Abstract
Background: There is an increased prevalence of diabetes. Doctors in training, irrespective of specialty, will have patients with diabetes under their care.
Aim: To determine levels of confidence of doctors in training in the management of diabetes and establish their training needs in this area of clinical practice
Design: A national online survey of trainee doctors in the UK using a pre-validated questionnaire.
Methods: A four-point confidence rating scale was used to rate confidence in the management of diabetes and comparators. A six-point scale was used to quantify how often trainees would contribute to the management of patients with diabetes and trainees were asked about their training in managing diabetes.
Results: A total of 2149 doctors completed the survey. The percentage ‘fully confident’ in diagnosing diabetes was 27%, diagnosing and managing hypoglycaemia 55%, diagnosing and managing diabetic ketoacidosis 43%, managing intravenous (IV) insulin 27%, prescribing IV fluids for patients with diabetes 39% and altering diabetes therapy prior to surgery/other procedure 18%. In comparison, 66% and 65% were ‘fully confident’ in the management of angina and asthma, respectively (P < 0.05). Forty-one percent would take the initiative to optimize glycaemic control for patients under their care >80% of the time. Respectively, 19% and 35% of respondents reported that their undergraduate and postgraduate training had prepared them adequately to optimize treatment of diabetes. The majority (>70%) wanted further training in managing all aspects of diabetes care.
Conclusions: Trainee doctors in the UK lack confidence in the management of diabetes, are unlikely to take the initiative to optimize glycaemic control and report a need for further training.
Introduction
It has been estimated that the prevalence of diabetes in the UK could be as much as 3.6 million in 2010 rising to more than 5.3 million in 2030.1 At present in the UK, 10–20% of all hospital inpatients have diabetes.2 With this increasing prevalence, the percentage of hospital inpatients with diabetes is expected to rise. Therefore, trainee doctors working in hospitals are likely to be responsible for the care of patients who have diabetes, irrespective of their specialty role or the patients’ presenting complaints. Additionally, trainees drawn from various specialties currently make up hospital teams that provide acute medical care out of hours, which includes the management of diabetes emergencies.
In a multi-centre pilot cohort of UK trainee doctors, we have demonstrated a lack of confidence in managing diabetes, including the management of diabetes-related emergencies.3 Meanwhile, qualitative studies assessing the inpatient experiences of people with diabetes suggest dissatisfaction with the level of care received including the perception that staff not specializing in diabetes appeared to lack a basic knowledge about diabetes, leading to suboptimal clinical care.4
For any health-care system to cope with the increasing prevalence while providing best care to all patients with diabetes, doctors at the frontline need to be confident, competent and adequately trained in the diagnosis and management of diabetes and diabetic emergencies. The Trainees Own Perception of Delivery of Care (TOPDOC) Diabetes Study was established to assess UK trainees’ confidence in managing diabetes, to assess their current practice in the management of patients with diabetes and to identify specific training needs.
Aims
The TOPDOC Diabetes Study aimed to quantify the self-reported confidence levels of trainee doctors working in the UK in the diagnosis and management of diabetes and diabetic emergencies, by using a validated questionnaire. The study also aimed to assess the current practice of trainees in optimizing diabetes care and establish whether trainees desired further training in various aspects of diabetes care.
Methods
The TOPDOC study was an online survey of trainee doctors using a pre-validated questionnaire using peer-reviewed assessment tools. The protocol for the study is published in full elsewhere.5
Study participants
All trainee doctors (foundation and specialist trainees) practicing in the UK at the time of the survey were eligible to take part. Statistical calculations indicated that 248 respondents were needed to give 90% power, at 5% significance, between consecutive answers in the six-point rating scale used in the study. We targeted responses from 1000 UK trainee doctors across all specialties other than diabetes and endocrinology. This would represent around 2% of the total potential study population.
Assessment tools
We assessed the confidence of respondents using the validated Royal College of Physicians ‘Confidence Rating’ (CR) scale.6 This scale, commonly used in the self-assessment of trainee doctors, has four points—CR1: ‘not confident’, CR2: ‘satisfactory but lacking confidence’, CR3: ‘confident in some cases’ and CR4: ‘fully confident in most cases’. To assess how frequently trainees would be doing something in day-to-day practice, we used a six-point scale with narrative description in combination with numeric values. Respondents had a choice of ‘always’ (100% of the time), ‘almost always’ (80–99% of the time), ‘often’ (50–79% of the time), ‘not very often’ (20–49% of the time), ‘rarely’ (5–19% of the time) or ‘never’ (<5% of the time). Trainees were also asked whether they felt that their undergraduate and postgraduate training was adequate and whether they felt they required further training to deal with aspects of managing patients with diabetes.
Validation
The TOPDOC Study questionnaire was pre-validated in a four-stage process: (i) initial review by external experts in the field of diabetes, (ii) administration of initial draft on a sample cohort, (iii) revision of questionnaire based on feedback received and (iv) final external review. To ensure the validity of respondents and to prevent the submission of duplicate forms, General Medical Council registration numbers, requested and necessary to complete the study, were crosschecked with the medical register.7
Recruitment
Trainee doctors were recruited through a comprehensive campaign using regional facilitators who encouraged completion of the questionnaire through their local hospital or regional training networks, and a promotional campaign through medical news sources. Promotional material highlighting this study was sent to all post-graduate training centres in the UK. Incentives were offered to respondents completing the study, in the form of online vouchers.
Statistics
We used the χ2 test to establish significance, comparing full confidence in the diagnosis and management of both diabetic and non-diabetic problems. Data are reported as median (25th to 75th centile).
Governance
The Research Ethics Committee of Glasgow Royal Infirmary reviewed the study and the Chairman advised that no formal ethical approval was required.
Results
Demographics
A total of 2149 validated complete responses to the online questionnaire were received. All regions of the UK were represented including 312 (14.5%) responses from Scotland, 306 (14.2%) from Wales and 172 (8.0%) from Northern Ireland. The median number of years of full-time post-graduate training was two. The respondents stated it was likely they would pursue a career in the following specialties: 41% in general (internal) medicine and its subspecialties, 18% in primary care, 12% in anaesthetics, 10% in surgery, 6% in paediatrics, 4% in emergency medicine, 4% in women’s health, 2% in psychiatry and 2% in diagnostics.
Confidence in diagnosis and management
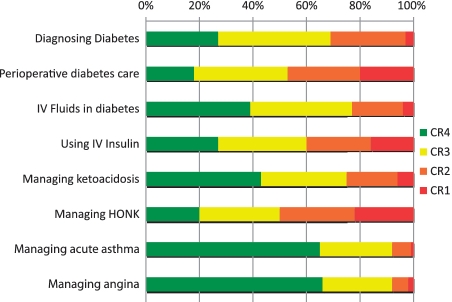
Trainee doctors’ confidence in diagnosis and management of various aspects of diabetes care are shown in Table 1. The percentage of respondents, respectively, reporting that they were ‘fully confident’ in different aspects of diabetes management (in brackets) were: diagnosing diabetes (27%); diagnosing impaired glucose tolerance (13%); diagnosing and managing hypoglycaemia (55%); diagnosing and managing diabetic ketoacidosis (43%); diagnosing and managing hyperosmolar hyperglycaemic non-ketotic coma (20%); commencing, titrating and discontinuing intravenous (IV) insulin (27%); prescribing IV fluids for patients with diabetes (39%); and altering diabetes therapy prior to surgery/other procedure (18%). Self-reported confidence levels across all diabetes-related domains studied were significantly lower than in the two similar areas of medicine studied with 66% fully confident in the management of angina and 65% fully confident in the management of asthma (P < 0.05; Figure 1). This finding was found irrespective of numbers of years of postgraduate experience.
Table 1.
Postgraduate trainee doctors’ confidence in managing diabetes
| Questions | Fully confident | Confident | Satisfactory | Not confident |
|---|---|---|---|---|
| How confident are you in | ||||
| Making a diagnosis of diabetes? | 576 (27) | 903 (42) | 600 (28) | 70 (3) |
| Making a diagnosis of impaired glucose tolerance? | 287 (13) | 802 (37) | 745 (35) | 315 (15) |
| Diagnosing and managing hypoglycaemia? | 1189 (55) | 657 (31) | 285 (13) | 18 (1) |
| Diagnosing and managing DKA? | 932 (43) | 680 (32) | 410 (19) | 127 (6) |
| Diagnosing and managing HONK? | 423 (20) | 645 (30) | 605 (28) | 476 (22) |
| Commencing, titrating and discontinuing IV insulin? | 586 (27) | 705 (33) | 512 (24) | 346 (16) |
| Prescribing IV fluids for patients with diabetes? | 828 (39) | 811 (38) | 418 (19) | 92 (4) |
| Altering diabetes therapy prior to surgery/other procedure? | 378 (18) | 762 (35) | 570 (27) | 439 (20) |
Data are expressed as n (%).
DKA: diabetic ketoacidosis; HONK: hyperosmloar hyperglycaemic non-ketotic coma; IV: Intravenous.
Figure 1.
Confidence in managing aspects of diabetes care vs. other common diseases (CR4: ‘fully confident in most cases’, CR3: ‘confident in some cases’, CR2: ‘satisfactory but lacking confidence’ and CR1: ‘not confident’. Confidence in managing all aspects of diabetes care is significantly lower compared with confidence in managing angina or acute asthma.
Current practice
Table 2 shows the frequency that trainees become actively involved in the management of people with diabetes. Forty-one percent of trainees reported that they would take the initiative to optimize glycaemic control for patients under their care ‘always’ or ‘almost always’ (80% of the time or more) but 59% would not. When faced with suboptimal glycaemic control, 13% would optimize oral therapy, 29% modify insulin regime and 31% would educate patients at least 80% of the time. A higher proportion of senior trainees took these therapeutic initiatives (data not shown in table), but there was not a statistically significant difference in their responses from the total group. The reasons cited by trainees for not optimizing patient care include: glycaemic control not an acute issue, not had enough training, care should be left to the specialist and a perception that other clinical issues were higher priorities.
Table 2.
Postgraduate trainee doctors’ current management of diabetes
| Questions | Always | Almost always | Often | Not very often | Rarely | Never |
|---|---|---|---|---|---|---|
| If a patient under your care has diabetes how often would you take the initiative to improve diabetes control? | 174 (8) | 703 (33) | 766 (36) | 381 (18) | 103 (5) | 22 (1) |
| When faced with a patient with poor blood glucose control: | ||||||
| How often do you educate the patients on lifestyle factors? | 150 (7) | 508 (24) | 590 (27) | 562 (26) | 281 (13) | 58 (3) |
| On oral therapy how often do you change the dose/timing of oral diabetes therapy? | 44 (2) | 241 (11) | 495 (23) | 629 (29) | 443 (21) | 297 (14) |
| On insulin how often do you change the dose/ timing/type of insulin? | 120 (6) | 488 (23) | 637 (30) | 424 (20) | 313 (15) | 167 (8) |
| When managing patients with specific problems related to their diabetes do you take the initiative to involve diabetes specialists (doctors/nurses)? | 422 (20) | 996 (46) | 588 (27) | 113 (5) | 25 (1) | 5 (0) |
| Do you follow-up on blood glucose control once patients have been seen by the diabetes specialists? | 219 (10) | 663 (31) | 621 (29) | 371 (17) | 167 (8) | 108 (5) |
| When discharging patients with diabetes do you make arrangements for ongoing monitoring of control? | 231 (11) | 537 (25) | 588 (27) | 450 (21) | 239 (11) | 104 (5) |
Data are expressed as n (%).
Training needs
Trainees’ previous training and perceived training needs are shown in Table 3. Fifty-eight percent of respondents felt their undergraduate training had prepared them to diagnose diabetes. Fifty-four percent felt postgraduate training provided them with the skills to diagnose diabetes. Nineteen percent of respondents felt their undergraduate training had prepared them to optimize the treatment of diabetes and 35% reported the same about their postgraduate training. Finally, 51% of respondents felt their undergraduate training had not prepared them adequately to treat diabetes emergencies and 67% reported the same about their postgraduate training. Seventy-five percent of all respondents would welcome further training in diagnosing diabetes, 85% in optimizing diabetes therapy and 70% in the management of diabetes emergencies.
Table 3.
Postgraduate trainee doctors’ self-assessment of the adequacy of their training
| Questions | Yes | No |
|---|---|---|
| Do you think that your undergraduate training has prepared you adequately to diagnose diabetes and other glucose abnormalities? | 1250 (58) | 899 (42) |
| Do you think that your postgraduate training has prepared you adequately to diagnose diabetes and other glucose abnormalities? | 1163 (54) | 986 (46) |
| Do you require further training in the diagnosis of diabetes and other glucose abnormalities? | 1607 (75) | 542 (25) |
| Do you think that your undergraduate training has prepared you adequately to treat diabetic emergencies? | 1050 (49) | 1099 (51) |
| Do you think that your postgraduate training has prepared you adequately to treat diabetic emergencies? | 1430 (67) | 719 (33) |
| Do you require more training in the management of diabetic emergencies? | 1510 (70) | 639 (30) |
| Do you think that your undergraduate training has prepared you adequately to optimize treatment of diabetes? | 419 (19) | 1730 (81) |
| Do you think that your postgraduate training has prepared you adequately to optimize treatment of diabetes? | 760 (35) | 1389 (65) |
| Do you require further training in the use of tablets and insulin to control blood glucose levels? | 1820 (85) | 329 (15) |
Data are expressed as n (%).
Discussion
This national survey of a large number of UK trainee doctors indicates insufficient confidence in diagnosing and managing all aspects of diabetes care. The study included a representative spread of trainees with varied specialty career intentions currently based in the UK, capturing >4% of the 50 145 doctors in postgraduate training.8 Many are likely to continue in those specialties given that there is evidence that only about one-quarter finally work in a specialty that is different to one chosen early in their career.9 One weakness of the study may be that the results are based on self-reported confidence, and that this might not necessarily equate to trainee competence, but this was not the intention at the outset. The results have demonstrated significantly lower confidence in managing diabetes compared with other common acute medical conditions such as angina or asthma. Areas of suboptimal confidence include the management of diabetic emergencies where mortality and morbidity can be high.
Over two-thirds of all respondents would welcome further training in all aspects of diabetes care. In addition to trainee doctors being directed towards currently available training resources such as the safe use of insulin e-learning course,10 further efforts are needed to provide structured education in all aspects of the management of diabetes. This would complement national organizational changes being implemented to reduce prescription errors in diabetes11 and improve acute care for people with diabetes. If structured training can be provided, with subsequent improvement in confidence levels of trainees, it might ensure that people with diabetes admitted to hospital, whether it is primarily an admission related to their diabetes or not, get the quality of diabetes care that they require.
Funding
This work was supported by the Association of British Clinical Diabetologists (ABCD) through a competitive audit prize administered and adjudicated independently by the ABCD but supported by Eli Lily and Co. Ltd. The study design and the collection, analysis, interpretation of data, the writing of this article and the decision to submit it for publication, are all independent of the funding body. Initial pump-priming funding for this study was provided by Sanofi-aventis UK as an unrestricted educational grant.
Conflict of interest: None declared.
Acknowledgements
Consultant diabetologists Dr David M Matthews (deceased), Dr Elizabeth McIntyre and Dr A Anwar helped us with external validation of the initial questionnaire. Kim Suares provides administrative support for the TOPDOC Diabetes Study. We are also grateful to the National Director for Diabetes (Dr Rowan Hillson), Diabetes UK, Society for Endocrinology, British Medical Association, postgraduate deaneries across the UK and the Young Diabetologists’ Forum for supporting participant recruitment. The Medical Research Council funds J.T.G.’s current position. J.T.G. came up with the concept for this research project. J.T.G., G.A.M. and E.B.J. designed the study questionnaire, modified with input from H.C.P., E.G.W. and P.K. G.A.M. led the study and is the guarantor. J.T.G., K.S.R., D.J.M. and D.W. undertook the literature review and J.T.G. co-ordinated data acquisition. D.W. and J.T.G. carried out data analysis in accordance with statistical analysis plan developed by I.M.S. J.T.G. and G.A.M. drafted this manuscript, which was revised by D.J.M. and amended and approved by all authors who had full access to the data including statistics tables.
The TOPDOC Diabetes Study team includes McGovan B., Thow J.C., Atkin S.L., Abbas A., Ahluwalia R., Anthony J., Atkin M., Baburaj R., Balasanthiran A., Banarjee A., Bhake R., Black N., Chakera A., Chudleigh R.A., Diacon C., Fifri C., Fountain A.C.E., Herring R., Maitland R.A., Nathan Y., Noimark D., Otti C., Patel D., Phillip S., Schofield C.J., Shekar M., Vas P. and Vijayaraman A., who implemented the study in geographical regions across the UK.
References
- 1.Association of Public Health Observatories Diabetes Prevalence Model. [ http://www.yhpho.org.uk/default.aspx?RID=81090] 2010, Accessed 11 March 2011.
- 2.Wallymahmed ME, Dawes S, Clarke G, Saunders S, Younis N, MacFarlane IA. Hospital in-patients with diabetes: increasing prevalence and management problems. Diabetic Med. 2005;22:107–9. doi: 10.1111/j.1464-5491.2004.01355.x. [DOI] [PubMed] [Google Scholar]
- 3.George JT, Warriner DA, Anthony J, Rozario KS, Xavier S, Jude EB, et al. Training tomorrow’s doctors in diabetes: self-reported confidence levels, practice and perceived training needs of post-graduate trainee doctors in the UK. A multi-centre survey. BMC Med Educ. 2008;8:22. doi: 10.1186/1472-6920-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Healthcare Commission. The views of people with diabetes. 2007. [ http://www.cqc.org.uk/_db/_documents/Diabetes_survey_2006_summary.pdf] Accessed 11 March 2011.
- 5.George JT, McGrane DJ, Warriner D, Rozario KS, Price HC, Wilmot EG, et al. on behalf of the TOPDOC Study Team. Protocol for a national audit on self-reported confidence levels, training requirements and current practice among trainee doctors in the UK: the Trainees Own Perception of Delivery of Care in Diabetes (TOPDOC) Study. BMC Med Educ. 2010;10:54. doi: 10.1186/1472-6920-10-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Federation of Royal College of Physicians. Appraisal record for senior house officers. [ http://www.webcitation.org/5XTdGuCMO] Accessed 11 March 2011.
- 7.General Medical Council medical register. [ http://www.gmc-uk.org/doctors/medical_register.asp] Accessed 11 March 2011.
- 8.Postgraduate Medical Education Training Board. National Training Survey 2008/09. [ http://reports.pmetbtrainingsurveys.org/] Accessed 11 March 2011.
- 9.Goldacre MJ, Laxton L, Lambert TW. Medical graduates’ early career choices of specialty and their eventual specialty destinations: UK prospective cohort studies. Br Med J. 2010;340:c3199. doi: 10.1136/bmj.c3199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.NHS Diabetes – Safe use of insulin e-learning course. [ http://www.diabetes.nhs.uk/safe_use_of_insulin/elearning_course/] 2010, Accessed 11 March 2011.
- 11.Lamont L, Cousins D, Hillson R, Bischler A, Terblanche M. Safety alerts: safer administration of insulin: summary of a safety report from the National Patient Safety Agency. Br Med J. 2010;341:c5269. doi: 10.1136/bmj.c5269. [DOI] [PubMed] [Google Scholar]