Abstract
Rationale: Desert dust particles, including quartz, which causes inflammatory responses in the airway in animal studies, are transported to widespread regions around the globe. Epidemiologically, areas impacted by desert dust storms, such as communities in the Middle East and the Caribbean, seem to have higher incidences of asthma than might be expected.
Objectives: We investigated the magnitude of association between airborne mineral dust concentration and hospitalization of children for asthma exacerbation by using Light Detection And Ranging (LIDAR) with a polarization analyzer for an exposure measurement, which can distinguish mineral dust particles from other particles.
Methods: A case-crossover design was used. The exposure measurement was LIDAR's nonspherical extinction coefficient. The outcome measurement was hospitalization of children aged 1 to 15 years for asthma exacerbation in eight principal hospitals in Toyama, a local area in Japan bordering the Japan Sea, during February to April, 2005 to 2009.
Measurements and Main Results: During the study period, there were 620 admissions for asthma exacerbation, and 6 days with a heavy dust event (daily mineral dust concentration > 0.1 mg/m3). Conditional logistic regression showed a statistically significant association between asthma hospitalization and a heavy dust event. The crude odds ratio (OR) of the heavy dust event for hospitalization on the day was 1.88 (95% confidence interval [CI], 1.04–3.41; P = 0.037), and the OR of heavy dust event during the previous week was 1.83 (95% CI, 1.31–2.56; P = 0.00043). The OR adjusted by other air pollutant levels, pollen, and meteorological factors was 1.71 (95% CI, 1.18–2.48; P = 0.0050).
Conclusions: Heavy dust events are associated with an increased risk of hospitalizations for asthma.
Keywords: Asian dust, Kosa, mineral dust, African dust, quartz
AT A GLANCE COMMENTARY.
Scientific Knowledge on the Subject
Desert dust particles, including quartz, which cause inflammatory responses in the airway in animal studies are transported to widespread regions around the globe. However, no studies have investigated the magnitude of desert dust effects on asthma exacerbation with quantitative objective measures of desert dust in the air.
What This Study Adds to the Field
Desert dust exposure was associated with the increased risk of asthma hospitalization for children with asthma. The risk was particularly high for boys.
Aerosol particles are produced by a variety of processes, both natural and anthropogenic. Among them, desert dust constitutes about 40% of the aerosol mass injected into the troposphere (1).
Quartz, an amorphous and crystalline silica, included in dust sand, is known to cause respiratory disease in occupationally exposed people and highly exposed people who live close to deserts (2–5). It causes inflammatory responses with the release of inflammatory cytokines in the lungs of rats in experimental studies (6–8).
Desert dust is transported to wide regions of the world. Dust originating from the Sahara desert can be transported across the Atlantic Ocean and reach northeastern South America, the Caribbean, Central America, and southeastern United States (9). Dust originating from the Taklimakan desert was transported more than one full circle around the globe in about 13 days (10). Epidemiologically, areas impacted by desert dust storms, such as communities in the Middle East and the Caribbean, seem to have higher incidences of asthma than might be expected (2, 11–13). Although several clinical studies tried to relate desert dust to asthma, none had a quantitative objective measure of desert dust in the air (14–19) except one that measured the amount of some minerals in the air (20). On the other hand, extensive studies of the atmospheric aerosol particle load in the troposphere have been conducted in the last decades using the Light Detection and Ranging (LIDAR) technique in North America, Western Europe, and Asia (10, 21–27). LIDAR is an optical remote sensing technology that measures properties of scattered light to find range and/or other information on a distant target. The LIDAR system with a polarization analyzer can distinguish mineral dust particles (nonspherical particles) from non–mineral dust particles (spherical particles) (28–32). Although particulate matter 2.5 μm or smaller in size and particulate matter 10 μm or smaller in size differentiate the size of particles but do not differentiate mineral dust from nonmineral dust, the LIDAR system with a polarization analyzer does not differentiate the size of particles but does differentiate the shape of particles. Thus, the LIDAR system can specifically measure quantity of mineral dust. In Asia, observations of tropospheric aerosol particles are continuously being conducted using a network of LIDARs at 23 locations in Japan, Korea, and China.
The present study took place in Toyama, Japan, a local prefecture occasionally susceptible to Asian dust events in the spring. Asian dust is a windblown dust originating from the deserts of Mongolia and China. It is a seasonal event, and Asian cities experience yellowish air on several days in the spring when the dust is blowing. We investigated the magnitude of the effect of mineral dust particles on children's asthma exacerbation using the LIDAR measurement. The primary hypothesis was that heavy dust events are associated with an increased risk of hospitalizations for asthma.
METHODS
Study Design
The present study used a case-crossover design (33–35). Four controls were matched to each hospitalization, ± 2 weeks and ± 4 weeks. The study protocol was approved by the Human Research Protection Program of the University of California, San Diego.
Hospitalization Data
Data were obtained from the hospitalization records of eight principal hospitals in Toyama, Japan. Potential cases were children aged 1 to 15 years who had at least one hospitalization with the admission diagnosis of asthma in any of the eight principal hospitals in Toyama between February and April, from 2005 to 2009. Hospitalization referred to actual inpatient admission and did not include emergency visits that did not end in admission.
Dust, Air Pollution, and Meteorological Data
The mineral dust data were based on measurement by the LIDAR system with a polarization analyzer (10, 28, 36).
A heavy dust event day a priori was defined as the day when the daily (24 h) average dust extinction coefficient in Toyama, measured by LIDAR less than 1 km height from the ground, recorded more than 0.1/km, which corresponded to 0.1 mg/m3 mineral dust particles, the standard threshold for particulate matter (28, 36).
Statistical Analysis
Initially, a conditional logistic regression analysis was performed using hospitalization as the dependent variable, and heavy dust event as the independent variable changing the hazard/control period from 1 to 7 days to determine the crude odds ratio (OR) of heavy dust events for asthma hospitalization. We examined possible climatic confounders (daily average temperature, temperature difference from the previous day, temperature difference within the day, air pressure, air pressure difference from the previous day, humidity, and wind speed) if each had an increased OR for asthma hospitalization with various cut-off values and various lag structures up to lag 0 to 6 (Days 0–6). Then we performed cross-correlations of the variables and conducted a conditional logistic regression to determine the climatically adjusted OR using hospitalization as the dependent variable and, as independent variables, heavy dust event and all climatic variables that showed apparent increase (P < 0.1) of OR for asthma hospitalization among the above. We examined other air pollutants (gaseous NO2, SO2, and photochemical oxidants [Ox], non–mineral dust particles, and pollen) if each had an increased OR for asthma hospitalization with various cut-off values and various lag structures up to lag 0 to 6 (Days 0–6). Then these other air pollutants were each examined by a two-compartment model approach to determine if they had an effect on the OR of heavy dust event to asthma hospitalization. Finally, we conducted a conditional logistic regression to obtain the best fit OR using heavy dust event, the climatic variables described above, and other air pollutants described above as independent variables.
The same conditional logistic regression analysis was conducted on each subgroup of sex and age defined a priori (ages 1–5 yr, 6–12 yr, 13–15 yr).
We also conducted the same conditional logistic regression using a heavy dust event defined by a more conventional method, suspended particulate matter (daily average particulate matter level ≥ 0.1 mg/m3), as an exposure measurement. R version 2.9.2 was used for statistical analysis. Additional detail on the method for making these measurements is provided in an online data supplement.
RESULTS
Subjects
During the study period, there were a total of 620 initial hospitalizations for asthma in children who were 1 to 15 years of age. The hospitalization characteristics are described in Table 1. There were more male than female pediatric asthma admissions, consistent with previously published global and regional reports (37). Half of the admissions were for children aged 2 to 5 years. Admissions were most frequent in the month of April and in 2006.
TABLE 1.
DEMOGRAPHICS OF HOSPITALIZATIONS
| No. (%) |
No. (%) |
||||
|---|---|---|---|---|---|
| Sex | Month | ||||
| Male | 367 (59) | Feb | 175 (28) | ||
| Female | 253 (41) | Mar | 199 (32) | ||
| Total | 620 (100) | Apr | 246 (40) | ||
| Total | 620 (100) | ||||
| Age, yr |
Male |
Female |
All |
Year |
|
| 1 | 133 | 52 | 185 (30) | 2005 | 151 (24) |
| 2–5 | 178 | 132 | 310 (50) | 2006 | 170 (27) |
| 6–12 | 52 | 65 | 117 (19) | 2007 | 90 (14) |
| 13–15 | 4 | 4 | 8 (1) | 2008 | 118 (19) |
| Total | 367 | 253 | 620 (100) | 2009 | 91 (15) |
| Mean | 3.2 | 4.2 | 3.6 | Total | 620 (100) |
| Median | 2 | 3 | 2 | ||
Mineral Dust Levels and Other Air Pollutant Levels
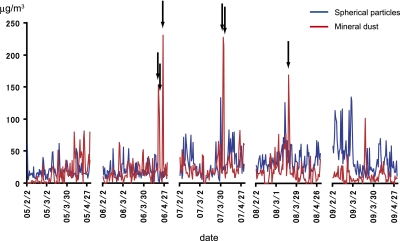
Daily average mineral dust levels greater than 0.1 mg/m3 were recorded on 6 days in Toyama during the study period (Figure 1). Other air pollutant levels and meteorological observations during the study period are shown in Table 2. Correlations between mineral dust levels and air pollutants or meteorological variables are presented in Table E1 in the online supplement. There were no particularly strong correlations among them. In the local area during the study period, cedar was the major source of pollen, and cypress pollen was also observed in a lesser amount.
Figure 1.
Daily levels of mineral dust particles (nonspherical particles) and nonmineral dust particles (spherical particles) during the study period. Red represents mineral dust level, and blue represents nonmineral dust level. Arrows represent the days with more than 0.1 mg/m3 mineral dust particle levels.
TABLE 2.
FREQUENCY DISTRIBUTION OF THE DAILY LEVELS FOR AIR POLLUTANTS AND METEOROLOGICAL OBSERVATIONS DURING THE STUDY PERIOD
| Days | Mean | SD | 25th percentile | Med | 75th percentile | |
|---|---|---|---|---|---|---|
| Mineral dust particles, μg/m3 | 400 | 21.27 | 25.66 | 7.82 | 15 | 25.08 |
| Non–mineral dust particles, μg/m3 | 446 | 28.05 | 20.55 | 4.6 | 22.87 | 35.77 |
| Suspended particulate matter, μg/m3 | 446 | 17.52 | 11.68 | 9 | 14 | 23 |
| NO2, ppm | 446 | 12.61 | 5.85 | 8 | 12 | 17 |
| SO2, ppm | 446 | 0.86 | 0.69 | 0 | 1 | 1 |
| Ox, ppm | 446 | 35.17 | 9.79 | 29 | 36 | 41 |
| Pollen, /cm2 | 400 | 31.8 | 76.7 | 0 | 3 | 21 |
| Average temperature, °C | 446 | 7.64 | 4.86 | 3.8 | 7.2 | 11.2 |
| Temperature difference from the previous day, °C | 446 | 0.15 | 2.9 | −1.4 | 0.3 | 1.8 |
| Temperature difference within the day, °C | 446 | 9.1 | 3.7 | 6.2 | 8.8 | 1.2 |
| Average air pressure, hPa | 446 | 1,014.7 | 6.34 | 1,010.1 | 1,015.2 | 1,019.5 |
| Air pressure difference from the previous day, hPa | 446 | −0.01 | 0.29 | −3.90 | 0.55 | 4.20 |
| Wind speed, m/s | 446 | 6.7 | 2.6 | 4.6 | 6.2 | 8.4 |
| Humidity, % | 446 | 74.4 | 12.4 | 66 | 76 | 84 |
Defnition of abbreviations: Ox = photochemical oxidants.
Relationship between Heavy Mineral Dust Exposure and Asthma Hospitalization
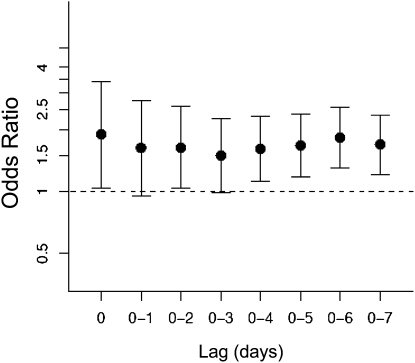
Figure 2 shows the crude ORs for the relationship between asthma hospitalizations and a heavy dust event on the day of the admission (lag 0) and on the previous cumulative 1 to 7 days (lag 0–1 to lag 0–7). A statistically significant association was shown between asthma hospitalization and a heavy dust event. The crude OR of the heavy dust event for hospitalization on the day was 1.88 (95% CI, 1.04–3.41; P = 0.037). The positive association was maintained regardless of the hazard period studied. The crude OR of heavy dust event on any day during the previous week (lag 0–6) was 1.83 (95% CI, 1.31–2.56; P = 0.00043).
Figure 2.
Crude odds ratios for the relationship between asthma hospitalizations and heavy mineral dust exposure (daily average level > 0.1 mg/m3) on the day of the admission (lag 0) or the previous 1 to 7 days (lag 0–1 to lag 0–7). Error bars represent 95% confidence intervals.
A crude association between climatic observations and asthma hospitalization is shown in Table E2. Asthma hospitalization had apparent associations (P < 0.1) with average temperature, air pressure difference from the previous day, and humidity. We conducted a conditional logistic regression with hospitalization as the dependent variable and as independent variables, heavy dust event and climatic variables with apparent association for asthma hospitalization described above, and we obtained the climatically adjusted OR of 1.86 (95% CI, 1.32–2.62; P = 0.00037) for heavy dust event during the previous week.
Table 3 shows the OR and climatically adjusted OR for the heavy dust event (lag 0–6) taking into consideration one of the other pollutants (two-pollutant model). For each two-pollutant model, we examined various models with various lag structures from 0 to 0 to 6 days, and various cut-off levels, but the single-pollutant effect of heavy dust event was only slightly attenuated by other pollutants and remained significant after adjustment in all models. Table 3 shows the OR of heavy dust events for asthma hospitalization in the two-pollutant model using results from a model that showed the strongest association with asthma hospitalization for each other pollutant. The final model for obtaining the adjusted OR of heavy dust event for asthma hospitalization was determined to be the one with the climatic variables and other pollutant variables described above. The best fit OR of heavy dust event for asthma hospitalization was 1.71 (95% CI, 1.18–2.48; P = 0.0050).
TABLE 3.
ODDS RATIO OF HEAVY DUST EVENTS FOR ASTHMA HOSPITALIZATION ADJUSTED BY OTHER POLLUTANTS IN TWO-POLLUTANT MODEL
| Two-pollutant Model Adjusted by |
||||||
|---|---|---|---|---|---|---|
| Single-Pollutant Model | Non–M Dust | Pollen | NO2 | SO2 | Ox | |
| Crude OR | 1.83 | 1.79 | 2.04 | 1.70 | 1.80 | 1.63 |
| 95% CI | 1.31–2.56 | 1.28–2.51 | 1.44–2.88 | 1.21–2.39 | 1.28–2.55 | 1.15–2.29 |
| Climatically adjusted OR | 1.86 | 1.83 | 2.19 | 1.76 | 1.86 | 1.66 |
| 95% CI | 1.32–2.62 | 1.30–2.58 | 1.50–3.04 | 1.25–2.48 | 1.31–2.64 | 1.17–2.35 |
Definition of abbreviations: CI = confidence interval; Non–M dust = non–mineral dust particles; OR = odds ratio.
Non–mineral dust (on the day: lag 0 d) and pollen (on the previous day: lag 1 d) was treated as a five-level variable, NO2 was treated as dichotomous (with cut-off value of 80th percentile and cumulative lag 0–5 d), and SO2 (on the day: lag 0 d) was treated as a five-level nominal variable.
We also conducted the same conditional logistic regression using a heavy dust event defined by suspended particulate matter as an exposure measurement, and a statistically significantly increased OR was shown using this method (Figure E4).
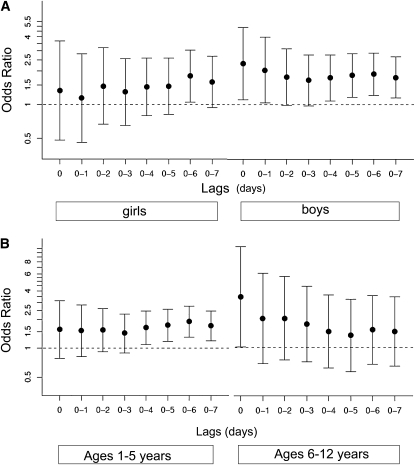
Figure 3 presents the crude OR of heavy dust event for asthma hospitalizations in each sex group and subgroup defined a priori (ages 1–5 yr, 6–12 yr, and 13–15 yr). The associations were particularly strong for boys. The risk for hospitalization on the day of heavy dust event was particularly high for boys (OR, 2.32; 95% CI, 1.10–4.87) and for elementary school ages (OR, 3.33; 95% CI, 1.02–10.92), whereas the risk for hospitalizations the following week seemed similar among the subgroups.
Figure 3.
Crude odds ratios of heavy mineral dust exposure (daily average level > 0.1 mg/m3) for asthma hospitalizations on the day of the admission (lag 0) or the previous 1 to 7 days (lag 0–1 to lag 0–7) in each subgroup. (A) Girls (n = 253) and boys (n = 367). (B) Children aged 1 to 5 years (n = 495) and 6 to12 years (n = 117). Error bars represent 95% confidence intervals.
DISCUSSION
In this study, heavy mineral dust exposure was significantly associated with an increased risk of asthma hospitalization in children. Although we presumed in the study protocol that a high association would be observed during 3 days after mineral dust exposure, a high association was maintained even after 4 to 6 days after the exposure. This is, as far as we know, the first report that showed a clear association between mineral dust exposure and increased risk of asthma hospitalization. Previously reported efforts to investigate the association between desert dust exposure and asthma exacerbation included two studies in the Caribbean islands on Sahara dust, one in Australia on local dust, and one in Taiwan and three in Korea on Asian dust (15–20). All but the Korean studies showed subtle linkage, or did not show obvious associations with visits or admissions for asthma. The studies from Korea showed a significant decrease in peak flow for children and adults with asthma on Asian dust days, although a quantitative definition of Asian dust days was not presented in the reports, and effects of other air pollutants were not taken into consideration (17, 19, 20). In all these studies, there were some days that had particulate matter greater than 0.1 mg/m3 during the study periods. Possible explanations for the variety of results would be difference in exposure measurement, study design, and the general knowledge of people about the risk of dust, and local variation of size, chemical, mineralogical, and microbiological composition of dust particles.
The size distribution of Asian dust particles being lifted into the air and carried to Japan had a peak of 4 μm, and ranged mostly from 0.5 to 10 μm in diameter. Particles this size can penetrate into the lower respiratory system and particles less than 2.5 μm in diameter can enter the gas-exchange region of the lung (2).
Asian dust contains silica and alumina as the main component (6). Quartz, an amorphous and crystalline silica, and aluminum have been reported to cause inflammatory responses with the release of inflammatory cytokines in the lungs of rats (7, 8, 38). Furthermore, Asian dust contains various chemical compounds, including sulfate (SO42−) or nitrate (NO3−), derived from alkaline soil, which capture acidic gases, such as sulfur oxides (SO2) and nitrogen oxides (NO2), during its transportation (39). Hiyoshi and colleagues reported that Asian dust and ovalbumin administered into mice demonstrated an enhanced adjuvant effect of sand dust on ovalbumin-specific IgG1 production when administered together with sulfate (40).
Another important constituent is organics, such as bacteria, fungi, viruses, and other microorganisms. During Asian dust events in Taejon, Korea, the bacterial cfu concentration increased on average 4.3 times over that observed under normal atmospheric conditions (41). Griffin reported that Asian dust included the known allergenic fungi (2). Dust-borne microorganisms in particular can directly impact the immune system of individuals sensitive to those agents, and lipopolysaccharide or β-glucan included in the microorganisms are known pattern-associated molecular patterns that activate dendritic cells to mount an immune response (42). A study by Ichinose and colleagues demonstrated that inhalation of dust sand from Tengger Desert (China), which had higher amounts of β-glucan than dust from the Maowusu Desert (Inner Mongolia), caused greater eosinophil infiltration in the murine airway than did dust from the Maowusu Desert (43). Another study further showed that the heated desert sand, in which microbiological materials and sulfate were excluded by heating, had less effect on allergic lung inflammation (44). Accordingly, quartz, sulfate, and microbiological materials would be included in the pathogenicity of desert sand.
The measured quartz content in a major dust storm is very similar between Asian dust and African dust (60.95% in North Africa and 60.26% in China), and the concentrations of culturable bacteria and fungi and fungal spores in dust storms are greatly elevated relative to background in most investigated places (2, 45). Accordingly, it is quite possible that not only in East Asia but also in many other areas where windborne desert dust is observed, desert dust exposure greatly contributes to asthma admissions of children.
In our study, there were no heavy dust event days in 2005, yet 25% of the hospitalizations occurred in that year. There was a downward trend in hospitalizations from 2007 to 2009 compared with 2006, yet there were three heavy dust event days during this period. Although the desert dust exposure was shown as an independent risk for asthma hospitalization in this study, the contribution of heavy dust events to the total number of asthma hospitalization may be limited in Japan. This is reasonable considering that the heavy dust event occurred only on 6 days of the 446 days of the study period. The heavy dust events may be a more substantial contributor to the total number of asthma hospitalizations in some other parts of the world where dust events occur more frequently than in Japan.
Not only desert dust but also infections, irritants such as tobacco smoke, and other pollutants are also known to exacerbate asthma. In our study, other than heavy dust events, we found statistically significant associations with asthma hospitalization in gaseous NO2, gaseous SO2, gaseous Ox, nonmineral particles, and pollen in some cut-off levels in some lag periods. Similarly, we observed an increased OR when using particulate matter count for an exposure measurement, although this method does not clearly differentiate mineral dust from other particles. Thus, using LIDAR system, it would be possible to caution children with asthma to avoid exposure to heavy dust environments.
In the present study, the risk of mineral dust for asthma hospitalization was particularly high for boys (Figure 3A). Especially, the risk on the first day of the exposure was high for boys and for elementary school ages (6–12 yr old), whereas girls and infants (1–5 yr old) showed the increased risk later in the week (Figure 3B). The percentage of elementary school ages among all ages in boys (14%) was lower than in girls (26%). Accordingly the stronger association observed in boys cannot be explained by the distribution of ages. It is interesting that boys showed a higher OR in heavy dust events and girls showed a higher OR for other air pollutants, such as NO2, SO2, and Ox, in our study. The high risk on the first day observed in boys and in elementary school–aged children may have been influenced by any of several factors: length of exposure to outdoor air, exercise in outdoor air, or any immune mechanism that might make these groups more susceptible to mineral dust particles. Further investigations should be conducted to investigate if there are any differences in pathogenesis between the earlier asthma symptoms and later ones and to determine if there are especially susceptible subpopulations among patients with asthma, including adults.
Aerosolized particles have various effects on the atmospheric environment, including chemical and radiative effects, and also on the oceanic environment (2). It is not realistic to eliminate the dust events, which would negatively influence living creatures in various ways. However, we believe that we can at least minimize the detrimental effects of desert dust exposure by giving information to relevant people, so that susceptible children can protect themselves.
Our study has following limitations. First, the interpretation was limited by the occurrence of only six heavy dust event days in the study period. Second, the exposure data were not individually based but were based on measurements in the locality. Accordingly, it is possible that we underestimated the association because of miscategorizations. Third, because we chose hospitalizations for the outcome measure, the study results are generalized only to children who can be hospitalized. However, an observational study in Japan shows that 17.5% of pediatric patients with intermittent mild asthma also experience hospitalization, and accordingly our study result will probably be applicable not only for patients with moderate to severe disease but also for patients with mild disease (46). Last, the associations we found were only for acute effects. Chronic effects should be further investigated.
As for the strength of our study, we used objective measures for both exposure and outcome, so that recall bias or presentation bias could be excluded. Additionally, we used the LIDAR nonspherical extinction coefficient for an exposure measure, so that we could focus on the effect of mineral dust particles.
In conclusion, this study suggested that heavy dust events were significantly associated with the increased risk of asthma admission for children with asthma. Physicians, patients, and the general public, including schools and preschools, should be adequately informed of the health implications of heavy desert dust exposure so that those at risk can minimize the deleterious effects.
Supplementary Material
Acknowledgments
The authors thank Tetsushi Komori and Hisashi Noma for statistical support; Mizuka Kido and Nobuo Sugimoto in the National Institute of Environmental Studies for providing us with LIDAR data and its technical information; Kazue Mano and Misao Aibe for providing us with meteorological data and gaseous air pollution data; Hideto Miyauchi in the Japan Weather Association for providing us with pollen data; Prof. Takashi Kawamura, Prof. Takamichi Ichinose, Prof. Michiaki Mishima, Dr. Akio Niimi, and Satoshi Ohtsuki for fruitful discussions; Dr. Hiroki Matsukura, Dr. Yoshie Okabe, Dr. Yoko S Adachi, Junko Matsuura, Yurina, and Wai-King Kwan for data management; and Sara for providing motivation.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.201002-0296OC on July 23, 2010
Author Disclosure: K.T.K. was a full-time employee for 1 year and a part-time employee for 2 years of Bayer Yakuhin, Ltd and received up to $1,000 from Taiho Seiyaku for a lecture at a seminar. I.I. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. W.K.A-D. received $5,001–$10,000 for serving as an expert witness for the Hansen Food Company. Y.A. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. W.C.M. received more than $100,001 from the National Institutes of Health in sponsored grants. J.W.R. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
Toyama Asian Desert Dust and Asthma Study Group Members: Yuichi Adachi, M.D., Ph.D., and Toshiko Itazawa, M.D., Ph.D. (University of Toyama); Yasunori Ito, M.D., Ph.D. (Kurobe City Hospital); Kentaro Tamura, M.D. (Toyama Prefectural Central Hospital); Yoko Shitano, M.D. (Toyama City Hospital); Gyokei Murakami, M.D., Ph.D. (Toyama Red Cross Hospital); Osamu Higuchi, M.D. (Kouseiren Takaoka Hospital); Takao Tsuji, M.D. (Takaoka Municipal Hospital); Tatsuya Fuchizawa, M.D., Ph.D. (Saiseikai Takaoka Hospital); and Junko Yamamoto, M.D., Ph.D. (Himi City Hospital).
References
- 1.Tegen I, Fung I. Contribution to the atmospheric mineral aerosol load from land surface modification. J Geophys Res 1995;100:18707–18726. [Google Scholar]
- 2.Griffin DW. Atmospheric movement of microorganisms in clouds of desert dust and implications for human health. Clin Microbiol Rev 2007;20:459–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Valiante DJ, Schill DP, Rosenman KD, Socie E. Highway repair: a new silicosis threat. Am J Public Health 2004;94:876–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eagan TM, Gulsvik A, Eide GE, Bakke PS. Occupational airborne exposure and the incidence of respiratory symptoms and asthma. Am J Respir Crit Care Med 2002;166:933–938. [DOI] [PubMed] [Google Scholar]
- 5.Al Kassimi FA, Al Majed SA, Al Hajjaj MS. Silicosis in a Himalayan village population: role of environmental dust. Thorax 1991;46:861–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ichinose T, Yoshida S, Sadakane K, Takano H, Yanagisawa R, Inoue K, Nishikawa M, Mori I, Kawazato H, Yasuda A, et al. Effects of Asian sand dust, Arizona sand dust, amorphous silica and aluminum oxide on allergic inflammation in the murine lung. Inhal Toxicol 2008;20:685–694. [DOI] [PubMed] [Google Scholar]
- 7.Murphy SA, Bérubéa KA, Pooleya FD, Richards RJ. The response of lung epithelium to well characterised fine particles. Life Sci 1998;62:1789–1799. [DOI] [PubMed] [Google Scholar]
- 8.Mancino D, Vuotto ML, Minucci M. Effects of a crystalline silica on antibody production to T-dependent and T-independent antigens in Balb/c mice. Int Arch Allergy Appl Immunol 1984;73:10–13. [DOI] [PubMed] [Google Scholar]
- 9.Prospero JM. Impat of the North African drought and El Nino on mineral dust in the Barbodas trade winds. Nature 1986;320:735–738. [Google Scholar]
- 10.Uno I, Eguchi K, Yumimoto K, Takemura T, Shimizu A, Uematsu M, Liu Z, Wang Z, Hara Y, Sugimoto N. Asian dust transported one full circuit around the globe. Nat Geosci 2009;2:557–560. [Google Scholar]
- 11.Al Frayh AR, Shakoor Z, Gad El Rab MO, Hasnain SM. Increased prevalence of asthma in Saudi Arabia. Ann Allergy Asthma Immunol. 2001;86:292–296. [DOI] [PubMed] [Google Scholar]
- 12.Bener A, Abdulrazzaq YM, Al-Mutawwa J, Debuse P. Genetic and environmental factors associated with asthma. Hum Biol 1996;68:405–414. [PubMed] [Google Scholar]
- 13.Howitt ME. Asthma management in the Caribbean—an update. Postgrad. Doctor Caribb 2000;16:86–104. [Google Scholar]
- 14.Prospero JM, Blades E, Naidu R, Mathison G, Thani H, Lavoie MC. Relationship between African dust carried in the Atlantic trade winds and surges in pediatric asthma attendances in the Caribbean. Int J Biometeorol 2008;52:823–832. [DOI] [PubMed] [Google Scholar]
- 15.Gyan K, Henry W, Lacaille S, Laloo A, Lamsee-Ebanks C, McKay S, Antoine RM, Monteil MA. African dust clouds are associated with increased paediatric asthma accident and emergency admissions on the Caribbean island of Trinidad. Int J Biometeorol 2005;49:371–376. [DOI] [PubMed] [Google Scholar]
- 16.Park JW, Lim YH, Kyung SY, An CH, Lee SP, Jeong SH, Ju YS. Effects of ambient particulate matter on peak expiratory flow rates and respiratory symptoms of asthmatics during Asian dust periods in Korea. Respirology 2005;10:470–476. [DOI] [PubMed] [Google Scholar]
- 17.Yoo Y, Choung JT, Yu J, Kim do K, Koh YY. Acute effects of Asian dust events on respiratory symptoms and peak expiratory flow in children with mild asthma. J Korean Med Sci 2008;23:66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rutherford S, Clark E, McTainsh G, Simpson R, Mitchell C. Characteristics of rural dust events shown to impact on asthma severity in Brisbane, Australia. Int J Biometeorol 1999;42:217–225. [DOI] [PubMed] [Google Scholar]
- 19.Yang CY, Tsai SS, Chang CC, Ho SC. Effects of Asian dust storm events on daily admissions for asthma in Taipei, Taiwan. Inhal Toxicol 2005;17:817–821. [DOI] [PubMed] [Google Scholar]
- 20.Hong YC, Pan XC, Kim SY, Park K, Park EJ, Jin X, Yie SM, Kim YH, Park CH, Song S, et al. Asian Dust Storm and pulmonary function of school children in Seoul. Sci Total Environ 2010;408:754–759. [DOI] [PubMed] [Google Scholar]
- 21.Hong CS, Lee KH, Kim YJ, Iwasaka Y. LIDAR measurements of the vertical aerosol profile and optical depth during the ACE-Asia 2001 IOP, at Gosan, Jeju Island, Korea. Environ Monit Assess 2004;92:43–57. [DOI] [PubMed] [Google Scholar]
- 22.Iwasaka Y, Shi GY, Kim YS, Matsuki A, Trochkine D, Zhang D, Yamada M, Nagatani T, Nagatani M, Shen Z, et al. Pool of dust particles over the Asian continent: balloon-borne optical particle counter and ground-based lidar measurements at Dunhuang, China. Environ Monit Assess. 2004;92:5–24. [DOI] [PubMed] [Google Scholar]
- 23.Krueger D, Caldwell L, Alvarez H, She C. Self-consistent method for determining vertical profiles of aerosols and atmospheric parameters using a high-spectral resolution Rayleigh-Mie lidar. J Atmos Ocean Technol 1995;10:533–545. [Google Scholar]
- 24.Takamura T, Sasano Y, Hayakashi T. Tropospheric aerosol optical properties derived from lidar, sun photometer and optical particle counter measurements. Appl Opt 1994;33:7132–7140. [DOI] [PubMed] [Google Scholar]
- 25.Marenco F, Santacesaria V, Bais A, Balis D, di Sarra A, Papayannis A, Zerefos CS. Optical properties of tropospheric aerosols determined by lidar and spectrophotometric measurements (PAUR campaign). Appl Opt 1997;36:6875–6886. [DOI] [PubMed] [Google Scholar]
- 26.Matthias V, Balis D, Bösenberg J, Eixmann R, Iarlori M, Komguem L, Mattis I, Papayannis A, Pappalardo G, Perrone MR, et al. Vertical aerosol distribution over Europe: statistical analysis of Raman lidar data from 10 European Aerosol Research Lidar Network (EARLINET) stations. J Geophys Res 2004;109:D18201. [Google Scholar]
- 27.Mona Saharan dust intrusions in the Mediterranean area: three years of Ramadan lidar measurements. J Geophys Res 2006;111:D16203. [Google Scholar]
- 28.Sugimoto N, Uno I, Nishikawa M, Shimizu A, Matsui I, Dong X, Chen Y, Quan H. Record Heavy Asian Dust in Beijing in 2002: observations and model analysis of recent events. Geophys Res Lett 2003;30:1640. [Google Scholar]
- 29.Shimizu A, Sugimoto N, Matsui I, Arao K, Uno I, Murayama T, Kagawa N, Aoki K, Uchiyama A, Yamazaki A. Continuous observations of Asian dust and other aerosols by polarization lidars in China and Japan during ACE-Asia. J Geophys Res 2004;109.
- 30.Browel EV, Butler CF, Ismail S, Robinette PA, Carter AF, Higdon NS, Toon OB, Schoeberl MR, Tuck AF. Airborne lidar observations in the wintertime Arctic stratosphere: polar stratosphere clouds. Geophys Res Lett 1990;17:385–388. [Google Scholar]
- 31.Sugimoto N, Lee CH. Characteristics of dust aerosols inferred from lidar depolarization measurements at two wavelengths. Appl Opt 2006;45:7468–7474. [DOI] [PubMed] [Google Scholar]
- 32.Murayama T, Okamoto H, Kaneyasu N, Kamataki H, Miura K. Application of llidar depolarization measurement in the atmospheric boundry layer. Effects of dust and sea-salt particles. J Geophys Res 1999;104:31781–31792. [Google Scholar]
- 33.Lin M, Chen Y, Burnett RT, Villeneuve PJ, Krewski D. Effect of short-term exposure to gaseous pollution on asthma hospitalisation in children: a bi-directional case-crossover analysis. J Epidemiol Community Health 2003;57:50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tecer LH, Alagha O, Karaca F, Tuncel G, Eldes N. Particulate matter (PM2.5, PM10–2.5, and PM10) and Children's Hospital admissions for asthma and respiratory diseases: a bidirectional case-crossover study. J Toxicol Environ Health A 2008;71:512–520. [DOI] [PubMed] [Google Scholar]
- 35.Maclure M, Mittleman MA. Should we use a case-crossover design? Annu Rev Public Health 2000;21:193–221. [DOI] [PubMed] [Google Scholar]
- 36.Sugimoto N, Matsuia I, Shimizu A, Nishizawa T, Hara Y, Xiea C, Uno I, Yumimoto K, Wang Z, Yoon SC. Lidar network observations of tropospheric aerosols. In: Singh UN, Asai K, Jayaraman A, editors. Lidar remote sensing for environmental monitoring IX. Proc SPIE 2008;7153.
- 37.Adachi M, Ohta K, Morikawa A, Nishima S, Disantostefano RL. Changes in asthma insights and reality in Japan (ARJ) in 2005 since 2000. Arerugi 2008;57:107–120. [PubMed] [Google Scholar]
- 38.Eisenbarth SC, Colegio OR, O'Connor Jr W, Sutterwala FS, Flavell RA. Crucial role for the Nalp3 inflammasome in the immunostimulatory properties of aluminium adjuvants. Nature 2008;453:1122–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Choi JC, Lee M, Chun Y, Kin J, Oh S. Chemical composition and source signature of spring aerosol in Seoul, Korea. J Geophys Res 2001;106:18067–18074. [Google Scholar]
- 40.Hiyoshi K, Ichinose T, Sadakane K, Takano H, Nishikawa M, Mori I, Yanagisawa R, Yoshida S, Kumagai Y, Tomura S, et al. Asian sand dust enhances ovalbumin-induced eosinophil recruitment in the alveoli and airway of mice. Environ Res 2005;99:361–368. [DOI] [PubMed] [Google Scholar]
- 41.Choi DS, Park YK, Oh SK, Yoon HJ, Kim JC, Seo WJ, Cha SH. Distribution of airborne microorganisms in yellow sands of Korea. J Microbiol 1997;35:1–9. [Google Scholar]
- 42.Willart MAM, Lambrecht BN. The danger within: endogenous danger signals, atopy and asthma. Clin Exp Allergy 2008;39:12–19. [DOI] [PubMed] [Google Scholar]
- 43.Ichinose T, Sadakane K, Takano H, Yanagisawa R, Nishikawa M, Mori I, Kawazato H, Yasuda A, Hiyoshi K, Shibamoto T. Enhancement of mite allergen-induced eosinophil infiltration in the murine airway and local cytokine/chemokine expression by Asian sand dust. J Toxicol Environ Health A 2006;69:1571–1585. [DOI] [PubMed] [Google Scholar]
- 44.Ichinose T, Yoshida S, Hiyoshi K, Sadakane K, Takano H, Nishikawa M, Mori I, Yanagisawa R, Kawazato H, Yasuda A, et al. The effects of microbial materials adhered to Asian sand dust on allergic lung inflammation. Arch Environ Contam Toxicol 2008;55:348–357. [DOI] [PubMed] [Google Scholar]
- 45.Derbyshire E. Natural minerogenic dust and human health. Ambio 2007;36:73–77. [DOI] [PubMed] [Google Scholar]
- 46.Chohnabayashi N, Sugiyama K, Kato M, Kimura T, Mochiduki H, Yasuba H, Yoshihara S, Fukuda T, Morikawa A, Adachi M. Impact of inhaled corticosteroid prescription at discharge from the emergency room on exacerbations of asthma in Japanese hospital. Arerugi 2010;59:123–136. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.