Abstract
A high pre-injury activity level, the desire of the patient to continue pivoting sports and fear of future give-way episodes are considered the most significant factors affecting the decision to perform anterior cruciate ligament reconstruction. However, since the functional status of the knee at the time of surgery affects the final outcome, assessments of knee function should be considered in the decision making for surgery. Individuals with anterior cruciate ligament injury can be classified as potential copers or non-copers from an existing screening examination. The purpose of this study was to investigate if the functional tests incorporated in the original screening examination could contribute to explain who later go through anterior cruciate ligament reconstruction, and to examine whether changes to the content or the time of conducting the screening examination (before or after ten sessions of exercise therapy) could improve its explanatory value. One-hundred and forty-five individuals were included and prospectively followed for 15 months, after where 51% had gone through anterior cruciate ligament reconstruction and 49% were managed non-operatively. The only significant baseline differences between those who later went through anterior cruciate ligament reconstruction and those who were non-operatively treated were that those who had surgery were younger and had a higher activity level (p<0.05). Regression analyses revealed that the explanatory value for those who later went through anterior cruciate ligament reconstruction significantly improved when the original screening examination was considered compared to only age, activity level and give-way episodes. Changes to the content further improved the explanatory value, with quadriceps muscle strength as the single variable with the highest impact. Finally, conducting the screening examination after ten sessions of progressive exercise therapy gave the overall highest explanatory values, suggesting that the screening examination should be conducted subsequent to a short period of rehabilitation to inform decision making for anterior cruciate ligament reconstruction.
Keywords: Knee injury, ACL, surgery, knee function, functional tests, screening examination
Introduction
Today there is no uniform consensus on the criteria for operative or non-operative management after anterior cruciate ligament (ACL) rupture, and the decision for ACL reconstruction seems to be based more upon expert opinions than evidence from well-designed prospective and randomized controlled trials [30]. In a survey including orthopedic surgeons in the US, the majority stated that give-way episodes and the demands posed in pivoting activities if subjects were to return to their previous activity level were the most significant factors affecting the decision for ACL reconstruction [27]. However, no study has reported if the criteria that surgeons state are in accordance with current clinical practice. Recent evidence suggests that knee function should be examined and considered in the decision making for ACL reconstruction [2,11]. Knee function at the time of surgery has been shown both to be of greater importance for the expected outcome after ACL reconstruction than the time since injury [1,24], and to affect the final outcome [5,8,25,34]. Still, few previous prospective cohort studies have compared functional characteristics in ACL-injured subjects who later go through surgery to those who continue non-operative management. An existing screening examination including functional tests has been developed to classify acute ACL-injured individuals as potential copers or non-copers, based on how they cope with their ACL injury [10]. However, no studies have investigated if this screening examination could also contribute to explain to what regard knee function plays a role in the decision making for ACL reconstruction. Also, it is not known if alterations of the included content or the time of conducting the screening examination can enhance the explanatory value for ACL reconstruction further.
More knowledge on the explanatory value of models for knee function assessments for those who later go through ACL reconstruction and those who do not could contribute to the development of more evidence-based criteria for surgery. The purpose of this study was therefore to investigate to what extent the functional outcome measurements included in the original screening examination could contribute to explain those who later were referred to ACL reconstruction, and to reveal whether alterations to either the content or the time of conduction could improve the explanatory value of the screening examination. We hypothesized that the functional tests comprised in the original screening examination could better explain who went through surgery compared to pre-injury activity level and give-way episodes alone, and that alterations to the content or timing of the original screening examination would enhance the explanatory value for those who later went through surgery further.
Material and Methods
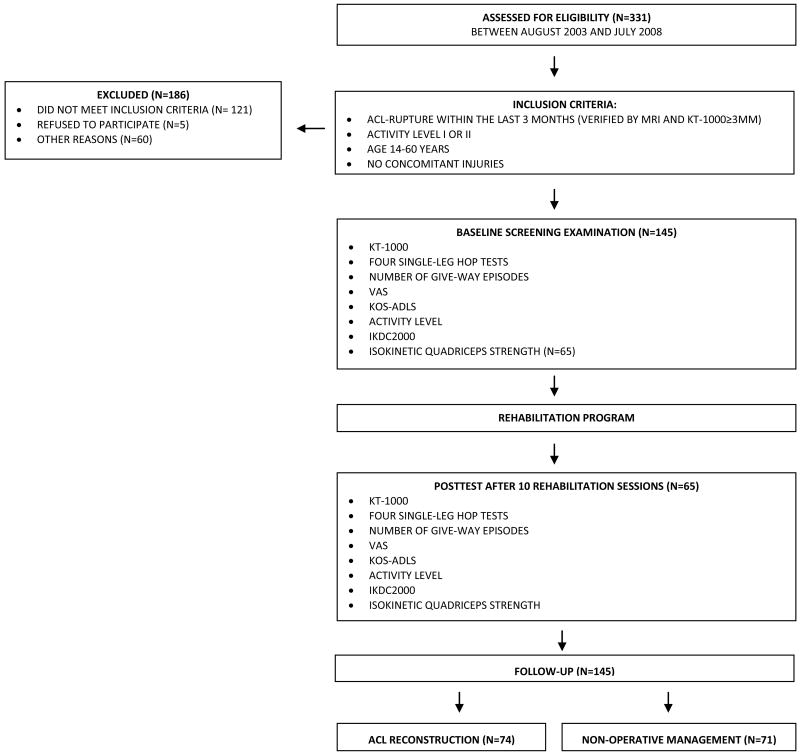
One-hundred and forty-five individuals referred to our outpatient clinic from 2003 to 2008 were included in this study (Figure 1). The inclusion criteria were a complete unilateral rupture of the ACL within the past three months confirmed by magnetic resonance imaging (MRI) and a minimum 3 mm side-to-side difference in knee joint laxity using the KT-1000 knee arthrometer, age between 13 and 60 years and regular participation in pivoting sports at level I or II in accordance with the criteria defined by Hefti et al. [12]. Exclusion criteria were concomitant grade III-IV injury to other ligaments in the index knee, previous injury to the index- or contralateral knee, cartilage lesions affecting subchondral bone, fractures, symptomatic meniscal injury or inability to meet the compliance requirements for participation.
Figure 1. Flowchart of the included subjects and assessments.
The study was approved by the Regional Ethical Committee for Eastern Norway and The Data Inspectorate, and all subjects signed a written informed consent prior to inclusion. The rights of the subjects are protected by the Declaration of Helsinki. All tests in the study were performed by one of the two responsible physical therapists in the study (IE and HM). The original screening examination consists of The Knee Outcome Survey Activities of Daily Living Scale (KOS-ADLS), a global rating of knee function, the number of give-way episodes since the index injury as well as the 6-meter timed hop test (6MTH). The KOS-ADLS includes items related to symptoms and functional abilities during activities of daily living, and the maximum score of 100% means no limitations during daily activities [21]. The subjects' global rating of their knee function was measured on a visual analogue scale (VAS) from 0 to 100 points, where 0 was equivalent to being unable to perform daily activities and 100 to normal knee function [21]. The number of give-way episodes since the injury was registered by self-reporting [10]. Give-way was defined as an episode of knee subluxation during activity [14]. To distinguish between minor episodes of knee buckling and serious give-way episodes, we specified that subluxation events should be followed by pain and effusion for at least 48 hours to be registered. Single-leg hop tests are commonly used in functional assessment after ACL injury and have shown to be a valid and reliable functional performance measurement [7,10,33,35]. The one-leg hop for distance (OLH), the triple cross-over hop for distance (TCH) and the triple hop for distance (TH) were included in our test battery in addition to the 6MTH that is incorporated in the original screening examination. The single-leg hop tests were performed as described by Noyes et al. [31]. No subjects wore a brace when performing the hop tests. In addition to the outcome measures included in the original screening examination and the supplemental hop-tests, we added The International Knee Documentation Committee Subjective Knee Form (IKDC2000) to our test battery. IKDC2000 is a self-evaluation of the impact the injury has on knee function and includes questions related to pain, stiffness, swelling and instability during sports activities, with a highest possible score of 100 points [18-20]. From January 2007, an isokinetic dynamometer (Biodex 6000, Biodex Medical Systems Inc., Shirley, New York) has been to our disposal. Therefore, quadriceps muscle strength assessment was incorporated in the test battery for the subjects included in 2007 and 2008 (n=65). Quadriceps muscle strength performance was evaluated from isokinetic dynamometer measurements of knee extension from 90° flexion to full extension (0°). The angular velocity was 60° per second (60°/sec); which is regarded as an adequate measurement for quadriceps muscle performance after ACL injury [6,13,25]. Peak torque (n-m) was used as the isokinetic muscle strength variable. Because we wanted to investigate the potential importance of changes in the timing of conducting the screening examination, both in general but also in particular when considering quadriceps muscle strength, we included a post-rehabilitation test of the subjects included in 2007 and 2008 when they had completed ten sessions of systematic rehabilitation subsequent to the baseline screening examination. Baseline data were thus collected for 145 subjects, and supplemental post-rehabilitation data for a subgroup of 65 subjects.
Rehabilitation
All subjects went through a pre-screening rehabilitation before the baseline screening examination at our outpatient clinic (Hjelp24 NIMI Ullevaal) to resolve knee impairments. After the baseline screening examination, subjects were enrolled in a progressive exercise therapy program consisting of strength training, plyometrics and neuromuscular exercises. The post-rehabilitation test for subjects included after 2007 (n=65) was performed after ten completed sessions of this rehabilitation program. The ten sessions were completed in no less than four, no more than six weeks after the baseline screening examination. All subjects (n=145) were monitored no less than once a week the first six weeks after the baseline screening examination and no less than once a month for the following four to six months.
Statistical analyses
Mean comparisons at baseline (n=145) and post-rehabilitation (n= 65) between those who later underwent ACL reconstruction and non-operative management were analyzed using independent Student t-tests after confirming estimated normal distribution of data. A Chi-Square test was used for comparison of nominal data (gender, activity level and > 1 give-way episode) between those who underwent ACL reconstruction or non-operative management for all subjects (n=145), and the Fishers' exact test was used for the corresponding analyses at both baseline and the post-rehabilitation test for the subgroup included after January 2007 (n=65). To investigate the explanatory value of both the original version and altered versions of the screening examination for those who later went through surgery, logistic regression analyses were included. ACL reconstruction (yes/no) was the dependent variable for all models. Independent variables in the regression models included age, activity level, give-way episodes, KOS-ADLS, VAS, IKDC2000, 6MTH and isokinetic quadriceps strength index. Thirteen altered models of the screening examination were outlined in addition to the original model; seven models (including the original screening examination) with the outcome measures used at baseline (n=145), and seven models with the outcome measures used at the post-rehabilitation test (n=65). For each of the models, the explanatory value was given as Nagelkerke R-Square. The explanatory value was based on poorer knee function; meaning an increased number of give-way episodes, lower score on self-assessment questionnaires, larger deficits in quadriceps strength and increased time to perform the 6MTH on the injured leg compared to the uninjured. All statistical analyses were conducted using the Statistical Package for Social Sciences version 16.0 (SPSS Inc., Chicago, Illinois). Level of statistical significance was set to p<0.05.
Results
Seventy-six (53%) women and 69 (48%) men with a mean age of 25.9 years (range 14-47 years) were included in the cohort (n=145). Ninety-six (66%) subjects were active at level I and 49 (34%) subjects at level II prior to injury. The mean number of days between injury and the baseline screening examination was 59.8 (range 11-91) days. For those going through ACL reconstruction, the average number of days between injury and surgery was 162.6 (range 48-445) days, and the average number of days between the baseline screening examination and surgery 104.8 (range 3-383) days. Seventy-four (51%) subjects went through ACL reconstruction within 15 months after injury, and 71 (49%) were managed non-operatively. Functional characteristics at baseline and outcome measurements after rehabilitation between those who later went through ACL reconstruction and those who underwent non-operative management are shown in Tables 1, 2 and 3. For all subjects (n=145), those who underwent ACL reconstruction were significantly younger (p=0.009) and a higher number of subjects performed level I-activities (p<0.001). For the subgroup (n=65) with post-rehabilitation tests included, significant differences were also found for gender, in that more females went through non-operative management (p=0.023). All the baseline models (n=145) could significantly distinguish between those who later went through ACL reconstruction and those who did not (p≤0.001-0.005) (Table 4). The simplest model including only age and activity level (model 1) explained 12% of the variance in those who went through surgery. When the number of give-way episodes since injury was added, the explanatory value increased to 15% (model 2). Adding functional tests to the models increased the explanatory value. The model with the highest Nagelkerke R-square at baseline incorporated all the variables included in the original screening examination except VAS, but in addition with IKDC2000 and quadriceps muscle strength. This model explained 43% of the variance in those who later went through surgery (model 7). The single variable with the highest impact on the explanatory value for the baseline models was quadriceps muscle strength.
Table 1. Comparison of subject characteristics and outcome measures at baseline and after rehabilitation for subjects who later went through ACL reconstruction and subjects who went through non-operative management.
| BASELINE (n=145) | POSTTEST (n=65) | |||||
|---|---|---|---|---|---|---|
| NON-OP (n=71) | RECON (n=74) | p-value | NON-OP (n=25) | RECON (n=40) | p-value | |
| Meanˆ(SD) | Meanˆ(SD) | Meanˆ(SD) | Meanˆ(SD) | |||
| Age (years) | 27.9 (8.9) | 24.4 (7.0) | .009 | 28.6 (8.5) | 23.8 (6.7) | .014 |
| KT-1000 (mm difference) | 6.4 (3.3) | 6.3 (2.7) | n.s. | 5.5 (2.2) | 6.2 (2.4) | n.s. |
| KOS-ADLS | 86 (10.6) | 83 (12.4) | n.s. | 89 (8.2) | 86 (9.8) | n.s. |
| VAS | 69 (18.4) | 67 (23.0) | n.s. | 88 (9.8) | 84 (13.1) | n.s. |
| IKDC2000 | 69 (12.7) | 66 (14.3) | n.s. | 81 (8.3) | 77 (11.2) | n.s. |
| Single-leg hop test for distance1 | 87 (10.9) | 89 (12.5) | n.s. | 93 (9.0) | 94 (8.7) | n.s. |
| Triple cross over hop test for distance1 | 88 (11.6) | 87 (15.8) | n.s. | 95 (6.5) | 94 (7.1) | n.s. |
| Triple hop test for distance1 | 87 (10.9) | 87 (14.4) | n.s. | 94 (6.7) | 94 (7.3) | n.s. |
| Six meter timed hop test1 | 91 (9.9) | 90 (15.2) | n.s. | 96 (5.7) | 96 (7.3) | n.s. |
| Quadriceps strength index2* | 89 (10.7) | 90(10.1) | n.s. | 93 (9.5) | 92 (9.8) | n.s. |
NON-OP = Non-operative treatment
RECON = ACL reconstruction
Rounded to nearest integer, except for age and KT-1000 mm. difference
Leg symmetry index (hop performance injured versus uninjured side, %)
Strength index (peak torque injured versus uninjured side, %)
n=65
Table 2. Baseline comparison (Chi-square) of gender, activity level and give-way episodes between subjects who later went through ACL reconstruction and subjects who went through non-operative management (n=145).
| Non-operated (n=71) | Reconstructed (n=74) | p-value | |
|---|---|---|---|
| (n, %) | (n, %) | ||
| Gender (females/males) | 40 (56%) / 31 (44%) | 36 (49%) / 38 (51%) | n.s. |
| Activity level (I/II) | 37 (52%) /34 (48%) | 59 (80%) /15 (20%) | <.001 |
| >1 give-way episodes (yes/no)* | 17 (24%) / 54 (76%) | 19 (26%) / 55 (74%) | n.s. |
> 1 give-way episode between injury and baseline screening
Table 3. Posttest comparison (Fishers' exact test) of gender, activity level and give-way episodes between subjects who later went through and subjects who went through non-operative management (n=65).
| Non-operated (n=25) | Reconstructed (n=40) | p-value | |
|---|---|---|---|
| (n, %) | (n, %) | ||
| Gender (females/males) | 20 (80%) / 5 (20%) | 21 (53%) / 19 (48%) | .023 |
| Activity level (I/II) | 9 (36%) / 16 (64%) | 33 (82%) / 7 (18%) | <.001 |
| > 1 give-way episodes (yes/no)* | 0 (0%) / 25 (100%) | 4 (10%) / 36 (90%) | n.s. |
> 1 give-way episode between baseline and retest
Table 4. Explanatory values of different modified models of the original screening examination for subjects who later went through ACL reconstruction and subjects who went through non-operative management.
| Regression models | Nagelkerke R-squareˆ | p-value | |
|---|---|---|---|
| Baseline screening examination models (n=145) | |||
| 1) | Age, activity level1 | 12 | .001 |
| 2) | Age, activity level1, give-way2 | 15 | <.001 |
| 3) | Age, activity level1, give-way2, KOS-ADLS, VAS, 6MTH* | 23 | <.001 |
| 4) | Age, activity level1, give-way2, IKDC2000, VAS, 6MTH* | 23 | <.001 |
| 5) | Age, activity level1 give-way2, KOS-ADLS, VAS, 6MTH, Quadriceps strength+ | 36 | .005 |
| 6) | Age, activity level1 give-way2, IKDC2000, VAS, 6MTH, Quadriceps strength+ | 41 | .001 |
| 7) | Age, activity level1, give-way2, KOS-ADLS, IKDC2000, 6MTH, Quadriceps strength+ | 43 | .002 |
| Posttest models after ten rehabilitation sessions (n=65) | |||
| 8) | Age, activity level1 | 28 | .001 |
| 9) | Age, activity level, give-way3 | 39 | <.001 |
| 10) | Age, activity level1, give-way3, KOS-ADLS, VAS, 6MTHx | 46 | <.001 |
| 11) | Age, activity level1, give-way3, IKDC2000, VAS, 6MTHx | 47 | <.001 |
| 12) | Age, activity level1, give-way3, KOS-ADLS, VAS, 6MTH, Quadriceps strengthx | 47 | .001 |
| 13) | Age, activity level1, give-way3, IKDC2000, VAS, 6MTH, Quadriceps strengthx | 47 | .001 |
| 14) | Age, activity level1, give-way3, KOS-ADLS, IKDC2000, 6MTH, Quadriceps strengthx | 45 | .001 |
Rounded to nearest integer
Pre-injury activity level
Number of give-way episodes between injury and baseline screening
Number of give-way episodes between injury and posttest
n=137 (8 excluded from model due to missing variables)
n= 63 (2 excluded from model due to missing variables)
n=60 (5 excluded from model due to missing variables)
The post-rehabilitation test models (n=65) could also significantly distinguish between those who later went through ACL reconstruction and those who did not (p≤0.001). In addition, the post-rehabilitation models had higher Nagelkerke R-Squared values (from 28% to 47%) compared to the corresponding baseline models (from 12% to 43%), revealing that performing the functional tests following ten sessions of progressive exercise therapy was superior to performing the screening examination early after injury.
Discussion
The most important finding in the present study was that including functional assessments in the evaluation of knee function after ACL injury increases our ability to explain those who later go through ACL reconstruction and those who continue non-operative management. At the baseline screening examination, ACL-injured subjects who later went through ACL reconstruction did not have poorer knee function compared to those who continued non-operative management when baseline outcome measurement means were compared one by one (Table 1). Still, our first hypothesis was confirmed in that the original screening examination could explain more of the variance in those who later were referred to ACL reconstruction than pre-injury activity level and give-way episodes alone. Thus, poorer test results from the baseline screening examination significantly increased the explanatory value for those who later had surgery. Moreover, changes to the content or timing of the original screening examination was shown to further improve the explanatory value of those who later went through surgery, confirming our second hypothesis. The altered baseline models including the IKDC2000 score and isokinetic quadriceps muscle strength tests were superior to the model containing the original screening examination, and all the post-rehabilitation test models gave superior explanatory values than each of the baseline models. Our overall findings support previous studies arguing that knee function should be emphasized in the treatment decisions after ACL injury [8,23,28,29,32]. Nevertheless, the combination of a high pre-injury activity level and the associated fear that the patient may not be able to maintain the same lifestyle in the future without an increased risk of give-way episodes and additional injuries seems to be the primary rationale when orthopedic surgeons recommend ACL reconstruction [22]. We did find that two thirds of those who later went through ACL reconstruction were active at level I prior to their injury, which is in correspondence to a multi-national survey where a lower pre-injury activity level was identified as the one most significant factor for advising subjects to try non-operative treatment [3]. However, we found no significant differences in the number of give-way episodes between those who went through ACL reconstruction and those who were managed non-operatively; either at baseline or after conduction of a progressive exercise therapy program. At baseline, give-way episodes added only 3% to the explanatory value for those ACL-injured subjects who went through surgery, despite the fact that orthopedic surgeons state that this is a significant factor in the decision to perform ACL reconstruction. Fithian et al. [9] performed a prospective study testing an alternative classification algorithm (the SURF-algorithm), labeling subjects as low, medium or high risk based on previous findings from Daniel et al. [4] that static anterior laxity and pre-injury activity level were the two most important factors for predicting later ACL reconstruction. Moderate or high risk subjects were recommended surgery, whereas low risk subjects were recommended non-operative treatment. We found no significant differences in static anterior laxity between subjects who went through ACL reconstruction and non-operative management (Table 1). Still, all of the subjects in our cohort would have been recommended surgery following the SURF algorithm, solely based on their pre-injury activity level.
The original screening examination is from Hurd et al. [15] suggested to be a better approach to evaluate knee function than solely knee laxity, age and activity level. Our results support this assumption in general. Still, we found that changes in the content of the screening examination improved the explanatory value for those who later went through ACL reconstruction. The single variable with the largest impact on the explanatory value was isokinetic quadriceps muscle strength. All the three models with the highest explanatory value at baseline include quadriceps muscle strength (models 5, 6 and 7, Table 4). The post rehabilitation models incorporating functional tests all revealed higher explanatory values than the corresponding baseline models, with values between 45% and 47% (models 10-14, Table 4). However, if quadriceps muscle strength is incorporated to the baseline models, two of these have almost as high explanatory values as the post rehabilitation models (model 6 and 7, Table 4). Adding the IKDC2000 seems at baseline to raise the explanatory value more than the KOS-ADLS when combined with quadriceps muscle strength. However, after rehabilitation, it does not seem to matter which one of the KOS-ADLS, VAS or IKDC2000 self-reported outcomes are incorporated in the model. Since quadriceps muscle strength deficits have been shown to be of particular importance after ACL injury [5,25,32], especially the observed post-operative persistency of pre-operative weakness [5,8,17], a specific implication drawn from this study is to emphasize incorporation of quadriceps muscle strength assessments in the decision making for surgery.
Conducting functional tests after completion of a short-term rehabilitation program seem from our results to be a better approach than performing the screening examination early after injury. It has been suggested that the functional status of the knee at time of surgery is more important than the time since injury [1,5,8,24,25,34]. Recent practice varies, however, in that some recommend early reconstruction whereas others recommend a period of systematic rehabilitation before the decision for surgery or non-operative treatment is made [2]. At the present time, no clear consensus exist for optimal timing of ACL reconstruction, and evidence can be found in favor of both early and delayed surgery [11]. Swirtun et al. [36] found that subjects who preferred early ACL reconstruction (within 6 months after injury) based this on an assumption that they would have future instability during activity; whereas those who chose later reconstruction did so first after experiencing problems with their knee function. Comparisons of large ACL cohorts from the Multicenter Orthopaedic Outcome Networks (MOON) in the United States (US) and the Norwegian National Knee Ligament Registry (NKLR) has revealed a significant difference in the timing of ACL reconstruction between the US and Norway; with a median time for ACL reconstruction in the MOON-cohort of 2.4 months versus 7.9 months in the NKLR-cohort [26], confirming that early surgery is advocated in the US [16]. Our findings indicate that postponing surgery until post-rehabilitation functional assessments have been conducted may be a reasonable strategy if the functional status of the knee is incorporated in the decision making. However, to investigate the optimal timing for surgery requires prospective studies with long-term follow-up outcomes.
Limitations
A limitation of this study is that only subjects with isolated unilateral ACL ruptures were included. ACL injuries are, however, often accompanied with concomitant injuries to the cartilage, collateral ligaments and menisci [37]. For patients with additional injuries, decision making for ACL reconstruction may be founded on different criteria. Our results must be interpreted within this limitation, and cannot be generalized to ACL-injured subjects with symptomatic concomitant injuries.
We did not ask the subjects at baseline or post-rehabilitation to state what their preferred treatment was and the underlying reasons for their preference. Such data could have added interesting aspects to the study, in enabling us to compare the subjective reasons for preferred treatment stated by the subjects and their knee functional status, as well as including these early subjective statements to the regression analyses for explaining those who later go through surgery and those who do not. A further limitation was that we did not include functional evaluation of the patients preoperatively to see if their knee function had worsened between the post-rehabilitation test and the final decision for ACL reconstruction. The strength of a prospective cohort study design is that it allows us to describe the functional characteristics of the subjects that later go through ACL reconstruction or non-operative management as a natural history of their knee injury and rehabilitation. But, we can from this study not establish criteria for those who can succeed from ACL reconstruction or non-operative management. Future studies following prospective cohorts of ACL- injured subjects for several years are needed to conclude what characterizes those who are able to succeed from ACL reconstruction or non-operative management on a long-term basis.
Conclusion
Including functional assessments based on the screening examination for potential copers and non-copers in the evaluation of knee function after ACL injury increases our ability to explain those who later go through ACL reconstruction and those who continue non-operative management. The one variable with the highest impact for explaining those who later go through ACL reconstruction was quadriceps muscle strength. The results from this study thus suggest that knee function in general, and quadriceps muscle strength assessments in particular, should be accentuated to a larger extent in treatment decisions after ACL injury. It also appears that conducting the functional assessments subsequent to a period of progressive exercise therapy provides more useful information than early after injury to inform surgical decision making.
Acknowledgments
This study received research grants from the South-Eastern Norway Regional Health Authority and NIH grant RO1 HD37985-04, RO1 HD37985-05 and RO1 HD37985-06.
Footnotes
Conflict of interest: The authors declare that they have no conflict of interest.
Contributor Information
Håvard Moksnes, NAR, Norwegian School of Sport Sciences, Hjelp24NIMI and Department of Orthopaedics, Oslo University Hospital, Oslo, Norway.
Lynn Snyder-Mackler, Department of Physical Therapy, University of Delaware, Delaware, US
Lars Engebretsen, Department of Orthopaedics, Oslo University Hospital, Oslo, Norway
May Arna Risberg, NAR, Norwegian School of Sport Sciences, Hjelp24NIMI and Department of Orthopaedics, Oslo University Hospital, Oslo, Norway
References
- 1.Beasley LS, Weiland DE, Vidal AF, Chhabra A, Herzka AS, Feng MT, West RW. Anterior cruciate ligament reconstruction: A literature review of the anatomy, biomechanics, surgical considerations, and clinical outcomes. Oper Tech Orthop. 2005;15:5–19. [Google Scholar]
- 2.Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE. Treatment of anterior cruciate ligament injuries, part I. Am J Sports Med. 2005;33:1579–1602. doi: 10.1177/0363546505279913. [DOI] [PubMed] [Google Scholar]
- 3.Cook C, Nguyen L, Hegedus E, Sandago A, Pietrobon R, Constantinou D, Chuckpaiwong B, Sandhu J, Moorman CT., 3rd Continental variations in preoperative and postoperative management of patients with anterior cruciate ligament repair. Eur J Phys Rehabil Med. 2008;44:253–261. [PubMed] [Google Scholar]
- 4.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22:632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 5.de Jong SN, van Caspel DR, van Haeff MJ, Saris DB. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23:21–28. doi: 10.1016/j.arthro.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 6.Dvir Z. Isokinetics Muscle testing, interpretation and clinical applications. Churchill Livingstone; London: 2004. [Google Scholar]
- 7.Eastlack ME, Axe MJ, Snyder-Mackler L. Laxity, instability, and functional outcome after ACL injury: copers versus noncopers. Med Sci Sports Exerc. 1999;31:210–215. doi: 10.1097/00005768-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Eitzen I, Holm I, Risberg MA. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009;43:371–376. doi: 10.1136/bjsm.2008.057059. [DOI] [PubMed] [Google Scholar]
- 9.Fithian DC, Paxton EW, Stone ML, Luetzow WF, Csintalan RP, Phelan D, Daniel DM. Prospective trial of a treatment algorithm for the management of the anterior cruciate ligament-injured knee. Am J Sports Med. 2005;33:335–346. doi: 10.1177/0363546504269590. [DOI] [PubMed] [Google Scholar]
- 10.Fitzgerald GK, Axe MJ, Snyder-Mackler L. A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2000;8:76–82. doi: 10.1007/s001670050190. [DOI] [PubMed] [Google Scholar]
- 11.Granan LP, Bahr R, Lie SA, Engebretsen L. Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears: a cohort study based on the Norwegian National Knee Ligament Registry. Am J Sports Med. 2009;37:955–961. doi: 10.1177/0363546508330136. [DOI] [PubMed] [Google Scholar]
- 12.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 13.Hole CD, Smit GH, Hammond J, Kumar A, Saxton J, Cochrane T. Dynamic control and conventional strength ratios of the quadriceps and hamstrings in subjects with anterior cruciate ligament deficiency. Ergonomics. 2000;43:1603–1609. doi: 10.1080/001401300750004023. [DOI] [PubMed] [Google Scholar]
- 14.Houck J, Lerner A, Gushue D, Yack HJ. Self-reported giving-way episode during a stepping-down task: case report of a subject with an ACL-deficient knee. J Orthop Sports Phys Ther. 2003;33:273–282. doi: 10.2519/jospt.2003.33.5.273. [DOI] [PubMed] [Google Scholar]
- 15.Hurd WJ, Axe MJ, Snyder-Mackler L. A 10-year prospective trial of a patient management algorithm and screening examination for highly active individuals with anterior cruciate ligament injury: Part 1, outcomes. Am J Sports Med. 2008;36:40–47. doi: 10.1177/0363546507308190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hurd WJ, Axe MJ, Snyder-Mackler L. A 10-year prospective trial of a patient management algorithm and screening examination for highly active individuals with anterior cruciate ligament injury: Part 2, determinants of dynamic knee stability. Am J Sports Med. 2008;36:48–56. doi: 10.1177/0363546507308191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ingersoll CD, Grindstaff TL, Pietrosimone BG, Hart JM. Neuromuscular consequences of anterior cruciate ligament injury. Clin Sports Med. 2008;27:383–404. doi: 10.1016/j.csm.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 18.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29:600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 19.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Neyret P, Richmond JC, Shelbourne KD. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2006;34:1567–1573. doi: 10.1177/0363546506288855. [DOI] [PubMed] [Google Scholar]
- 20.Irrgang JJ, Ho H, Harner CD, Fu FH. Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6:107–114. doi: 10.1007/s001670050082. [DOI] [PubMed] [Google Scholar]
- 21.Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80:1132–1145. doi: 10.2106/00004623-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Kapoor B, Clement DJ, Kirkley A, Maffulli N. Current practice in the management of anterior cruciate ligament injuries in the United Kingdom. Br J Sports Med. 2004;38:542–544. doi: 10.1136/bjsm.2002.002568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keays SL, Bullock-Saxton J, Keays AC. Strength and function before and after anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2000;373:174–183. doi: 10.1097/00003086-200004000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Keays SL, Bullock-Saxton JE, Keays AC, Newcombe PA, Bullock MI. A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and Gracilis tendon graft. Am J Sports Med. 2007;35:729–739. doi: 10.1177/0363546506298277. [DOI] [PubMed] [Google Scholar]
- 25.Keays SL, Bullock-Saxton JE, Newcombe P, Keays AC. The relationship between knee strength and functional stability before and after anterior cruciate ligament reconstruction. J Orthop Res. 2003;21:231–237. doi: 10.1016/S0736-0266(02)00160-2. [DOI] [PubMed] [Google Scholar]
- 26.Magnussen RA, Granan LP, Dunn WR, Amendola A, Andrish JT, Brophy R, Carey JL, Flanigan D, Huston LJ, Jones M, Kaeding CC, McCarty EC, Marx RG, Matava MJ, Parker RD, Vidal A, Wolcott M, Wolf BR, Wright RW, Spindler KP, Engebretsen L. Cross-cultural comparison of patients undergoing ACL reconstruction in the United States and Norway. Knee Surg Sports Traumatol Arthrosc. 2010;18:98–105. doi: 10.1007/s00167-009-0919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marx RG, Jones EC, Angel M, Wickiewicz TL, Warren RF. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19:762–770. doi: 10.1016/s0749-8063(03)00398-0. [DOI] [PubMed] [Google Scholar]
- 28.Moksnes H, Risberg MA. Performance-based functional evaluation of non-operative and operative treatment after anterior cruciate ligament injury. Scand J Med Sci Sports. 2009;19:345–355. doi: 10.1111/j.1600-0838.2008.00816.x. [DOI] [PubMed] [Google Scholar]
- 29.Moksnes H, Snyder-Mackler L, Risberg MA. Individuals with an anterior cruciate ligament-deficient knee classified as noncopers may be candidates for nonsurgical rehabilitation. J Orthop Sports Phys Ther. 2008;38:586–595. doi: 10.2519/jospt.2008.2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Muaidi QI, Nicholson LL, Refshauge KM, Herbert RD, Maher CG. Prognosis of conservatively managed anterior cruciate ligament injury: a systematic review. Sports Med. 2007;37:703–716. doi: 10.2165/00007256-200737080-00004. [DOI] [PubMed] [Google Scholar]
- 31.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 32.Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med. 2008;27:405–424. doi: 10.1016/j.csm.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 33.Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007;87:337–349. doi: 10.2522/ptj.20060143. [DOI] [PubMed] [Google Scholar]
- 34.Shelbourne KD, Klotz C. What I have learned about the ACL: utilizing a progressive rehabilitation scheme to achieve total knee symmetry after anterior cruciate ligament reconstruction. J Orthop Sci. 2006;11:318–325. doi: 10.1007/s00776-006-1007-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Snyder-Mackler L, Fitzgerald GK, Bartolozzi AR, 3rd, Ciccotti MG. The relationship between passive joint laxity and functional outcome after anterior cruciate ligament injury. Am J Sports Med. 1997;25:191–195. doi: 10.1177/036354659702500209. [DOI] [PubMed] [Google Scholar]
- 36.Swirtun LR, Eriksson K, Renstrom P. Who chooses anterior cruciate ligament reconstruction and why? A 2-year prospective study. Scand J Med Sci Sports. 2006;16:441–446. doi: 10.1111/j.1600-0838.2005.00505.x. [DOI] [PubMed] [Google Scholar]
- 37.Trees AH, Howe TE, Grant M, Gray HG. Exercise for treating anterior cruciate ligament injuries in combination with collateral ligament and meniscal damage of the knee in adults. Cochrane Database Syst Rev. 2007;3:CD005961. doi: 10.1002/14651858.CD005961.pub2. [DOI] [PubMed] [Google Scholar]