Abstract
Objectives
To investigate policies on neonatal vitamin K and their implementation.
Design
Two phase postal survey.
Setting
United Kingdom.
Participants
A 10% random sample of midwives registered with the United Kingdom Central Council for nursing, midwifery, and health visiting. Of 3191 midwives in the sample, 2515 (79%) responded to phase one and 2294 (72%) completed questionnaires on their current jobs (November 1998 to May 1999). In phase two, 853 (62%) of 1383 eligible midwives gave details on 2179 of their earliest jobs (start dates before 1990).
Results
All the midwives in clinical practice at the time of the survey (2271, 99%) reported that they were working in areas with official policies on neonatal vitamin K. Seven distinct policies were described: intramuscular vitamin K for all babies (1159, 51.0%); intramuscular vitamin K for babies at “high risk,” oral for others (470, 20.7%); oral vitamin K for all babies (323, 14.2%); parental choice for all (124, 5.5%); parental choice for all except babies at high risk, (119, 5.2%); intramuscular vitamin K for babies at high risk only (33, 1.5%); oral vitamin K for babies at high risk only (17, 0.7%); and a disparate group of policies including intravenous vitamin K for some babies (26, 1.1%). Previous policies were (and some may still be) open to individual interpretation and were not always followed.
Conclusions
Hospital policy is not necessarily a good guide to individual practice. The primary purpose of clinical records is to document patient care, and recording practices reflect this. There is considerable variation in vitamin K policies and midwifery practice in the United Kingdom, and there is no clear consensus on which babies should receive vitamin K intramuscularly.
What is already known on this topic
Neonatal administration of vitamin K by the intramuscular route is effective in the prevention of haemorrhagic disease in newborn babies but has been suggested as a possible risk factor for leukaemia in children
A written record confirming that vitamin K has (or has not) been given is often not found, and some research groups have attempted to impute a child's vitamin K status from hospital policy
Nothing is known about how midwives interpret and implement vitamin K policies
What this study adds
Earlier hospital policies were open to individual interpretation and they were not always followed
There is considerable variation in current vitamin K policies and midwifery practice in the United Kingdom and no clear consensus on which babies should receive vitamin K intramuscularly
Introduction
Concern over prophylactic administration of vitamin K to newborn babies has continued for almost a decade, following reports in the early 1990s of a statistically significant association between intramuscular vitamin K and childhood cancer.1 Subsequent studies have, in general, failed to support this association.2–10 Inconsistencies in results from the United Kingdom in particular have, however, left lingering doubts about the safety of administering vitamin K by the intramuscular route.1,6–10
Most British studies have had a case-control design, with exposure data collected retrospectively from maternity records.1,6,7,9,10 Details of vitamin K administration may be found in several places in maternity records,6 and all studies report that a written record confirming that it has (or has not) been given is often not found. Some research groups have attempted to impute a child's vitamin K status from the hospital policy in place at the time of the child's birth. Vitamin K is, however, unique among drugs given to newborn babies—although policies have customarily been decided by paediatricians, a midwife has usually made the final decision to give vitamin K to a healthy baby.
Three assumptions underpin imputation of vitamin K status: that previous policies are accurately recalled by current staff; that policies were followed rigidly; and that vitamin K was often given without a record being made. Anecdotal reports from midwives and paediatricians suggest, however, that official policies were not always followed. If true, this has serious implications for interpreting studies investigating neonatal vitamin K status. Furthermore, continuing controversy over vitamin K is having deleterious effects on babies, parents, midwives, and paediatricians.11–14
This two phase postal survey of midwives had two aims: to assess the validity of imputing vitamin K status from hospital policy and to investigate the impact of the controversy on current vitamin K polices and midwifery practice in the United Kingdom.
Methods
In September 1998 a 10% random sample of midwives registered as practising in the United Kingdom was selected from the professional register by the United Kingdom Central Council for nursing, midwifery, and health visiting. Questionnaires were posted directly to midwives by the central council, and names and addresses were not disclosed to the research team. Midwives could, however, add their names and contact details to the completed questionnaires.
In phase one, all midwives in the sample were sent a questionnaire, a postage-paid return envelope, and a letter describing the study. A freephone telephone number was provided for resolution of queries. The first questionnaire collected, among many other items, data on current vitamin K policies and their implementation. Questionnaires were posted in November 1998, and reminders were sent to non-responders in February and May 1999.
Midwives who returned completed questionnaires, who qualified before 1990 (the year of the first report suggesting a possible link between vitamin K and childhood cancer), and who could be contacted again were eligible for phase two. These midwives were sent an additional questionnaire requesting information on recording practices and whether policies were followed in their earliest jobs (up to four). No reminders were sent to non-responders in phase two.
Questionnaires were checked on receipt, and queries were resolved by discussion with respondents who provided contact information. Data were coded and entered into Microsoft Access databases designed for the study. Analyses were carried out using Access and the statistical software package Stata 6.0 (Stata Corporation, College Station, TX).
Results
Response
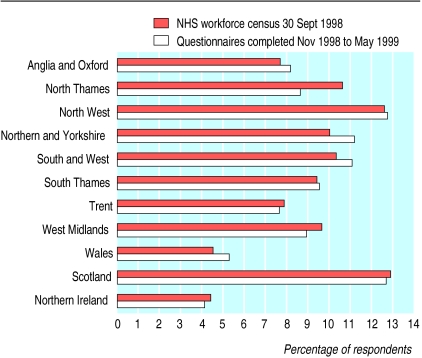
Of 3191 midwives surveyed, 2515 (79%) replied to phase one and 2294 (72%) completed questionnaires. The age distribution of midwives who completed questionnaires (respondents) closely matched that of all practising midwives on the professional register (statistical analysis of the United Kingdom Central Council's professional register—reports dated July 1998 and November 1999). Distribution of respondents by health region, compared with that of all midwives in post in the NHS at 30 September 1998, is shown in the figure.15–18
Most respondents (89.1%; 2045) were, at the time of the survey, working in general midwifery posts caring for mothers and babies. Of the remainder, 4.6% (106) were senior midwives or managers, 1.9% (44) were midwifery teachers, 1.7% (38) worked in special care nurseries, 2.0% (47) had specialist or research posts, and 0.6% (14) did not state their current job. All midwives who reported that they were currently in clinical practice (2271; 99%) were working in areas with an official vitamin K policy. In phase two, 853 (62%) of the 1383 eligible midwives returned completed questionnaires.
Vitamin K policies
Policies in midwives' current jobs (November 1998 to May 1999) are detailed in table 1. Seven distinct policies were described; the most common policy was intramuscular vitamin K for all babies (51.0%; 1159). Overall, in 96.7% (2195) of jobs with an official policy, the policy specifies some form of vitamin K for all babies, if parents consent.
Table 1.
Vitamin K policies in midwives' current jobs (November 1998 to May 1999), with criteria for including babies in group at “high risk” if policy selective
| Percentage (No) | |
|---|---|
| Jobs with an official policy specifying route of administration (n=2271) | |
| Vitamin K given by one route only: | |
| Intramuscular for all babies | 51.0 (1159) |
| Oral for all babies | 14.2 (323) |
| Intramuscular for babies at high risk* only | 1.5 (33) |
| Oral for babies at high risk* only | 0.7 (17) |
| Vitamin K given by more than one route: | |
| Intramuscular for babies at high risk*, oral for all others | 20.7 (470) |
| Parents choose route and/or if vitamin K given | 5.5 (124) |
| Parents choose route and/or if given unless high risk* | 5.2 (119) |
| Other selective policies | 1.1 (26) |
| Selective policies including each criterion (n=665) | |
| Premature birth† | 64.5 (429) |
| Difficult instrumental delivery (for example, high forceps) | 56.4 (375) |
| Admission to neonatal unit/special care nursery | 53.2 (354) |
| Birth trauma | 46.9 (312) |
| Breech delivery | 34.9 (232) |
| Caesarean section‡ | 34.9 (232) |
| Easy instrumental delivery (for example, low forceps) | 32.5 (216) |
| Birth asphyxia§ | 33.2 (221) |
| Maternal anticonvulsants | 25.4 (169) |
| Small for gestational age | 13.4 (89) |
| Breast feeding | 9.3 (62) |
| Jaundice | 8.9 (59) |
| Antibiotics prescribed | 3.5 (23) |
| Ventilated or unable to take oral feeds | 2.9 (19) |
| Poor feeding | 2.7 (18) |
| Circumcision | 2.4 (16) |
| Maternal antituberculosis drugs | 0.8 (5) |
| Other illness in mother or baby | 19.8 (132) |
| Paediatrician's clinical judgment | 1.8 (12) |
| Unknown, no criteria given | 3.6 (24) |
Considered at high risk of haemorrhagic disease.
Gestation varies: <37 weeks (53), <36 (149), <34 (66), <32 (22), <30 (7), <28 (5), unknown (127).
Emergency caesarean section only in one job.
One or more of the following criteria specified: birth asphyxia, low Apgar score, fetal distress, meconium liquor.
Also shown in table 1 are criteria for including babies in the group at “high risk” if policies are selective. Criteria included in more than 50% of policies were premature birth (64.5%; 429), difficult instrumental delivery (for example, high forceps) (56.4%; 375), and admission to a neonatal intensive or special care nursery (53.2%; 354). Other complicated or instrumental deliveries were included less frequently: breech delivery, 34.9% (232); caesarean section, 34.9% (232); and easy instrumental delivery (for example, low forceps), 32.5% (216). Interestingly, a paediatrician's clinical judgment was specified as a criterion in 1.8% (12) of policies.
There is considerable variation in the combinations of criteria included in individual policies, with more than one criterion applying to some babies—for example, premature birth and admission to a neonatal nursery. Additionally, definitions of some criteria vary from one policy to another; the gestation below which babies were considered to be at high risk, for example, ranged from <37 weeks (53 policies) to <36 (149), <34 (66), <32 (22), <30 (7), and <28 weeks (5), with gestation not stated for 127.
Implementation of current policies
Of the 2271 midwives whose current job had an official policy, 81.8% (1858) reported that the policy was always followed, with 14.3% (326) reporting that it was not and 3.8% (87) being unsure (table 2). The main reason given for not following official policy was parental refusal or insistence on an oral preparation (88.0%; 287), followed by paediatricians (8.0%; 26) and midwives (2.1%; 7) using their own clinical judgment and general practitioners' refusal to prescribe an oral preparation (0.6%; 2).
Table 2.
Implementation of policies on administration of vitamin K in midwives' current jobs (November 1998 to May 1999)
| Percentage (No) (n=2271) | |
|---|---|
| Policy always followed: | |
| Yes | 81.8 (1858) |
| No | 14.3 (326) |
| Not sure | 3.8 (87) |
| Reasons policy not followed: | |
| Parents refused or insisted on an oral preparation | 88.0 (287) |
| Paediatricians used their own clinical judgment | 8.0 (26) |
| Midwives used their own clinical judgment | 2.1 (7) |
| General practitioner refused to prescribe oral preparation | 0.6 (2) |
| Not stated | 1.2 (4) |
| Places vitamin K is recorded: | |
| Neonatal record or separate neonatal notes | 80.1 (1818) |
| Maternal obstetric notes | 73.4 (1666) |
| Discharge summary | 52.8 (1199) |
| Midwifery notes or Kardex (mother's or baby's) | 51.7 (1174) |
| Name tag on baby's cot | 27.6 (627) |
| Baby's observation, care, or feed charts | 27.0 (614) |
| Baby's personal drug/vitamin K chart or form | 8.4 (191) |
| Special vitamin K register | 0.4 (9) |
| Number of times or places each dose is recorded: | |
| 1 | 10.6 (241) |
| 2 | 18.7 (425) |
| 3 | 24.3 (552) |
| 4 | 21.4 (487) |
| ⩾5 | 24.4 (555) |
| Not stated | 0.5 (11) |
Also shown in table 2 are the places and number of times each dose of vitamin K may have been recorded. The places reported most often were neonatal records or notes (80.1%; 1818) and mothers' obstetric notes (73.4%; 1666). In only 10.6% (241) of jobs was vitamin K administration recorded once only, with each dose reported as recorded in five or more places by 24.4% (555) of midwives.
Reported recording practices for vitamin K administration (given or not given) in current jobs are shown in table 3. Of the 2271 midwives whose current job had an official policy, 99.3% reported that vitamin K was usually recorded if given, 93.6% that route of administration was also recorded, and 86.5% that a record was made when vitamin K was not given. However, there is some evidence of variation by policy type—“not given” was reported as recorded by 63.2% if the policy was to give vitamin K to babies at high risk only, by 85.6% if vitamin K was to be given to all babies by the same route, and by 91.0% if it was to be given to all babies but by differing routes.
Table 3.
Recording practices reported for current vitamin K policies (November 1998 to May 1999). Values are percentages (numbers)
| Recording practice | All policies (n=2271) | Vitamin K given to all babies
|
Vitamin K given only to babies at “high risk” (n=76) | |
|---|---|---|---|---|
| By the same route (n=1482) | By different routes (n=713) | |||
| Recorded if given: | 99.3 (2256) | 99.4 (1473) | 99.2 (707) | 100 (76) |
| Route recorded | 93.6 (2125) | 91.3 (1353) | 97.6 (696) | 100 (76) |
| Recorded if not given | 86.5 (1965) | 85.6 (1268) | 91.0 (649) | 63 (48) |
Implementation of historical policies
Details of 2179 previous jobs (held before 1990) were given in phase two; overall, only 8.5% (185) of these were reported as having no policy on vitamin K. However, midwives were unsure if there had been a policy for an additional 21.7% (473). Although for a minority of these jobs (14.4%) midwives were unable to remember the details of vitamin K administration, for most (85.6%) some details were given but midwives were unsure if it was an official policy.
The overall proportion of previous jobs reported to have definitely had official policies was 69.8% (1521/2179), but this increased gradually over the years from 50.2% (300/598) for those that ended in 1979 or earlier to 86.8% (613/706) for those that ended in 1990 or later. Of these 1521 jobs, policies were reported as always having been followed in 68.8%, a record was made when vitamin K was given in 90.9%, and a record was made when vitamin K was not given in 55.4% (table 4). The level of recording seems to have improved over time, but the likelihood that a policy was followed seems to have fallen.
Table 4.
Implementation practices of official policies on vitamin K administration in midwives' previous jobs (jobs held before 1990). Values are percentages (numbers)
| Year jobs ended
|
|||||
|---|---|---|---|---|---|
| All years (n=1521) | Before 1979 (n=300) | 1980-4 (n=239) | 1985-9 (n=369) | After 1990 (n=613) | |
| Policy always followed | 68.8 (1047) | 75.3 (226) | 69.9 (167) | 66.4 (245) | 66.7 (409) |
| Recorded if vitamin K given: | |||||
| Yes | 90.9 (1382) | 83.7 (251) | 87.4 (209) | 92.4 (341) | 94.8 (581) |
| Sometimes* | 3.6 (54) | 5.7 (17) | 5.0 (12) | 3.3 (12) | 2.1 (13) |
| No | 5.6 (85) | 10.7 (32) | 7.5 (18) | 4.3 (16) | 3.1 (19) |
| Recorded if vitamin K not given: | |||||
| Yes | 55.4 (843) | 39.3 (118) | 44.4 (106) | 58.5 (216) | 65.7 (403) |
| Sometimes* | 8.9 (135) | 9.0 (27) | 8.8 (21) | 8.1 (30) | 9.3 (57) |
| No | 35.7 (543) | 51.7 (155) | 46.9 (112) | 33.3 (123) | 25.0 (153) |
Recorded in some circumstances (for example, given by a different route, admission to special care baby unit, parental refusal).
Discussion
This survey of midwives differs from the two previous British surveys of vitamin K prophylaxis in several important ways.In the previous surveys information about vitamin K policies was obtained from postal questionnaires sent to each special care nursery listed by the Neonatal Nurses' Association. No data were collected on births outside these maternity units or on the implementation of policies, and it is not clear who in each unit completed the questionnaire.19,20 The present survey, by asking individual midwives to provide information, has collected data on how policies are interpreted by those who implement them, rather than on how they are interpreted by those who set them.
The response to phase one of this survey was higher than Asch et al reported as the mean for surveys of nurses, the closest comparison group (this survey 79%, Asch et al 61%); the response in phase two (62%) was comparable to the reported mean.21 More importantly, the distribution of midwives by health region was broadly similar in both phases to that of all midwives working in the NHS at the time the sample was selected.15–18
Current vitamin K policies
More than 97% of newborn babies are likely to receive some form of vitamin K routinely, if their parents consent; this is comparable to the 98% reported in a 1993 survey in the British Isles.19The downward turn reported in 1993 in the proportion receiving vitamin K intramuscularly does, however, seem to have been reversed, with levels reported here likely to be close to the 57% and 58% figures reported in 1988 and 1982, and higher than the 38% reported in 1993.19,20It is difficult to assess accurately the proportions receiving vitamin K orally and intramuscularly: numbers receiving it by each route under selective policies, with differing criteria for high risk, are unknown, and 11% of current policies actively encourage parental choice. There is no clear consensus on which babies should receive vitamin K intramuscularly.
Reasons reported in phase two for not giving vitamin K intramuscularly to babies who in some studies would be imputed as receiving it, if policy was selective (given only to babies at high risk)
Previous policies were simply guidelines
Wide interpretation of policies—midwives did not like giving babies injections
Baby in good condition at birth
Individual paediatricians had different policies
Baby admitted to postnatal ward—only given on neonatal unit
Baby admitted to general practitioner unit—only given on consultant unit
Confusion over policy
Neonatal vitamin K administration in the United Kingdom seems highly unusual in comparison with other drugs, given the variety of places and number of times each dose may be recorded. This phenomenon is not entirely new, however, and was noted in an earlier study that collected data retrospectively from maternity records.6
Imputation of vitamin K
It is not known whether previous policies are accurately recalled by current staff. It is, however, difficult to feel confident that they always are, given the variety of combinations of criteria for high risk reported for current policies. Only three out of 17 specified criteria are included in more than 50% of selective policies, with additional variation in how some criteria are defined. Although clinical judgment is mentioned as a criterion in only 1.8% of policies, details given by some midwives suggest that it plays a larger part—one example is making the distinction between difficult and easy instrumental deliveries. Judging such distinctions would be difficult for those collecting data many years later.
Interestingly, many midwives stressed that in their previous jobs it was the condition of the baby, rather than policy, that determined if vitamin K was given. The box lists other reasons stated for not giving vitamin K intramuscularly when the policy was that it should be given. Such comments may of course be biased, as not all midwives chose to add comments to the questionnaire. However, the comments support other findings reported here, and previous anecdotal evidence, that official policies were (and may still be) open to individual interpretation and were not always followed rigidly.
The purpose of clinical records is to document patient care, and variation in recording practices by policy type, especially if vitamin K was not given, reflects this. There have been changes over the years, but, for all time periods, if no written record was made the most likely reason is that vitamin K was not given.
Figure.
Distribution by health region of respondents in phase one (excluding midwives for whom health region not known) and of midwives in post in the NHS at 30 September 1998
Acknowledgments
We thank the midwives for enthusiastically sharing their knowledge and experience and Peter Hope and Pat Townshend for comments on an earlier draft of the paper.
Footnotes
Funding: Data collection was funded by a nursing research fellowship awarded to PA by the Smith and Nephew Foundation. Other aspects of the study were funded by the Leukaemia Research Fund.
Competing interests: None declared.
References
- 1.Golding J, Greenwood R, Birmingham K, Mott M. Childhood cancer, intramuscular vitamin K, and pethidine given during labour. BMJ. 1992;305:341–346. doi: 10.1136/bmj.305.6849.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ekelund H, Finnstrom O, Gunnarskog J, Kallen B, Larsson Y. Administration of vitamin K to newborn infants and childhood cancer. BMJ. 1993;307:89–91. doi: 10.1136/bmj.307.6896.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klebanoff MA, Read JS, Mills JL, Shiono PH. The risk of childhood cancer after neonatal exposure to vitamin K. N Engl J Med. 1993;329:905–908. doi: 10.1056/NEJM199309233291301. [DOI] [PubMed] [Google Scholar]
- 4.Olsen JH, Hetz H, Blinkenberg K, Verder H. Vitamin K regimens and incidence of childhood cancer in Denmark. BMJ. 1994;308:895–896. doi: 10.1136/bmj.308.6933.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Von Kries R, Göbel U, Hachmeister A, Kaletsch U, Michaelis J. Vitamin K and childhood cancer: a population based case-control study in Lower Saxony, Germany. BMJ. 1996;313:199–203. doi: 10.1136/bmj.313.7051.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ansell P, Bull D, Roman E. Childhood leukaemia and intramuscular vitamin K: findings from a case-control study. BMJ. 1996;313:204–205. doi: 10.1136/bmj.313.7051.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McKinney PA, Juszczak E, Findlay E, Smith K. Case-control study of childhood leukaemia and cancer in Scotland: findings for neonatal intramuscular vitamin K. BMJ. 1998;316:173–177. doi: 10.1136/bmj.316.7126.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Passmore SJ, Draper G, Brownhill P, Kroll M. Ecological studies of relation between hospital policies on neonatal vitamin K administration and subsequent occurrence of childhood cancer. BMJ. 1998;316:184–189. doi: 10.1136/bmj.316.7126.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Passmore SJ, Draper G, Brownhill P, Kroll M. Case-control studies of relation between childhood cancer and neonatal vitamin K administration. BMJ. 1998;316:178–184. doi: 10.1136/bmj.316.7126.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parker L, Cole M, Craft AW, Hey EN. Neonatal vitamin K administration and childhood cancer in the north of England: retrospective case-control study. BMJ. 1998;316:184–193. doi: 10.1136/bmj.316.7126.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barton JS, McNinch AW, Tripp JH. Oral vitamin K prophylaxis and frequency of late vitamin K deficiency bleeding. Lancet. 1994;343:1168. doi: 10.1016/s0140-6736(94)90277-1. [DOI] [PubMed] [Google Scholar]
- 12.National Childbirth Trust. Parents' rights denied over vitamin K. Report to the Department of Health. London: NCT; 1994. [Google Scholar]
- 13.Department of Health. Vitamin K for newborn babies. Letter from the chief medical and nursing officers of England to all doctors, regional directors of public health, district nursing officers, midwives and health visitors. London: Stationery Office; 1998. . (PL/CNO/998/4.) [Google Scholar]
- 14.Royal College of Midwives. Position paper 13b: vitamin K. RCM Midwives Journal. 1999;2(8):252–253. [Google Scholar]
- 15.Department of Health. NHS hospital and community health services non-medical workforce census England: 30 September 1998. Detailed results. Leeds: NHS Executive; 1999. [Google Scholar]
- 16.Scottish health statistics 2000. Edinburgh: ISD Scotland; 2000. www.show.scot.nhs.uk/isd/Scottish_Health_Statistics/SHS2000/home.htm :table P3.8. on www.show.scot.nhs.uk/isd/Scottish_Health_Statistics/SHS2000/home.htm (accessed 23 March 2001). (accessed 23 March 2001). [Google Scholar]
- 17.Health Statistics and Analysis Unit, National Assembly for Wales, personal communication, 2000.
- 18.Project Support Analysis Branch, Northern Ireland Assembly, personal communication, 2000.
- 19.Barton JH, Tripp JS, McNinch AW. Neonatal vitamin K prophylaxis in the British Isles: current practice and trends. BMJ. 1995;310:632–633. doi: 10.1136/bmj.310.6980.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Handel J, Tripp JH. Vitamin K prophylaxis against haemorrhagic disease of the newborn in the United Kingdom. BMJ. 1991;303:1109. doi: 10.1136/bmj.303.6810.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]