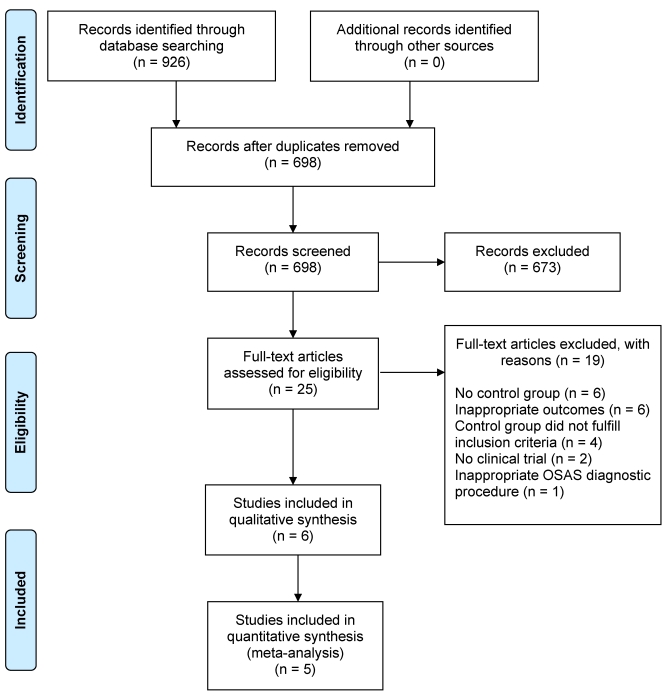
Figure 1 (Fig. 1) displays the flow of information through the review.
Figure 1. Flow Diagram.
Assessment of methodological quality of included studies
Two authors (LH and RM) assessed each trial independently. Disagreement was solved by discussion and consensus finding.
For randomised controlled trials the following criteria were applied:
Minimisation of selection bias: Adequate randomisation procedure and allocation concealment?
Minimisation of performance bias: Were participants and the investigators administering the treatment blinded towards the intervention? Similar treatment of study groups except intervention under investigation?
Minimisation of detection bias: Blinding of outcome assessors?
For non-randomised controlled studies the following criteria were applied:
Minimisation of selection bias: Description of all relevant patient characteristics (age, BMI, AHI, etc.)? Study groups comparable in terms of all relevant patient characteristics?
Minimisation of performance bias: Similar treatment of study groups except intervention under investigation?
Minimisation of detection bias: Adjustment for confounding?
For both, randomised and non-randomised trials:
-
Minimisation of attrition bias:
Follow-up of at least 80% of participants?
Intention-to-treat (ITT) principle used?
Data extraction
Patients’ clinical and demographic characteristics, outcomes, administration way and duration of therapy, and side effects were obtained independently by two reviewers using a standardised form and cross-checked for accuracy. Disagreement was solved by discussion and consensus finding.
Extracted data were entered into the Review Manager (RevMan) Version 5 Software.
Data analysis
A meta-analysis was carried out on the outcomes from parallel group studies with a fixed-effect model with mean differences (MD) as summary statistics for continuous variables. For crossover studies, mean differences and standard errors for the mean differences were calculated and entered into RevMan as generic inverse variance data. Heterogeneity was identified by visual inspection of the forest plots and by using a standard χ2-test with a significance level of α=0.1, in view of the low power of such tests. Heterogeneity was specifically examined with I2, where I2 values of 50% and more indicate a substantial level of heterogeneity.
Results
Results of the search
Our search strategy yielded a total of 926 studies; 920 papers were excluded.
Figure 1 (Fig. 1) displays the Flow Diagram.
Included studies
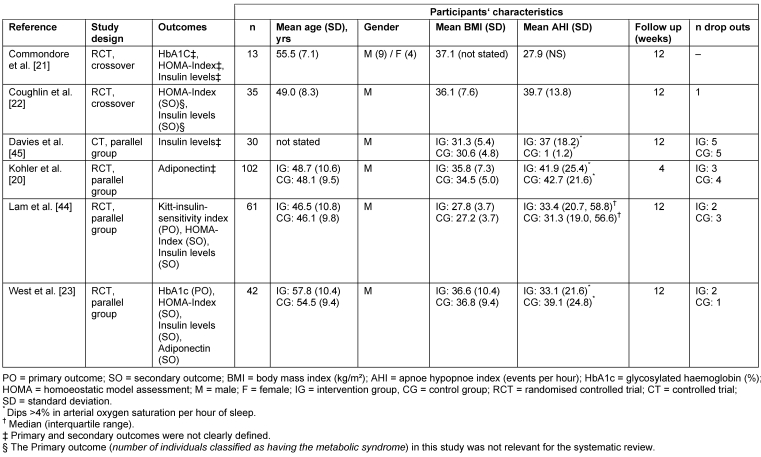
The final sample comprised six studies with a total of 296 participants. Five studies [20], [21], [22], [23], [44] were individually randomised, one [45] was a non-randomised controlled trial. Sample sizes ranged from n=13 to n=102 participants. Trials were carried out in three countries (China, United Kingdom, and Canada) between 1994 and 2009. One small study [21] investigated men and women; all other studies investigated only men. Participants’ age ranged from 18 to 75 years, mean BMI from 27.2 kg/m² to 37.1 kg/m², mean AHI from 29.7 to 39.7 events per hour, and mean dips >4% in arterial oxygen saturation per hour of sleep from 1 to 42.7 events. Five studies [20], [21], [22], [23], [44] stated OSAS diagnosed by polysomnography as inclusion criterion. Only the non-randomised trial by Davies et al. [45] included patients without OSAS in the control group. Four studies [20], [21], [23], [44] excluded patients requiring urgent CPAP because of respiratory failure, driving or job issues and one study [22] excluded patients with diabetes. The non-randomised trial by Davies et al. [45] stated no inclusion or exclusion criteria. Four trials [20], [22], [23], [44] compared CPAP respectively APAP with placebo-CPAP while two studies [21], [45] compared CPAP with no therapy. Insulin resistance was assessed by fasting plasma insulin levels and HOMA-Index, adiponectin, or Kitt-insulin-sensitivity index. HbA1c was assessed in two studies [21], [23].
Studies’ characteristics are displayed in Table 1 (Tab. 1).
Table 1. Characteristics of included studies.
Risk of bias in included studies
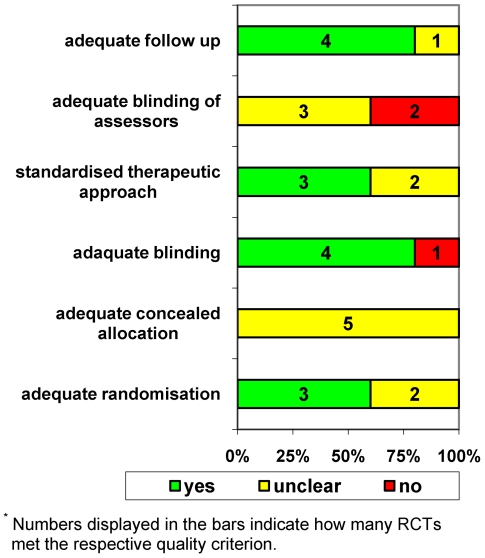
Figure 2 (Fig. 2) indicates varying methodological quality of the five included randomised controlled trials.
Figure 2. Methodological quality of the included randomised controlled trials (n=5)*.
Randomisation
Three studies seem to have used proper randomisation [22], [23], [44] whereas the randomisation method has not been described adequately in two studies [20], [21].
Adequate allocation of participants
None of the studies reported about the allocation procedure.
Blinding
Four out of five RCTs [20], [21], [23], [44] used double blinding of CPAP respiration in a subtherapeutical manner (placebo CPAP), in the fifth RCT [21] the control group did not receive treatment.
Standardized therapeutic approach
Three RCTs described methods to avoid unequal treatment of study groups [22], [23], [44].
Follow-up
Three RCTs [20], [22], [44] used ITT analysis. The study by West et al. [23] does not specify how data were analysed. Since more than 80% of patients randomised have been analysed, adequate follow-up examination can be assumed. The fifth study [21] does not describe exactly the number of participants analysed.
Power analysis
Three RCTs [22], [23], [44] reported to have performed a power analysis.
The non-randomised controlled study [45] lacks of a detailed description. It remains unclear whether the groups have been equally treated beyond the intervention in question. The dropout rate is 33% in both groups. Statistic analysis is precisely represented.
Effects of intervention
Results of the meta-analysis
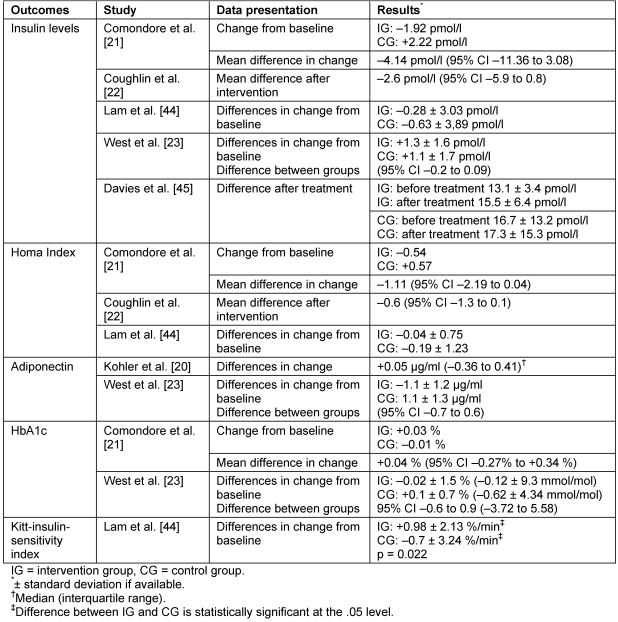
To judge the effect of CPAP respiration on marker of either insulin resistance or the glucose metabolism the mean values of the study group differences where pooled and assessed, respectively. Assuming that different authors used different laboratory techniques to determine their respective parameters, we also calculated standardised mean values of the differences. The results however remained the same and are therefore not displayed. A significant influence of the CPAP respiration on marker of either insulin resistance or the glucose metabolism was neither observable in the results of the individual (Table 2 (Tab. 2)) nor the pooled study. The study by Kohler et al. [20] was not included in the meta-analysis as this study reported the median rather than mean values.
Table 2. Results of included studies.
Statistical heterogeneity between studies was not apparent.
Results of the crossover studies
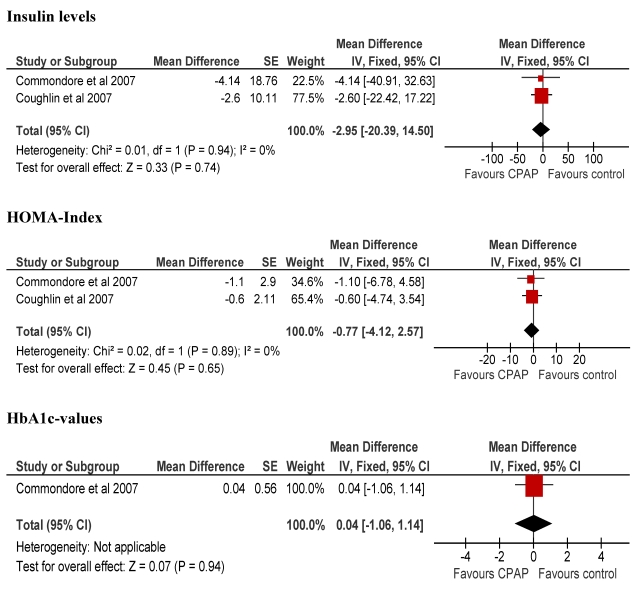
A significant reduction in insulin levels (2 studies, n=61) as a result of the CPAP-therapy was not calculated [mean difference (MD) –2.95 pmol/L, 95% CI –20.39 to 14.50]. Likewise the HOMA-index (2 studies, n=61) did not change significantly (MD –0.77, 95% CI –4.12 to 2.57). Changes in HbA1c-values were analysed to evaluate the glucose metabolism. A slight increase was calculated although it did not reach statistical significance (MD 0.04%, 95% CI –1.06 to 1.14) (MD 0.25 mmol/mol, 95% CI 6.57 to 7.07).
The results of crossover studies are displayed in Figure 3 (Fig. 3).
Figure 3. Results of crossover studies.
Results of the parallel group studies
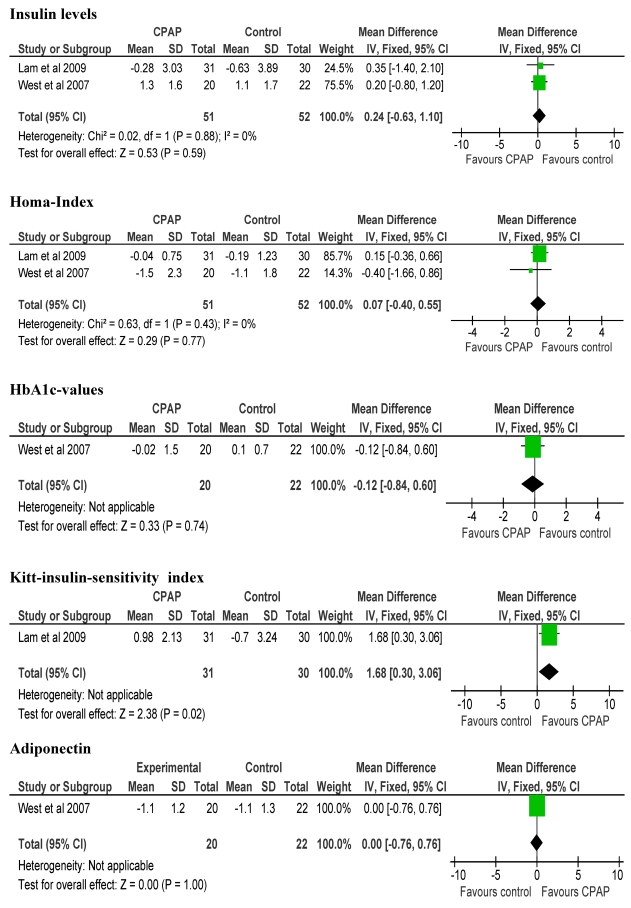
Pooling of data from two studies did not reveal a significant reduction in insulin levels (MD 0.24 pmol/L, 95% CI –0.63 to 1.10). The non-randomised controlled study by Davies et al. [45] did not show any influence of the CPAP therapy on plasma insulin levels either. Due to methodological shortcomings this study was not included in the meta-analysis.
Similar to the crossover studies the HOMA-index (2 studies n=103) did not change (MD 0.07, 95% CI –0.40 to 0.55).
Adiponectin levels have been assessed in two studies. A significant change of this parameter could not be observed.
Lam et al. [44] additionally determined the Kitt-insulin-sensitivity index, which increased statistically significant (MD 1.68%/min, 95% CI 0.3 to 3.06).
West et al. [23] did not report a positive influence of CPAP respiration on the HbA1c-value (MD –0.12%, 95% CI –0.84 to 0.60).
The results of parallel group studies are displayed in Figure 4 (Fig. 4).
Figure 4. Results of parallel group studies.
Discussion
Our meta-analysis demonstrated that CPAP-therapy neither positively affects clinical markers of glucose metabolism nor markers of insulin resistance.
Four studies have investigated plasma insulin level, HOMA-index and adiponectin in order to assess the extent of insulin resistance. None of the studies found beneficial effects. A single study [44] describes a significant increase of the insulin sensitivity index. The authors suggest a positive influence of CPAP-therapy on insulin resistance. However, no changes in the HOMA-index and plasma insulin level were found. Although considered as gold standard, the hyperinsulinemic-euglycemic clamp technique has not been used for assessment of insulin resistance. Nevertheless, the HOMA-index and the plasma insulin level are also well accepted methods [46]. Two groups [21], [23] examined HbA1c-values to evaluate the influence of CPAP on glucose metabolism. A significant reduction could not be found.
Non-controlled trials suggest that CPAP-therapy has beneficial effects towards the improving of glucose metabolism [28], [29], [30], [32], [36], [37], [47]. Since our meta-analysis did not confirm these findings, this is another piece of evidence demonstrating the discrepancies in results and conclusions between non-randomised and randomised trials.
The method to determine insulin resistance importantly influences the studies’ results. Harsch et al. [32] found a significant reduction of insulin resistance in n=40 OSAS patients studying the effect of CPAP-respiration in a non-controlled setting. The hyperinsulinemic-euglycemic clamp technique was used to determine insulin resistance. The diagnostic procedure is complex implicating insertion of a venous indwelling catheter, repeated blood testing and prolonged immobilisation. This might lead to an activation of the sympathetic nervous system which in turn could increase insulin resistance. Changes in the magnitude of insulin resistance before and after the deployment of a CPAP-therapy could therefore only result from the adaption to examination conditions [48].
It is of particular interest whether OSAS independently influences insulin resistance and glucose metabolism or whether an association solely coexists in the presence of obesity. Four of the five trials [20], [21], [22], [23] analysed in our review investigated participants with BMI between 35.8 and 37.1 kg/m². There was no evidence for an independent CPAP-therapy related effect on the glucose metabolism. Ip et al. [49] already suggested obesity as major determinant of insulin resistance while OSAS was judged to have a marginal influence.
Some experts argue that patients with high AHI may benefit more by CPAP concerning markers of insulin resistance or glucose metabolism. However, the results generated by the present review are independent of the severity of OSAS and populations’ characteristics. It remains unclear whether the results can be extrapolated to women since only four women were included in the review’s sample.
Compliance with CPAP was on average good varying between 4.7 and 5.5 hours per night in the three trials explicitly reporting on this issue [20], [21], [44]. Thus, lack of compliance is unlikely to explain our results. In the study by Coughlin et al. [22] good therapy compliance (>3.5 hrs per night) did not lead to better outcome. West et al. [44] did not find a significant correlation between the length of CPAP use and glucose metabolism.
Strengths and limitations of the review
The strength of our meta-analysis is the inclusion of randomised controlled trials only.
However, the primary studies are likely to be affected by important methodological flaws. Three of five randomised studies [20], [21], [22] did not report predefinition of the markers of insulin resistance and glucose metabolism as primary endpoints, two studies [20], [21] did not report a power analysis.
Agreement on a set of meaningful endpoints seems to be important for future randomised controlled trials investigating the effects of CPAP on diabetes outcomes. Design and reporting of trials should meet the contemporary standards of the CONSORT statement [50]. Unwanted side effects of CPAP-respiration should be carefully assessed. It is quite unacceptable that none of the six publications included in our review reported on adverse effects. Beyond that, four out of six publications [20], [21], [23], [45] did not present participants’ concomitant medication. However, information about participants’ prescribed medication is indispensable in this field of diabetes research.
We could not rule out a language bias of our systematic review since only English or German language publications were considered for inclusion. Two Chinese publications [24], [34] were excluded since the English full text was not accessible. However, the English abstract indicated that these publications would not have influenced our results.
We could also not exclude a publication bias. Funnel plot statistic was not feasible since the number of included studies was too small.
Conclusions
In summary, an independent influence of OSAS on glucose metabolism could not be confirmed. Thus, CPAP-therapy indication should be placed independently of these parameters especially for people suffering from diabetes.
The longest follow-up period of the included studies was 12 weeks only. Unfortunately, currently ongoing trials did not plan longer observation periods [51], [52], [53]. Since OSAS is a chronic disease a possible gradual reduction of insulin resistance or improvement of glucose metabolism through CPAP treatment lasting several months could not be excluded. This issue remains to be addressed in long-term randomised controlled trials. These trials should be sufficiently powered, include both sexes, and define changes of insulin resistance as primary endpoint. In the end, clinical efficacy remains to be proven in high quality trials investigating important outcomes such as diabetic complications and patient-reported outcomes.
Appendix: Search strategy
PubMed
exp. Sleep Apnea Syndromes
sas. tw
sleep apn* syndromes.tw
osa.tw
obstructive sleep apn*.tw
osas.tw
obstructive sleep apn* syndrome.tw
sahs.tw
sleep apn* / hypopn* syndrome.tw
apn*.tw
hypopn*.tw
#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11
continuous positive airway pressure.sh
positive-pressure respiration.sh
cpap.tw
continuous positive airway pressure.tw
ncpap.tw
nasal continuous positive airway pressure.tw
positive pressure respiration.tw
continuous distending pressure.tw
cdap.tw
distending pressure.tw
continuous positive transpulmonary pressure.tw
continuous transpulmonary pressure.tw
#13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24
exp. glucose metabolism disorder
diabetes mellitus.tw
diabetes.tw
iddm.tw
niddm.tw
mody.tw
glucose intolerance.sh
glucose toleran*.tw
reduced glucose toleran*.tw
reduced glucose metabolism.tw
glucose.tw
blood gluose.tw
exp. insulin resistance
insulin Resistance.tw
insulin sensitivity.tw
reduced insulin secret*.tw
impaired insulin secret*.tw
hemoglobin A, glycosylated.sh
HbA1c.tw
hemoglobin A1c.tw
#26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45
exp. clinical trial
prospective studies.sh
randomized controlled trials.sh
randomized controlled trial.pt
clinical trial.pt
controlled clinical trial.pt
meta-analysis.sh
exp. Review
systematic review.tw
#47 or #48 or #49 or #50 or #51 or #52 or #53 or #54 or #55
#12 and #25 and #46 and #56
tw = denotes a textword
exp = denotes a exploded Medical Subject Heading (MeSH) term
sh = denotes a Medical Subject Heading (MeSH) term
pt = denotes a Publication Type term
Notes
Competing interests
The authors declare that they have no competing interests.
References
- 1.Becker HF, Classen M, Dierkesmann R, Heimpel H. Rationelle Diagnostik und Therapie in der Inneren Medizin [Rational Diagnosis and Treatment in internal medicine] München-Jena: Urban & Fischer; 2003. Schlafbezogene Atmungsstörungen; pp. C 6: 1–C 6: 4. (Ger). [Google Scholar]
- 2.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):136–143. doi: 10.1513/pats.200709-155MG. Available from: http://dx.doi.org/10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):10. doi: 10.1056/NEJM199304293281704. Available from: http://dx.doi.org/10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 4.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217–1239. doi: 10.1164/rccm.2109080. Available from: http://dx.doi.org/10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 5.Ballester E, Badia JR, Hernández L, Carrasco E, de Pablo J, Fornas C, Rodriguez-Roisin R, Montserrat JM. Evidence of the effectiveness of continuous positive airway pressure in the treatment of sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med. 1999;159(2):495–501. doi: 10.1164/ajrccm.159.2.9804061. [DOI] [PubMed] [Google Scholar]
- 6.Engleman HM, Kingshott RN, Wraith PK, Mackay TW, Deary IJ, Douglas NJ. Randomized placebo-controlled crossover trial of continuous positive airway pressure for mild sleep Apnea/Hypopnea syndrome. Am J Respir Crit Care Med. 1999;159(2):461–467. doi: 10.1164/ajrccm.159.2.9803121. [DOI] [PubMed] [Google Scholar]
- 7.Jenkinson C, Davies RJ, Mullins R, Stradling JR. Comparison of therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised prospective parallel trial. Lancet. 1999;353(9170):2100–2105. doi: 10.1016/S0140-6736(98)10532-9. Available from: http://dx.doi.org/10.1016/S0140-6736(98)10532-9. [DOI] [PubMed] [Google Scholar]
- 8.Engleman HM, Martin SE, Kingshott RN, Mackay TW, Deary IJ, Douglas NJ. Randomised placebo controlled trial of daytime function after continuous positive airway pressure (CPAP) therapy for the sleep apnoea/hypopnoea syndrome. Thorax. 1998;53(5):341–345. doi: 10.1136/thx.53.5.341. Available from: http://dx.doi.org/10.1136/thx.53.5.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Giles TL, Lasserson TJ, Smith BJ, White J, Wright J, Cates CJ. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 2006;(1):CD001106. doi: 10.1002/14651858.CD001106.pub2. Available from: http://dx.doi.org/10.1002/14651858.CD001106.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Shaw JE, Punjabi NM, Wilding JP, Alberti KG, Zimmet PZ International Diabetes Federation Taskforce on Epidemiology and Prevention. Sleep-disordered breathing and type 2 diabetes: a report from the International Diabetes Federation Taskforce on Epidemiology and Prevention. Diabetes Res Clin Pract. 2008;81(1):2–12. doi: 10.1016/j.diabres.2008.04.025. Available from: http://dx.doi.org/10.1016/j.diabres.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 11.Reichmuth KJ, Austin D, Skatrud JB, Young T. Association of sleep apnea and type II diabetes: a population-based study. Am J Respir Crit Care Med. 2005;172(12):1590–1595. doi: 10.1164/rccm.200504-637OC. Available from: http://dx.doi.org/10.1164/rccm.200504-637OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meslier N, Gagnadoux F, Giraud P, Person C, Ouksel H, Urban T, Racineux JL. Impaired glucose-insulin metabolism in males with obstructive sleep apnoea syndrome. Eur Respir J. 2003;22(1):156–160. doi: 10.1183/09031936.03.00089902. Available from: http://dx.doi.org/10.1183/09031936.03.00089902. [DOI] [PubMed] [Google Scholar]
- 13.West SD, Nicoll DJ, Stradling JR. Prevalence of obstructive sleep apnoea in men with type 2 diabetes. Thorax. 2006;61(11):945–950. doi: 10.1136/thx.2005.057745. Available from: http://dx.doi.org/10.1136/thx.2005.057745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foster GD, Sanders MH, Millman R, Zammit G, Borradaile KE, Newman AB, Wadden TA, Kelley D, Wing RR, Sunyer FX, Darcey V, Kuna ST Sleep AHEAD Research Group. Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care. 2009;32(6):1017–1019. doi: 10.2337/dc08-1776. Available from: http://dx.doi.org/10.2337/dc08-1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsigos C, Papanicolaou DA, Kyrou I, Defensor R, Mitsiadis CS, Chrousos GP. Dose-dependent effects of recombinant human interleukin-6 on glucose regulation. J Clin Endocrinol Metab. 1997;82(12):4167–4170. doi: 10.1210/jc.82.12.4167. Available from: http://dx.doi.org/10.1210/jc.82.12.4167. [DOI] [PubMed] [Google Scholar]
- 16.Stith RD, Luo J. Endocrine and carbohydrate responses to interleukin-6 in vivo. Circ Shock. 1994;44(4):210–215. [PubMed] [Google Scholar]
- 17.Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, Nakayama O, Makishima M, Matsuda M, Shimomura I. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest. 2004;114(12):1752–1761. doi: 10.1172/JCI21625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E. Sleep loss: a novel risk factor for insulin resistance and Type 2 diabetes. J Appl Physiol. 2005;99(5):2008–2019. doi: 10.1152/japplphysiol.00660.2005. Available from: http://dx.doi.org/10.1152/japplphysiol.00660.2005. [DOI] [PubMed] [Google Scholar]
- 19.Patruno V, Aiolfi S, Costantino G, Murgia R, Selmi C, Malliani A, Montano N. Fixed and autoadjusting continuous positive airway pressure treatments are not similar in reducing cardiovascular risk factors in patients with obstructive sleep apnea. Chest. 2007;131(5):1393–1399. doi: 10.1378/chest.06-2192. Available from: http://dx.doi.org/10.1378/chest.06-2192. [DOI] [PubMed] [Google Scholar]
- 20.Kohler M, Ayers L, Pepperell JC, Packwood KL, Ferry B, Crosthwaite N, Craig S, Siccoli MM, Davies RJ, Stradling JR. Effects of continuous positive airway pressure on systemic inflammation in patients with moderate to severe obstructive sleep apnoea: a randomised controlled trial. Thorax. 2009;64(1):67–73. doi: 10.1136/thx.2008.097931. Available from: http://dx.doi.org/10.1136/thx.2008.097931. [DOI] [PubMed] [Google Scholar]
- 21.Comondore VR, Cheema R, Fox J, Butt A, John Mancini GB, Fleetham JA, Ryan CF, Chan S, Ayas NT. The impact of CPAP on cardiovascular biomarkers in minimally symptomatic patients with obstructive sleep apnea: a pilot feasibility randomized crossover trial. Lung. 2009;187(1):17–22. doi: 10.1007/s00408-008-9115-5. Available from: http://dx.doi.org/10.1007/s00408-008-9115-5. [DOI] [PubMed] [Google Scholar]
- 22.Coughlin SR, Mawdsley L, Mugarza JA, Wilding JP, Calverley PM. Cardiovascular and metabolic effects of CPAP in obese males with OSA. Eur Respir J. 2007;29(4):720–727. doi: 10.1183/09031936.00043306. Available from: http://dx.doi.org/10.1183/09031936.00043306. [DOI] [PubMed] [Google Scholar]
- 23.West SD, Nicoll DJ, Wallace TM, Matthews DR, Stradling JR. Effect of CPAP on insulin resistance and HbA1c in men with obstructive sleep apnoea and type 2 diabetes. Thorax. 2007;62(11):969–974. doi: 10.1136/thx.2006.074351. Available from: http://dx.doi.org/10.1136/thx.2006.074351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.He L, Li S, Shi H, Feng Y. The clinical investigation of the relationship between obstructive sleep apnea-hypopnea syndrome and insulin resistance. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2007;21(8):353–355. [PubMed] [Google Scholar]
- 25.Lindberg E, Berne C, Elmasry A, Hedner J, Janson C. CPAP treatment of a population-based sample--what are the benefits and the treatment compliance? Sleep Med. 2006;7(7):553–560. doi: 10.1016/j.sleep.2005.12.010. Available from: http://dx.doi.org/10.1016/j.sleep.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 26.Trenell MI, Ward JA, Yee BJ, Phillips CL, Kemp GJ, Grunstein RR, Thompson CH. Influence of constant positive airway pressure therapy on lipid storage, muscle metabolism and insulin action in obese patients with severe obstructive sleep apnoea syndrome. Diabetes Obes Metab. 2007;9(5):679–687. doi: 10.1111/j.1463-1326.2006.00649.x. Available from: http://dx.doi.org/10.1111/j.1463-1326.2006.00649.x. [DOI] [PubMed] [Google Scholar]
- 27.Dorkova Z, Petrasova D, Molcanyiova A, Popovnakova M, Tkacova R. Effects of continuous positive airway pressure on cardiovascular risk profile in patients with severe obstructive sleep apnea and metabolic syndrome. Chest. 2008;134(4):686–692. doi: 10.1378/chest.08-0556. Available from: http://dx.doi.org/10.1378/chest.08-0556. [DOI] [PubMed] [Google Scholar]
- 28.Nakagawa Y, Kishida K, Kihara S, Sonoda M, Hirata A, Yasui A, Nishizawa H, Nakamura T, Yoshida R, Shimomura I, Funahashi T. Nocturnal reduction in circulating adiponectin concentrations related to hypoxic stress in severe obstructive sleep apnea-hypopnea syndrome. Am J Physiol Endocrinol Metab. 2008;294(4):E778–E784. doi: 10.1152/ajpendo.00709.2007. Available from: http://dx.doi.org/10.1152/ajpendo.00709.2007. [DOI] [PubMed] [Google Scholar]
- 29.Pallayova M, Donic V, Tomori Z. Beneficial effects of severe sleep apnea therapy on nocturnal glucose control in persons with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2008;81(1):e8–11. doi: 10.1016/j.diabres.2008.03.012. Available from: http://dx.doi.org/10.1016/j.diabres.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 30.Babu AR, Herdegen J, Fogelfeld L, Shott S, Mazzone T. Type 2 diabetes, glycemic control, and continuous positive airway pressure in obstructive sleep apnea. Arch Intern Med. 2005;165(4):447–452. doi: 10.1001/archinte.165.4.447. Available from: http://dx.doi.org/10.1001/archinte.165.4.447. [DOI] [PubMed] [Google Scholar]
- 31.Shimizu Y, Dobashi K, Horie T, Koga Y, Yoshii A, Utsugi M, et al. Rapid effect of nCPAP therapy on circulating plasma leptin in OSAS patients. Kitakanto Med J. 2005;55(1):29–35. doi: 10.2974/kmj.55.29. Available from: http://dx.doi.org/10.2974/kmj.55.29. [DOI] [Google Scholar]
- 32.Harsch IA, Schahin SP, Brückner K, Radespiel-Tröger M, Fuchs FS, Hahn EG, Konturek PC, Lohmann T, Ficker JH. The effect of continuous positive airway pressure treatment on insulin sensitivity in patients with obstructive sleep apnoea syndrome and type 2 diabetes. Respiration. 2004;71(3):252–259. doi: 10.1159/000077423. Available from: http://dx.doi.org/10.1159/000077423. [DOI] [PubMed] [Google Scholar]
- 33.Harsch IA, Schahin SP, Radespiel-Tröger M, Weintz O, Jahreiss H, Fuchs FS, Wiest GH, Hahn EG, Lohmann T, Konturek PC, Ficker JH. Continuous positive airway pressure treatment rapidly improves insulin sensitivity in patients with obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2004;169(2):156–162. doi: 10.1164/rccm.200302-206OC. Available from: http://dx.doi.org/10.1164/rccm.200302-206OC. [DOI] [PubMed] [Google Scholar]
- 34.Huang R, Huang XZ, Wang HG, Li M, Xiao Y. Effects of nasal continuous positive airway pressure on serum leptin concentration and the metabolic parameters in obstructive sleep apnea hypopnea syndrome. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2004;26(2):168–171. [PubMed] [Google Scholar]
- 35.Harsch IA, Wallaschofski H, Koebnick C, Pour Schahin S, Hahn EG, Ficker JH, Lohmann T. Adiponectin in patients with obstructive sleep apnea syndrome: course and physiological relevance. Respiration. 2004;71(6):580–586. doi: 10.1159/000081758. Available from: http://dx.doi.org/10.1159/000081758. [DOI] [PubMed] [Google Scholar]
- 36.Pierzchala W, Ograbek M. Sleep apnea syndrome in patients with diabetes. Effectiveness of treatment for respiratory assistance at night with continuous positive airway pressure. Wiad Lek. 1998;51(3-4):166–172. [PubMed] [Google Scholar]
- 37.Brooks B, Cistulli PA, Borkman M, Ross G, McGhee S, Grunstein RR, Sullivan CE, Yue DK. Obstructive sleep apnea in obese noninsulin-dependent diabetic patients: effect of continuous positive airway pressure treatment on insulin responsiveness. J Clin Endocrinol Metab. 1994;79(6):1681–1685. doi: 10.1210/jc.79.6.1681. Available from: http://dx.doi.org/10.1210/jc.79.6.1681. [DOI] [PubMed] [Google Scholar]
- 38.Harsch IA, Koebnick C, Wallaschofski H, Schahin SP, Hahn EG, Ficker JH, Lohmann T, Konturek PC. Resistin levels in patients with obstructive sleep apnoea syndrome--the link to subclinical inflammation? Med Sci Monit. 2004;10(9):CR510–CR515. [PubMed] [Google Scholar]
- 39.Cooper BG, White JE, Ashworth LA, Alberti KG, Gibson GJ. Hormonal and metabolic profiles in subjects with obstructive sleep apnea syndrome and the acute effects of nasal continuous positive airway pressure (CPAP) treatment. Sleep. 1995;18(3):172–179. [PubMed] [Google Scholar]
- 40.Steiropoulos P, Papanas N, Nena E, Maltezos E, Bouros D. Continuous positive airway pressure treatment in patients with sleep apnoea: does it really improve glucose metabolism? Curr Diabetes Rev. 2010;6(3):156–166. doi: 10.2174/157339910791162943. Available from: http://dx.doi.org/10.2174/157339910791162943. [DOI] [PubMed] [Google Scholar]
- 41.Bhadriraju S, Kemp CR, Jr, Cheruvu M, Bhadriraju S. Sleep apnea syndrome: implications on cardiovascular diseases. Crit Pathw Cardiol. 2008;7(4):248–253. doi: 10.1097/HPC.0b013e31818ae644. Available from: http://dx.doi.org/10.1097/HPC.0b013e31818ae644. [DOI] [PubMed] [Google Scholar]
- 42.Schulz R, Eisele HJ, Reichenberger F, Seeger W. Obstruktive Schlaf-Apnoe und metabolisches Syndrom. [Obstructive sleep apnoea and metabolic syndrome]. Pneumologie. 2008;62(2):88–91. doi: 10.1055/s-2007-996175. (Ger). Available from: http://dx.doi.org/10.1055/s-2007-996175. [DOI] [PubMed] [Google Scholar]
- 43.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.2. The Cochrane Collaboration; 2010. [accessed 18 Sep 2010]. Available from: http://www.cochrane-handbook.org. [Google Scholar]
- 44.Lam JC, Lam B, Yao TJ, Lai AY, Ooi CG, Tam S, Lam KS, Ip MS. A randomised controlled trial of nasal continuous positive airway pressure on insulin sensitivity in obstructive sleep apnoea. Eur Respir J. 2010;35(1):138–145. doi: 10.1183/09031936.00047709. Available from: http://dx.doi.org/10.1183/09031936.00047709. [DOI] [PubMed] [Google Scholar]
- 45.Davies RJ, Turner R, Crosby J, Stradling JR. Plasma insulin and lipid levels in untreated obstructive sleep apnoea and snoring; their comparison with matched controls and response to treatment. J Sleep Res. 1994;3(3):180–185. doi: 10.1111/j.1365-2869.1994.tb00126.x. Available from: http://dx.doi.org/10.1111/j.1365-2869.1994.tb00126.x. [DOI] [PubMed] [Google Scholar]
- 46.Ferrannini E, Mari A. How to measure insulin sensitivity. J Hypertens. 1998;16(7):895–906. doi: 10.1097/00004872-199816070-00001. Available from: http://dx.doi.org/10.1097/00004872-199816070-00001. [DOI] [PubMed] [Google Scholar]
- 47.Schahin SP, Nechanitzky T, Dittel C, Fuchs FS, Hahn EG, Konturek PC, Ficker JH, Harsch IA. Long-term improvement of insulin sensitivity during CPAP therapy in the obstructive sleep apnoea syndrome. Med Sci Monit. 2008;14(3):CR117–CR121. [PubMed] [Google Scholar]
- 48.Moan A, Høieggen A, Nordby G, Birkeland K, Eide I, Kjeldsen SE. The glucose clamp procedure activates the sympathetic nervous system even in the absence of hyperinsulinemia. J Clin Endocrinol Metab. 1995;80(11):3151–3154. doi: 10.1210/jc.80.11.3151. Available from: http://dx.doi.org/10.1210/jc.80.11.3151. [DOI] [PubMed] [Google Scholar]
- 49.Ip MS, Lam B, Ng MM, Lam WK, Tsang KW, Lam KS. Obstructive sleep apnea is independently associated with insulin resistance. Am J Respir Crit Care Med. 2002;165(5):670–676. doi: 10.1164/ajrccm.165.5.2103001. [DOI] [PubMed] [Google Scholar]
- 50.Schulz KF, Altman DG, Moher D CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. doi: 10.1136/bmj.c332. Available from: http://dx.doi.org/10.1136/bmj.c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Van Cauter E. Effects of Continuous Positive Airway Pressure (CPAP) Treatment on Glucose Control in Patients with Type 2 Diabetes. ClinicalTrials.gov; [accessed 01 Nov 2010]. Available from: http://clinicaltrials.gov/ct2/show/NCT01136785. [Google Scholar]
- 52.Lam JC. The Effect of Nasal Continuous Positive Airway Pressure Treatment on Glycemic Control and Vascular Function in Patients with Obstructive Sleep Apnea and Type II Diabetes Mellitus. ClinicalTrials.gov.; [accessed 01 Nov 2010]. Available from: http://clinicaltrials.gov/ct2/show/NCT00876980. [Google Scholar]
- 53.Tasali E. Effective Treatment of Sleep Apnea in Prediabetes to Reduce Cardiometabolic Risk. ClinicalTrials.gov.; [accessed 01 Nov 2010]. Available from: http://clinicaltrials.gov/ct2/show/NCT01156116. [Google Scholar]