Abstract
Two cases of pulmonary alveolar proteinosis, including one death, occurred in workers at a facility producing indium-tin oxide (ITO), a compound used in recent years to make flat panel displays. Both workers were exposed to airborne ITO dust and had indium in lung tissue specimens. One worker was tested for autoantibodies to granulocytemacrophage–colonystimulating factor (GM-CSF) and found to have an elevated level. These cases suggest that inhalational exposure to ITO causes pulmonary alveolar proteinosis, which may occur via an autoimmune mechanism.
Keywords: pulmonary alveolar proteinosis, indium
Indium is a relatively rare element that has been used for decades as a metal, in alloys, and for electronics applications. More recently, indium-tin oxide (ITO), a sintered material typically consisting of 90% indium oxide (In2O3) and 10% tin oxide (SnO2), has been used for the production of flat panel displays including liquid crystal displays (LCDs). In these applications, a thin film of ITO is used as a transparent conductive coating. In 2003 and 2005, Japanese investigators reported two cases of interstitial lung disease in young men who worked with ITO at a metal plant (1, 2). In this article, we describe two cases of pulmonary alveolar proteinosis, including one death, occurring in ITO workers at a United States metal manufacturing facility. Our investigation was prompted by inquiries made by treating physicians to the National Institute for Occupational Safety and Health (NIOSH) and involved a review of medical records and workers' compensation documents. Some information on one of the cases was initially reported in the form of an abstract (3).
The documents describe that the production of ITO for planar tiles began in the facility's refinery, where solid indium metal was used to make indium oxide powder (4). In the ITO department, indium oxide, tin oxide, and other compounds including ammonium hydroxide were mixed in a ball mill. The resultant liquid was agitated in a series of high-speed mixers and poured into molds to harden. The castings were sanded by hand to eliminate rough edges and then fired. The resulting tiles, now sintered, were transferred to the grinding room, outside of the ITO department, where they were shaped to the customer's specifications. Final deburring took place in the ITO department.
The facility also had an indium reclamation process run by the hydrogen furnace operator. Indium oxide produced in the refinery that did not meet specifications, cuttings and grindings from tile processing, and rejected tiles were collected. Solid pieces were crushed by machine or by hand with a hammer and were placed in crucibles, along with the powders. A conveyor belt carried the crucibles into the furnace where an oxygen-deficient atmosphere promoted the reduction of ITO to indium-tin metal alloy. The hydrogen furnace was eliminated after the mid-2002 purchase of the facility by the current owner. About 15 workers at the facility were involved in the production of ITO and reclamation of indium.
CASE REPORTS
Case 1
A healthy 49-year-old nonsmoker began working at the facility in March 1999. He had previously worked in the warehouse of a toy company, installing vinyl siding and cellulose insulation, and driving a forklift at a steel plant. At the metal manufacturing facility, he packed finished cadmium bars for 4 months and then became a hydrogen furnace operator. He described the hydrogen furnace room as being 20 × 80 feet in size, without windows. The room's four doors were generally kept closed, and he noted that its ventilation system rarely functioned. He described smoke and dust coming from the furnace door when crucibles went in and out. He reported that he did not wear respiratory protection when operating the furnace, and he described being exposed to “intense and irritating fumes” when he had to open the oven in the event of a conveyor belt malfunction. He did use respiratory protection when operating the crushing machine, necessitated, he stated, by the amount of dust generated. The facility did not conduct air sampling in the hydrogen furnace room during his employment. Air sampling conducted in the crushing area in early 2005 showed that levels of indium exceeded the NIOSH recommended exposure limit (REL) (5).
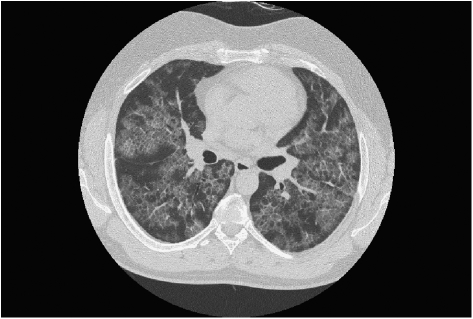
After approximately 9 months as a hydrogen furnace operator, the worker noted the onset of dyspnea on exertion and paroxysmal nocturnal dyspnea. These symptoms increased over several months and were accompanied at times by substernal chest pressure and dry cough. In September 2000 he was admitted to the hospital for suspected myocardial infarction. Cardiac evaluation did not reveal acute issues, but a chest radiograph showed a diffuse micronodular interstitial process. High resolution computed tomography scan of the chest demonstrated extensive ground glass opacity bilaterally, centrilobular nodules, and intralobular and interlobular septal thickening (Figure 1). Pulmonary function tests showed FVC of 3.47 L (73% predicted), FEV1 of 3.11 L (82% predicted), FEV1 to FVC ratio of 90%, total lung capacity (TLC) of 4.83 L (75% predicted), resting room air oxygen saturation of 86 to 89%, and a single-breath carbon monoxide diffusing capacity (Dlco) of 10.70 ml/min/mm Hg (37% predicted). Arterial blood gas on 40% inspired oxygen showed pH of 7.40, Pco2 of 46 mm Hg, and Po2 of 59 mm Hg. Serum lactate dehydrogenase (LDH) was elevated at 318 IU/L.
Figure 1.
High resolution computed tomography scan of the (A) left and (B) right chest showing bilateral ground glass opacities, centrilobular nodules, and intralobular and interlobular septal thickening. The changes were most prominent in the lower lobes.
During his initial hospitalization, the worker underwent bronchoscopy with bronchoalveolar lavage, which demonstrated a predominance of vacuolated macrophages and lymphocytes. A subsequent open-lung biopsy revealed intraalveolar proteinaceous material and globules positive with periodic acid-Schiff (PAS) stain consistent with pulmonary alveolar proteinosis (Figure 2). Additional pathological evaluation using a scanning electron microscope and energy dispersive x-ray analyses (6) identified particles within the proteinaceous material as primarily indium (Figure 3). He was treated with oral steroids and initially opted for segmental lung lavage in early 2001. In August 2001 he underwent whole lung lavage of the right lung with 15 L of saline, followed 2 weeks later by whole lung lavage of the left lung with 14.5 L of saline. The worker remained dependent on supplemental oxygen and was unable to resume employment but expressed a reluctance to undergo a repeat whole lung lavage. In August 2006, due to worsening symptoms, he underwent whole lung lavage of the right lung with 9 L of saline, followed by whole lung lavage of the left lung with 7.5 L of saline. He died in October 2006 of respiratory failure due to pulmonary alveolar proteinosis.
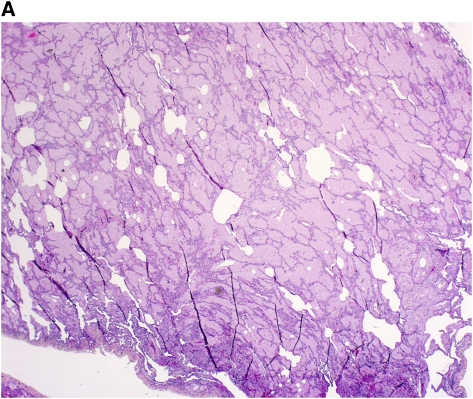
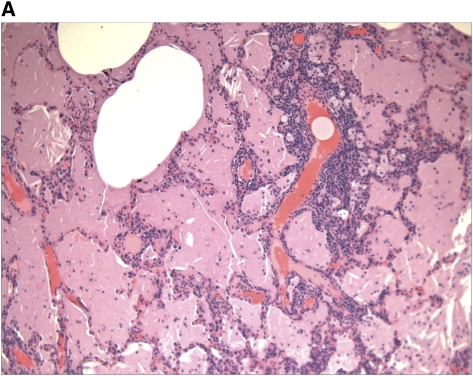
Figure 2.
Histopathological sections of lung biopsy, hematoxylin and eosin stain. (A) Low-power overview showing filling of alveolar spaces by eosinophilic material (magnification ×10). (B) High-power view showing granular eosinophilic material and cholesterol clefts. Note the particulate material within the intraalveolar exudate (magnification ×200). Birefrigent particles were identified with polarizing microscopy, consistent with the presence of crystalline indium-tin oxide. (C) Periodic acid-Schiff (PAS) stain after diastase digestion, showing granular, PAS-positive intraalveolar material, and cholesterol clefts (magnification ×100).
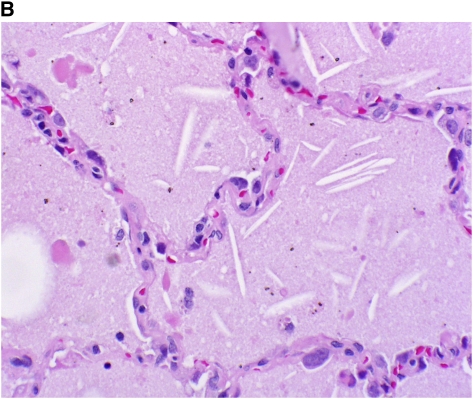
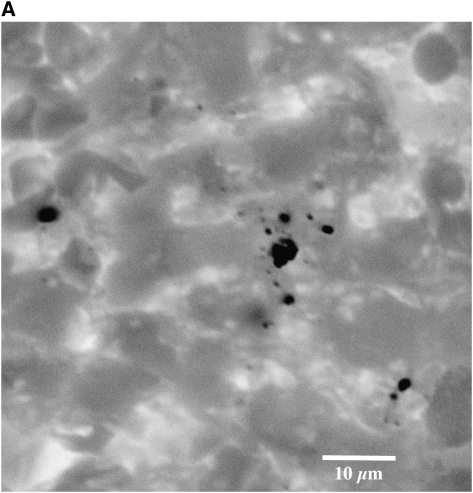
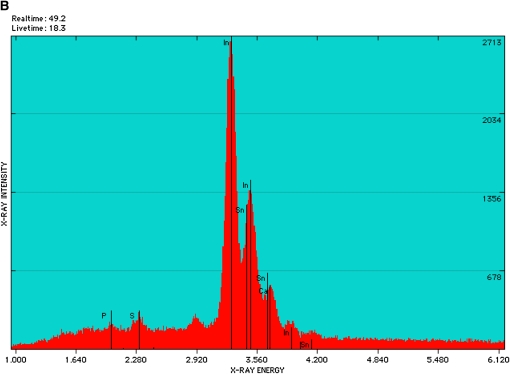
Figure 3.
(A) Negative backscattered electron image obtained with the scanning electron microscope in an area of proteinosis shows numerous (dark) angulated particles within the respiratory size range (magnification ×2300). (B) Energy dispersive x-ray analyses of dozens of these particles identified only indium (In) and tin (Sn). A representative energy dispersive spectrum from one of these particles shows multiple peaks for In (including the small peak at 2.920 keV). There is overlap of the peaks between In and Sn, but the small right-most peak almost certainly represents Sn.
Case 2
A healthy 39-year old smoker began working at the facility in January 2004 in the ITO department. He had no prior industrial experience, having previously worked as a food sales representative. A chest radiograph done in 2001 as part of an evaluation for trauma was interpreted as unremarkable, without lung infiltrates. He described the ITO department as “dusty,” particularly in the area where castings were sanded before firing. He reported that he did not routinely wear respiratory protection. Air sampling conducted in the sanding area in early 2005 showed that levels of indium exceeded the NIOSH REL (5).
The worker described that, approximately 6 to 9 months after hire, he noted the onset of intermittent dry cough, chest tightness, and shortness of breath for which he did not seek care, attributing the symptoms to the common cold. In May 2005, a plasma indium level, part of a workplace surveillance program, was undetectable. In September 2005, he experienced cough, sore throat, nausea, shortness of breath, and chest heaviness after an inhalational exposure to ammonium hydroxide in the vicinity of the ball mill. He was evaluated that day in a clinic, treated with oxygen, and sent home. The following day he was referred for persistent respiratory symptoms to the emergency room, where his oxygen saturation was 96% on room air and a chest radiograph showed moderate to marked increase in interstitial markings. Two days later, he underwent bronchoscopy for airway examination, which revealed hyperemic mucosa but no airway edema.
Over the course of the next month, he was treated with oral steroids and an inhaled beta-agonist, but had little improvement in his dyspnea on exertion and worsening infiltrates on chest radiograph. High resolution computed tomography scan of the chest demonstrated bilateral alveolar and interstitial abnormalities (Figure 4). Pulmonary function tests showed FVC of 3.66 (77% predicted), FEV1 of 3.18 L (83% predicted), FEV1 to FVC ratio of 87%, TLC of 4.47 L (66% predicted), resting room air oxygen saturation of 94% that fell to 90% with exercise, and DlCO of 19.07 ml/min/mm Hg (63% predicted).
Figure 4.
High resolution computed tomography scan of the chest showing bilateral alveolar ground-glass opacities and interstitial thickening in a mosaic pattern. These findings, commonly referred to as “crazy paving,” are consistent with, but not specific for, pulmonary alveolar proteinosis (10).
In December 2005 the worker underwent bronchoscopy with bronchoalveolar lavage, which revealed the presence of granular eosinophilic material. Video-assisted thoracoscopic lung biopsy performed 2 days later demonstrated pathological findings consistent with pulmonary alveolar proteinosis (Figure 5). The presence of indium in the lung was confirmed using inductively coupled plasma/mass spectrometry and reported as 29.3 μg per gram of lung tissue. One month later, arterial blood gas on 100% inspired oxygen showed pH of 7.51, Pco2 of 26 mmHg, and Po2 of 509 mm Hg. In June 2006, due to progressive dyspnea and hypoxia, he underwent whole lung lavage of the left lung with 22 L of saline, followed 2 days later by whole lung lavage of the right lung with 24 L of saline. He had subsequent clinical and radiographic improvement but remains limited in his activities and unable to resume employment. An enzyme-linked immunosorbent assay (ELISA) of the worker's serum in September 2009 was positive for autoantibodies against granulocyte macrophage colony–stimulating factor (GM-CSF), with a level of 52.9 μg/ml (normal = <3 μg/ml).
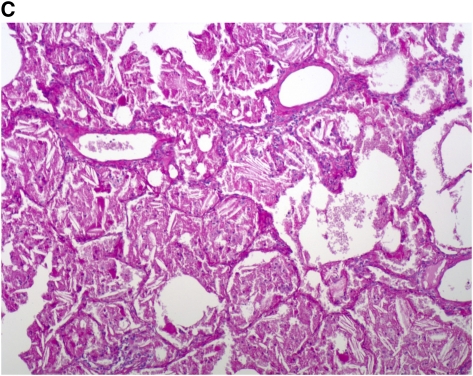
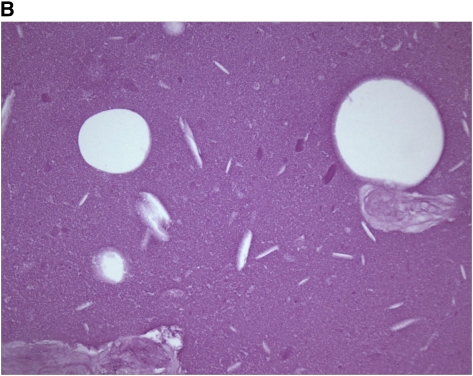
Figure 5.
Histopathological sections of lung biopsy. (A) Hematoxylin and eosin stain showing filling of alveolar spaces with eosinophilic material (magnification ×40). (B) Periodic acid-Schiff (PAS) stain after diastase digestion, showing granular, PAS-positive intraalveolar material and cholesterol clefts (magnification ×400).
DISCUSSION
In the past decade, the demand for indium has grown worldwide, driven by the popularity of LCDs (7). Although ITO substitutes that provide the dual functions of transparency and conductivity are available, they are regarded as technically inferior (zinc-tin oxide) or untested for mass production (carbon nanotubes) (7). Thus, an understanding of the health effects of ITO production is imperative.
We describe two cases of pulmonary alveolar proteinosis in workers involved in the production and recycling of ITO. Pulmonary alveolar proteinosis is a rare disease, characterized by an intraalveolar accumulation of surfactant components and resultant impaired gas exchange (8–10). Progressive dyspnea and cough are common presenting symptoms, and chest imaging typically shows alveolar infiltrates, although interstitial patterns are seen (10). Since the introduction of whole lung lavage, in which saline is used to physically remove excess alveolar material, survival has improved, but the therapy is not curative and residual impairment and recurrence are observed (9, 10). Although most cases of adult pulmonary alveolar proteinosis traditionally have been considered idiopathic, a minority is classified as secondary to another disease, such as a hematological disorder (8–10). Cases of pulmonary alveolar proteinosis also have been reported in association with occupational exposures, including silica, titanium, aluminum, cement, and tin (11–16). Recent investigations into the pathophysiology of idiopathic pulmonary alveolar proteinosis have implicated autoantibodies against GM-CSF that lead to impaired alveolar macrophage function and decreased surfactant clearance (8–10).
Previous reports have provided evidence that exposure to indium can result in pulmonary pathology. Animal studies have demonstrated that exposure to indium oxide, indium phosphide, and ITO results in a spectrum of lesions including alveolar proteinosis and interstitial fibrosis (17–20). Lison and colleagues recently suggested that ITO is particularly reactive (21). In rats, a single administration of ITO, indium oxide, tin oxide, or a nonsintered mixture of indium oxide and tin oxide resulted in alveolitis that persisted at 60 days, accompanied by proteinaceous material in the alveolar lumen; the response to ITO appeared more marked than the responses to its components or the nonsintered mixture (21). The authors also reported that ITO was cytotoxic to cultured alveolar macrophages but not cultured lung epithelial cells (21), which is notable given the role of macrophage impairment in the pathogenesis of pulmonary alveolar proteinosis.
In the two cases of lung disease in Japanese ITO workers, the pathology was described as interstitial pneumonia in the first worker, who ultimately died of bilateral pneumothorax (1), and pulmonary fibrosis in the second (2). Both of those workers were engaged in surface grinding of ITO, each had elevated serum indium levels, and the presence of indium in their lungs was confirmed (1, 2). A subsequent investigation found interstitial changes on high-resolution computed tomography scans of the chest in 23 (21%) of 108 tested current and former workers from the same workplace and a positive correlation between serum indium concentration and degree of radiographic changes (22). More recently, a cross-sectional study of 93 indium-exposed and 93 nonexposed workers in ITO manufacturing and recycling plants in Japan did not find an association between radiograph changes and indium exposure but did demonstrate exposure–response relationships between serum indium concentrations and serum markers of lung inflammation (23).
We were unable to find other reports of pulmonary alveolar proteinosis in ITO workers. In addition to the corroborative results of animal exposure studies and previous reports of lung pathology, several lines of evidence suggest that these cases resulted from workplace exposures. Pulmonary alveolar proteinosis is an exceedingly uncommon disease: there have been fewer than 800 cases reported in the literature since its first description in the 1950s (8, 9, 24). Estimates of the disease's annual incidence and prevalence vary from 0.24 to 0.49 and 2.0 to 6.2 per million population, respectively (8, 24). Thus, the occurrence by chance of two cases in a single facility's small workforce is highly unlikely. The temporal relationship to employment is also compelling: neither worker had a history of respiratory symptoms or disease before being hired, and each became symptomatic months into employment. Furthermore, the finding of indium particles within their lungs, although not irrefutable evidence of causation, confirms occupational respiratory exposure and is consistent with a case-control study that found higher concentrations of inorganic particles in the lung tissue of patients with pulmonary alveolar proteinosis than in the lung tissue of control subjects (25). Finally, we are aware of two additional young workers from the same facility who had diffuse abnormalities on chest imaging studies detected through a workplace medical surveillance program; whereas their subsequent work-ups were insufficient to establish a diagnosis, the overall burden of lung disease in this small group of workers serves to implicate shared workplace exposures.
There are several challenges to be addressed. The worker in Case 1 had previous occupational experience installing cellulose insulation, and pulmonary alveolar proteinosis related to household exposure to cellulose insulation dust has been reported (26). However, his work with insulation preceded the symptom onset by years, he reported consistent use of respiratory protection in that job, and pathological examination did not reveal fibrous material, all which indicates that his prior occupational experience is likely noncontributory. In addition, early in his employment at the facility he worked with cadmium, which has been found to cause pathological changes similar to pulmonary alveolar proteinosis in animals (27). Yet cadmium is an unlikely cause of his disease, given the relatively short period he worked with the substance and the minimal exposure expected with packing finished product. In Case 2, the worker's diagnosis was prompted by an inhalational exposure to ammonium hydroxide, which raises questions about that compound's role in his development of pulmonary alveolar proteinosis. However, it is difficult to reconcile his brief exposure to ammonium hydroxide, a well-recognized irritant that damages the respiratory epithelium through chemical and thermal mechanisms (28, 29), with his earlier onset of respiratory symptoms and the diffuse interstitial changes on chest radiograph detected within a day of the exposure. Far more plausible is the notion that the ammonium hydroxide exposure served to bring an underlying condition to medical attention. Another issue is that this worker did not have a detectable blood indium level when tested, in contrast to the Japanese experience (1, 2, 22, 23). Whether technical differences, such as use of plasma or serum, significantly affect results remains to be determined. Nonetheless, the detection of indium in his lung tissue confirms his exposure.
Why some ITO-exposed workers appear to have developed interstitial lung disease and others pulmonary alveolar proteinosis is unclear. Both of the Japanese case reports described histopathological features suggestive of pulmonary alveolar proteinosis (30): intraalveolar accumulation of cholesterol clefts and particle-laden alveolar macrophages (1, 2). Furthermore, although the abnormalities in pulmonary alveolar proteinosis are classically confined to the alveolar spaces, interstitial infiltration and fibrosis have been described (9, 31–33). Thus, the Japanese cases may represent pulmonary alveolar proteinosis with associated interstitial involvement. Given the possible variations in disease manifestions, pulmonary alveolar proteinosis should be considered in the differential diagnosis of unexplained interstitial lung disease generally (31) and in patients with ITO exposure specifically.
Pulmonary alveolar proteinosis associated with occupational exposure has traditionally been categorized, along with that associated with hematological disorders and other conditions, as secondary disease (8–10). Whereas autoantibodies to GM-CSF have been found to be absent in secondary pulmonary alveolar proteinosis, the secondary cases studied have been limited to those with implicated comorbid diseases (24, 34, 35). Inoue and colleagues recently described a large pulmonary alveolar proteinosis cohort with autoantibodies to GM-CSF (24). The observation that 26% of this group reported a history of inhalational dust exposure (24) raises the possibility that autoimmunity plays a role in the pathophysiology of exposure-related pulmonary alveolar proteinosis and highlights the limitations of the conventional categorizations of this disease. The concept of a chemical exposure triggering an autoimmune response is not new; indeed, a growing literature links heavy metals and other xenobiotics to immune activation and loss of self-tolerance (36, 37, 38). We were unable to find other reports of GM-CSF antibody testing in patients with exposure-related pulmonary alveolar proteinosis. Although the test was not performed in the first case we describe, the presence of autoantibodies to GM-CSF in Case 2 serves to tie the ITO exposure to an autoimmune disease mechanism. Yet this intriguing finding prompts many further questions: for instance, do all cases of ITO-related disease involve autoimmunity; what is the pathophysiologic relevance of the direct macrophage toxicity of ITO (21); and what is the role of exposures, more generally, in autoimmune pulmonary alveolar proteinosis? Ultimately, an investigation into how exposure to ITO and other compounds might lead to the development of GM-CSF autoantibodies would shed needed light on disease mechanism.
In conclusion, these cases, as well as previous experimental and clinical reports, suggest that inhalational exposure to ITO causes pulmonary alveolar proteinosis. Clinicians and public health officials should be alert to the potential for pulmonary toxicity with ITO exposure, and effective control measures should be determined and implemented in workplaces where ITO is used. The role of autoantibodies to GM-CSF in ITO-related pulmonary alveolar proteinosis specifically, and exposure-related pulmonary alveolar proteinosis more generally, should be explored further.
Acknowledgments
The authors thank the following individuals for their assistance: Bassam Aswad, M.D., Rhode Island Hospital, Providence, Rhode Island; David G. Kern, M.D., Togus VA Medical Center, Augusta, Maine; Stanley Schwartz, M.D., Miriam Hospital, Providence, Rhode Island; Charles Sherman, M.D., Coastal Medical, East Providence, Rhode Island; and M. Abbas Virji, Sc.D., NIOSH, Morgantown, West Virginia.
Supported by intramural funding from the National Institute for Occupational Safety and Health. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
Originally Published in Press as DOI: 10.1164/rccm.200907-1022CR on December 17, 2009
Conflict of Interest Statement: K.J.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. W.E.D. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. D.B.E. has received lecture fees paid by Boehringer Ingelheim and, GlaxoSmithKline ($1,001–$5,000). V.L.R. has served served as an expert witness in asbestos litigation (more than $100,000). P.I. has received royalties from Academic Press (more than $1,000). K.K. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.Homma T, Ueno T, Sekizawa K, Tanaka A, Hirata M. Interstial pneumonia developed in a worker dealing with particles containing indium-tin oxide. J Occup Health 2003;45:137–139. [DOI] [PubMed] [Google Scholar]
- 2.Homma S, Miyamoto A, Sakamoto S, Kishi K, Motoi N, Yoshimura K. Pulmonary fibrosis in an individual occupationally exposed to inhaled indium-tin oxide. Eur Respir J 2005;25:200–204. [DOI] [PubMed] [Google Scholar]
- 3.Watanabe WT, Ettensohn DB, Jhung JW, Roggli VL. Pulmonary alveolar proteinosis associated with occupational indium exposure [abstract]. Chest 2002;122:246S–247S. [Google Scholar]
- 4.Medvedovski E, Alvarez N, Yankov O, Olsson MK. Advanced indium-tin oxide ceramics for sputtering targets. Ceram Int 2008;34:1173–1182. [Google Scholar]
- 5.National Institute for Occupational Safety and Health (NIOSH). NIOSH pocket guide to chemical hazards. U.S. Department of Health and Human Services; 2005. DHHS Publication No. (NIOSH) 2005-149.
- 6.Ingram P, Shelburne JD, Roggli VL, LeFurgey A. Biomedical applications of microprobe analysis. San Diego, California: Academic Press; 1999.
- 7.U.S. Geological Survey. Mineral commodity summaries 2008. Washington, DC: U.S. Government Printing Office; 2008:80–81.
- 8.Seymour JF, Presneill JJ. Pulmonary alveolar proteinosis: progress in the first 44 years. Am J Respir Crit Care Med 2002;166:215–235. [DOI] [PubMed] [Google Scholar]
- 9.Trapnell BC, Whitsett JA, Nakata K. Pulmonary alveolar proteinosis. N Engl J Med 2003;349:2527–2539. [DOI] [PubMed] [Google Scholar]
- 10.Ioachimescu OC, Kavuru MS. Pulmonary alveolar proteinosis. Chron Respir Dis 2006;3:149–159. [DOI] [PubMed] [Google Scholar]
- 11.Buechner HA, Ansari A. Acute silico-proteinosis. A new pathologic variant of acute silicosis in sandblasters, characterized by histologic features resembling alveolar proteinosis. Dis Chest 1969;55:274–278. [DOI] [PubMed] [Google Scholar]
- 12.Xipell JM, Ham KN, Price CG, Thomas DP. Acute silicoproteinosis. Thorax 1977;32:104–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keller CA, Frost A, Cagle PT, Abraham JL. Pulmonary alveolar proteinosis in a painter with elevated pulmonary concentrations of titanium. Chest 1995;108:277–280. [DOI] [PubMed] [Google Scholar]
- 14.Miller RR, Churg AM, Hutcheon M, Lam S. Pulmonary alveolar proteinosis and aluminum dust exposure. Am Rev Respir Dis 1984;130:312–315. [DOI] [PubMed] [Google Scholar]
- 15.McCunney RJ, Godefroi R. Pulmonary alveolar proteinosis and cement dust: a case report. J Occup Med 1989;31:233–237. [DOI] [PubMed] [Google Scholar]
- 16.Ray RL, Salm R. A fatal case of pulmonary alveolar proteinosis. Thorax 1962;17:257–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leach LJ, Scott JK, Armstrong RD, Steadman LT, Maynard EA. The inhalation toxicity of indium sesquioxide in the rat. Rochester, NY: University of Rochester; 1961. Atomic Energy Project Report No. UR-590. [DOI] [PubMed]
- 18.American Conference of Governmental Industrial Hygienists (ACGIH). Indium and compounds. In: Documentation of the threshold limit values for chemical substances. 7th ed. Cincinnati: ACGIH Worldwide; 2001.
- 19.National Toxicology Program. Toxicology and carcinogenesis studies of indium phosphide (CAS No. 22398-90-7) in F344/N rats and B6C3F1 mice (inhalation studies). Natl Toxicol Program Tech Rep Ser 2001;499:7–340. [PubMed] [Google Scholar]
- 20.Tanaka A, Hirata M, Omura M, Inoue N, Ueno T, Homma T, Sekizawa K. Pulmonary toxicity of indium-tin oxide and indium phosphide after intratracheal instillations into the lung of hamsters. J Occup Health 2002;44:99–102. [Google Scholar]
- 21.Lison D, Laloy J, Corazzari I, Muller J, Rabolli V, Panin N, Huaux F, Fenoglio I, Fubini B. Sintered indium-tin-oxide (ITO) particles: a new pneumotoxic entity. Toxicol Sci 2009;108:472–481. [DOI] [PubMed] [Google Scholar]
- 22.Chonan T, Taguchi O, Omae K. Interstitial pulmonary disorders in indium-processing workers. Eur Respir J 2007;29:317–324. [DOI] [PubMed] [Google Scholar]
- 23.Hamaguchi T, Omae K, Takebayashi T, Kikuchi Y, Yoshioka N, Nishiwaki Y, Tanaka A, Hirata M, Taguchi O, Chonan T. Exposure to hardly soluble indium compounds in ITO production and recycling plants is a new risk for interstitial lung damage. Occup Environ Med 2008;65:51–55. [DOI] [PubMed] [Google Scholar]
- 24.Inoue Y, Trapnell BC, Tazawa R, Arai T, Takada T, Hizawa N, Kasahara Y, Tatsumi K, Hojo M, Ichiwata T, et al.; Japanese Center of the Rare Lung Diseases Consortium. Characteristics of a large cohort of patients with autoimmune pulmonary alveolar proteinosis in Japan. Am J Respir Crit Care Med 2008;177:752–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abraham JL, McEuen DD. Inorganic particulates associated with pulmonary alveolar proteinosis: SEM and X-ray microanalysis results. Appl Pathol 1986;4:138–146. [PubMed] [Google Scholar]
- 26.McDonald JW, Alvarez F, Keller CA. Pulmonary alveolar proteinosis in association with household exposure to fibrous insulation material. Chest 2000;117:1813–1817. [DOI] [PubMed] [Google Scholar]
- 27.Johansson A, Camner P. Adverse effects of metals on the alveolar part of the lung. Scan Electron Microsc 1986; (Pt 2):631–637. [PubMed]
- 28.National Institute for Occupational Safety and Health (NIOSH). Criteria for a recommended standard: occupational exposure to ammonia. U.S. Department of Health, Education, and Welfare; 1974. DHEW Publication No. (NIOSH) 74-136.
- 29.Arwood R, Hammond J, Ward GG. Ammonia inhalation. J Trauma 1985;25:444–447. [DOI] [PubMed] [Google Scholar]
- 30.Fisher M, Roggli V, Merten D, Mulvihill D, Spock A. Coexisting endogenous lipoid pneumonia, cholesterol granulomas, and pulmonary alveolar proteinosis in a pediatric population: a clinical, radiographic, and pathologic correlation. Pediatr Pathol 1992;12:365–383. [DOI] [PubMed] [Google Scholar]
- 31.Arbiser ZK, Guidot DM, Pine JR, Giltman LI, Gal AA. Pulmonary alveolar proteinosis mimicking idiopathic pulmonary fibrosis. Ann Diagn Pathol 2003;7:82–86. [DOI] [PubMed] [Google Scholar]
- 32.Agarwal PP, Seely JM, Perkins DG, Matzinger FR, Alikhan Q. Pulmonary alveolar proteinosis and end-stage pulmonary fibrosis: a rare association. J Thorac Imaging 2005;20:242–244. [DOI] [PubMed] [Google Scholar]
- 33.Chroneou A, Zias N, Tronic BS, Gonzalez AV, Beamis JF Jr. A case of uncomplicated pulmonary alveolar proteinosis evolving to pulmonary fibrosis. Monaldi Arch Chest Dis 2007;67:234–237. [DOI] [PubMed] [Google Scholar]
- 34.Kitamura T, Tanaka N, Watanabe J, Uchida K, Kanegasaki S, Yamada Y, Nakata K. Idiopathic pulmonary alveolar proteinosis as an autoimmune disease with neutralizing antibody against granulocyte/macrophage colony-stimulating factor. J Exp Med 1999;190:875–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kitamura T, Uchida K, Tanaka N, Tsuchiya T, Watanabe J, Yamada Y, Hanaoka K, Seymour JF, Schoch OD, Doyle I, et al. Serological diagnosis of idiopathic pulmonary alveolar proteinosis. Am J Respir Crit Care Med 2000;162:658–662. [DOI] [PubMed] [Google Scholar]
- 36.Rowley B, Monestier M. Mechanisms of heavy metal-induced autoimmunity. Mol Immunol 2005;42:833–838. [DOI] [PubMed] [Google Scholar]
- 37.Stanca CM, Babar J, Singal V, Ozdenerol E, Odin JA. Pathogenic role of environmental toxins in immune-mediated liver diseases. J Immunotoxicol 2008;5:59–68. [DOI] [PubMed] [Google Scholar]
- 38.Schiraldi M, Monestier M. How can a chemical element elicit complex immunopathology? Lessons from mercury-induced autoimmunity. Trends Immunol 2009;30:502–509. [DOI] [PubMed] [Google Scholar]