Abstract
Purpose. To describe the distribution of ocular variables, risk factors, and disease severity in newly diagnosed ocular hypertension (OH) or open-angle glaucoma (OAG). Methods. Eligible subjects underwent a complete history and examination. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) obtained from multiple logistic regression models were used to compare OAG to OH and advanced to early/moderate OAG. Results. 405 subjects were enrolled: 292 (72.1%) with OAG and 113 (27.9%) with OH. 51.7% had early, 27.1% moderate, and 20.9% advanced OAG. The OR for OAG versus OH was 8.19 (P < 0.0001) for disc notch, 5.36 (P < 0.0001) for abnormal visual field, 1.45 (P = 0.001) for worsening mean deviation, 1.91 (P < 0.0001) for increased cupping, 1.03 for increased age (P = 0.030), and 0.36 (P = 0.010) for smoking. Conclusions. Increased age was a risk for OAG, and smoking decreased the risk of OAG compared to OH. Almost half of the OAG subjects had moderate/advanced disease at diagnosis.
1. Introduction
Understanding disease risk factors is important for diagnosis and treatment. Several glaucoma risk factors are known; however, the literature is occasionally conflicting, suggesting that risk factors may vary depending on glaucoma type and stage [1]. Presently, risk factors with strongest evidence for conversion of ocular hypertension (OH) to glaucoma, or presence and progression of open-angle glaucoma (OAG), include older age, thinner central corneal thickness (CCT), greater cup-to-disc ratio (C/D ratio), and higher intraocular pressure (IOP).
Other potential risk factors for the development or progression of OAG include gender [2–4], race [5], body mass index (BMI) [6], myopia [7–11], bilateral disease [12], family history of glaucoma [7, 13–16], hypertension [7, 17–20], hypotension [21–23], smoking [24], thyroid disease [25, 26], migraine [4, 27], Raynaud's disease [28], concomitant medications (including corticosteroids, alpha-blockers, statins) [29–31], asymmetric [32] and diurnal variation in IOP [33], sleep apnea [34], phakic status [35], optic disc size [36], disc hemorrhage [37], pseudoexfoliation [8, 37], and pigment dispersion [38].
The varying results of studies on glaucoma risk factors require further research. We describe the presence and distribution of previously published glaucoma risk factors in patients newly diagnosed with OH or OAG comparing these two groups and analyze the distribution of risk factors in relation to OAG disease severity.
2. Materials and Methods
This was a multicentre, prospective, noninterventional, cross-sectional study registered with http://ClinicalTrials.gov NCT00334750 conducted at 18 Canadian centers in accordance with the Declaration of Helsinki and approved by the ethics committee of each center.
Inclusion criteria included minimum age of 18 years, diagnosed at or within 3 months of the study visit with OH (at least one measurement of IOP ≥ 24 mm Hg and no evidence of glaucomatous damage) or OAG (open angle on gonioscopy and any two of the following: IOP ≥ 21 mmHg, glaucomatous optic neuropathy, and glaucomatous visual field defect), and willing and able to comply with study procedures, and provide written informed consent. Exclusion criteria included subjects previously or currently receiving ocular hypotensive therapy, a history of ocular surgery (except cataract surgery), or ocular trauma.
The study consisted of one visit for each subject; however, some assessments were allowed within one month of enrolment. The following information was collected on standardized data collection sheets: demographics, medical history, ocular family history, and complete ophthalmic examination including visual fields. Ocular data included refraction, best corrected visual acuity, pupil responses, slit-lamp biomicroscopy, and gonioscopy. Diurnal IOP (08:00, 10:00, 12:00, 14:00, and 16:00) was measured with a calibrated Goldmann applanation tonometer. CCT was measured ultrasonically with 3 readings per eye averaged. Dilated fundus examination was performed to assess disc size, C/D ratio, and presence of disc hemorrhage, peripapillary atrophy, and nerve fiber layer defect (NFLD). Optic disc size was classified based on comparing disc area with the target light of a direct ophthalmoscope's smallest aperture. If the disc fits the target it was classified “normal,” if smaller it was classified “small,” and if larger, it was classified “large.” Visual fields were performed using the Humphrey Field Analyzer 24-2 Swedish Interactive Thresholding Algorithm (SITA) Fast (Carl Zeiss Meditec, Dublin, Calif, USA) and included the Glaucoma Hemifield Test (GHT) analysis. Information obtained included mean deviation (MD), pattern standard deviation (PSD), and any abnormalities.
Classification as OH or OAG was determined by the study site. Severity of glaucoma was based on visual field and optic disc examination: advanced (C/D ratio ≥ 0.9 or MD < −12.0 dB or VF defect within 10° of fixation), moderate (C/D ratio 0.65–0.9 or MD −5.0 to −12.0 dB, no VF defect within 10° of fixation), and early (C/D ratio ≤0.65 or MD > −5.0 dB, no VF defect within 10° of fixation) [39].
2.1. Statistical Analysis
All analyses were based on data from a single eye per subject. If both eyes qualified, the eye with the worst disease was included; if equal, the right eye was designated.
Descriptive statistics of demographic characteristics and other potential risk factors for the two conditions (OAG and OH) were provided. To compare differences between the two, mean difference (and SD), 95% CI of the mean difference and P-value were calculated for continuous variables, and odds ratio (OR), 95% CI of odds ratio, and P-value for binary variables.
To assess which risk factors and/or ocular variables were associated with OAG versus OH, adjusted ORs, along with 95% CIs, were obtained from multiple logistic regression models with diagnosis (OAG versus OH) as the response variable and risk factors and/or ocular variables as independent variables. Correlation matrices checked for colinearity between potential risk factors and/or ocular variables within each of 3 classes of variables; highly correlated variables may not have been jointly considered within a model. Potential risk factors were selected based on a stepwise procedure using entry fixed at 5% and stay fixed at 10%. OR and 95% CIs were presented for the selected factors in the final model (also called reduced model).
Additionally, to assess which risk factors and/or ocular variables were associated with severity of OAG, ordinal logistic regression (proportional odds model) was performed, with severity of disease (early, moderate, and advanced) as a response variable and risk factors and/or ocular variables as independent variables. Statistical analysis was performed using SAS version 9.
3. Results
410 subjects were enrolled. Information regarding diagnosis was available for 405 subjects who were analyzed. Overall, 404 (98.5%) subjects completed the study and 6 (1.5%) subjects discontinued.
292 (72.1%) of 405 subjects were diagnosed with OAG and 113 (27.9%) with OH. In OAG most had primary open-angle glaucoma (POAG, 202/292, 69.2%). Other diagnoses included normal tension glaucoma (65/292, 22.3%), pseudoexfoliation (16/292, 5.5%), and pigmentary glaucoma (9/292, 3.1%). 151 (51.7%) of 292 subjects had early OAG at diagnosis; a similar percent had moderate or advanced OAG: 79/292 (27.1%) and 61/292 (20.9%), respectively. Overall 60.5% of subjects (245/405) had symmetrical disease compared with 39.5% (160/405) with asymmetrical disease. A higher percentage of subjects with OH had symmetrical findings (73.5%) than subjects with OAG (55.5%).
Table 1 summarizes the demographic characteristics. Subjects with newly diagnosed OAG were significantly older than those with OH (63.0 ± 13.0 years for OAG and 56.5 ± 12.6 for OH, P < 0.0001). The distribution of male (145 OAG versus 59 OH) and female (147 OAG versus 54 OH) subjects was similar within the groups. The majority of subjects were Caucasian (348/405; 85.9%) and the proportion of Caucasian subjects was greater in OH, P = 0.013. Mean weight and BMI were both greater in OH, P = 0.004 and 0.001, respectively.
Table 1.
Demographic characteristics.
| Characteristic | OAG (n = 292) | OH (n = 113) | P-valuea |
|---|---|---|---|
| Age groups, n (%) | 0.001 | ||
| 18–44 years | 22 (7.5) | 15 (13.3) | |
| 45–64 years | 137 (46.9) | 70 (61.9) | |
| ≥65 years | 133 (45.5) | 28 (24.8) | |
|
| |||
| Age, year, Mean ± SD | 63.0 ± 13.0 | 56.5 ± 12.6 | <0.0001 |
| (Range) | (22–89) | (21–91) | |
|
| |||
| Male/female, n (%) | 145 (49.7)/147 (50.3) | 59 (52.2)/54 (47.8) | 0.645 |
|
| |||
| Race, n (%) | 0.013 | ||
| Caucasian | 241 (82.5) | 107 (94.7) | |
| Black | 18 (6.2) | 1 (0.9) | |
| Asian | 26 (8.9) | 3 (2.7) | |
| Other | 7 (2.4) | 2 (1.8) | |
|
| |||
| Weight, mean ± SD (kg) | 74.8 ± 15.6 | 80.9 ± 19.6 | 0.004 |
|
| |||
| Height, mean ± SD (cm) | 168.0 ± 10.6 | 167.9 ± 9.1 | 0.937 |
|
| |||
| BMI, Mean ± SD (kg/m2) | 26.5 ± 5.0 | 28.6 ± 6.0 | 0.001 |
|
| |||
| Location, n (%) | 0.015 | ||
| Ontario | 118 (40.4) | 34 (30.1) | |
| Quebec/atlantic | 97 (33.2) | 55 (48.7) | |
| Western | 77 (26.4) | 24 (21.2) | |
Abbreviations: BMI: body mass index; n: number of subjects; OAG: open-angle glaucoma; OH: ocular hypertension; SD: standard deviation.
aSignificance of differences between the OAG and OH groups was tested using the chi-square test for categorical data and the t-test for continuous data.
Table 2 summarizes the ocular examination results and Table 3 the optic nerve assessment. The OAG subjects had lower mean IOP, thinner CCT, and greater degree of myopia than OH subjects. 6.2% of the OAG subjects had a relative afferent pupillary defect (RAPD) compared to none in OH subjects, P = 0.005. For the optic nerve characteristics evaluated, more OAG subjects had abnormalities than OH. The mean C/D ratio was 0.7 ± 0.2 in OAG and 0.4 ± 0.2 in OH, P < 0.0001. There were more large discs in OAG (13.7%) compared to OH (6.2%), P = 0.035.
Table 2.
Summary of ocular examination findings.
| Variable | OAG | OH | Mean Differencea | P-valueb |
|---|---|---|---|---|
| N = 292 | N = 113 | (95% CI) | ||
| Mean Intraocular pressure ±SD, mmHgc | 20.5 ± 5.2 | 23.4 ± 3.3 | −2.9 (−3.7, −2.0) | <0.0001 |
| Mean central corneal thickness ±SD, micronsd | 554.2 ± 38.2 | 583.4 ± 34.6 | −29.1 (−36.9, −21.4) | <0.0001 |
| Mean visual acuity ±SD, LogMAR | 0.2 ± 0.2 | 0.1 ± 0.2 | 0.1 (0.0, 0.1) | <0.001 |
| Mean spherical equivalence ± SD, diopterse | −1.3 ± 3.3 | −0.6 ± 2.5 | −0.7 (−1.3, −0.0) | 0.038 |
| Abnormal anterior segment examination, n (%)f | 19 (6.5) | 10 (8.9) | 0.7 (0.3, 1.6) | 0.404 |
| Presence of relative afferent pupillary defect, n (%)f | 18 (6.2) | 0 (0.0) | Infinite (Infinite) | 0.005 |
| Myopia, n (%)g | 135 (46.2) | 46 (40.7) | 1.3 (0.8, 1.9) | 0.316 |
Abbreviations: CI: confidence interval; LogMAR: logarithm of the minimum angle of resolution; n: number of subjects; OAG: open-angle glaucoma; OH: ocular hypertension; SD: standard deviation.
aMean difference calculated as OAG−OH.
bSignificance of differences between the OAG and OH groups was tested using the chi-square test for categorical data and the t-test for continuous data. Fisher's exact test was used for categorical data when the expected marginal size was <5.
cMissing data for 1 subject in the OH group.
dMissing data for 1 subject in the OAG group.
e n = 266 in the OAG and n = 100 in the OH group.
fMissing data for 1 subject in both the OAG and OH groups.
gData concerning myopia were collected under medical history.
Table 3.
Summary of optic nerve head examination findings.
| Variable | OAG | OH | Mean differencea | P-valueb |
|---|---|---|---|---|
| N = 292 | N = 113 | (95% CI) | ||
| Mean C/D ratioc ± SD | 0.7 ± 0.2 | 0.4 ± 0.2 | 0.3 (0.3, 0.3) | <0.0001 |
| Localized notch or thinning of the neuroretinal rim, n (%)d | 191 (65.4) | 6 (5.4) | 33.3 (14.2, 78.7) | <0.0001 |
| Presence of nerve fiber layer defect, n (%)d | 55 (18.8) | 0 (0.0) | Infinite (Infinite) | <0.0001 |
| Presence of peripapillary atrophy, n (%)d | 115 (39.4) | 17 (15.2) | 3.6 (2.1, 6.4) | <0.0001 |
| Presence of optic disc hemorrhage, n (%)d | 15 (5.1) | 1 (0.9) | 6.0 (0.8, 46.1) | 0.082 |
| Diffuse or localized area of pallor, n (%)d | 17 (5.8) | 0 (0.0) | Infinite (Infinite) | 0.005 |
| Large disc size, n (%) | 40 (13.7) | 7 (6.2) | 2.4 (1.0, 5.5) | 0.035 |
Abbreviations: C/D: cup-to-disc; CI: confidence interval; n: number of subjects; OAG: open-angle glaucoma; OH: ocular hypertension; SD: standard deviation.
aMean differences calculated as OAG-OH.
bSignificance of differences between the OAG and OH groups was tested using the chi-square test for categorical data and the t-test for continuous data. Fisher's exact test was used for categorical data when the expected marginal size was <5.
cC/D ratio: mean of horizontal and vertical C/D ratios; if 1 of 2 was missing, the nonmissing value was used as the average.
dMissing data for 1 subject in the OH group.
Table 4 summarizes the VF results. For each measurement, the median was approximately double or higher for the OAG subjects; however, the 95% CIs were significantly different for only MD, PSD, and false negative rate, and there was a trend towards significance for fixation losses with P = 0.058.
Table 4.
Summary of the Humphrey visual field test findings.
| Variable | OAG | OH | Mean differencea | P-valueb |
|---|---|---|---|---|
| N = 292 | N = 113 | (95% CI) | ||
| Mean fixation losses ± SDc | 9.3 ± 13.2 | 7.0 ± 9.6 | 2.3 (−0.1, 4.6) | 0.058 |
| Mean false positive rate ± SD | 3.6 ± 5.9 | 4.3 ± 6.3 | −0.71 (−2.1, 0.6) | 0.299 |
| Mean false negative rate ± SD | 4.6 ± 6.7 | 1.9 ± 4.1 | 2.7 (1.6, 3.8) | <0.0001 |
| Mean of mean deviation ± SD | −4.6 ± 5.7 | −0.4 ± 1.6 | −4.1 (−4.8, −3.4) | <0.0001 |
| Mean pattern standard deviation ± SD | 4.4 ± 3.6 | 1.7 ± 0.8 | 2.7 (2.3, 3.1) | <0.0001 |
| Visual field unreliable, n (%) | 43 (14.7) | 16 (14.2) | 1.0 (0.6, 1.9) | 0.885 |
| Presence of artifacts, n (%)c | 10 (3.4) | 5 (4.5) | 0.8 (0.3, 2.3) | 0.625 |
| Abnormal visual field overall, n (%)c | 181 (62.2) | 13 (11.6) | 12.5 (6.7, 23.4) | <0.0001 |
| Within 10° of fixation, n (%)d | 134 (45.9) | 27 (24.1) | 2.7 (1.6, 4.4) | <0.0001 |
| Glaucoma hemifield test outside normal limits, n (%)e | 166 (59.1) | 14 (13.0) | 9.7 (5.3, 17.8) | <0.0001 |
Abbreviations: CI: confidence interval; n: number of subjects; OAG: open-angle glaucoma; OH: ocular hypertension; SD: standard deviation.
aMean difference calculated as OAG − OH.
bSignificance of differences between the OAG and OH groups was tested using the chi-square test for categorical data and the t-test for continuous data. Fisher's exact test was used for categorical data when the expected marginal size was <5.
cMissing data for 1 subject in both the OAG and OH groups.
dMissing data for 1 subject in the OH group.
e n: 281 in the OAG and n: 108 in the OH group.
The majority of subjects in both OAG and OH groups had no family history of glaucoma (62.0%) or elevated IOP (87.9%). Subjects with OH reported less frequent family history of blindness (3.5%) than subjects with OAG (11.0%), P = 0.019. Overall, 45.1% of subjects with OH reported a family history of glaucoma, elevated IOP, or blindness compared with 42.1% of subjects with OAG.
Table 5 summarizes glaucoma risk factors by subjects' medical histories; past or current histories were classified as “yes.” The most frequently reported medical histories for the OAG and OH groups, respectively, were vascular dysfunction (43.8% and 32.7%), smoking (29.5% and 46.9%), and hypercholesterolemia (31.8% and 27.4%). There were no significant differences between the groups for all medical conditions evaluated except vascular dysfunction and smoking with P-values of 0.042 and 0.001, respectively.
Table 5.
Summary of medical history, n (%).
| Medical history (past or current) | OAG | OH | Odds ratio | P-valuea |
|---|---|---|---|---|
| N = 292 | N = 113 | (95% CI) | ||
| Vascular dysfunction | 128 (43.8) | 37 (32.7) | 1.6 (1.0, 2.5) | 0.042 |
| Hypercholestero- lemia | 93 (31.8) | 31 (27.4) | 1.2 (0.8, 2.0) | 0.387 |
| Smoking | 86 (29.5) | 53 (46.9) | 0.5 (0.3, 0.7) | 0.001 |
| Migraine | 37 (12.7) | 16 (14.2) | 0.9 (0.5, 1.7) | 0.690 |
| Thyroid disease | 34 (11.6) | 15 (13.3) | 0.9 (0.4, 1.7) | 0.652 |
| Diabetes mellitus | 32 (11.0) | 17 (15.0) | 0.7 (0.4, 1.3) | 0.258 |
| Pseudoexfoliation syndrome | 19 (6.5) | 3 (2.7) | 2.6 (0.7, 8.8) | 0.148 |
| Raynaud's disease | 15 (5.1) | 5 (4.4) | 1.2 (0.4, 3.3) | 0.767 |
| Pigment dispersion syndrome | 12 (4.1) | 6 (5.3) | 0.8 (0.3, 2.1) | 0.599 |
| Sleep apnea | 9 (3.1) | 7 (6.2) | 0.5 (0.2, 1.3) | 0.149 |
Abbreviations: CI = confidence interval; n = number of subjects; OAG = open-angle glaucoma; OH = ocular hypertension.
aSignificance of differences between the OAG and OH groups was tested using the chi-square test; Fisher's exact test was used when the expected marginal size was <5.
The medication most frequently taken was statins, reported by 83 (28.4%; 95% CI: 23.32–33.97) of 292 OAG subjects and 23 (20.4%; 95% CI: 13.49–29.20) of 113 OH subjects. There were no significant differences between OAG and OH subjects for any concomitant medication including statins, corticosteroids, or alpha blockers.
Figure 1 shows which risk factors and ocular variables were significantly associated with diagnosis (OAG versus OH) in the reduced model. The predicted odds ratio of OAG for localized notch or thinning of neuroretinal rim was 8.19; subjects with these factors were 8.19 times more likely to have OAG than OH (95% CI: 2.93–22.88; P < 0.0001). Subjects who smoked had 0.36 times the odds of having OAG than OH (95% CI: 0.17–0.78; P = 0.010). Additional significant risk factors were age (OR 1.03; 95% CI 1.00–1.06; P = 0.030) per year increase, C/D ratio (OR 1.91; 95% CI: 1.54–2.37; P < 0.0001) per 0.1 unit increase, MD (OR 1.45; 95% CI 1.17–1.80; P = 0.001) per 1 dB decrease, and abnormal VF (OR 5.36; 95% CI: 2.12–13.56; P < 0.0001).
Figure 1.
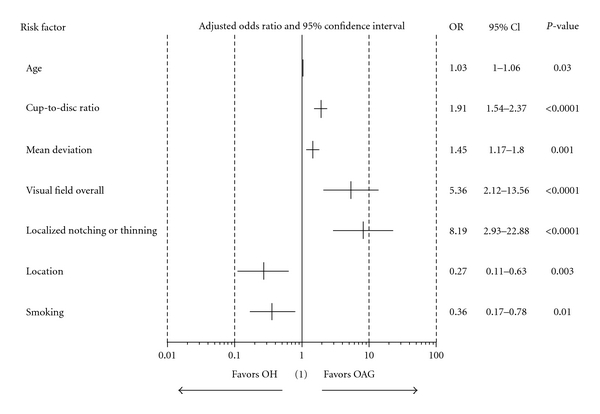
Association of primary diagnosis versus risk factors (reduced model). (i) Primary diagnosis: OAG versus OH. (ii) Age, cup-to-disc ratio, and mean deviation are continuous variables, and the others are categorical. Age was estimated in every one-year increment, cup-to-disc ratio in every 0.1-unit increment, and mean deviation in every 1 dB unit of worsening. Categorical variables were estimated as follows: visual field overall (abnormal versus normal, localized notching/thinning (Yes versus No), location (Quebec/Atlantic versus Ontario), smoking (Yes versus No). (iii) Odds ratio, 95% confidence interval. (1) OR = 1 implies a specific risk factor is equally likely in both OAG and OH groups, OR >1 implies more likely in OAG, and OR < 1 implies more likely in OH.
Figure 2 shows which factors were associated with advanced versus early or moderate OAG. Subjects with diffuse or localized areas of pallor had over 5 times the odds as subjects without pallor of having advanced OAG (95% CI: 1.27–21.10; P = 0.022) at diagnosis. Additional significant factors included worse MD (OR 1.25; 95% CI: 1.17–1.33; P < 0.0001), NFLD (OR 2.60; 95% CI: 1.30–5.19, P = 0.007), localized notch or rim thinning (OR 2.08; 95% CI: 1.12–3.86; P = 0.021), presence of peripapillary atrophy (OR 2.66; 95% CI: 1.51–4.69; P = 0.001), abnormal VF (OR 6.40; 95% CI: 3.15–12.99; P < 0.0001), and presence of smoking (OR 1.89, 95% CI: 1.05–3.41; P = 0.034).
Figure 2.
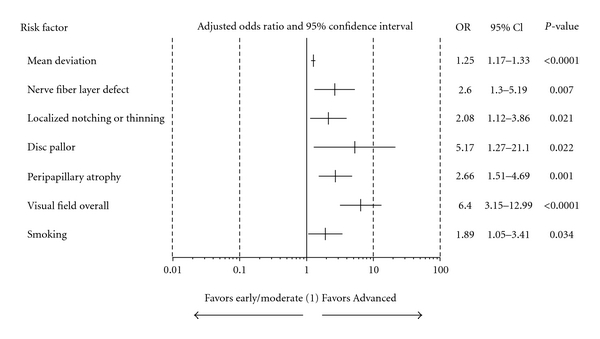
Association of severity of OAG versus risk factors (reduced model). (i) severity of OAG. Advanced disease versus early or moderate disease. (ii) Mean deviation (MD) is a continuous variable, and the others are categorical. MD was estimated in every 1 dB unit of worsening. Categorical variables were estimated as follows: nerve fiber layer defect, localized notching/thinning, disc pallor, peripapillary atrophy, smoking (Yes versus No) and visual field overall (abnormal versus normal). (1) OR = 1 implies a specific risk factor is equally likely in both severity levels, OR > 1 implies more likely in advanced, and OR < 1 implies more likely in early/moderate.
4. Discussion
Understanding glaucoma risk factors can aid diagnosis and influence management decisions, including when to treat, aggressiveness of treatment, and potentially developing new treatment strategies. Our understanding of risk factors continues to evolve as the literature increases; however, publications have occasionally been conflicting thus underlining the importance of continued studies. Some confusion may relate to different study populations; for example, risk factors for the conversion of OH to OAG may differ from those for incident OAG. Similarly, risk factors for progression of OAG as well as for stages of glaucoma, and for geographic or ethnic groups, may vary. Our study was designed to describe the distribution of glaucoma risk factors in subjects with newly diagnosed treatment-naïve OH and OAG. A comparison between OH and OAG groups provided OR for each factor. Finally, risk factors were further analysed to determine an association with disease severity.
We found that optic disc characteristics such as increased C/D ratio, localized notching or thinning, NFLD, peripapillary atrophy, pallor, and disc hemorrhage were more common in OAG than OH. VF features such as increased MD, PSD, and GHT outside normal limits, defects within 10 degrees of fixation, and false negative rate were all greater in OAG. These results are expected as optic disc, and VF features are used to diagnose disease and likely should not be considered as risk factors per se. However, since most of these ocular variables lack a clear distinction between definitive glaucoma and normal (e.g., there is no cutoff for C/D ratio or MD to diagnose glaucoma), these were included in the analysis.
A total of 11.6% (13/112) of the OH subjects' VFs were abnormal with 13% having a GHT outside normal limits and 24.1% with a defect within 10 degrees of fixation. These abnormal VFs were not felt to be glaucomatous and may represent artifact or other pathology such as age-related macular changes, and these subjects were not classified as having OAG. Other ocular features more common in OAG were worse acuity, presence of a RAPD, thinner CCT, and myopia. In the final multiple regression analysis, the only ocular variables that remained significant included increased C/D ratio, worse MD, abnormal VF, and localized notch or thinning.
Thinner CCT has previously been considered a risk factor for both conversion of OH to OAG [2] and for the presence of OAG [40–43]. In this study OAG had significantly thinner CCT compared to OH (554.2 ± 38.2 μm versus 583.4 ± 34.6 μm, resp.), P < 0.0001; in the univariate analysis, however, CCT was not significant in the regression model.
IOP has consistently been recognized as a glaucoma risk factor including both the mean level [2, 12, 14, 21, 30, 44–47] and degree of fluctuation [33, 47]. In our study, mean IOP was higher in OH as compared to OAG, 23.4 ± 3.3 mmHg versus 20.5 ± 5.2 mmHg, respectively (P < 0.0001). This difference is explained both by the definition of OH (at least one IOP measurement of ≥24 mmHg) and the frequency of normal-tension glaucoma (65/292, 22.3%) in OAG.
Evaluation of nonocular variables found the following significant differences between the groups: younger age (56.5 ± 12.6 versus 63.0 ± 13.0, P < 0.0001), greater proportion of Caucasian subjects (94.7% versus 82.5%. P = 0.013), higher weight (80.9 ± 19.6 versus 74.8 ± 15.6 kg, P = 0.004), greater BMI (28.6 ± 6.0 versus 26.5 ± 5.0 kg/m2, P = 0.001), and higher frequency of smoking history (46.9% versus 29.5%, P = 0.001) in the OH versus OAG group, respectively. Of these, only age and smoking were significant in the final multiple regression analysis.
Age is a recognized risk factor for glaucoma [48–51]. The results for smoking are controversial. We found that a history of smoking (past or current) was protective with an odds ratio of 0.36 (P = 0.010) for OAG versus OH. Cigarette smoking is linked to many diseases including cataracts [52] and macular degeneration [53]. Epidemiological studies have also found a negative correlation between smoking and the development of neurodegenerative disorders such as Parkinson's, and in some studies, Alzheimer's disease [54]. One large prevalence survey found no association between smoking and POAG [55]. Finally, for concomitant medications it has previously been suggested that statin use may be protective for OAG [31]. Statin use in our study was not significant in the univariate or final multiple regression analysis.
Study location was significant in both the univariate and final multiple regression model when comparing Quebec/Atlantic region to Ontario but was not significant for comparisons including the Western region. The diagnosis of OH occurred more frequently in Quebec/Atlantic region than Ontario (48.7% versus 30.1%, resp.), and the diagnosis of OAG was more frequent in Ontario than Quebec/Atlantic region (40.4% versus 33.2%, resp.), P = 0.015. In the final multiple regression model, the OR of OAG versus OH was 0.27 (95% CI 0.11–0.63) for Quebec/Atlantic region versus Ontario. The significance of this finding is unclear, and further study of this is warranted.
We evaluated OAG by severity of disease at diagnosis using the definition of Damji et al. [39]. Almost half the subjects with OAG presented with moderate or advanced disease at diagnosis. Evaluation of various risk factors using logistic regression analysis found the presence of a NFLD, optic disc pallor, peripapillary atrophy, localized notch or rim thinning, and smoking to be significant in addition to variables associated with the definition of severity (MD and abnormal VF). It is interesting that smoking was a risk factor for OH when compared to OAG; however, within the OAG group, a history of smoking was a significant risk factor for advanced disease. This seemingly conflicting result deserves further study. Possibly our definition of smoking, with “yes” defined as a previous or current history of smoking, is obscuring the results. Perhaps a definition of smoking including duration and number of cigarettes per day might provide a different conclusion.
There are limitations to our study. Firstly, many of the ocular variables studied are used in the definition of OAG and likely should not be considered risk factors per se; however, these are often reported, and given the lack of a clear distinction between disease and no disease for most of these variables, we included them in the analysis. Secondly, self-reported risk factors including family and medical history may be unreliable. Finally, there may be selection bias as this study relied on the diagnosis of OAG and OH from the study site. To minimize this optic disc, visual field reading centers were responsible for independently verifying results.
5. Conclusions
In summary, we evaluated the distribution of previously published risk factors for glaucoma in subjects with newly diagnosed OH or OAG. In addition, within OAG, we evaluated risk factors in terms of disease severity. Logistic regression analysis determined several factors to be significantly associated with OH or OAG and severity of OAG. An interesting result was a history of smoking, which seemed to be protective for OAG versus OH; however, within OAG, it was a significant risk factor for advanced disease at presentation. In addition, subjects with advanced versus early or moderate OAG, the presence of a NFLD, optic disc pallor, peripapillary atrophy, and localized notch or rim thinning were all associated with advanced disease (OR 2.60, 5.17, 2.66, 2.08, resp.). Finally, we found that nearly 50% of subjects with OAG presented with moderate or advanced disease at initial diagnosis. This finding alone supports the importance of further studies regarding risk factors to assist in earlier diagnosis of glaucoma.
Acknowledgments
The research was supported by Pfizer Canada Inc., Kirkland, Québec, Canada. Participating Centers in the Canadian Glaucoma Risk Factor Study Group include the following. (i) British Columbia: Robert L. G. Piemontesi MD Nanaimo, Briar Sexton MD Vancouver. (ii) Alberta: Andrew Crichton MD Calgary, Marianne E. Edwards MD Edmonton, and Jitendra Gohill MD Calgary Ophthalmology Center, Calgary. (iii) Manitoba: Lisa F Gould MD Winnipeg Clinic, Winnipeg. (iv) Saskatchewan: Paul H. Murphy MD Saskatoon. (v) Ontario: Iqbal K. Ahmed MD Credit Valley Eyecare, Credit Valley, Robert Amy MD Oakville Trafalgar Hospital, Oakville, Catherine M. Birt MD, Sunnybrook Health Sciences Centre, Toronto, Yvonne M. Buys MD, FRCSC University Health Network, Toronto, Michael M Henry MD Toronto, Khalid Hasanee MD Oakville Eye Associates, Oakville, and Cindy LM Hutnik MD PhD, Ivey Institute, London, Delan Jinapryia MD Hotel Dieu, Queen's University, Kingston. (vi) Quebec: Pierre Blondeau MD Sherbrooke, Mark R Lesk MD Hopital Maisonneuve-Rosemont, Montreal, and Paul Harasymowycz MD Institut de glaucome de Montreal, Montreal. (vii) Nova Scotia: Monica Carrillo MD Sydney. The authors also wish to thank Dr. Duo Zhou for providing extensive statistical assistance and Dr. Sophia Calmels for her involvement in trial design.
References
- 1.Friedman DS, Wilson MR, Liebmann JM, Fechtner RD, Weinreb RN. An evidence-based assessment of risk factors for the progression of ocular hypertension and glaucoma. American Journal of Ophthalmology. 2004;138(3):S19–S31. doi: 10.1016/j.ajo.2004.04.058. [DOI] [PubMed] [Google Scholar]
- 2.Gordon MO, Beiser JA, Brandt JD, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Archives of Ophthalmology. 2002;120(6):714–720. doi: 10.1001/archopht.120.6.714. [DOI] [PubMed] [Google Scholar]
- 3.Blackwell B, Gaasterland D, Ederer F, et al. The Advanced Glaucoma Intervention Study (AGIS): 12. Baseline risk factors for sustained loss of visual field and visual acuity in patients with advanced glaucoma. American Journal of Ophthalmology. 2002;134(4):499–512. doi: 10.1016/s0002-9394(02)01659-8. [DOI] [PubMed] [Google Scholar]
- 4.Drange S, Anderson DR, Schulzer M. Risk factors for progression of visual field abnormalities in normal-tension glaucoma. American Journal of Ophthalmology. 2001;131(6):699–708. doi: 10.1016/s0002-9394(01)00964-3. [DOI] [PubMed] [Google Scholar]
- 5.Girkin CA. Primary open-angle glaucoma in African Americans. International Ophthalmology Clinics. 2004;44(2):43–60. doi: 10.1097/00004397-200404420-00006. [DOI] [PubMed] [Google Scholar]
- 6.Klein BEK, Klein R, Linton KLP. Intraocular pressure in an American community: the Beaver Dam Eye Study. Investigative Ophthalmology and Visual Science. 1992;33(7):2224–2228. [PubMed] [Google Scholar]
- 7.Georgopoulos G, Andreanos D, Liokis N, Papakonstantinou D, Vergados J, Theodossiadis G. Risk factors in ocular hypertension. European Journal of Ophthalmology. 1997;7(4):357–363. doi: 10.1177/112067219700700409. [DOI] [PubMed] [Google Scholar]
- 8.Mitchell P, Wang JJ, Hourihan F. The relationship between glaucoma and pseudoexfoliation: the blue mountains eye study. Archives of Ophthalmology. 1999;117(10):1319–1324. doi: 10.1001/archopht.117.10.1319. [DOI] [PubMed] [Google Scholar]
- 9.Chihara E, Liu X, Dong J, et al. Severe myopia as a risk factor for progressive visual field loss in primary open-angle glaucoma. Ophthalmologica. 1997;211(2):66–71. doi: 10.1159/000310760. [DOI] [PubMed] [Google Scholar]
- 10.Perkins ES, Phelps CD. Open angle glaucoma, ocular hypertension, low-tension glaucoma, and refraction. Archives of Ophthalmology. 1982;100(9):1464–1467. doi: 10.1001/archopht.1982.01030040442015. [DOI] [PubMed] [Google Scholar]
- 11.Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: the blue mountains eye study. Ophthalmology. 1999;106(10):2010–2015. doi: 10.1016/s0161-6420(99)90416-5. [DOI] [PubMed] [Google Scholar]
- 12.Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E. Factors for glaucoma progression and the effect of treatment: the Early Manifest Glaucoma Trial. Archives of Ophthalmology. 2003;121(1):48–56. doi: 10.1001/archopht.121.1.48. [DOI] [PubMed] [Google Scholar]
- 13.Peeters H, Debeer Ph, Groenen P, et al. Inheritance of open-angle glaucoma in the Barbados family study. American Journal of Medical Genetics. 2001;103(1):36–43. doi: 10.1002/ajmg.1498. [DOI] [PubMed] [Google Scholar]
- 14.Landers J, Goldberg I, Graham SL. Analysis of risk factors that may be associated with progression from ocular hypertension to primary open angle glaucoma. Clinical and Experimental Ophthalmology. 2002;30(4):242–247. doi: 10.1046/j.1442-9071.2002.00528.x. [DOI] [PubMed] [Google Scholar]
- 15.Klein BEK, Klein R, Lee KE. Heritability of risk factors for primary open-angle glaucoma: The Beaver Dam Eye Study. Investigative Ophthalmology and Visual Science. 2004;45(1):59–62. doi: 10.1167/iovs.03-0516. [DOI] [PubMed] [Google Scholar]
- 16.Wolfs RCW, Klaver CCW, Ramrattan RS, Van Duijn CM, Hofman A, De Jong PTVM. Genetic risk of primary open-angle glaucoma: population-based familial aggregation study. Archives of Ophthalmology. 1998;116(12):1640–1645. doi: 10.1001/archopht.116.12.1640. [DOI] [PubMed] [Google Scholar]
- 17.Klein BEK, Klein R, Knudtson MD. Intraocular pressure and systemic blood pressure: longitudinal perspective: the Beaver Dam Eye Study. British Journal of Ophthalmology. 2005;89(3):284–287. doi: 10.1136/bjo.2004.048710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mitchell P, Lee AJ, Rochtchina E, Wang JJ. Open-angle glaucoma and systemic hypertension: the Blue Mountains Eye Study. Journal of Glaucoma. 2004;13(4):319–326. doi: 10.1097/00061198-200408000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Bonomi L, Marchini G, Marraffa M, Bernardi P, Morbio R, Varotto A. Vascular risk factors for primary open angle glaucoma: the Egna-Neumarkt Study. Ophthalmology. 2000;107(7):1287–1293. doi: 10.1016/s0161-6420(00)00138-x. [DOI] [PubMed] [Google Scholar]
- 20.Langman MJS, Lancashire RJ, Cheng KK, Stewart PM. Systemic hypertension and glaucoma: mechanisms in common and co-occurrence. British Journal of Ophthalmology. 2005;89(8):960–963. doi: 10.1136/bjo.2004.053397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leske MC, Wu S-Y, Nemesure B, Hennis A. Incident open-angle glaucoma and blood pressure. Archives of Ophthalmology. 2002;120(7):954–959. doi: 10.1001/archopht.120.7.954. [DOI] [PubMed] [Google Scholar]
- 22.Graham SL, Drance SM. Nocturnal hypotension: role in glaucoma progression. Survey of Ophthalmology. 1999;43(6):S10–S16. doi: 10.1016/s0039-6257(99)00016-8. [DOI] [PubMed] [Google Scholar]
- 23.Pache M, Dubler B, Flammer J. Peripheral vasospasm and nocturnal blood pressure dipping—two distinct risk factors for glaucomatous damage? European Journal of Ophthalmology. 2003;13(3):260–265. doi: 10.1177/112067210301300304. [DOI] [PubMed] [Google Scholar]
- 24.Bonovas S, Filioussi K, Tsantes A, Peponis V. Epidemiological association between cigarette smoking and primary open-angle glaucoma: a meta-analysis. Public Health. 2004;118(4):256–261. doi: 10.1016/j.puhe.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 25.Girkin CA, McGwin G, Jr., McNeal SF, Lee PP, Owsley C. Hypothyroidism and the development of open-angle glaucoma in a male population. Ophthalmology. 2004;111(9):1649–1652. doi: 10.1016/j.ophtha.2004.05.026. [DOI] [PubMed] [Google Scholar]
- 26.Lee AJ, Rochtchina E, Wang JJ, Healey PR, Mitchell P. Open-angle glaucoma and systemic thyroid disease in an older population: the Blue Mountains Eye Study. Eye. 2004;18(6):600–608. doi: 10.1038/sj.eye.6700731. [DOI] [PubMed] [Google Scholar]
- 27.Wang JJ, Mitchell P, Smith W. Is there an association between migraine headache and open-angle glaucoma? Findings from the Blue Mountains Eye Study. Ophthalmology. 1997;104(10):1714–1719. doi: 10.1016/s0161-6420(97)30075-x. [DOI] [PubMed] [Google Scholar]
- 28.Haefliger IO, Meyer P, Flammer J, Lüscher TF. The vascular endothelium as a regulator of the ocular circulation: a new concept in ophthalmology? Survey of Ophthalmology. 1994;39(2):123–132. doi: 10.1016/0039-6257(94)90157-0. [DOI] [PubMed] [Google Scholar]
- 29.Garbe E, LeLorier J, Boivin JF, Suissa S. Risk of ocular hypertension or open-angle glaucoma in elderly patients on oral glucocorticoids. Lancet. 1997;350(9083):979–982. doi: 10.1016/S0140-6736(97)03392-8. [DOI] [PubMed] [Google Scholar]
- 30.Le A, Mukesh BN, McCarty CA, Taylor HR. Risk factors associated with the incidence of open-angle glaucoma: the visual impairment project. Investigative Ophthalmology and Visual Science. 2003;44(9):3783–3789. doi: 10.1167/iovs.03-0077. [DOI] [PubMed] [Google Scholar]
- 31.McGwin G, Jr., McNeal S, Owsley C, Girkin C, Epstein D, Lee PP. Statins and other cholesterol-lowering medications and the presence of glaucoma. Archives of Ophthalmology. 2004;122(6):822–826. doi: 10.1001/archopht.122.6.822. [DOI] [PubMed] [Google Scholar]
- 32.Lee AJ, Rochtchina E, Mitchell P. Intraocular pressure asymmetry and undiagnosed open-angle glaucoma in an older population. American Journal of Ophthalmology. 2004;137(2):380–382. doi: 10.1016/j.ajo.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 33.Asrani S, Zeimer R, Wilensky J, Gieser D, Vitale S, Lindenmuth K. Large diurnal fluctuations in intraocular pressure are an independent risk factor in patients with glaucoma. Journal of Glaucoma. 2000;9(2):134–142. doi: 10.1097/00061198-200004000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Mojon DS, Hess CW, Goldblum D, et al. High prevalence of glaucoma in patients with sleep apnea syndrome. Ophthalmology. 1999;106(5):1009–1012. doi: 10.1016/S0161-6420(99)00525-4. [DOI] [PubMed] [Google Scholar]
- 35.Arvind H, George R, Raju P, et al. Glaucoma in aphakia and pseudophakia in the Chennai Glaucoma Study. British Journal of Ophthalmology. 2005;89(6):699–703. doi: 10.1136/bjo.2004.056234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Healey PR, Mitchell P. Optic disk size in open-angle glaucoma: the Blue Mountains Eye Study. American Journal of Ophthalmology. 1999;128(4):515–517. doi: 10.1016/s0002-9394(99)00195-6. [DOI] [PubMed] [Google Scholar]
- 37.Ekstrom C. Elevated intraocular pressure and pseudoexfoliation of the lens capsule as risk factors for chronic open-angle glaucoma. A population-based five-year follow-up study. Acta Ophthalmologica. 1993;71(2):189–195. doi: 10.1111/j.1755-3768.1993.tb04989.x. [DOI] [PubMed] [Google Scholar]
- 38.Siddiqui Y, Ten Hulzen RD, Cameron JD, Hodge DO, Johnson DH. What is the risk of developing pigmentary glaucoma from pigment dispersion syndrome? American Journal of Ophthalmology. 2003;135(6):794–799. doi: 10.1016/s0002-9394(02)02289-4. [DOI] [PubMed] [Google Scholar]
- 39.Damji KF, Behki R, Wang L. Canadian perspectives in glaucoma management: setting target intraocular pressure range. Canadian Journal of Ophthalmology. 2003;38(3):189–197. doi: 10.1016/s0008-4182(03)80060-1. [DOI] [PubMed] [Google Scholar]
- 40.Iwase A, Suzuki Y, Araie M, et al. The prevalence of primary open-angle glaucoma in Japanese: the Tajimi Study. Ophthalmology. 2004;111(9):1641–1648. doi: 10.1016/j.ophtha.2004.03.029. [DOI] [PubMed] [Google Scholar]
- 41.Foster PJ, Machin D, Wong TY, et al. Determinants of intraocular pressure and its association with glaucomatous optic neuropathy in Chinese Singaporeans: the Tanjong Pagar study. Investigative Ophthalmology and Visual Science. 2003;44(9):3885–3891. doi: 10.1167/iovs.03-0012. [DOI] [PubMed] [Google Scholar]
- 42.Nemesure B, Wu SY, Hennis A, Leske MC. Corneal thickness and intraocular pressure in the Barbados Eye Studies. Archives of Ophthalmology. 2003;121(2):240–244. doi: 10.1001/archopht.121.2.240. [DOI] [PubMed] [Google Scholar]
- 43.Vijaya L, George R, Paul PG, et al. Prevalence of open-angle glaucoma in a rural south Indian population. Investigative Ophthalmology and Visual Science. 2005;46(12):4461–4467. doi: 10.1167/iovs.04-1529. [DOI] [PubMed] [Google Scholar]
- 44.Sommer A, Tielsch JM, Katz J, et al. Relationship between intraocular pressure and primary open angle glaucoma among white and black Americans: the Baltimore Eye Survey. Archives of Ophthalmology. 1991;109(8):1090–1095. doi: 10.1001/archopht.1991.01080080050026. [DOI] [PubMed] [Google Scholar]
- 45.Quigley HA, Enger C, Katz J, Sommer A, Scott R, Gilbert D. Risk factors for the development of glaucomatous visual field loss in ocular hypertension. Archives of Ophthalmology. 1994;112(5):644–649. doi: 10.1001/archopht.1994.01090170088028. [DOI] [PubMed] [Google Scholar]
- 46.Thomas R, Parikh R, George R, Kumar RS, Muliyil J. Five-year risk of progression of ocular hypertension to primary open angle glaucoma. A population-based study. Indian Journal of Ophthalmology. 2003;51(4):329–333. [PubMed] [Google Scholar]
- 47.Nouri-Mahdavi K, Hoffman D, Coleman AL, et al. Predictive factors for glaucomatous visual field progression in the Advanced Glaucoma Intervention Study. Ophthalmology. 2004;111(9):1627–1635. doi: 10.1016/j.ophtha.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 48.Wa Kaimbo DK, Buntinx F, Missotten L. Risk factors for open-angle glaucoma: a case-control study. Journal of Clinical Epidemiology. 2001;54(2):166–171. doi: 10.1016/s0895-4356(00)00291-2. [DOI] [PubMed] [Google Scholar]
- 49.Martinez GS, Campbell AJ, Reinken J, Allan BC. Prevalence of ocular disease in a population study of subjects 65 years old and older. American Journal of Ophthalmology. 1982;94(2):181–189. doi: 10.1016/0002-9394(82)90073-3. [DOI] [PubMed] [Google Scholar]
- 50.Leske MC, Connell AMS, Wu SY, Hyman LG, Schachat AP. Risk factors for open-angle glaucoma: the Barbados eye study. Archives of Ophthalmology. 1995;113(7):918–924. doi: 10.1001/archopht.1995.01100070092031. [DOI] [PubMed] [Google Scholar]
- 51.Mukesh BN, McCarty CA, Rait JL, Taylor HR. Five-year incidence of open-angle glaucoma: the Visual Impairment Project. Ophthalmology. 2002;109(6):1047–1051. doi: 10.1016/s0161-6420(02)01040-0. [DOI] [PubMed] [Google Scholar]
- 52.Abraham AG, Condon NG, West Gower E. The new epidemiology of cataract. Ophthalmology Clinics of North America. 2006;19(4):415–425. doi: 10.1016/j.ohc.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 53.Thornton J, Edwards R, Mitchell P, Harrison RA, Buchan I, Kelly SP. Smoking and age-related macular degeneration: a review of association. Eye. 2005;19(9):935–944. doi: 10.1038/sj.eye.6701978. [DOI] [PubMed] [Google Scholar]
- 54.Picciotto MR, Zoli M. Neuroprotection via nAChRs: the role of nAChRs in neurodegenerative disorders such as Alzheimer’s and Parkinson’s disease. Frontiers in Bioscience. 2008;13(2):492–504. doi: 10.2741/2695. [DOI] [PubMed] [Google Scholar]
- 55.Kang JH, Pasquale LR, Rosner BA, et al. Prospective study of cigarette smoking and the risk of primary open-angle glaucoma. Archives of Ophthalmology. 2003;121(12):1762–1768. doi: 10.1001/archopht.121.12.1762. [DOI] [PubMed] [Google Scholar]


