Abstract
A dysfunction of cortical and limbic GABAergic circuits has been postulated to contribute to multiple neurodevelopmental disorders in humans, including schizophrenia, autism, and epilepsy. In the current paper, I summarize the characteristics that underlie the great diversity of cortical GABAergic interneurons and explore how the multiple roles of these cells in developing and mature circuits might contribute to the aforementioned disorders. Furthermore, I review the tightly controlled genetic cascades that determine the fate of cortical interneurons and summarize how the dysfunction of genes important for the generation, specification, maturation, and function of cortical interneurons might contribute to these disorders.
1. Introduction
The exquisite complexity of cognitive functions stems from tightly regulated interactions between distributed cortical networks performing precise neural computations. GABAergic inhibitory interneurons (INs), which represent a minority of neocortical neurons (20% in rodents [1]), play a crucial role in these cortical circuits. GABAergic INs shape the responses of pyramidal cells to incoming inputs, prevent runaway excitation, refine cortical receptive fields, and are involved in the timing and synchronisation of population rhythms expressed as cortical oscillations [2–9]. Consequently, disruption of cortical GABAergic IN function has been linked to various neurodevelopmental disorders, including epilepsy, mental retardation, autism, and schizophrenia [10–15].
Cortical INs are diverse in terms of their anatomical laminar distribution, histochemical marker expression, intrinsic physiological properties, and connectivity (Figure 1) [5, 6, 9, 16–22]. This heterogeneity is characterized by the expression of specific combinations of ion channels, receptors, and membrane cell adhesion molecules [7]. These specific protein expression profiles are the result of tightly controlled genetic pathways that regulate cortical IN identity [8, 23–29]. Anomalies in these genetic pathways might therefore underlie some of the neurodevelopmental and neurocognitive disorders seen in humans. In the current paper, I will give an overview of cortical IN diversity, summarise the various roles of cortical INs in neuronal circuit development and function, review the genetic pathways involved in specifying cortical GABAergic IN diversity, and explore the pathological correlates of genetic anomalies leading to interneuron dysfunction in rodents and humans. As the current paper focuses on neocortical INs, readers are directed to other sources for a broader description of other GABAergic populations, including those of the amygdala, striatum, hippocampus, thalamus, and olfactory bulbs, which also participate in the corticolimbic and corticosubcortical circuits involved in cognition and emotional processing [7, 30–40].
Figure 1.
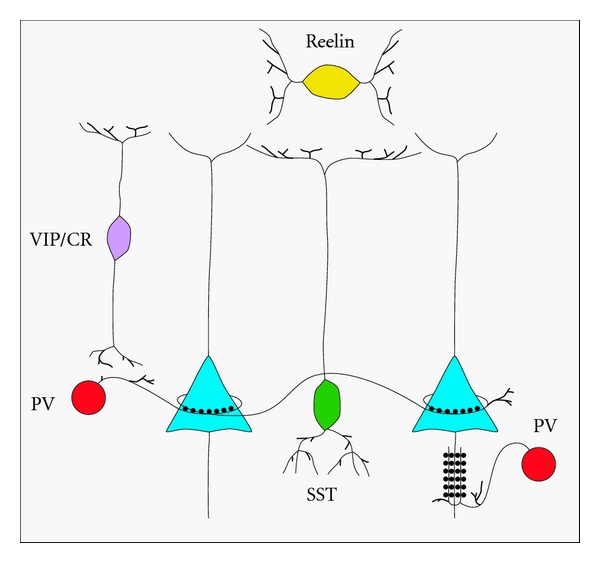
Interneuron diversity. Interneurons are diverse in terms of their histochemical profile, morphology, physiological properties, and connectivity. In this schematic representation, parvalbumin-positive (PV) interneurons (red) include basket cells forming perisomatic contacts on adjacent pyramidal cells (dark blue), as well as chandelier cells that target the pyramidal cell axon initial segment. Somatostatin-positive (SST) interneurons include Martinotti cells that contact pyramidal cell dendrites in layer I. Vasointestinal peptide (VIP) and calretinin (CR) double-positive bitufted interneurons target pyramidal cells and other interneurons. Neurogliaform cells, marked with reelin, are the most abundant interneurons in layer I and provide tonic GABAergic inhibition via volume transmission of GABA.
1.1. Diversity of Cortical GABAergic Interneurons Subtypes and Roles
Neocortical GABAergic INs are heterogeneous, and different subtypes of INs have different spatial and temporal origins. As a group, neocortical INs are derived from transient ventral telencephalic structures referred to as the ganglionic eminences [27, 29, 41–46] as well as from the preoptic area [47]. The medial ganglionic eminence (MGE) produces approximately 70% of neocortical INs, including the parvalbumin-positive (PV) fast-spiking interneurons and the somatostatin-positive (SST) interneurons, which represent 40% and 30% of all neocortical INs, respectively [27, 46, 48]. By contrast, the caudal ganglionic eminence (CGE) gives rise to the remaining 30% of neocortical INs, a more heterogeneous group of cortical INs that share the unique expression of 5HT3A ionotropic serotoninergic receptors, rendering them highly responsive to the neuromodulatory effects of serotonin [9, 43, 46, 48, 49]. A majority of CGE-derived interneurons belong to either the reelin-positive multipolar population (including the late-spiking neurogliaform cells), the vasointestinal-peptide- (VIP-) positive bitufted population (including a calretinin- (CR)-positive population), or the VIP-positive, calretinin-negative bipolar population. Finally, the preoptic area contributes a small portion of neocortical INs (<3%) that are not labelled by the usual interneuron markers mentioned above [47]. The lateral ganglionic eminence (LGE) mainly produces olfactory bulb and amygdalar INs, as well as striatal and nucleus accumbens medium spiny neurons, but is generally thought not to give rise to cortical INs [23, 33, 38, 41, 50, 51]. Different subtypes of cortical INs are identified based on their immunohistochemical, morphological, physiological, and connectivity properties, and they mediate different functions in mature networks as detailed below.
1.2. Parvalbumin-Positive Basket Cells
PV-positive interneurons include the perisomatically targeting basket cells and the less abundant axon-initial segment-targeting chandelier cells. PV-positive basket cells can be further divided according to various morphological characteristics, including somatic diameter, firing properties, and extent of dendritic and axonal arborisation [5, 9, 52, 53]. As a group, PV-positive basket cells display many characteristics which render them one of the fastest and most reliable sources of inhibition in the cortex. They exhibit low input resistance, fast membrane kinetics, brief action potentials with large afterhyperpolarisation, and minimal spike adaptation and are able to sustain high frequency firing rates [5, 18, 19, 21, 44, 52, 54]. These fast kinetics are partly due to their expression of Kv3 voltage-gated potassium channels [52, 55–59], which ensure quick repolarisation and termination of action potentials. In addition, PV-positive fast-spiking cells mediate fast reliable neurotransmission, as they rely mainly on P/Q-type presynaptic Ca2+ channels for tight coupling between action potentials and neurotransmitter release [60–63]. Furthermore, these PV-positive basket cells might be able to buffer calcium more efficiently, as they express high levels of Ca2+-binding proteins, including parvalbumin and calbindin. It is possible that this expression of Ca2+-binding proteins renders these cells more resistant to Ca2+-induced excitotoxicity in the face of high firing rates.
PV-positive INs are the main inhibitory target of thalamocortical projections in the cortex. In addition, PV-positive basket cells form intricate nests of synaptic contacts on the soma of adjacent pyramidal cells, giving them rapid control over the excitability of their pyramidal cell targets. These INs are therefore well positioned to provide strong and fast feedforward inhibition to adjacent pyramidal cells, limiting the time window for temporal summation of excitatory inputs and spike generation within populations of pyramidal cells. This feature sharpens the cortical response and prevents runaway excitation following thalamocortical excitation [64–68].
In addition, PV-positive basket cells are highly interconnected with one another through both chemical and electric synapses (gap junctions), creating a vast web of synchronously active INs [69, 70]. This network of inhibitory INs triggers and maintains high-frequency gamma oscillations within ensembles of cortical pyramidal cells [69, 71–77]. In support of this, the loss of connexin32, which forms gap junction connections between PV-positive INs, results in the partial loss of task-induced gamma oscillations [78]. Gamma oscillations are important for the maintenance of attention, working memory, and the refinement of executive functions in humans and rodents [79–83]. Therefore, PV-positive interneuron dysfunction has been postulated to underlie the loss of gamma oscillations in schizophrenic patients displaying working memory and executive function abnormalities [14, 82, 84, 85].
1.3. Parvalbumin-Positive Chandelier Cells
Like PV-positive basket cells, PV-positive chandelier cells display brief nonadapting trains of action potentials upon stimulation and are able to sustain high frequency firing rates [17, 86, 87]. They are characterised morphologically by their cartridges of vertically oriented candlestick-like axonal arbors [88–90]) forming synapses on the axon initial segment (AIS) of pyramidal cells [89, 91]. Chandelier cells are unusual among interneurons in that their output has been postulated to be excitatory rather than inhibitory. Indeed, the stimulation of chandelier cells triggers depolarisations in target pyramidal cells in the cortex and dentate gyrus [92–95]. This has been attributed to the high concentration of chloride and elevated GABAA reversal potential at the AIS, due to efficient Cl− import by the NKCC1 transporter in the absence of the KCC2 transporter (see below) [92, 93]. However, it is still unclear whether such depolarizing responses are obligatorily excitatory [95]. Furthermore, in other circuits, such as in the CA1 region of the hippocampus, chandelier cells appear to trigger hyperpolarising responses [96]. Overall, the net effect of chandelier cells might be dependent on the local state of network activity and on the particular ion channel composition of local pyramidal cells in different brain regions. In vivo, chandelier cells might be involved in the generation of specific oscillatory activities as they fire immediately before hippocampal pyramidal cells during sharp-wave-associated ripples [97].
1.4. Somatostatin-Positive (SST) Interneurons
Somatostatin-positive interneurons, including Martinotti cells and non-Martinotti cells, are heterogeneous in terms of their immunohistochemical profile (variable colabelling with calretinin and calbindin), morphology (multipolar, bipolar, or unipolar), axonal projections (most target pyramidal cell dendrites in layer I but some project locally within their cortical layer), and intrinsic electrophysiological properties [9, 45, 98–100]. A majority of SST interneurons (including the Martinotti cells) share some physiological characteristics, including a low spike threshold, prominent after-hyperpolarisation, and spike rate adaptation. However, these cells differ in their spiking pattern at threshold (regular versus bursting), especially when fired from hyperpolarized step currents [17, 98, 99]. In general, compared to fast-spiking basket cells, SST-positive interneurons tend to be more excitable: they display a lower spike threshold and have a higher resting membrane potential [101]. One exception to this rule is a population of non-Martinotti cells, which have a high firing threshold, higher firing rate, shorter spike half width, and lower input resistance [45, 99]. These cells have been mostly described in layer 4 of the cortex and are preferentially labelled in the X94 GAD67-GFP transgenic line [9, 99].
SST-positive Martinotti cells are found across cortical layers II-VI but are most abundant in cortical layer V. They project vertically towards layer I where they contact pyramidal cell dendrites and extend multiple axonal collaterals towards adjacent cortical columns [19, 102, 103]. Martinotti cells regulate pyramidal cell excitability by controlling the dendritic summation and integration of synaptic inputs and sharpening the coding of stimulus intensity [104]. Furthermore, as their connectivity is simultaneously divergent, convergent, and recurrent, they mediate disynaptic inhibition between interconnected pyramidal cells as well as recurrent feedback inhibition onto presynaptic pyramidal cells [105, 106]. They are therefore well suited to prevent excessive and recurrent excitation within cortical networks. Furthermore, they are increasingly recruited by sustained stimulation, owing to the fact that the synapses that they receive from pyramidal cells are in most cases facilitating [101, 107]. This renders them good candidates to dampen excitation during high activation states. Dysfunction of somatostatin cells has therefore been postulated to underlie some forms of experimental or poststatus epilepticus seizure disorders [108].
Because of their expression of low-threshold voltage-gated calcium channels and persistent sodium currents, about 40% of SST cells display intrinsic bursting abilities and might act as pacemaker cells, thereby triggering particular cortical oscillations [224]. Indeed, SST-positive cells, which are highly interconnected via gap junctions, tend to oscillate spontaneously in the theta range (3–9 Hz) when stimulated electrically or with cholinergic agonists in vitro [101]. They could therefore be involved in pacing cortical pyramidal cells in the theta range.
1.5. Vasoactive Intestinal Peptide- (VIP-) Positive Interneurons
CGE-derived interneurons tend to populate more superficial cortical layers than MGE-derived interneurons. Approximately 40% of CGE INs express VIP, and these cells tend to be enriched in layers II/III [19, 46, 48, 225, 226]. VIP-positive INs are diverse morphologically, histochemically, and physiologically [9]. The most abundant type are the bitufted VIP+ INs that tend to colabel with CR [46, 48], display an irregular-spiking firing pattern near threshold [18, 46, 48, 49, 227], and send a downward projecting axon towards deeper cortical layers. The second most abundant type is the VIP+, CR− bipolar cells, which display a fast adapting firing pattern [44, 46, 48, 227] and send extensively branched projections both locally and towards deep cortical layers. Due to their high input resistance, VIP INs tend to be highly excitable [18, 46, 48]. They have been shown to target pyramidal cell dendrites and somata [17], but some subsets appear to target other interneurons more preferentially [228–230]. The precise function of VIP interneurons in cortical networks remains to be determined. However, their physiological characteristics and diverse synaptic targets render them well suited to rapidly modulate the interactions between pyramidal cells and MGE-derived interneurons. Furthermore, as they receive strong input from pyramidal cells in layers II-III [231], which also receive input from pyramidal cells in other functionally connected cortical areas, VIP interneurons might be important in regulating cross-cortical communication (i.e., sensorimotor modulation where inputs from the sensory cortex modulate the output of cortical motoneurons).
1.6. Neurogliaform Cells
Neocortical neurogliaform cells exist in all cortical layers but are the most abundant GABAergic population in superficial layer I [46, 48]. They express reelin (as well as alpha actinin 2 in the rat [103, 232]), but not VIP or SST [9, 46]. They are morphologically distinct as they have multiple radially oriented dendrites extending from a small round soma, as well as a finely branched dense axonal plexus typically extending well beyond the dendritic tree, giving them a spider web appearance [19, 233]. Neurogliaform cells display late-spiking firing patterns with spike accommodation during sustained depolarisations [19, 44, 45, 48, 234]. They have been shown to elicit slow long-lasting inhibitory events (IPSPs) in pyramidal cells and other interneurons by activating both GABAA and GABAB receptors after nonsynaptic volume release of GABA [233–235]. Some of this tonic inhibition is thought to be mediated through the activation of delta subunit-containing GABAA receptors, which are modulated by neurosteroids [235]. This effect might underlie the antiepileptic effect of steroids used to treat pharmacoresistant epilepsies [236, 237]. Furthermore, neurogliaform cells are extensively interconnected by electrical gap-junction synapses but also contact most other interneurons subtypes via similar electrical synapses [238–240]. They are therefore well suited to shape synchronous cortical oscillations. Finally, some neurogliaform cells release nitric oxide, a potent vasodilator, and may therefore play a role in the neurovascular adjustment of blood flow in the face of cerebral hypoperfusion (i.e., strokes, shock, etc.) [241, 242].
2. The Development of Cortical Interneurons Depends on Tightly Regulated Genetic Cascades
Cortical interneurons originate in the ventricular zone of the ventral telencephalic ganglionic eminences [41, 43, 243], migrate tangentially up to the cortex [218, 244], and reach their final destination after radial migration across cortical layers. This is quite distinct from cortical pyramidal cells, which originate from the cortical ventricular zone, migrate radially, and reach their final position after a brief bout of tangential migration [42, 245]. The ganglionic eminences are divided into three different subdomains, the medial (MGE), caudal (CGE), and lateral (LGE) ganglionic eminences, which produce distinct subtypes of interneurons in a temporally dynamic fashion [44–46, 246]. Cortical interneurons originate from the MGE and CGE [41, 43, 243], as well as from the preoptic area [47]. Although this has been debated, it is generally believed that the LGE does not give rise to cortical interneurons, instead generating medium spiny neurons of the striatum, nucleus accumbens, and olfactory tubercules, as well as olfactory bulb and amygdalar interneurons [23, 33, 38, 41, 50, 51].
The genetic code that governs the generation and specification of cortical interneurons has been extensively studied over the last decade (Figure 2). The Dlx homeobox genes, including Dlx1/2 and Dlx5/6, encode a family of transcription factors crucial for the generation, specification, and migration of all interneurons. The proneural gene mammalian achaete-scute homolog 1 (Mash1), which encodes a basic helix-loop-helix transcription factor, is also crucial for these processes. These genes are broadly expressed across the subpallial subventricular zone (SVZ) of the ganglionic eminences [218, 247–249]. In mice carrying compound Dlx1 and Dlx2 knock-out mutations, GABAergic interneurons fail to migrate out of the ganglionic eminences, resulting in striking reductions in cortical and olfactory bulb interneurons as well as abnormal striatal differentiation [23, 219]. Similar results are seen in mice lacking Mash1 [250]. Interestingly, Dlx1/2 gene dosage appears to be important, as interneurons in mice carrying a Dlx1−/−; Dlx2+/− genotype displays normal tangential migration to the cortical plate, but shows altered laminar positioning and simplified morphology (long axons and dendrites with few branches) [220]. Furthermore, Dlx1−/− mutants display selective defects in the dendritic morphology of SST+/CR+ interneurons, with a progressive loss of these interneurons in the postnatal brain, resulting in spontaneous seizures [221].
Figure 2.
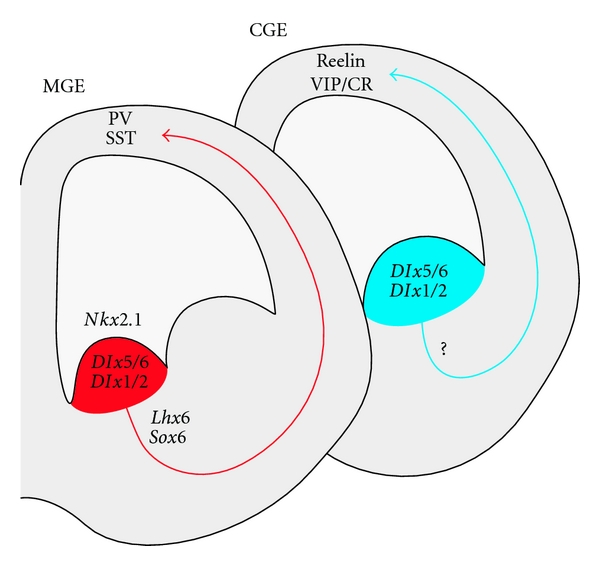
Genetic cascade governing cortical interneuron generation. Corticolimbic interneurons originate in the medial and caudal ganglionic eminences (MGE and CGE). The homeobox transcription factors Dlx5/6, Dlx1/2 and the proneural gene Mash1 (not shown) are expressed throughout the ganglionic eminences and are required for the generation of all GABAergic interneurons. The MGE generates parvalbumin-positive (PV) basket cells and chandelier cells, as well as somatostatin-positive (SST) cells (including Martinotti cells). These rely on the sequential expression of Nkx2.1, Lhx6, and Sox6 for proper specification and maturation (see text). The genetic cascade governing the specification of CGE-derived interneurons has not been fully elucidated yet, but Nkx6.2 and Gsh2 are expressed in the CGE and might be important players (see text).
The MGE and CGE give rise to distinct cortical interneuronal populations [25, 41]. The MGE generates the parvalbumin-positive (fast-spiking basket cells and chandelier cells) and somatostatin-positive interneurons (including Martinotti cells) [8, 9, 22, 25, 41, 44, 45, 251]. The specification of these interneurons relies on the expression of NK2 homeobox 1 (Nkx2-1) [22, 222]. The loss of Nkx2-1 as interneuron progenitors are exiting their last mitotic division in the ganglionic ventricular zone leads to respecification of these cells into CGE-type interneurons (of all major subtypes) and the consequent absence of cortical PV and SST interneurons [22]. Interestingly, PV interneurons originate mainly from the ventral MGE whereas SST cells are preferentially produced by the dorsal MGE [251, 252], a phenomenon likely mediated by the combinatorial expression of particular transcription factors within different subdomains of the MGE [252, 253], resulting in part from a gradient of SHH expression [254]. Furthermore, a portion of the dorsal MGE and the MGE-CGE sulcus region is delineated by the expression of the homeodomain transcription factor Nkx6-2, which partially overlaps with Nkx2-1. This area gives rise to the subgroup of somatostatin cells (about 30%) that coexpress somatostatin and calretinin and display a delayed nonfast spiking firing pattern [251, 255].
As they leave the ventricular zone, MGE-derived interneurons begin to express the transcription factor LIM homeobox protein 6 (Lhx6), which is expressed into adulthood [26, 222, 251, 256, 257]. Lhx6 is required for proper specification and migration of MGE-derived interneurons, and the loss of Lhx6 results in misspecified hippocampal and cortical INs. These cells retain their GABAergic identity, but they fail to express PV or SST and are mislocalised within the neocortex [257]. Indeed, Lhx6 loss disrupts the correct expression of downstream effectors known to be important for IN migration, including v-erb-a erythroblastic leukemia viral oncogene homolog 4 (ErbB4), C-X-C chemokine receptor type 4 (CXCR4) and type 7 (CXCR7), and aristaless-related homeobox (ARX) [26, 258].
Downstream of Lhx6 is SRY-box 6 (Sox6), another transcription factor expressed by MGE-derived interneurons as they initiate their tangential migration. Sox6 is required for the proper laminar distribution and maturation of MGE-derived interneurons [28]. Its loss results in mislocalised MGE-derived INs that accumulate ectopically in layer I and deep layer VI, failing to adequately populate cortical layers II–V [28, 223]. Furthermore, these cells fail to express their mature markers, leading to a striking loss of cortical PV- and SST-expressing cells (PV being more severely affected). Although they remain correctly specified as MGE-INs, as evidenced by their morphology, electrophysiological properties, and expression of GABA, the resulting mutant cells fail to acquire mature intrinsic properties. For instance, PV-cells are unable to sustain the high frequency firing rates expected from these cells by P17-18 [28]. This results in a severe developmental epileptic encephalopathy with early lethality during the 3rd postnatal week [28].
As detailed above, the CGE produces a great variety of cortical interneurons, which populate the more superficial cortical layers. CGE-derived INs include all VIP- and reelin-positive cells, including the calretinin bipolar and neurogliaform cells, as well as multiple smaller subgroups of cortical interneurons, which are distinguishable by their morphological and physiological properties [25, 43, 44, 46]. The master regulatory genes for CGE cell-fate determination have yet to be fully determined. However, some transcription factors are expressed in both the CGE and dorsal MGE, including Nkx6-2 and CoupTF1/2, and might play a role in the specification of CGE interneurons [255].
3. GABAergic Interneurons Play Fundamental Roles in Developing Circuits
GABA signalling is crucial during embryogenesis for both neural and nonneural populations of cells [259]. In fact, early GABAergic signalling has been shown to affect neurogenesis, differentiation, migration, and integration of developing neurons into neuronal circuits [260, 261]. Indeed, GABAA receptors are expressed early in newborn pyramidal neurons, which receive GABAergic inputs long before forming excitatory synapses [262, 263]. GABA is excitatory in immature neurons due to the high level of NKCC1 expression. NKCC1 increases the intracellular concentration of Cl−, shifting the GABA equilibrium potential (EGABA) to more depolarised levels, thereby leading to an extrusion of negatively charged chloride anions upon activation of GABAA receptors and a depolarisation of the cell membrane [264]. With time, the progressive expression of another chloride transporter, KCC2, lowers the baseline intracellular concentration of Cl− and underlies the developmental switch of EGABA in favour of an inhibitory effect of GABA in mature neurons [265, 266].
This developmental switch is important in controlling the migration, final position, and morphological maturation of interneurons. Tangentially migrating interneurons have been shown to release GABA in a nonvesicular manner [267]. GABA then acts synergistically with AMPA/NMDA receptor-mediated currents to promote tangential migration of interneurons as long as it is depolarising. However, the gradual expression of KCC2 shifts the reversal potential of GABA and the resulting hyperpolarisation acts as a stop signal to arrest the migration of cortical interneurons [268]. Interestingly, interneurons derived from the MGE, which reach their final layer earlier than CGE-derived interneurons, also appear to express KCC2 earlier than CGE cells born simultaneously [246]. KCC2 might therefore regulate some of the differences observed in the laminar distribution of interneurons originating from different sources.
Furthermore, GABA-mediated depolarisations have recently been shown to promote excitatory synapse formation by facilitating NMDA receptor activation in cortical pyramidal neurons [269]. Blocking these GABA-mediated depolarisations, by in utero knock-down of NKCC1 or with the NKCC1 antagonist bumetanide, results in decreased numbers of functional excitatory synapses [269]. These manipulations also lead to altered cell morphologies, including thinner apical dendrites, simplified dendritic trees, and decreased dendritic spine densities [269]. These detrimental effects of bumetanide appear to be long-lasting, as they persist in the adult cortex and are associated with developmental delay and altered prepulse inhibition in adult mice [270]. Premature overexpression of KCC2 leads to similar dendritic anomalies in cortical pyramidal cells as those reported after blocking NKCC1 [271].
In summary, GABA plays fundamental roles at different stages of neuronal development, affecting migration, maturation, and synapse formation of both pyramidal cells and interneurons. Furthermore, the precise effect of GABA postsynaptically is dependent on the intracellular concentration of chloride, which is developmentally regulated via the expression of various chloride cotransporters and which varies depending on the age of the cells.
4. Interneurons and Early Network Activities
GABergic INs serve diverse functions in developing and in mature networks. As detailed above, they provide local circuit inhibition and participate in the genesis and organisation of specific mature neocortical and limbic oscillations, which in turn modify how local circuits respond to incoming signals. In addition, GABAergic interneurons are critical for the proper maturation and wiring of developing networks [8, 272], as well as for the regulation of critical period experience-dependent cortical plasticity [132, 273–276]. In particular, they have been involved in the generation of some of the early postnatal cortical and limbic oscillatory activities appearing during the first postnatal week in rodents. These synchronised network activities are thought to be important for the proper morphological maturation of excitatory and inhibitory neurons, including for the development of complex dendritic trees and synaptic contacts.
The first postnatal activities recorded are the synchronous plateau assemblies (SPAs), which are prolonged gap-junction-mediated calcium plateaus appearing between P0-P3 in the rat hippocampus [277] and neocortex [278]. The cellular substrates that drive these SPAs are still unknown, but it is interesting to note that some subsets of cortical interneurons are extensively interconnected through gap junctions [69, 70, 101] and could contribute to the generation of SPAs. In the cortex, SPAs progressively coexist with cortical early network oscillations (cENOs) between P0-P5. cENOs are infrequent (0.01 Hz) synaptically driven calcium events with slow kinetics that depend on glutamatergic AMPA- and NMDA-mediated synaptic activity and that cause sustained depolarisation of large groups of neurons.
These early network activities are then replaced by the giant depolarising potentials (GDPs) recorded in the hippocampus [279] and neocortex [278] between P6-P8. GDPs are much more frequent (mean 0.1 Hz), consist of fast calcium events, and are entirely dependent on GABAergic synaptic activity (as they are blocked by the GABAA antagonist bicuculline). In the hippocampus, GDPs have been shown to result from the spontaneous activity of a subset of highly connected GABAergic neurons, the hub neurons, that pace whole populations of pyramidal cells in a rhythmic fashion [280]. These hub cells receive more excitatory inputs (EPSPs), display a lower action potential threshold, and have a wider axonal arborisation than neighbouring local GABAergic interneurons [280]. These characteristics render them particularly well suited to generate waves of activity in wide sets of neurons upon stimulation by incoming inputs. GDPs coincide with a phase of active synaptogenesis within the developing neocortical and limbic circuits. It is therefore likely that a selective dysfunction of GABAergic interneurons in these early developmental steps might alter the process of synapse formation, either by decreasing these early network activities or by exerting more direct effects on the postsynaptic membrane.
In summary, interneurons participate in the genesis of early network activities which provide critical input for the normal maturation and plasticity of corticolimbic networks. In the mature brain, they provide local circuit inhibition and govern the onset and maintenance of some of the corticolimbic oscillations. These combined functions underlie the extensive impact of interneuronopathies on neurodevelopment and cognition.
5. Interneuronopathies and Neurodevelopmental Disorders
Interneuron anomalies have been suspected to underlie a variety of neurodevelopmental disorders in humans, including epilepsy, autism, and schizophrenia [14, 15]. This hypothesis stemmed from the observation of decreased GAD67 expression in postmortem brain tissue from affected individuals [110]. Later genetic studies also supported this hypothesis as variants in the GAD67 promoter area were discovered in patients with childhood-onset schizophrenia [113] or bipolar disorder [281]. Interestingly, many other genes linked to neuropsychiatric disease have since been shown to be preferentially expressed in developing cortical interneurons in mice [282]. It is therefore appealing to consider the possibility that genetic anomalies known to affect the development or function of interneurons in mice might be involved in neuropathologies in humans. Although genetic anomalies may manifest differently in mice and humans due to differences in expression patterns or compensation by other genes across species, alterations in highly conserved genetic pathways or disturbances in fundamental physiological processes might translate similarly in humans and mice. Furthermore, a host of environmental factors will likely modify the disease expression in these highly heterogeneous and likely polygenic pathologies. An exhaustive review of the genetic causes of schizophrenia, autism, and epilepsy is beyond the scope of this paper, but we will attempt to summarize some of the compelling evidence pointing to the roles of GABAergic neurons in these disorders.
5.1. Interneuron Development in Humans
Human GABAergic interneurons appear to be highly diverse as initially recognized by Ramon y Cajal [283, 284], with a similar array of PV-positive basket cells, PV-positive chandelier cells, SST-positive Martinotti cells, VIP-CR bitufted cells, VIP bipolar cells, and neurogliaform cells as that described in other species [284, 285]. However, the relative proportion of these various populations varies across species [286]. The superficial cortical layers II-III are considerably larger in the human cortex, presumably underlying some of the enhanced intercortical connectivity mediating higher brain functions in primates. Consequently, CR-positive double-bouquet INs appear to be considerably more numerous in the human cortex [284, 285]. Furthermore, although most cortical GABAergic interneurons develop in the ventral ganglionic eminences in humans, a proportion of cortical INs appear to originate from the cortical ventricular zone [284, 287–289]. Nonetheless, similarities do exist with regards to the molecular pathways involved in cortical interneuron genesis in humans and rodents, with preservation of some of the same fundamental genes including Mash1, Dlx1/2, Nkx2-1, and Lhx6 [288, 290–293].
5.2. Interneurons and Schizophrenia
Schizophrenia is a chronic psychiatric condition that combines neurocognitive dysfunctions (i.e., delusions, hallucinations, and disorganisation of thought), negative symptoms (i.e., flat affect, avolition, and alogia), and social or occupational deterioration (i.e., altered social interactions, deterioration in personal hygiene, and inability to self-sustain) [294]. This is accompanied by more specific cognitive impairments such as abnormalities in perception, inferential thinking, volition, linguistic fluency, attention, executive functions (planning), and working memory [295, 296].
The involvement of interneurons in the pathophysiology of schizophrenia was suggested when the number of prefrontal cortical GAD67-expressing cells was found to be decreased in autopsy specimens from schizophrenic patients [109, 110]. There is no net loss of cortical PV-positive interneurons or calretinin-positive interneurons in schizophrenic cortices, as the total number of cells stained for either marker is preserved [111, 112]. However, there appears to be a selective downregulation of GAD67 in PV-positive interneurons in schizophrenic brains [112]. Furthermore, the level of parvalbumin expression in these cells is decreased [112]. As both parvalbumin and GAD67 expression are known to be regulated by cortical activity [297, 298], these findings could reflect secondary changes in response to altered levels of cortical activity in schizophrenic patients. Indeed, two schizophrenia susceptibility genes encoding the trophic factor neuregulin 1 (NRG1) and its receptor ErbB4 (ERB4) [117–121] have been shown to facilitate activity-dependent GABA release from PV-positive basket cells in the mouse prefrontal cortex [299]. Selective loss of ErbB4 in PV cells causes a disinhibition of prefrontal pyramidal cells and results in a schizophrenia-like phenotype in mice [126]. In addition, the specific expression of ErbB4 in PV cells is required for neuregulin-1-dependent regulation of hippocampal long-term potentiation [127], which is altered in schizophrenic patients. Interestingly, hypostimulation of PV-positive basket cells via selective ablation of the NR1 subunit of the NMDA receptors in these cells resulted in schizophrenia-like behaviors (working memory deficits, impaired prepulse inhibition, locomotor hyperactivity, and anxiety) and decreased PV and GAD67 expression in PV basket cells in a mouse model of schizophrenia [128]. Therefore, hypofunction of prefrontal PV INs, either through a primary dysfunction of these cells or a decreased excitatory drive to these cells, appears to result in behavioural consequences in mice, which recapitulate aspects of the phenotype observed in schizophrenic patients.
Additionally, other genetic anomalies found in schizophrenic patients that are predicted to affect cortical maturation more broadly appear to impact interneuron maturation and GAD67 expression. For instance, brain-derived neurotrophic factor (BDNF) is normally released in an activity-dependent fashion from pyramidal cells and was shown to regulate the maturation of GABAergic INs [129]. Both BDNF and its receptor TrkB have been found to be downregulated in the prefrontal cortex of schizophrenic patients [122–124]. Knock-out mice for both BDNF and TrkB display behavioral anomalies and a decrease in the synaptic expression of GAD67/GABA [130, 131]. Similarly, the neural cell adhesion molecule NCAM, important for neuronal morphological maturation and synapse formation, requires the addition of a polysialic acid (PSA) moiety to function properly. The activity-mediated expression of PSA has been shown to regulate PV-positive basket cell maturation and determine critical-period plasticity [132]. Interestingly, this PSA-NCAM coupling has been reported to be decreased in hippocampal specimens from schizophrenic patients [125], which would suggest abnormalities in interneuron maturation and cortical plasticity.
Another interesting hypothesis is that PV-positive chandelier cells might be affected in schizophrenic brains. Indeed, a specific loss of more than 40% of the axonal cartridges (the GAT-1 positive axonal branches from chandelier cells which contact the axon initial segments of pyramidal cells) has been demonstrated in the prefrontal cortex of schizophrenic patients [114, 115]. This is accompanied by enhanced expression of the alpha2 GABAA receptor subunit on the axon initial segment of pyramidal cells, likely as a compensatory mechanism for the decreased input from chandelier cells [300]. However, since chandelier cells are possibly excitatory [94, 95], the net effect of these structural changes on local cortical excitability is uncertain. More recently, the levels of SST, NPY, and CCK were shown to be decreased in a microarray analysis of prefrontal cortical samples from schizophrenic patients [116] (Table 1). Furthermore, there seems to be a specific decrease in SST-positive interneurons, as shown by in situ hybridisation staining, in these samples [116]. However, these results await replication.
Table 1.
Findings in schizophrenic patients and correlations in mice models.
| Findings | References | |
|---|---|---|
| Humans | ||
|
| ||
| GAD67 | ↓ GAD67 in prefrontal cortex | Volk et al. [109] |
| Akbarian et al. [110] | ||
| Preserved # number of PV cells, cortex | Woo et al. [111] | |
| Hashimoto et al. [112] | ||
| ↓ GAD67 level in PV cells, cortex | Hashimoto et al. [112] | |
| Association with polymorphisms in GAD67 promoter | Addington et al. [113] | |
| Chandelier | Decrease in chandelier cells cartridges (GAT1+) in prefrontal cortex | Woo et al. [114] |
| Volk et al. [115] | ||
| SST | ↓ levels of SST in microarray analysis and ↓ number of SST cells, prefrontal cortex | Hashimoto et al. [116] |
| NPY/CCK | ↓ levels of NPY and CCK in microarray analysis | Hashimoto et al. [116] |
| NRG1 | Susceptibility locus in NRG1 | Stefansson et al. [117, 118] |
| Zhang et al. [119] | ||
| Yang et al. [120] | ||
| ERB4 | Susceptibility locus in ERB4 | Silberberg et al. [121] |
| BDNF/Trkb | Downregulation of BDNF in prefrontal cortex | Weickert et al. [122] |
| Wong et al. [123] | ||
| Downregulation of BDNF and Trkb in prefrontal cortex | Takahashi et al. [124] | |
| PSA/NCAM | ↓ PSA-NCAM complexes in hippocampus | Barbeau et al. [125] |
| Gamma | Gamma oscillations are triggered by working memory tasks + selective attention | Tallon-Baudry et al. [79] |
| Howard et al. [81] | ||
| Decreased power of cortical gamma oscillations and phase locking to memory task | Spencer et al. [82, 84] | |
| Cho et al. [85] | ||
|
| ||
| Mice | ||
|
| ||
| Erb4 | Selective interneuron loss of Erb4: “schizophrenia-like behaviors” | Wen et al. [126] |
| Erb4/Nrg1 | Erb4 in PV cells is required for Nrg1-dependant regulation of LTP (hippocampus) | Chen et al. [127] |
| NR1 | Selective loss of the NMDAr NR1 subunit in PV cells: decreased excitatory input to PV cells results in “schizophrenia-like behaviors” and ↓ expression of PV and GAD67 | Belforte et al. [128] |
| BDNF | BDNF regulates activity-dependant maturation of PV cells Bdnf−/− and Trkb−/−: ↓ synaptic GAD67 and GABA and behavioral anomalies | Huang et al. [129] |
| Cotrufo et al. [130] | ||
| Hashimoto et al. [131] | ||
| PSA/NCAM | Activity-mediated expression of PSA regulates PV cells maturation and visual plasticity | Di Cristo et al. [132] |
| Gamma | Gamma oscillations are triggered by stimulating PV cells: enhanced performance | Cardin et al. [77] |
| Sohal et al. [83] | ||
| Gamma oscillations depend on PV cells-mediated fast-synaptic inhibition | Bartos et al. [72] | |
Nonetheless, even if the numbers of various interneuron subtypes are preserved and if the morphological structure of these cells is intact in most cases, functional abnormalities in the connectivity of GABAergic circuits likely play a role in the pathogenesis of psychiatric disorders. Modifications of the specific GABAA receptor subunits expressed in the prefrontal cortex of schizophrenic patients have been described [116, 301]. Furthermore, cortical prefrontal gamma oscillations triggered by working memory tasks and selective attention in humans and primates [79–81] are decreased in schizophrenic patients with working memory deficits. These patients display a loss of gamma oscillation power and gamma oscillations are less tightly phase-locked to the task [82, 84, 85]. These changes might reflect functional alterations in the PV-positive basket cells, which contribute to the generation and regulation of the gamma oscillations that synchronise assemblies of pyramidal cells involved in a specific task [69, 72, 76–78, 83, 302]. In summary, multiple studies point to putative anomalies, either structural or functional, in PV-positive INs in the prefrontal cortex of schizophrenic patients.
5.3. Interneurons and Autism
Autism is a neurodevelopmental disorder combining impairments in socialization, communication, and restricted interests and/or stereotyped behaviors [294]. Autistic traits can be found in a variety of well-defined neurogenetic syndromes, including tuberous sclerosis [303, 304], fragile X syndrome [133, 134], and Rett syndrome [294]. In addition, nonsyndromic autism (re: without a clear underlying pathology, dysmorphic traits, or structural brain anomalies) has been associated with a variety of de novo copy number variants (CNVs) in large genome-wide association studies [141, 305–308], a finding which must be interpreted with caution [309]. However, the discovery of point mutations in genes encoding various synaptic scaffolding proteins in patients with nonsyndromic autism has begun to shed light on the pathophysiology of this disorder (recently reviewed in [309]). In particular, the discovery of mutations in postsynaptic neuroligins (NRL4X, NRL3) [135, 136], in other postsynaptic scaffolding proteins (SHANK2, SHANK3) [137–140, 310], in the presynaptic neurexins (NRXN1) [141, 142], and in fragile X mental retardation protein (FMR1 gene) suggest that dysfunction in the maintenance of excitatory synapses, synaptic plasticity, and long-term depression participate in the neurobiology of autism and that this might be rescued by metabotropic glutamatergic antagonists [151–154, 156, 311, 312].
In parallel, a dysfunction in GABAergic signalling has been postulated to contribute to the emergence of autistic behaviours. In fact, epilepsy is a frequent comorbidity of autism. Interictal epileptic activity is recorded on scalp EEG in up to 85% of autistic children, although seizures occur in only ~30% of patients [313, 314] (Table 2). This, together with the finding of decreased cortical GAD67/GAD65 expression in autistic patients' brains [143], has suggested that inhibitory dysfunction might play a role in subsets of autistic patients. Furthermore, polymorphisms in the Dlx1/2 genes have been associated with an increased susceptibility for autism [144] supporting the link between GABAergic anomalies and autism. In addition, nonsyndromic autism has been repeatedly associated with maternal chromosomal duplications in the 15q11-13 region [145, 146], which includes multiple genes encoding various GABAA receptor subunits (GABRA5, GABRG3, and GABRB3). Interestingly, MecP2, a transcription factor that broadly regulates gene expression by binding methylated CPG islands and which is responsible for the majority of cases of Rett syndrome (see next section), also exerts epigenetic control over this chromosomal region [157]. The loss of MecP2 results in dysregulation of multiple genes, including the downregulation of GABRB3. Furthermore, the loss of MecP2 is particularly detrimental to interneurons and a conditional MecP2 ablation in GABAergic neurons in mice was recently shown to recapitulate most of the behavioral anomalies associated with Rett syndrome, including autistic-like behavior [158].
Table 2.
Findings in autistic children and correlations in mice models.
| Findings | References | |
|---|---|---|
| Humans | ||
|
| ||
| FMR1 | Patients with fragile X syndrome often display autistic traits | Levitas et al. [133] |
| Brown et al. [134] | ||
| NRL4X/NRL3 | Point mutations in NRL4X and NRL3 associated with X-linked autism | Jamain et al. [135] |
| Point mutations in NRL4X in nonsyndromic autism | Laumonnier et al. [136] | |
| SHANK3 | Mutations in SHANK3 in nonsyndromic autism | Durand et al. [137] |
| Gauthier et al. [138] | ||
| Moessner et al. [139] | ||
| SHANK2 | Mutations in SHANK2 in nonsyndromic autism | Berkel et al. [140] |
| NRXN1 | Mutations in NRXN1 nonsyndromic autism | Szatmari et al. [141] |
| Kim et al. [142] | ||
| GAD65/67 | ↓ levels of GAD65/67 in cortex | Fatemi et al. [143] |
| Dlx1/2 | Polymorphisms in Dlx1/2 with increased susceptibility to autism | Liu et al. [144] |
| 15q11-13 | Maternal duplications in 15q11-13 in nonsyndromic autism | Baker et al. [145] |
| including GABRA5, GABRG3, GABRB3 (GABAAR subunits) | Hogart et al. [146] | |
| MECP2 | Mutations in MECP2 explain the majority of Rett syndrome. | Amir et al. [147] |
| Patients display autistic behaviors. | Buyse et al. [148] | |
| MET | Polymorphisms in MET promoter associated with autism | Jackson et al. [149] |
| Susceptibility locus for autism at 7q31 includes MET gene. | Campbell et al. [150] | |
|
| ||
| Mice | ||
|
| ||
| Fmr1 | Fmr1 k/o: behavioral anomalies improve with glutamatergic antagonists | Dolen et al. [151] |
| Bear et al. [152, 153] | ||
| Neuroligins/ neurexins |
NRL1/2 expression in nonneuronal cells trigger synapse formation in presynaptic cells | Scheiffele et al. [154] |
| NL-1 overexpression in hippocampal neurons promotes assembly of excitatory and inhibitory synapses and knock-down results in loss of inhibitory > excitatory synapses | Chih [155] | |
| Presynaptic β-neurexin induces GABA and glutamate synapse differentiation in postcell | Graf et al. [156] | |
| NRL1,3,4 localise at glutamatergic synapses, NRL2 at both excitatory and inhibitory | Graf et al. [156] | |
| MecP2 | Binds methylated CPG islands and exerts epigenetic control of UBE3A and GABR3 | Samaco et al. [157] |
| Interneuron selective loss of MecP2 recapitulates the Rett-like behavioral aN in mice | Chao et al. [158] | |
| uPAR, HGF, MET | uPAR−/− displays 50% loss of IN in cortex and seizure susceptibility | Powell et al. [11] |
| uPAR is required for the processing of HGF (an interneuron motogen), | Powell et al. [159] | |
| HGF, through its receptor MET, can rescue the phenotype of uPAR−/− mice | Bae et al. [160] | |
| Interneuron selective MET ablation: ↓ PV cortex, ↑ striatal PV cells, disrupts reversal learning | Martins et al. [161] | |
Finally, another well-characterised mouse model of autism, the uPAR−/− mouse, displays a spatially selective defect in interneuron migration, such that the frontoparietal cortices of these mice show 50% less calbindin-positive interneurons (with a near absence of PV cells) whereas more caudal cortices are spared [11, 12]. These mice display autistic-like behaviors with increased anxiety and altered socialisation, as well as interictal epileptiform EEG activity and an increased susceptibility to seizures [11, 12]. uPAR encodes an urokinase plasminogen activator which is required for the proper processing of the hepatocyte growth factor (HGF). In turn, HGF, through its receptor MET, has been shown to be a critical motogen for interneuron migration and is able to rescue the interneuron migration defect and seizure susceptibility of uPAR−/− mice [159, 160]. Interestingly, polymorphisms in the MET promoter have recently been described to confer an increased susceptibility to autism and this gene is included in one of the genomic sequences linked to autism susceptibility (7q31) [149, 150]. Autism is a complex disorder and alterations in other GABAergic circuits, including the striatocortical circuits, likely contribute to this behavioural phenotype. Indeed, an interneuron-selective ablation of MET results in decreased cortical PV cells, but massively increased dorsal striatal PV interneurons, leading to a disruption in striatal-mediated procedural and reversal learning [161]. Nonetheless, cortical and hippocampal GABAergic deficits certainly play a role in some of the cognitive-behavioral manifestations of autism, as well as in the associated susceptibility to seizures.
5.4. Interneurons and Epilepsy
Perhaps one of the most intuitive consequences of interneuron dysfunction is the development of epilepsy. Multiple mouse models carrying interneuronopathies have been shown to develop seizures [22, 28, 57, 63, 206, 207, 221]. In parallel, various reports point to probable GABAergic interneuron dysfunction in developmental and symptomatic (posttraumatic or poststatus epilepticus) epileptic disorders in humans [315–318]. In most situations, early developmental interneuron anomalies might contribute to seizure disorders both by altering the normal development of cortical circuits, as detailed above, and by failing to provide the acute inhibition required to control excessive excitation in the mature network. Paradoxically, in a state of chronic excitation, INs have been shown to contribute actively to ictogenesis when GABA becomes depolarizing due to the failure of chloride extrusion from damaged neurons [319, 320]. Therefore, both a primary dysfunction of GABAergic inhibitory transmission and a secondary switch to excitatory GABAergic transmission could contribute to the pathogenesis of epilepsy. Understanding the molecular mechanisms governing interneuron development, maturation, and normal function would therefore be very informative in our quest to comprehend human epileptic disorders.
Epilepsy is a heterogeneous disorder, and most cases are symptomatic of focal or widespread CNS lesions (e.g., malformations, tumors, infections, trauma, strokes, hypoxia, etc.). INs dysfunctions might contribute to seizure disorders following such insults, as suggested by the finding of limbic interneuronal loss after brain trauma or prolonged seizures [321–324]. Hippocampal somatostatin-positive interneurons appear to be particularly sensitive to seizure-induced damage as demonstrated in animal models of drug-induced epilepsy [13, 108, 324, 325], as well as in patients with chronic temporal lobe epilepsy [326]. This might point to a more selective vulnerability of this cell type which could be amendable to neuroprotective therapies. A loss of hippocampal PV cells [327] and alterations in the axonal projections of PV-positive chandelier cells have also been reported in patients with chronic epilepsy [316, 325, 328, 329]. Although it is not clear if these changes are the cause or the consequence of repeated seizures [330, 331], they probably contribute to the chronicity of the disease.
5.5. Interneurons in Genetic Developmental Epilepsies
Perhaps most interestingly, GABAergic interneuron dysfunction might contribute to a subset of genetic developmental epilepsies. In those cryptogenic epilepsies where no apparent etiology is found on examination or imaging (re: no dysmorphic traits or neurocutaneous stigma and normal brain CT/MRI), but where patients present clear neurological dysfunction as episodic seizures with or without interictal cognitive impairment, an underlying circuit dysfunction is postulated. These patients with severe developmental epilepsies (i.e., Ohtahara syndrome, West syndrome, Lennox-Gastaut syndrome, Dravet syndrome, etc.) are rarely amendable to surgical interventions, and only few reports of neuropathological examination of surgical or postmortem specimens are available. In most cases of West syndrome, the neuropathological evaluation reveals either focal cortical malformations or diffuse brain damage [332–335] but it is found to be “normal” in up to 45% of cases [336]. Nonetheless, functional inhibitory defects with disrupted GABAAR function or immature patterns of GABAAR subunit expression have been demonstrated in some cases of infantile spasms [318, 337]. Such inhibitory defects might arise as a consequence of genetic mutations that disrupt genes critical for proper interneuron generation or function. For instance, mutations in the alpha1 subunit of the voltage-gated sodium channel NaV 1.1 (SCN1A), the aristaless-related homeobox transcription factor (ARX), the cyclin-dependent kinase-like 5 (CDKL5), various GABAA receptor subunits and in the alpha 1 subunit of the voltage-dependent P/Q-type Ca2+ channel (CACNA1A) have been described in patients with a variety of epileptic disorders and similar mutations have been shown to impair GABAergic signalling in rodents (Table 3).
Table 3.
Selected examples of genes causing epilepsy in humans and interneuron dysfunctions in mice.
| Findings | References | |
|---|---|---|
| Humans | ||
|
| ||
| SCN1A | SCN1A mutations explain the majority of Dravet syndrome | Claes et al. [162]; Ohmori et al. [163] |
| Sugawara et al. [164]; Orrico et al. [165] | ||
| Escayg and Goldin et al. [166] | ||
| SCN1A mutations display phenotypic heterogeneity: GEFS, febrile seizures, cognitive impairment | Escayg et al. [167, 168] | |
| Fujiwara et al. [169]; Osaka et al. [170] | ||
| Zucca et al. [171]; Orrico et al. [165] | ||
| Variants in other channels modify the phenotype of SCN1A: SCN8A | Martin et al. [172] | |
| CACNB4 | Ohmori et al. [173] | |
| SCN1B | SCN1B mutations cause GEFS | Wallace et al. [174] |
| ARX | ARX mutations cause various phenotypes including infantile spasms | Shoubridge et al. [175] |
| CDKL5 | CDKL5 mutations cause early epileptic encephalopathies | Kalscheuer et al. [176]; Weaving et al. 2004 [177] |
| Scala et al. [178]; Archer et al. [179] | ||
| Cordova-Fletes et al. [180]; Mei et al. [181] | ||
| Melani et al. [182] | ||
| MECP2 | MECP2 mutations explain most cases of Rett syndrome. These patients often display seizures. | Amir et al. [147]; Buyse et al. [148] |
| GABRG2 | Mutations in the gamma2 subunit of the GABAAR cause childhood absence epilepsy ± febrile seizure | Wallace et al. [174]; Kananura et al. [183] |
| Truncation of GABRG2 causes generalised epilepsy with febrile seizure (GEFS) | Harkin et al. [184] | |
| GABRA1 | Mutations in the alpha1 subunit of the GABAAR cause juvenile myoclonic epilepsy | Cossette et al. [185] |
| Mutations in the alpha1 subunit of the GABAAR can also cause childhood absence epilepsy | Maljevic et al. [186] | |
| CACNA1A | Polymorphisms associated with generalised epilepsy syndromes | Chioza et al. [187] |
| Mutations in CACNA1A can cause ataxia with generalized seizures | Jouvenceau et al. [188]; Imbrici et al. [189] | |
| CACNB4 | Mutations in CACNB4 cause episodic ataxia with generalized seizures | Escayg et al. [190] |
| CACNA1H | Mutations in T-type calcium channel Cav3.2 cause childhood absence epilepsy | Khosravani et al. [191] |
| Nkx2.1 | Nkx2.1 haploinsufficiency leads to the “brain-lung-thyroid syndrome” | Carre et al. [192] |
| variable phenotype: severe respiratory distress at birth, mild-moderate hypothyroidism, chorea | Guillot et al. [193] | |
| Some patients present benign hereditary chorea, occasionally with cognitive impairment and seizures | Kleiner-Fisman et al. [194, 195] | |
| Dlx5/6 | Dlx5/6 mutations result in craniofacial and limb anomalies: ectodermal dysplasia | Morasso et al. [196]; Lo Lacono et al. [197] |
| Sox 6 | 1 patient described with heterozygote Sox6 mutation: craniosynostosis and facial dysmorphisms. | Tagariello et al. [198] |
|
| ||
| Mice | ||
|
| ||
| Scn1a | Scn1a (Nav1.1) expressed in most neuronal populations | Yu et al. [199] |
| Scn1a+/−and Scn1a−/−mice develop spontaneous seizures and die prematurely | Yu et al. [199] | |
| ↓ sodium currents are specific to GABAergic interneurons in Scn1a+/− and Scn1a−/− | Yu et al. [199] | |
| Selective loss of Scn1a in interneurons recapitulates seizure disorder | Martin et al. [200] | |
| Arx | Role in neuronal proliferation and migration | Fricourt et al. [201, 202] |
| Specific requirement of Arx for interneuron migration | Friocourt and Parnavelas [203]; Poirier et al. [204] | |
| Arx is a downstream target of Dlx1 | Colasante et al. [205] | |
| Arx(GCG)10+7 mice display seizures including spasms and ↓ no. of CB and NPY interneurons | Price et al. [206] | |
| Selective loss of Arx in interneurons recapitulates the seizure disorder | Marsh et al. [207] | |
| Cdkl5 | Cdkl5 is coexpressed with Mecp2 in cortical neurons and can phosphorylate Mecp2 | Mari et al. [208], Bertani et al. [209] |
| MecP2 | Mecp2 broadly represses gene expression by binding methylated CPG islands | Nan et al. [210, 211] |
| Cacna1a | Cacna1atg/tg tottering mutant displays ataxia and absence seizures | Noebels et al. [212]; Fletcher et al. [213] |
| Gain of thalamic T-type currents cause enhanced rebound bursting of TC cells in Cacna1atg/tg, Cacna1aln/ln | Zhang et al. [214]; Tsakiridou et al. [215] | |
| Interneuron selective ablation of Cacna1a leads to multiple types of generalised seizures incl. absences | Rossignol et al. [63] (abstract) | |
| Cacnb4 | Cacnb4lh/lh loss-of-function mutants display spontaneous absence seizures and ataxia | Burgess et al. [216] |
| Thalamic tonic GABAA currents enhance rebound bursting of TC cells in Cacnb4lh/lh | Cope et al. [217] | |
| Dlx1/2 | Dlx1−/−Dlx2−/− mice die perinatally and display a failure of IN migration to cortex and olfactory bulb | Anderson et al. [23, 218]; Bulfone et al. [219] |
| Dlx1−/−Dlx2+/− abnormal laminar distribution of IN and simplified morphology | Cobos et al. [220] | |
| Dlx1−/− morphological defect and postnatal loss of SST+/CR+ interneurons: spontaneous seizures | Cobos et al. [221] | |
| Nkx2.1 | Nkx2.1−/− die perinatally. Nkx2.1 is required for MGE interneuron generation. | Sussel et al. [222] |
| Interneuron specific removal of Nkx2.1 results in misspecification of MGE cells into CGE cells, and seizures | Butt et al. [22] | |
| Sox6 | Sox6−/− dies perinatally of craniofacial anomalies | |
| Conditional loss of Sox6 in interneurons results in misplaced/ectopic and immature basket cells (loss PV) | Batista-Brito et al. [28]; Azim et al. [223] | |
| Conditional loss of Sox6 in interneurons results in a severe epileptic encephalopathy | Batista-Brito et al. [28] | |
5.5.1. SCN1A
Mutations in SCN1A, which encodes the neuronal voltage-gated sodium channel Nav1.1, have been found to underlie a majority (75–85%) of cases of severe myoclonic epilepsy of infancy (Dravet syndrome) [162–166]. Interestingly, SCN1A mutations have also been found to cause generalised epilepsy with febrile seizures (GEFS) as well as a variety of disorders with neurocognitive impairment and variable seizure susceptibility [165, 167–171]. This extended phenotypic variability stems both from the nature of the mutations (nonsense mutations cause Dravet syndrome whereas missense mutations tend to cause different phenotypes depending on their location [166, 338–340]) and from the coexistence of genetic modifiers in other genes [172, 173]. Although Nav1.1 channels are found in most neuronal populations in the rodent brain, their loss was found to result in a more selective impairment of interneuronal transmission in mice [199, 200]. Nav1.1 channels tend to cluster predominantly at the level of the axon initial segment of PV-positive interneurons [341], and their loss results in failure of PV cells to maintain high frequency firing rates [341]. By contrast, pyramidal cell transmission is relatively well preserved in Nav1.1 mutants, presumably though compensation by other channels. Therefore, dysfunctions of INs might contribute significantly to the onset of epilepsy in Scn1a mutants.
5.5.2. ARX
In a similar fashion, mutations in the ARX gene are associated with a variety of neurological syndromes that combine epilepsy and various degrees of cognitive disabilities. The spectrum of phenotypes associated with ARX mutations extends from severe X-linked lissencephaly with ambiguous genitalia and severe myoclonic encephalopathies (Ohtahara syndrome, West syndrome), to isolated nonsyndromic mental retardation [175]. The ARX gene is necessary for proper neural proliferation, migration, and differentiation [201–203, 342]. In particular, ARX was shown to be essential for proper migration and laminar positioning of interneurons [203, 204], partly because it is a direct downstream target of Dlx1 [205]. Interestingly, ARX knock-in mice carrying trinucleotide repeat insertion mutations recapitulating mutations found in IS cases, display decreased numbers of telencephalic NPY+ and calbindin+ interneurons, and present an epileptic phenotype with early epileptic spasms [206]. Furthermore, a conditional deletion of ARX in GABAergic interneurons leads to a similar loss of interneuron migration and is sufficient to cause a developmental epileptic phenotype including brief spasm-like seizures [207]. This supports the hypothesis that even if ARX mutations might have broader consequences for cortical development, the specific effect on IN migration is fundamental to the development of epilepsy.
5.5.3. CDKL5/MECP2
Other patients with early epileptic encephalopathies have been found to carry mutations in CDKL5 [176–182], a protein kinase highly expressed in developing and mature neurons [343]. Interestingly, CDKL5 can directly bind and phosphorylate MecP2 and is coexpressed with MecP2 in cortical neurons [208, 209]. In turn, MecP2 is a transcription factor that broadly represses gene expression by binding methylated CPG islands [210, 211] and is therefore involved in the epigenetic control of gene expression. MECP2 mutations explain a majority of cases of Rett syndrome [147, 148], a neurodevelopmental disorder manifested by progressive microcephaly, developmental regression, stereotypies, and epilepsy. Interestingly, an interneuron selective ablation of MecP2 recapitulates most of the neurological and behavioral consequences of MecP2 knock-out mutations in mice [158]. Since MecP2 is a direct downstream target of CDKL5, it is possible that interneuron dysfunction also contributes to the cognitive and epileptic phenotype seen in both CDKL5 and MecP2 mutants.
5.6. Voltage-Gated Ca2+ Channels
Finally, patients with idiopathic generalized epilepsy syndromes (IGE) have been shown to carry mutations in various GABAA receptor subunits [174, 183–186, 344], as well as mutations or polymorphisms in multiple subunits of voltage-gated calcium channels, including the CACNA1A, CACNB4, and CACNA1H genes [187–191, 345]. These patients present various combinations of myoclonus, generalised tonic-clonic “grand-mal” seizures, and absence seizures “petit-mal.” Mutant mice carrying loss-of-function mutations in Cacna1a or Cacnb4 display similar generalised spike-wave absence seizures and have been instrumental in advancing our understanding of generalised epilepsies [212, 213, 216, 346]. In these models, an enhanced thalamocortical rebound bursting due to a gain in low-voltage activated Ca2+ currents and excessive thalamic GABAA signalling have been shown to result in hypersynchronisation of the thalamocortical circuitry and absence seizures [214, 215, 217, 347]. In addition, we recently demonstrated that selective loss of Cacna1a from cortical and limbic MGE-derived interneurons in mice is sufficient to create a severe epileptic encephalopathy with multiple types of generalised seizures [63]. We showed that Cacna1a loss resulted in unreliable neurotransmission from PV-positive interneurons. Furthermore, we demonstrated that concurrent loss of Cacna1a from both MGE-derived interneurons and cortical pyramidal cells results in a milder epileptic phenotype characterised by absence seizures [63]. These findings suggest that, in some cases, alterations in MGE-derived interneuron function might lead to a variety of generalised seizures and that the severity of the phenotype can be modulated by the involvement of other neuronal populations. Concurrent with these observations, various mouse models with either misspecified or immature MGE-derived interneurons have also been shown to develop severe epilepsies. For instance, Nkx2-1−/− and Sox6−/− null mutants die embryonically or perinatally due to a variety of craniofacial and lung anomalies [222, 348]. However, conditional mutants lacking either Nkx2-1 or Sox6 in an MGE-specific manner develop generalised seizures during the 2nd or 3rd postnatal week, leading to early lethality [22, 28]. In a similar fashion, Dlx1−/− mice also develop spontaneous seizures [221].
One of the limitations in extending some of the experimental findings from genetic models of interneuronopathy to human diseases is that most of the transcription factors important for interneuron development and specification are also involved in specification of other organs (bone, skin, cartilage, lung, and thyroid). Mutations in these genes therefore cause multisystemic disorders in which neurological involvement is often overlooked. For instance, human heterozygote mutations in Nkx2-1 have been described in a variety of clinical disorders affecting the thyroid, the lungs, and the brain, the so-called “brain-lung-thyroid” syndrome [192]. In some cases, truncating mutations result in severe respiratory failure at birth, due to the lack of surfactant proteins, with mild congenital hypothyroidism and neurocognitive anomalies [193]. In other cases, Nkx2-1 mutations have been described in patients with benign hereditary chorea, a movement disorder occasionally accompanied by intellectual impairment and seizures [194, 195]. In a similar fashion, heterozygous mutations in Dlx5/6 genes cause craniofacial and limb anomalies (ectodermal dysplasias) [196, 197]. Sox6 is known to be important for proper cartilage formation [348–350], and one child with craniosynostosis (premature fusion of the cranial sutures) and facial dysmorphisms has been shown to carry a heterozygous mutation in SOX6 [198]. However, even when direct inferences cannot be made between mouse mutants and human patients, the study of these animal models is instrumental in clarifying the role of specific interneuron populations in preventing various types of seizures and is critical to our understanding of epileptogenesis.
6. Conclusions and Future Perspectives
In summary, GABAergic INs include diverse neuronal populations which present significant heterogeneity in terms of their biochemical, morphological, and physiological properties. The fate of these INs is governed by tightly regulated genetic cascades. Disruption of these genetic programs, or of genes important for the proper specification, migration, maturation, and/or function of these cells, leads to a variety of cognitive, behavioural, and neurological consequences including autistic behaviors and epilepsy in rodents and humans. For this reason, furthering our understanding of interneuron development across mammalian species might become the cornerstone for the subsequent development of improved diagnostic approaches, and hopefully new therapeutic strategies, for patients with a variety of neurodevelopmental disorders. A fascinating example of this is the development of stem cell transplantation in the treatment of epileptic disorders in rodents [351, 352]. Other such innovative therapeutic approaches will likely emerge as the exquisite complexity of cortical interneurons diversity unravels.
Acknowledgments
The author is grateful to J. Hjerling-Leffler, J. Close, and S. Rossignol for their enlightening input in reviewing this paper. The author also wishes to thank the Fond de recherche en santé du Québec (FRSQ), the U. de Montréal, and the Centre de recherche de l'Hôpital Ste-Justine for their support.
References
- 1.Tamamaki N, Yanagawa Y, Tomioka R, Miyazaki JI, Obata K, Kaneko T. Green fluorescent protein expression and colocalization with calretinin, parvalbumin, and somatostatin in the GAD67-GFP knock-in mouse. Journal of Comparative Neurology. 2003;467(1):60–79. doi: 10.1002/cne.10905. [DOI] [PubMed] [Google Scholar]
- 2.McBain CJ, Fisahn A. Interneurons unbound. Nature Reviews Neuroscience. 2001;2(1):11–23. doi: 10.1038/35049047. [DOI] [PubMed] [Google Scholar]
- 3.Pouille F, Scanziani M. Enforcement of temporal fidelity in pyramidal cells by somatic feed-forward inhibition. Science. 2001;293(5532):1159–1163. doi: 10.1126/science.1060342. [DOI] [PubMed] [Google Scholar]
- 4.Wehr M, Zador AM. Balanced inhibition underlies tuning and sharpens spike timing in auditory cortex. Nature. 2003;426(6965):442–446. doi: 10.1038/nature02116. [DOI] [PubMed] [Google Scholar]
- 5.Markram H, Toledo-Rodriguez M, Wang Y, Gupta A, Silberberg G, Wu C. Interneurons of the neocortical inhibitory system. Nature Reviews Neuroscience. 2004;5(10):793–807. doi: 10.1038/nrn1519. [DOI] [PubMed] [Google Scholar]
- 6.Somogyi P, Klausberger T. Defined types of cortical interneurone structure space and spike timing in the hippocampus. Journal of Physiology. 2005;562(1):9–26. doi: 10.1113/jphysiol.2004.078915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klausberger T, Somogyi P. Neuronal diversity and temporal dynamics: the unity of hippocampal circuit operations. Science. 2008;321(5885):53–57. doi: 10.1126/science.1149381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Batista-Brito R, Fishell G. Chapter 3 the developmental integration of cortical interneurons into a functional network. Current Topics in Developmental Biology. 2009;87:81–118. doi: 10.1016/S0070-2153(09)01203-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rudy B, Fishell G, Lee S, Hjerling-Leffler J. Three groups of interneurons account for nearly 100% of neocortical GABAergic neurons. Developmental Neurobiology. 2010;71(1):45–61. doi: 10.1002/dneu.20853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Noebels JL. The biology of epilepsy genes. Annual Review of Neuroscience. 2003;26:599–625. doi: 10.1146/annurev.neuro.26.010302.081210. [DOI] [PubMed] [Google Scholar]
- 11.Powell EM, Campbell DB, Stanwood GD, Davis C, Noebels JL, Levitt P. Genetic disruption of cortical interneuron development causes region- and GABA cell type-specific deficits, epilepsy, and behavioral dysfunction. The Journal of Neuroscience. 2003;23(2):622–631. doi: 10.1523/JNEUROSCI.23-02-00622.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levitt P, Eagleson KL, Powell EM. Regulation of neocortical interneuron development and the implications for neurodevelopmental disorders. Trends in Neurosciences. 2004;27(7):400–406. doi: 10.1016/j.tins.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 13.Cossart R, Bernard C, Ben-Ari Y. Multiple facets of GABAergic neurons and synapses: multiple fates of GABA signalling in epilepsies. Trends in Neurosciences. 2005;28(2):108–115. doi: 10.1016/j.tins.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 14.Lewis DA, Hashimoto T, Volk DW. Cortical inhibitory neurons and schizophrenia. Nature Reviews Neuroscience. 2005;6(4):312–324. doi: 10.1038/nrn1648. [DOI] [PubMed] [Google Scholar]
- 15.Akbarian S, Huang HS. Molecular and cellular mechanisms of altered GAD1/GAD67 expression in schizophrenia and related disorders. Brain Research Reviews. 2006;52(2):293–304. doi: 10.1016/j.brainresrev.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 16.DeFelipe J. Neocortical neuronal diversity: chemical heterogeneity revealed by colocalization studies of classic neurotransmitters, neuropeptides, calcium-binding proteins, and cell surface molecules. Cerebral Cortex. 1993;3(4):273–289. doi: 10.1093/cercor/3.4.273. [DOI] [PubMed] [Google Scholar]
- 17.Kawaguchi Y, Kubota Y. Physiological and morphological identification of somatostatin- or vasoactive intestinal polypeptide-containing cells among GABAergic cell subtypes in rat frontal cortex. The Journal of Neuroscience. 1996;16(8):2701–2715. doi: 10.1523/JNEUROSCI.16-08-02701.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cauli B, Audinat E, Lambolez B, et al. Molecular and physiological diversity of cortical nonpyramidal cells. The Journal of Neuroscience. 1997;17(10):3894–3906. doi: 10.1523/JNEUROSCI.17-10-03894.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kawaguchi Y, Kubota Y. GABAergic cell subtypes and their synaptic connections in rat frontal cortex. Cerebral Cortex. 1997;7(6):476–486. doi: 10.1093/cercor/7.6.476. [DOI] [PubMed] [Google Scholar]
- 20.Gupta A, Wang Y, Markram H. Organizing principles for a diversity of GABAergic interneurons and synapses in the neocortex. Science. 2000;287(5451):273–278. doi: 10.1126/science.287.5451.273. [DOI] [PubMed] [Google Scholar]
- 21.Ascoli GA, Alonso-Nanclares L, Anderson SA, et al. Petilla terminology: nomenclature of features of GABAergic interneurons of the cerebral cortex. Nature Reviews Neuroscience. 2008;9(7):557–568. doi: 10.1038/nrn2402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Butt SJB, Sousa VH, Fuccillo MV, et al. The requirement of Nkx2-1 in the temporal specification of cortical interneuron subtypes. Neuron. 2008;59(5):722–732. doi: 10.1016/j.neuron.2008.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anderson SA, Qiu M, Bulfone A, et al. Mutations of the homeobox genes Dlx-1 and Dlx-2 disrupt the striatal subventricular zone and differentiation of late born striatal neurons. Neuron. 1997;19(1):27–37. doi: 10.1016/s0896-6273(00)80345-1. [DOI] [PubMed] [Google Scholar]
- 24.Marín O, Anderson SA, Rubenstein JLR. Origin and molecular specification of striatal interneurons. The Journal of Neuroscience. 2000;20(16):6063–6076. doi: 10.1523/JNEUROSCI.20-16-06063.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xu Q, Cobos I, de La Cruz ED, Rubenstein JL, Anderson SA. Origins of cortical interneuron subtypes. The Journal of Neuroscience. 2004;24(11):2612–2622. doi: 10.1523/JNEUROSCI.5667-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Du T, Xu Q, Ocbina PJ, Anderson SA. NKX2.1 specifies cortical interneuron fate by activating Lhx6 . Development. 2008;135(8):1559–1567. doi: 10.1242/dev.015123. [DOI] [PubMed] [Google Scholar]
- 27.Xu Q, Tam M, Anderson SA. Fate mapping Nkx2.1-lineage cells in the mouse telencephalon. Journal of Comparative Neurology. 2008;506(1):16–29. doi: 10.1002/cne.21529. [DOI] [PubMed] [Google Scholar]
- 28.Batista-Brito R, Rossignol E, Hjerling-Leffler J, et al. The cell-intrinsic requirement of Sox6 for cortical interneuron development. Neuron. 2009;63(4):466–481. doi: 10.1016/j.neuron.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Welagen J, Anderson S. Origins of neocortical interneurons in mice. Developmental Neurobiology. 2011;71(1):10–17. doi: 10.1002/dneu.20857. [DOI] [PubMed] [Google Scholar]
- 30.Plotkin JL, Wu N, Chesselet MF, Levine MS. Functional and molecular development of striatal fast-spiking GABAergic interneurons and their cortical inputs. European Journal of Neuroscience. 2005;22(5):1097–1108. doi: 10.1111/j.1460-9568.2005.04303.x. [DOI] [PubMed] [Google Scholar]
- 31.Chesselet MF, Plotkin JL, Wu N, Levine MS. Development of striatal fast-spiking GABAergic interneurons. Progress in Brain Research. 2007;160:261–272. doi: 10.1016/S0079-6123(06)60015-0. [DOI] [PubMed] [Google Scholar]
- 32.Woodruff AR, Sah P. Networks of parvalbumin-positive interneurons in the basolateral amygdala. The Journal of Neuroscience. 2007;27(3):553–563. doi: 10.1523/JNEUROSCI.3686-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Batista-Brito R, Close J, Machold R, Fishell G. The distinct temporal origins of olfactory bulb interneuron subtypes. The Journal of Neuroscience. 2008;28(15):3966–3975. doi: 10.1523/JNEUROSCI.5625-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Likhtik E, Popa D, Apergis-Schoute J, Fidacaro GA, Paré D. Amygdala intercalated neurons are required for expression of fear extinction. Nature. 2008;454(7204):642–645. doi: 10.1038/nature07167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Truitt WA, Johnson PL, Dietrich AD, Fitz SD, Shekhar A. Anxiety-like behavior is modulated by a discrete subpopulation of interneurons in the basolateral amygdala. Neuroscience. 2009;160(2):284–294. doi: 10.1016/j.neuroscience.2009.01.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ciocchi S, Herry C, Grenier F, et al. Encoding of conditioned fear in central amygdala inhibitory circuits. Nature. 2010;468(7321):277–282. doi: 10.1038/nature09559. [DOI] [PubMed] [Google Scholar]
- 37.Tricoire L, Pelkey KA, Daw MI, et al. Common origins of hippocampal ivy and nitric oxide synthase expressing neurogliaform cells. The Journal of Neuroscience. 2010;30(6):2165–2176. doi: 10.1523/JNEUROSCI.5123-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Waclaw RR, Ehrman LA, Pierani A, Campbell K. Developmental origin of the neuronal subtypes that comprise the amygdalar fear circuit in the mouse. The Journal of Neuroscience. 2010;30(20):6944–6953. doi: 10.1523/JNEUROSCI.5772-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ghiglieri V, Sgobio C, Costa C, Picconi B, Calabresi P. Striatum-hippocampus balance: from physiological behavior to interneuronal pathology. Progress in Neurobiology. 2011;94(2):102–114. doi: 10.1016/j.pneurobio.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 40.Spampanato J, Polepalli J, Sah P. Interneurons in the basolateral amygdala. Neuropharmacology. 2010;60:765–773. doi: 10.1016/j.neuropharm.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 41.Wichterle H, Turnbull DH, Nery S, Fishell G, Alvarez-Buylla A. In utero fate mapping reveals distinct migratory pathways and fates of neurons born in the mammalian basal forebrain. Development. 2001;128(19):3759–3771. doi: 10.1242/dev.128.19.3759. [DOI] [PubMed] [Google Scholar]
- 42.Anderson SA, Kaznowski CE, Horn C, Rubenstein JLR, McConnell SK. Distinct origins of neocortical projection neurons and interneurons in vivo. Cerebral Cortex. 2002;12(7):702–709. doi: 10.1093/cercor/12.7.702. [DOI] [PubMed] [Google Scholar]
- 43.Nery S, Fishell G, Corbin JG. The caudal ganglionic eminence is a source of distinct cortical and subcortical cell populations. Nature Neuroscience. 2002;5(12):1279–1287. doi: 10.1038/nn971. [DOI] [PubMed] [Google Scholar]
- 44.Butt SJB, Fuccillo M, Nery S, et al. The temporal and spatial origins of cortical interneurons predict their physiological subtype. Neuron. 2005;48(4):591–604. doi: 10.1016/j.neuron.2005.09.034. [DOI] [PubMed] [Google Scholar]
- 45.Miyoshi G, Butt SJB, Takebayashi H, Fishell G. Physiologically distinct temporal cohorts of cortical interneurons arise from telencephalic Olig2-expressing precursors. The Journal of Neuroscience. 2007;27(29):7786–7798. doi: 10.1523/JNEUROSCI.1807-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Miyoshi G, Hjerling-Leffler J, Karayannis T, et al. Genetic fate mapping reveals that the caudal ganglionic eminence produces a large and diverse population of superficial cortical interneurons. The Journal of Neuroscience. 2010;30(5):1582–1594. doi: 10.1523/JNEUROSCI.4515-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gelman DM, Martini FJ, Nobrega-Pereira S, et al. The embryonic preoptic area is a novel source of cortical GABAergic interneurons. The Journal of Neuroscience. 2009;29(29):9380–9389. doi: 10.1523/JNEUROSCI.0604-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lee S, Hjerling-Leffler J, Zagha E, Fishell G, Rudy B. The largest group of superficial neocortical GABAergic interneurons expresses ionotropic serotonin receptors. The Journal of Neuroscience. 2010;30(50):16796–16808. doi: 10.1523/JNEUROSCI.1869-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Férézou I, Cauli B, Hill EL, Rossier J, Hamel E, Lambolez B. 5-HT3 receptors mediate serotonergic fast synaptic excitation of neocortical vasoactive intestinal peptide/cholecystokinin interneurons. The Journal of Neuroscience. 2002;22(17):7389–7397. doi: 10.1523/JNEUROSCI.22-17-07389.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Campbell K, Olsson M, Björklund A. Regional incorporation and site-specific differentiation of striatal precursors transplanted to the embryonic forebrain ventricle. Neuron. 1995;15(6):1259–1273. doi: 10.1016/0896-6273(95)90006-3. [DOI] [PubMed] [Google Scholar]
- 51.Wonders CP, Anderson SA. The origin and specification of cortical interneurons. Nature Reviews Neuroscience. 2006;7(9):687–696. doi: 10.1038/nrn1954. [DOI] [PubMed] [Google Scholar]
- 52.Goldberg EM, Clark BD, Zagha E, Nahmani M, Erisir A, Rudy B. K+ channels at the axon initial segment dampen near-threshold excitability of neocortical fast-spiking GABAergic interneurons. Neuron. 2008;58(3):387–400. doi: 10.1016/j.neuron.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Helmstaedter M, Sakmann B, Feldmeyer D. Neuronal correlates of local, lateral, and translaminar inhibition with reference to cortical columns. Cerebral Cortex. 2009;19(4):926–937. doi: 10.1093/cercor/bhn141. [DOI] [PubMed] [Google Scholar]
- 54.Gibson JR, Belerlein M, Connors BW. Two networks of electrically coupled inhibitory neurons in neocortex. Nature. 1999;402(6757):75–79. doi: 10.1038/47035. [DOI] [PubMed] [Google Scholar]
- 55.Erisir A, Lau D, Rudy B, Leonard CS. Function of specific K+ channels in sustained high-frequency firing of fast-spiking neocortical interneurons. Journal of Neurophysiology. 1999;82(5):2476–2489. doi: 10.1152/jn.1999.82.5.2476. [DOI] [PubMed] [Google Scholar]
- 56.Rudy B, Chow A, Lau D, et al. Contributions of Kv3 channels to neuronal excitability. Annals of the New York Academy of Sciences. 1999;868:304–343. doi: 10.1111/j.1749-6632.1999.tb11295.x. [DOI] [PubMed] [Google Scholar]
- 57.Lau D, Vega-Saenz de Miera EC, Contreras D, et al. Impaired fast-spiking, suppressed cortical inhibition, and increased susceptibility to seizures in mice lacking Kv3.2 K+ channel proteins. The Journal of Neuroscience. 2000;20(24):9071–9085. doi: 10.1523/JNEUROSCI.20-24-09071.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rudy B, McBain CJ. Kv3 channels: voltage-gated K+ channels designed for high-frequency repetitive firing. Trends in Neurosciences. 2001;24(9):517–526. doi: 10.1016/s0166-2236(00)01892-0. [DOI] [PubMed] [Google Scholar]
- 59.Chang SY, Zagha E, Kwon ES, et al. Distribution of Kv3.3 potassium channel subunits in distinct neuronal populations of mouse brain. Journal of Comparative Neurology. 2007;502(6):953–972. doi: 10.1002/cne.21353. [DOI] [PubMed] [Google Scholar]
- 60.Zaitsev AV, Povysheva NV, Lewis DA, Krimer LS. P/Q-type, but not N-type, calcium channels mediate GABA release from fast-spiking interneurons to pyramidal cells in rat prefrontal cortex. Journal of Neurophysiology. 2007;97(5):3567–3573. doi: 10.1152/jn.01293.2006. [DOI] [PubMed] [Google Scholar]
- 61.Bucurenciu I, Kulik A, Schwaller B, Frotscher M, Jonas P. Nanodomain coupling between Ca2+ channels and Ca2+ sensors promotes fast and efficient transmitter release at a cortical GABAergic synapse. Neuron. 2008;57(4):536–545. doi: 10.1016/j.neuron.2007.12.026. [DOI] [PubMed] [Google Scholar]
- 62.Kruglikov I, Rudy B. Perisomatic GABA release and thalamocortical integration onto neocortical excitatory cells are regulated by neuromodulators. Neuron. 2008;58(6):911–924. doi: 10.1016/j.neuron.2008.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rossignol E, Kruglikov I, van den Maagdenberg AMJM, Fishell G, Rudy B. Defective cortical signaling results in generalised seizures. In: Proceedings of the 40th Annual Meeting of Neuroscience; 2010; San Diego, Calif, USA. Society for Neuroscience; [Google Scholar]
- 64.Pinto DJ, Brumberg JC, Simons DJ. Circuit dynamics and coding strategies in rodent somatosensory cortex. Journal of Neurophysiology. 2000;83(3):1158–1166. doi: 10.1152/jn.2000.83.3.1158. [DOI] [PubMed] [Google Scholar]
- 65.Pinto DJ, Hartings JA, Brumberg JC, Simons DJ. Cortical damping: analysis of thalamocortical response transformations in rodent barrel cortex. Cerebral Cortex. 2003;13(1):33–44. doi: 10.1093/cercor/13.1.33. [DOI] [PubMed] [Google Scholar]
- 66.Gabernet L, Jadhav SP, Feldman DE, Carandini M, Scanziani M. Somatosensory integration controlled by dynamic thalamocortical feed-forward inhibition. Neuron. 2005;48(2):315–327. doi: 10.1016/j.neuron.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 67.Cruikshank SJ, Lewis TJ, Connors BW. Synaptic basis for intense thalamocortical activation of feedforward inhibitory cells in neocortex. Nature Neuroscience. 2007;10(4):462–468. doi: 10.1038/nn1861. [DOI] [PubMed] [Google Scholar]
- 68.Pouille F, Marin-Burgin A, Adesnik H, Atallah BV, Scanziani M. Input normalization by global feedforward inhibition expands cortical dynamic range. Nature Neuroscience. 2009;12(12):1577–1585. doi: 10.1038/nn.2441. [DOI] [PubMed] [Google Scholar]
- 69.Tamas G, Buhl EH, Lorincz A, Somogyi P. Proximally targeted G.ABAergic synapses and gap junctions synchronize cortical interneurons. Nature Neuroscience. 2000;3(4):366–371. doi: 10.1038/73936. [DOI] [PubMed] [Google Scholar]
- 70.Szabadics J, Lorincz A, Tamas G. Beta and gamma frequency synchronization by dendritic gabaergic synapses and gap junctions in a network of cortical interneurons. The Journal of Neuroscience. 2001;21(15):5824–5831. doi: 10.1523/JNEUROSCI.21-15-05824.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Deans MR, Gibson JR, Sellitto C, Connors BW, Paul DL. Synchronous activity of inhibitory networks in neocortex requires electrical synapses containing connexin36. Neuron. 2001;31(3):477–485. doi: 10.1016/s0896-6273(01)00373-7. [DOI] [PubMed] [Google Scholar]
- 72.Bartos M, Vida I, Frotscher M, et al. Fast synaptic inhibition promotes synchronized gamma oscillations in hippocampal interneuron networks. Proceedings of the National Academy of Sciences of the United States of America. 2002;99(20):13222–13227. doi: 10.1073/pnas.192233099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Traub RD, Cunningham MO, Gloveli T, et al. GABA-enhanced collective behavior in neuronal axons underlies persistent gamma-frequency oscillations. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(19):11047–11052. doi: 10.1073/pnas.1934854100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Traub RD, Bibbig A, LeBeau FEN, Buhl EH, Whittington MA. Cellular mechanisms of neuronal population oscillations in the hippocampus in vitro. Annual Review of Neuroscience. 2004;27:247–278. doi: 10.1146/annurev.neuro.27.070203.144303. [DOI] [PubMed] [Google Scholar]
- 75.Traub RD, Michelson-Law H, Bibbig AEJ, Buhl EH, Whittington MA. Gap junctions, fast oscillations and the initiation of seizures. Advances in Experimental Medicine and Biology. 2004;548:110–122. doi: 10.1007/978-1-4757-6376-8_9. [DOI] [PubMed] [Google Scholar]
- 76.Bartos M, Vida I, Jonas P. Synaptic mechanisms of synchronized gamma oscillations in inhibitory interneuron networks. Nature Reviews Neuroscience. 2007;8(1):45–56. doi: 10.1038/nrn2044. [DOI] [PubMed] [Google Scholar]
- 77.Cardin JA, Carlén M, Meletis K, et al. Driving fast-spiking cells induces gamma rhythm and controls sensory responses. Nature. 2009;459(7247):663–667. doi: 10.1038/nature08002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Buhl DL, Harris KD, Hormuzdi SG, Monyer H, Buzsáki G. Selective impairment of hippocampal gamma oscillations in connexin-36 knock-out mouse in vivo. The Journal of Neuroscience. 2003;23(3):1013–1018. doi: 10.1523/JNEUROSCI.23-03-01013.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tallon-Baudry C, Bertrand O, Peronnet F, Pernier J. Induced γ-band activity during the delay of a visual short-term memory task in humans. The Journal of Neuroscience. 1998;18(11):4244–4254. doi: 10.1523/JNEUROSCI.18-11-04244.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fries P, Reynolds JH, Rorie AE, Desimone R. Modulation of oscillatory neuronal synchronization by selective visual attention. Science. 2001;291(5508):1560–1563. doi: 10.1126/science.1055465. [DOI] [PubMed] [Google Scholar]
- 81.Howard MW, Rizzuto DS, Caplan JB, et al. Gamma oscillations correlate with working memory load in humans. Cerebral Cortex. 2003;13(12):1369–1374. doi: 10.1093/cercor/bhg084. [DOI] [PubMed] [Google Scholar]
- 82.Spencer KM, Nestor PG, Niznikiewicz MA, Salisbury DF, Shenton ME, McCarley RW. Abnormal neural synchrony in schizophrenia. The Journal of Neuroscience. 2003;23(19):7407–7411. doi: 10.1523/JNEUROSCI.23-19-07407.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sohal VS, Zhang F, Yizhar O, Deisseroth K. Parvalbumin neurons and gamma rhythms enhance cortical circuit performance. Nature. 2009;459(7247):698–702. doi: 10.1038/nature07991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Spencer KM, Nestor PG, Perlmutter R, et al. Neural synchrony indexes disordered perception and cognition in schizophrenia. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(49):17288–17293. doi: 10.1073/pnas.0406074101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cho RY, Konecky RO, Carter CS. Impairments in frontal cortical γ synchrony and cognitive control in schizophrenia. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(52):19878–19883. doi: 10.1073/pnas.0609440103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kawaguchi Y. Physiological subgroups of nonpyramidal cells with specific morphological characteristics in layer II/III of rat frontal cortex. The Journal of Neuroscience. 1995;15(4):2638–2655. doi: 10.1523/JNEUROSCI.15-04-02638.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gonzalez-Burgos G, Krimer LS, Povysheva NV, Barrionuevo G, Lewis DA. Functional properties of fast spiking interneurons and their synaptic connections with pyramidal cells in primate dorsolateral prefrontal cortex. Journal of Neurophysiology. 2005;93(2):942–953. doi: 10.1152/jn.00787.2004. [DOI] [PubMed] [Google Scholar]
- 88.Jones EG. Varieties and distribution of non pyramidal cells in the somatic sensory cortex of the squirrel monkey. Journal of Comparative Neurology. 1975;160(2):205–267. doi: 10.1002/cne.901600204. [DOI] [PubMed] [Google Scholar]
- 89.Fairen A, Valverde F. A specialized type of neuron in the visual cortex of cat: golgi golgi and electron microscope study of chandelier cells. Journal of Comparative Neurology. 1980;194(4):761–779. doi: 10.1002/cne.901940405. [DOI] [PubMed] [Google Scholar]
- 90.DeFelipe J, Hendry SHC, Jones EG. Visualization of chandelier cell axons by parvalbumin immunoreactivity in monkey cerebral cortex. Proceedings of the National Academy of Sciences of the United States of America. 1989;86(6):2093–2097. doi: 10.1073/pnas.86.6.2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Somogyi P. A specific “axo-axonal” interneuron in the visual cortex of the rat. Brain Research. 1977;136(2):345–350. doi: 10.1016/0006-8993(77)90808-3. [DOI] [PubMed] [Google Scholar]
- 92.Szabadics J, Varga C, Molnar G, Olah S, Barzo P, Tamas G. Excitatory effect of GABAergic axo-axonic cells in cortical microcircuits. Science. 2006;311(5758):233–235. doi: 10.1126/science.1121325. [DOI] [PubMed] [Google Scholar]
- 93.Khirug S, Yamada J, Afzalov R, Voipio J, Khiroug L, Kaila K. GABAergic depolarization of the axon initial segment in cortical principal neurons is caused by the Na-K-2Cl cotransporter NKCC1. The Journal of Neuroscience. 2008;28(18):4635–4639. doi: 10.1523/JNEUROSCI.0908-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Woodruff AR, Xu Q, Anderson SA, Yuste R. Depolarizing effect of neocortical chandelier neurons. Frontiers in Neural Circuits. 2009;3(15):10 pages. doi: 10.3389/neuro.04.015.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Woodruff AR, Anderson SA, Yuste R, et al. The enigmatic function of chandelier cells. Frontiers in Neuroscience. 2010;4, article 201 doi: 10.3389/fnins.2010.00201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Glickfeld LL, Roberts JD, Somogyi P, Scanziani M. Interneurons hyperpolarize pyramidal cells along their entire somatodendritic axis. Nature Neuroscience. 2009;12(1):21–23. doi: 10.1038/nn.2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Klausberger T, Magill PJ, Marton LF, et al. Brain-state and cell-type-specific firing of hippocampal interneurons in vivo. Nature. 2003;421(6925):844–848. doi: 10.1038/nature01374. [DOI] [PubMed] [Google Scholar]
- 98.Halabisky B, Shen F, Huguenard JR, Prince DA. Electrophysiological classification of somatostatin-positive interneurons in mouse sensorimotor cortex. Journal of Neurophysiology. 2006;96(2):834–845. doi: 10.1152/jn.01079.2005. [DOI] [PubMed] [Google Scholar]
- 99.Ma Y, Hu H, Berrebi AS, Mathers PH, Agmon A. Distinct subtypes of somatostatin-containing neocortical interneurons revealed in transgenic mice. The Journal of Neuroscience. 2006;26(19):5069–5082. doi: 10.1523/JNEUROSCI.0661-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.McGarry LM, Packer AM, Fino E, Nikolenko V, Sippy T, Yuste R. Quantitative classification of somatostatin-positive neocortical interneurons identifies three interneuron subtypes. Frontiers in Neural Circuits. 2010;4(12):19 pages. doi: 10.3389/fncir.2010.00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fanselow EE, Richardson KA, Connors BW. Selective, state-dependent activation of somatostatin-expressing inhibitory interneurons in mouse neocortex. Journal of Neurophysiology. 2008;100(5):2640–2652. doi: 10.1152/jn.90691.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang Y, Toledo-Rodriguez M, Gupta A, et al. Anatomical, physiological and molecular properties of Martinotti cells in the somatosensory cortex of the juvenile rat. Journal of Physiology. 2004;561(1):65–90. doi: 10.1113/jphysiol.2004.073353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Uematsu M, Hirai Y, Karube F, et al. Quantitative chemical composition of cortical GABAergic neurons revealed in transgenic venus-expressing rats. Cerebral Cortex. 2008;18(2):315–330. doi: 10.1093/cercor/bhm056. [DOI] [PubMed] [Google Scholar]
- 104.Murayama M, Pérez-Garci E, Nevian T, Bock T, Senn W, Larkum ME. Dendritic encoding of sensory stimuli controlled by deep cortical interneurons. Nature. 2009;457(7233):1137–1141. doi: 10.1038/nature07663. [DOI] [PubMed] [Google Scholar]
- 105.Silberberg G, Markram H. Disynaptic inhibition between neocortical pyramidal cells mediated by martinotti cells. Neuron. 2007;53(5):735–746. doi: 10.1016/j.neuron.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 106.Berger TK, Perin R, Silberberg G, Markram H. Frequency-dependent disynaptic inhibition in the pyramidal network: a ubiquitous pathway in the developing rat neocortex. Journal of Physiology. 2009;587(22):5411–5425. doi: 10.1113/jphysiol.2009.176552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Fanselow EE, Connors BW. The roles of somatostatin-expressing (GIN) and fast-spiking inhibitory interneurons in UP-DOWN states of mouse neocortex. Journal of Neurophysiology. 2010;104(2):596–606. doi: 10.1152/jn.00206.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cossart R, Dinocourt C, Hirsch JC, et al. Dendritic but not somatic GABAergic inhibition is decreased in experimental epilepsy. Nature Neuroscience. 2001;4(1):52–62. doi: 10.1038/82900. [DOI] [PubMed] [Google Scholar]
- 109.Volk DW, Austin MC, Pierri JN, Sampson AR, Lewis DA. Decreased glutamic acid decarboxylase67 messenger RNA expression in a subset of prefrontal cortical γ-aminobutyric acid neurons in subjects with schizophrenia. Archives of General Psychiatry. 2000;57(3):237–245. doi: 10.1001/archpsyc.57.3.237. [DOI] [PubMed] [Google Scholar]
- 110.Akbarian S, Kim JJ, Potkin SG, et al. Gene expression for glutamic acid decarboxylase is reduced without loss of neurons in prefrontal cortex of schizophrenics. Archives of General Psychiatry. 1995;52(4):258–278. doi: 10.1001/archpsyc.1995.03950160008002. [DOI] [PubMed] [Google Scholar]
- 111.Woo TU, Miller JL, Lewis DA. Schizophrenia and the parvalbumin-containing class of cortical local circuit neurons. American Journal of Psychiatry. 1997;154(7):1013–1015. doi: 10.1176/ajp.154.7.1013. [DOI] [PubMed] [Google Scholar]
- 112.Hashimoto T, Volk DW, Eggan SM, et al. Gene expression deficits in a subclass of GABA neurons in the prefrontal cortex of subjects with schizophrenia. The Journal of Neuroscience. 2003;23(15):6315–6326. doi: 10.1523/JNEUROSCI.23-15-06315.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Addington AM, Gornick M, Duckworth J, et al. GAD1 (2q31.1), which encodes glutamic acid decarboxylase (GAD67), is associated with childhood-onset schizophrenia and cortical gray matter volume loss. Molecular Psychiatry. 2005;10(6):581–588. doi: 10.1038/sj.mp.4001599. [DOI] [PubMed] [Google Scholar]
- 114.Woo TU, Whitehead RE, Melchitzky DS, Lewis DA. A subclass of prefrontal γ-aminobutyric acid axon terminals are selectively altered in schizophrenia. Proceedings of the National Academy of Sciences of the United States of America. 1998;95(9):5341–5346. doi: 10.1073/pnas.95.9.5341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Volk DW, Austin MC, Pierri JN, Sampson AR, Lewis DA. GABA transporter-1 mRNA in the prefrontal cortex in schizophrenia: decreased expression in a subset of neurons. American Journal of Psychiatry. 2001;158(2):256–265. doi: 10.1176/appi.ajp.158.2.256. [DOI] [PubMed] [Google Scholar]
- 116.Hashimoto T, Arion D, Unger T, et al. Alterations in GABA-related transcriptome in the dorsolateral prefrontal cortex of subjects with schizophrenia. Molecular Psychiatry. 2008;13(2):147–161. doi: 10.1038/sj.mp.4002011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Stefansson H, Sigurdsson E, Steinthorsdottir V, et al. Neuregulin 1 and susceptibility to schizophrenia. American Journal of Human Genetics. 2002;71(4):877–892. doi: 10.1086/342734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Stefansson H, Sarginson J, Kong A, et al. Association of neuregulin 1 with schizophrenia confirmed in a Scottish population. American Journal of Human Genetics. 2003;72(1):83–87. doi: 10.1086/345442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zhang HX, Li WQ, Zhang Y, Zhao JP, Lv LX, Yang G. Association analysis of neuregulin 1 gene polymorphism with schizophrenia in Chinese Han population. Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 2009;26(1):16–20. doi: 10.3760/cma.j.issn.1003-9406.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 120.Yang JZ, Si TM, Ruan Y, et al. Association study of neuregulin 1 gene with schizophrenia. Molecular Psychiatry. 2003;8(7):706–709. doi: 10.1038/sj.mp.4001377. [DOI] [PubMed] [Google Scholar]
- 121.Silberberg G, Darvasi A, Pinkas-Kramarski R, Navon R. The involvement of ErbB4 with schizophrenia: association and expression studies. American Journal of Medical Genetics Part B. 2006;141(2):142–148. doi: 10.1002/ajmg.b.30275. [DOI] [PubMed] [Google Scholar]
- 122.Weickert CS, Hyde TM, Lipska BK, Herman MM, Weinberger DR, Kleinman JE. Reduced brain-derived neurotrophic factor in prefrontal cortex of patients with schizophrenia. Molecular Psychiatry. 2003;8(6):592–610. doi: 10.1038/sj.mp.4001308. [DOI] [PubMed] [Google Scholar]
- 123.Wong J, Hyde TM, Cassano HL, Deep-Soboslay A, Kleinman JE, Weickert CS. Promoter specific alterations of brain-derived neurotrophic factor mRNA in schizophrenia. Neuroscience. 2010;169(3):1071–1084. doi: 10.1016/j.neuroscience.2010.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Takahashi M, Shirakawa O, Toyooka K, et al. Abnormal expression of brain-derived neurotrophic factor and its receptor in the corticolimbic system of schizophrenic patients. Molecular Psychiatry. 2000;5(3):293–300. doi: 10.1038/sj.mp.4000718. [DOI] [PubMed] [Google Scholar]
- 125.Barbeau D, Liang JJ, Robitaille Y, Quirion R, Srivastava LK. Decreased expression of the embryonic form of the neural cell adhesion molecule in schizophrenic brains. Proceedings of the National Academy of Sciences of the United States of America. 1995;92(7):2785–2789. doi: 10.1073/pnas.92.7.2785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wen L, Lu YS, Zhu XH, et al. Neuregulin 1 regulates pyramidal neuron activity via ErbB4 in parvalbumin-positive interneurons. Proceedings of the National Academy of Sciences of the United States of America. 2010;107(3):1211–1216. doi: 10.1073/pnas.0910302107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Chen YJ, Zhang M, Yin DM, et al. ErbB4 in parvalbumin-positive interneurons is critical for neuregulin 1 regulation of long-term potentiation. Proceedings of the National Academy of Sciences of the United States of America. 2010;107(50):21818–21823. doi: 10.1073/pnas.1010669107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Belforte JE, Zsiros V, Sklar ER, et al. Postnatal NMDA receptor ablation in corticolimbic interneurons confers schizophrenia-like phenotypes. Nature Neuroscience. 2010;13(1):76–83. doi: 10.1038/nn.2447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Huang ZJ, Kirkwood A, Pizzorusso T, et al. BDNF regulates the maturation of inhibition and the critical period of plasticity in mouse visual cortex. Cell. 1999;98(6):739–755. doi: 10.1016/s0092-8674(00)81509-3. [DOI] [PubMed] [Google Scholar]
- 130.Cotrufo T, Viegi A, Berardi N, Bozzi Y, Mascia L, Maffei L. Effects of neurotrophins on synaptic protein expression in the visual cortex of dark-reared rats. The Journal of Neuroscience. 2003;23(9):3566–3571. doi: 10.1523/JNEUROSCI.23-09-03566.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hashimoto T, Bergen SE, Nguyen QL, et al. Relationship of brain-derived neurotrophic factor and its receptor TrkB to altered inhibitory prefrontal circuitry in schizophrenia. The Journal of Neuroscience. 2005;25(2):372–383. doi: 10.1523/JNEUROSCI.4035-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Di Cristo G, Chattopadhyaya B, Kuhlman SJ, et al. Activity-dependent PSA expression regulates inhibitory maturation and onset of critical period plasticity. Nature Neuroscience. 2007;10(12):1569–1577. doi: 10.1038/nn2008. [DOI] [PubMed] [Google Scholar]
- 133.Levitas A, Hagerman RJ, Braden M, Rimland B, McBogg P, Matus I. Autism and the fragile X syndrome. Journal of Developmental & Behavioral Pediatrics. 1983;4(3):151–158. doi: 10.1097/00004703-198309000-00002. [DOI] [PubMed] [Google Scholar]
- 134.Brown WT, Jenkins EC, Cohen IL, et al. Fragile X and autism: a multicenter survey. American Journal of Medical Genetics. 1986;23(1-2):341–352. doi: 10.1002/ajmg.1320230126. [DOI] [PubMed] [Google Scholar]
- 135.Jamain S, Quach H, Betancur C, et al. Mutations of the X-linked genes encoding neuroligins NLGN3 and NLGN4 are associated with autism. Nature Genetics. 2003;34(1):27–29. doi: 10.1038/ng1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Laumonnier F, Bonnet-Brilhault F, Gomot M, et al. X-linked mental retardation and autism are associated with a mutation in the NLGN4 gene, a member of the neuroligin family. American Journal of Human Genetics. 2004;74(3):552–557. doi: 10.1086/382137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Durand CM, Betancur C, Boeckers TM, et al. Mutations in the gene encoding the synaptic scaffolding protein SHANK3 are associated with autism spectrum disorders. Nature Genetics. 2007;39(1):25–27. doi: 10.1038/ng1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Gauthier J, Spiegelman D, Piton A, et al. Novel de novo SHANK3 mutation in autistic patients. American Journal of Medical Genetics Part B. 2009;150(3):421–424. doi: 10.1002/ajmg.b.30822. [DOI] [PubMed] [Google Scholar]
- 139.Moessner R, Marshall CR, Sutcliffe JS, et al. Contribution of SHANK3 mutations to autism spectrum disorder. American Journal of Human Genetics. 2007;81(6):1289–1297. doi: 10.1086/522590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Berkel S, Marshall CR, Weiss B, et al. Mutations in the SHANK2 synaptic scaffolding gene in autism spectrum disorder and mental retardation. Nature Genetics. 2010;42(6):489–491. doi: 10.1038/ng.589. [DOI] [PubMed] [Google Scholar]
- 141.Szatmari P, Paterson AD, Zwaigenbaum L, et al. Mapping autism risk loci using genetic linkage and chromosomal rearrangements. Nature Genetics. 2007;39(3):319–328. doi: 10.1038/ng1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kim HG, Kishikawa S, Higgins AW, et al. Disruption of neurexin 1 associated with autism spectrum disorder. American Journal of Human Genetics. 2008;82(1):199–207. doi: 10.1016/j.ajhg.2007.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Fatemi SH, Halt AR, Stary JM, Kanodia R, Schulz SC, Realmuto GR. Glutamic acid decarboxylase 65 and 67 kDa proteins are reduced in autistic parietal and cerebellar cortices. Biological Psychiatry. 2002;52(8):805–810. doi: 10.1016/s0006-3223(02)01430-0. [DOI] [PubMed] [Google Scholar]
- 144.Liu X, Novosedlik N, Wang A, et al. The DLX1and DLX2 genes and susceptibility to autism spectrum disorders. European Journal of Human Genetics. 2009;17(2):228–235. doi: 10.1038/ejhg.2008.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Baker P, Piven J, Schwartz S, Patil S. Brief report: duplication of chromosome 15q11-13 in two individuals with autistic disorder. Journal of Autism and Developmental Disorders. 1994;24(4):529–535. doi: 10.1007/BF02172133. [DOI] [PubMed] [Google Scholar]
- 146.Hogart A, Wu D, LaSalle JM, Schanen NC. The comorbidity of autism with the genomic disorders of chromosome 15q11.2-q13. Neurobiology of Disease. 2010;38(2):181–191. doi: 10.1016/j.nbd.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Amir RE, van den Veyver IB, Wan M, Tran CQ, Francke U, Zoghbi HY. Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nature Genetics. 1999;23(2):185–188. doi: 10.1038/13810. [DOI] [PubMed] [Google Scholar]
- 148.Buyse IM, Fang P, Hoon KT, Amir RE, Zoghbi HY, Roa BB. Diagnostic testing for Rett syndrome by DHPLC and direct sequencing analysis of the MECP2 gene: identification of several novel mutations and polymorphisms. American Journal of Human Genetics. 2000;67(6):1428–1436. doi: 10.1086/316913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Jackson PB, Boccuto L, Skinner C, et al. Further evidence that the rs1858830 C variant in the promoter region of the MET gene is associated with autistic disorder. Autism Research. 2009;2(4):232–236. doi: 10.1002/aur.87. [DOI] [PubMed] [Google Scholar]
- 150.Campbell DB, Sutcliffe JS, Ebert PJ, et al. A genetic variant that disrupts MET transcription is associated with autism. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(45):16834–16839. doi: 10.1073/pnas.0605296103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Dölen G, Osterweil E, Rao BSS, et al. Correction of fragile X syndrome in mice. Neuron. 2007;56(6):955–962. doi: 10.1016/j.neuron.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Bear MF, Huber KM, Warren ST. The mGluR theory of fragile X mental retardation. Trends in Neurosciences. 2004;27(7):370–377. doi: 10.1016/j.tins.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 153.Bear MF, Dölen G, Osterweil E, Nagarajan N. Fragile X: translation in action. Neuropsychopharmacology. 2008;33(1):84–87. doi: 10.1038/sj.npp.1301610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Scheiffele P, Fan J, Choih J, Fetter R, Serafini T. Neuroligin expressed in nonneuronal cells triggers presynaptic development in contacting axons. Cell. 2000;101(6):657–669. doi: 10.1016/s0092-8674(00)80877-6. [DOI] [PubMed] [Google Scholar]
- 155.Chih B, Engelman H, Scheiffele P, et al. Control of excitatory and inhibitory synapse formation by neuroligins. Science. 2005;307(5713):1324–1328. doi: 10.1126/science.1107470. [DOI] [PubMed] [Google Scholar]
- 156.Graf ER, Zhang X, Jin SX, Linhoff MW, Craig AM. Neurexins induce differentiation of GABA and glutamate postsynaptic specializations via neuroligins. Cell. 2004;119(7):1013–1026. doi: 10.1016/j.cell.2004.11.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Samaco RC, Hogart A, LaSalle JM. Epigenetic overlap in autism-spectrum neurodevelopmental disorders: MECP2 deficiency causes reduced expression of UBE3A and GABRB3 . Human Molecular Genetics. 2005;14(4):483–492. doi: 10.1093/hmg/ddi045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Chao HT, Chen H, Samaco RC, et al. Dysfunction in GABA signalling mediates autism-like stereotypies and Rett syndrome phenotypes. Nature. 2010;468(7321):263–269. doi: 10.1038/nature09582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Powell EM, Mars WM, Levitt P. Hepatocyte growth factor/scatter factor is a motogen for interneurons migrating from the ventral to dorsal telencephalon. Neuron. 2001;30(1):79–89. doi: 10.1016/s0896-6273(01)00264-1. [DOI] [PubMed] [Google Scholar]
- 160.Bae MH, Bissonette GB, Mars WM, et al. Hepatocyte growth factor (HGF) modulates GABAergic inhibition and seizure susceptibility. Experimental Neurology. 2010;221(1):129–135. doi: 10.1016/j.expneurol.2009.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Martins GJ, Shahrokh M, Powell EM. Genetic disruption of Met signaling impairs GABAergic striatal development and cognition. Neuroscience. 2010;176(10):199–209. doi: 10.1016/j.neuroscience.2010.12.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Claes L, Del-Favero J, Ceulemans B, Lagae L, van Broeckhoven C, de Jonghe P. De novo mutations in the sodium-channel gene SCN1A cause severe myoclonic epilepsy of infancy. American Journal of Human Genetics. 2001;68(6):1327–1332. doi: 10.1086/320609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Ohmori I, Ouchida M, Ohtsuka Y, Oka E, Shimizu K. Significant correlation of the SCN1A mutations and severe myoclonic epilepsy in infancy. Biochemical and Biophysical Research Communications. 2002;295(1):17–23. doi: 10.1016/s0006-291x(02)00617-4. [DOI] [PubMed] [Google Scholar]
- 164.Sugawara T, Mazaki-Miyazaki E, Fukushima K, et al. Frequent mutations of SCN1A in severe myoclonic epilepsy in infancy. Neurology. 2002;58(7):1122–1124. doi: 10.1212/wnl.58.7.1122. [DOI] [PubMed] [Google Scholar]
- 165.Orrico A, Galli L, Grosso S, et al. Mutational analysis of the SCN1A, SCN1B and GABRG2 genes in 150 Italian patients with idiopathic childhood epilepsies. Clinical Genetics. 2009;75(6):579–581. doi: 10.1111/j.1399-0004.2009.01155.x. [DOI] [PubMed] [Google Scholar]
- 166.Escayg A, Goldin AL. Sodium channel SCN1A and epilepsy: mutations and mechanisms. Epilepsia. 2010;51(9):1650–1658. doi: 10.1111/j.1528-1167.2010.02640.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Escayg A, MacDonald BT, Meisler MH, et al. Mutations of SCN1A, encoding a neuronal sodium channel, in two families with GEFS+2. Nature Genetics. 2000;24(4):343–345. doi: 10.1038/74159. [DOI] [PubMed] [Google Scholar]
- 168.Escayg A, Heils A, Macdonald BT, Haug K, Sander T, Meisler MH. A novel SCN1A mutation associated with generalized epilepsy with febrile seizures plus—and prevalence of variants in patients with epilepsy. American Journal of Human Genetics. 2001;68(4):866–873. doi: 10.1086/319524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Fujiwara T, Sugawara T, Mazaki-Miyazaki E, et al. Mutations of sodium channel α subunit type 1 (SCN1A) in intractable childhood epilepsies with frequent generalized tonic-clonic seizures. Brain. 2003;126(3):531–546. doi: 10.1093/brain/awg053. [DOI] [PubMed] [Google Scholar]
- 170.Osaka H, Ogiwara I, Mazaki E, et al. Patients with a sodium channel alpha 1 gene mutation show wide phenotypic variation. Epilepsy Research. 2007;75(1):46–51. doi: 10.1016/j.eplepsyres.2007.03.018. [DOI] [PubMed] [Google Scholar]
- 171.Zucca C, Redaelli F, Epifanio R, et al. Cryptogenic epileptic syndromes related to SCN1A: twelve novel mutations identified. Archives of Neurology. 2008;65(4):489–494. doi: 10.1001/archneur.65.4.489. [DOI] [PubMed] [Google Scholar]
- 172.Martin MS, Tang B, Papale LA, Yu FH, Catterall WA, Escayg A. The voltage-gated sodium channel Scn8a is a genetic modifier of severe myoclonic epilepsy of infancy. Human Molecular Genetics. 2007;16(23):2892–2899. doi: 10.1093/hmg/ddm248. [DOI] [PubMed] [Google Scholar]
- 173.Ohmori I, Ouchida M, Miki T, et al. A CACNB4 mutation shows that altered Cav2.1 function may be a genetic modifier of severe myoclonic epilepsy in infancy. Neurobiology of Disease. 2008;32(3):349–354. doi: 10.1016/j.nbd.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 174.Wallace RH, Marini C, Petrou S, et al. Mutant GABAA receptor γ2-subunit in childhood absence epilepsy and febrile seizures. Nature Genetics. 2001;28(1):49–52. doi: 10.1038/ng0501-49. [DOI] [PubMed] [Google Scholar]
- 175.Shoubridge C, Fullston T, Gécz J. ARX spectrum disorders: making inroads into the molecular pathology. Human Mutation. 2010;31(8):889–900. doi: 10.1002/humu.21288. [DOI] [PubMed] [Google Scholar]
- 176.Kalscheuer VM, Tao J, Donnelly A, et al. Disruption of the serine/threonine kinase 9 gene causes severe X-linked infantile spasms and mental retardation. American Journal of Human Genetics. 2003;72(6):1401–1411. doi: 10.1086/375538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Weaving LS, Christodoulou J, Williamson SL, et al. Mutations of CDKL5 cause a severe neurodevelopmental disorder with infantile spasms and mental retardation. American Journal of Human Genetics. 2004;75(6):1079–1093. doi: 10.1086/426462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Scala E, Ariani F, Mari F, et al. CDKL5/STK9 is mutated in Rett syndrome variant with infantile spasms. Journal of Medical Genetics. 2005;42(2):103–107. doi: 10.1136/jmg.2004.026237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Archer HL, Evans J, Edwards S, et al. CDKL5 mutations cause infantile spasms, early onset seizures, and severe mental retardation in female patients. Journal of Medical Genetics. 2006;43(9):729–734. doi: 10.1136/jmg.2006.041467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Cordova-Fletes C, Rademacher N, Muller I, et al. CDKL5 truncation due to a t(X;2)(p22.1;p25.3) in a girl with X-linked infantile spasm syndrome. Clinical Genetics. 2010;77(1):92–96. doi: 10.1111/j.1399-0004.2009.01286.x. [DOI] [PubMed] [Google Scholar]
- 181.Mei D, Marini C, Novara F, et al. Xp22.3 genomic deletions involving the CDKL5 gene in girls with early onset epileptic encephalopathy. Epilepsia. 2010;51(4):647–654. doi: 10.1111/j.1528-1167.2009.02308.x. [DOI] [PubMed] [Google Scholar]
- 182.Melani F, Mei D, Pisano T, et al. CDKL5 gene-related epileptic encephalopathy: electroclinical findings in the first year of life. Developmental Medicine and Child Neurology. 2010;53,(4):354–360. doi: 10.1111/j.1469-8749.2010.03889.x. [DOI] [PubMed] [Google Scholar]
- 183.Kananura C, Haug K, Sander T, et al. A splice-site mutation in GABRG2 associated with childhood absence epilepsy and febrile convulsions. Archives of Neurology. 2002;59(7):1137–1141. doi: 10.1001/archneur.59.7.1137. [DOI] [PubMed] [Google Scholar]
- 184.Harkin LA, Bowser DN, Dibbens LM, et al. Truncation of the GABAA-receptor γ2 subunit in a family with generalized epilepsy with febrile seizures plus. American Journal of Human Genetics. 2002;70(2):530–536. doi: 10.1086/338710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Cossette P, Liu L, Brisebois K, et al. Mutation of GABRA1 in an autosomal dominant form of juvenile myoclonic epilepsy. Nature Genetics. 2002;31(2):184–189. doi: 10.1038/ng885. [DOI] [PubMed] [Google Scholar]
- 186.Maljevic S, Krampfl K, Cobilanschi J, et al. A mutation in the GABAA receptor α 1-subunit is associated with absence epilepsy. Annals of Neurology. 2006;59:983–987. doi: 10.1002/ana.20874. [DOI] [PubMed] [Google Scholar]
- 187.Chioza B, Wilkie H, Nashef L, et al. Association between the α1a calcium channel gene CACNA1A and idiopathic generalized epilepsy. Neurology. 2001;56(9):1245–1246. doi: 10.1212/wnl.56.9.1245. [DOI] [PubMed] [Google Scholar]
- 188.Jouvenceau A, Eunson LH, Spauschus A, et al. Human epilepsy associated with dysfunction of the brain P/Q-type calcium channel. The Lancet. 2001;358(9284):801–807. doi: 10.1016/S0140-6736(01)05971-2. [DOI] [PubMed] [Google Scholar]
- 189.Imbrici P, Jaffe SL, Eunson LH, et al. Dysfunction of the brain calcium channel Cav2.1 in absence epilepsy and episodic ataxia. Brain. 2004;127(12):2682–2692. doi: 10.1093/brain/awh301. [DOI] [PubMed] [Google Scholar]
- 190.Escayg A, de Waard M, Lee DD, et al. Coding and noncoding variation of the human calcium-channel β4-subunit gene CACNB4 in patients with idiopathic generalized epilepsy and episodic ataxia. American Journal of Human Genetics. 2000;66(5):1531–1539. doi: 10.1086/302909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Khosravani H, Altier C, Simms B, et al. Gating effects of mutations in the Cav3.2 T-type calcium channel associated with childhood absence epilepsy. Journal of Biological Chemistry. 2004;279(11):9681–9684. doi: 10.1074/jbc.C400006200. [DOI] [PubMed] [Google Scholar]
- 192.Carré A, Szinnai G, Castanet M, et al. Five new TTF1/NKX2.1 mutations in brain-lung-thyroid syndrome: rescue by PAX8 synergism in one case. Human Molecular Genetics. 2009;18(12):2266–2276. doi: 10.1093/hmg/ddp162. [DOI] [PubMed] [Google Scholar]
- 193.Guillot L, Carré A, Szinnai G, et al. NKX2-1 mutations leading to surfactant protein promoter dysregulation cause interstitial lung disease in ‘brain-lung-thyroid syndrome’. Human Mutation. 2010;31(2):E1146–E1162. doi: 10.1002/humu.21183. [DOI] [PubMed] [Google Scholar]
- 194.Kleiner-Fisman G, Rogaeva E, Halliday W, et al. Benign hereditary chorea: clinical, genetic, and pathological findings. Annals of Neurology. 2003;54(2):244–247. doi: 10.1002/ana.10637. [DOI] [PubMed] [Google Scholar]
- 195.Kleiner-Fisman G, Lang AE. Benign hereditary chorea revisited: a journey to understanding. Movement Disorders. 2007;22(16):2297–2305. doi: 10.1002/mds.21644. [DOI] [PubMed] [Google Scholar]
- 196.Morasso MI, Radoja N. Dlx genes, p63, and ectodermal dysplasias. Birth Defects Research C. 2005;75(3):163–171. doi: 10.1002/bdrc.20047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Iacono NL, Mantero S, Chiarelli A, et al. Regulation of Dlx5 and Dlx6 gene expression by p63 is involved in EEC and SHFM congenital limb defects. Development. 2008;135(7):1377–1388. doi: 10.1242/dev.011759. [DOI] [PubMed] [Google Scholar]
- 198.Tagariello A, Heller R, Greven A, et al. Balanced translocation in a patient with craniosynostosis disrupts the SOX6 gene and an evolutionarily conserved non-transcribed region. Journal of Medical Genetics. 2006;43(6):534–540. doi: 10.1136/jmg.2005.037820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Yu FH, Mantegazza M, Westenbroek RE, et al. Reduced sodium current in GABAergic interneurons in a mouse model of severe myoclonic epilepsy in infancy. Nature Neuroscience. 2006;9(9):1142–1149. doi: 10.1038/nn1754. [DOI] [PubMed] [Google Scholar]
- 200.Martin MS, Dutt K, Papale LA, et al. Altered function of the SCN1A voltage-gated sodium channel leads to γ-aminobutyric acid-ergic (GABAergic) interneuron abnormalities. Journal of Biological Chemistry. 2010;285(13):9823–9834. doi: 10.1074/jbc.M109.078568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Friocourt G, Kanatani S, Tabata H, et al. Cell-autonomous roles of ARX in cell proliferation and neuronal migration during corticogenesis. The Journal of Neuroscience. 2008;28(22):5794–5805. doi: 10.1523/JNEUROSCI.1067-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Friocourt G, Poirier K, Rakić S, Parnavelas JG, Chelly J. The role of ARX in cortical development. European Journal of Neuroscience. 2006;23(4):869–876. doi: 10.1111/j.1460-9568.2006.04629.x. [DOI] [PubMed] [Google Scholar]
- 203.Friocourt G, Parnavelas JG. Mutations in ARX result in several defects involving GABAergic neurons. Frontiers in Cellular Neuroscience. 2010;4, article 4 doi: 10.3389/fncel.2010.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Poirier K, van Esch H, Friocourt G, et al. Neuroanatomical distribution of ARX in brain and its localisation in GABAergic neurons. Molecular Brain Research. 2004;122(1):35–46. doi: 10.1016/j.molbrainres.2003.11.021. [DOI] [PubMed] [Google Scholar]
- 205.Colasante G, Collombat P, Raimondi V, et al. Arx is a direct target of Dlx2 and thereby contributes to the tangential migration of GABAergic interneurons. The Journal of Neuroscience. 2008;28(42):10674–10686. doi: 10.1523/JNEUROSCI.1283-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Price MG, Yoo JW, Burgess DL, et al. A triplet repeat expansion genetic mouse model of infantile spasms syndrome, Arx(GCG)10+7, with interneuronopathy, spasms in infancy, persistent seizures, and adult cognitive and behavioral impairment. The Journal of Neuroscience. 2009;29(27):8752–8763. doi: 10.1523/JNEUROSCI.0915-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Marsh E, Fulp C, Gomez E, et al. Targeted loss of Arx results in a developmental epilepsy mouse model and recapitulates the human phenotype in heterozygous females. Brain. 2009;132(6):1563–1576. doi: 10.1093/brain/awp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Mari F, Azimonti S, Bertani I, et al. CDKL5 belongs to the same molecular pathway of MeCP2 and it is responsible for the early-onset seizure variant of Rett syndrome. Human Molecular Genetics. 2005;14(14):1935–1946. doi: 10.1093/hmg/ddi198. [DOI] [PubMed] [Google Scholar]
- 209.Bertani I, Rusconi L, Bolognese F, et al. Functional consequences of mutations in CDKL5, an X-linked gene involved in infantile spasms and mental retardation. Journal of Biological Chemistry. 2006;281(42):32048–32056. doi: 10.1074/jbc.M606325200. [DOI] [PubMed] [Google Scholar]
- 210.Nan X, Ng HH, Johnson CA, et al. Transcriptional repression by the methyl-CpG-binding protein MeCP2 involves a histone deacetylase complex. Nature. 1998;393(6683):386–389. doi: 10.1038/30764. [DOI] [PubMed] [Google Scholar]
- 211.Nan X, Bird A. The biological functions of the methyl-CpG-binding protein MeCP2 and its implication in Rett syndrome. Brain and Development. 2001;23(1):S32–S37. doi: 10.1016/s0387-7604(01)00333-3. [DOI] [PubMed] [Google Scholar]
- 212.Noebels JL, Sidman RL. Inherited epilepsy: spike-wave and focal motor seizures in the mutant mouse tottering. Science. 1979;204(4399):1334–1336. doi: 10.1126/science.572084. [DOI] [PubMed] [Google Scholar]
- 213.Fletcher CF, Lutz CM, O’Sullivan TN, et al. Absence epilepsy in tottering mutant mice is associated with calcium channel defects. Cell. 1996;87(4):607–617. doi: 10.1016/s0092-8674(00)81381-1. [DOI] [PubMed] [Google Scholar]
- 214.Zhang Y, Mori M, Burgess DL, Noebels JL. Mutations in high-voltage-activated calcium channel genes stimulate low-voltage-activated currents in mouse thalamic relay neurons. The Journal of Neuroscience. 2002;22(15):6362–6371. doi: 10.1523/JNEUROSCI.22-15-06362.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Tsakiridou E, Bertollini L, de Curtis M, Avanzini G, Pape HC. Selective increase in T-type calcium conductance of reticular thalamic neurons in a rat model of absence epilepsy. The Journal of Neuroscience. 1995;15(4):3110–3117. doi: 10.1523/JNEUROSCI.15-04-03110.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Burgess DL, Jones JM, Meisler MH, Noebels JL. Mutation of the Ca2+ channel β subunit gene Cchb4 is associated with ataxia and seizures in the lethargic (lh) mouse. Cell. 1997;88(3):385–392. doi: 10.1016/s0092-8674(00)81877-2. [DOI] [PubMed] [Google Scholar]
- 217.Cope DW, Di Giovanni G, Fyson SJ, et al. Enhanced tonic GABAA inhibition in typical absence epilepsy. Nature Medicine. 2009;15:1392–1398. doi: 10.1038/nm.2058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Anderson SA, Eisenstat DD, Shi L, Rubenstein JLR. Interneuron migration from basal forebrain to neocortex: dependence on Dlx genes. Science. 1997;278(5337):474–476. doi: 10.1126/science.278.5337.474. [DOI] [PubMed] [Google Scholar]
- 219.Bulfone A, Wang F, Hevner R, et al. An olfactory sensory map develops in the absence of normal projection neurons or GABAergic interneurons. Neuron. 1998;21(6):1273–1282. doi: 10.1016/s0896-6273(00)80647-9. [DOI] [PubMed] [Google Scholar]
- 220.Cobos I, Borello U, Rubenstein JLR. Dlx transcription factors promote migration through repression of axon and dendrite growth. Neuron. 2007;54(6):873–888. doi: 10.1016/j.neuron.2007.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Cobos I, Calcagnotto ME, Vilaythong AJ, et al. Mice lacking Dlx1 show subtype-specific loss of interneurons, reduced inhibition and epilepsy. Nature Neuroscience. 2005;8(8):1059–1068. doi: 10.1038/nn1499. [DOI] [PubMed] [Google Scholar]
- 222.Sussel L, Marin O, Kimura S, Rubenstein JLR. Loss of Nkx2.1 homeobox gene function results in a ventral to dorsal molecular respecification within the basal telencephalon: evidence for a transformation of the pallidum into the striatum. Development. 1999;126(15):3359–3370. doi: 10.1242/dev.126.15.3359. [DOI] [PubMed] [Google Scholar]
- 223.Azim E, Jabaudon D, Fame RM, MacKlis JD. SOX6 controls dorsal progenitor identity and interneuron diversity during neocortical development. Nature Neuroscience. 2009;12(10):1238–1247. doi: 10.1038/nn.2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Le Bon-Jego M, Yuste R. Persistently active, pacemaker-like neurons in neocortex. Frontiers in Neuroscience. 2007;1(1):123–129. doi: 10.3389/neuro.01.1.1.009.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Xu X, Roby KD, Callaway EM. Mouse cortical inhibitory neuron type that coexpresses somatostatin and calretinin. Journal of Comparative Neurology. 2006;499(1):144–160. doi: 10.1002/cne.21101. [DOI] [PubMed] [Google Scholar]
- 226.Xu X, Roby KD, Callaway EM. Immunochemical characterization of inhibitory mouse cortical neurons: three chemically distinct classes of inhibitory cells. Journal of Comparative Neurology. 2010;518(3):389–404. doi: 10.1002/cne.22229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Porter JT, Cauli B, Staiger JF, Lambolez B, Rossier J, Audinat E. Properties of bipolar VIPergic interneurons and their excitation by pyramidal neurons in the rat neocortex. European Journal of Neuroscience. 1998;10(12):3617–3628. doi: 10.1046/j.1460-9568.1998.00367.x. [DOI] [PubMed] [Google Scholar]
- 228.Acsády L, Arabadzisz D, Freund TF. Correlated morphological and neurochemical features identify different subsets of vasoactive intestinal polypeptide-immunoreactive interneurons in rat hippocampus. Neuroscience. 1996;73(2):299–315. doi: 10.1016/0306-4522(95)00610-9. [DOI] [PubMed] [Google Scholar]
- 229.Hajos N, Acsady L, Freund TF. Target selectivity and neurochemical characteristics of VIP-immunoreactive interneurons in the rat dentate gyrus. European Journal of Neuroscience. 1996;8(7):1415–1431. doi: 10.1111/j.1460-9568.1996.tb01604.x. [DOI] [PubMed] [Google Scholar]
- 230.Dávid C, Schleicher A, Zuschratter W, Staiger JF. The innervation of parvalbumin-containing interneurons by VIP-immunopositive interneurons in the primary somatosensory cortex of the adult rat. European Journal of Neuroscience. 2007;25(8):2329–2340. doi: 10.1111/j.1460-9568.2007.05496.x. [DOI] [PubMed] [Google Scholar]
- 231.Xu X, Callaway EM. Laminar specificity of functional input to distinct types of inhibitory cortical neurons. The Journal of Neuroscience. 2009;29(1):70–85. doi: 10.1523/JNEUROSCI.4104-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Karagiannis A, Gallopin T, Dávid C, et al. Classification of NPY-expressing neocortical interneurons. The Journal of Neuroscience. 2009;29(11):3642–3659. doi: 10.1523/JNEUROSCI.0058-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Olah S, Komlosi G, Szabadics J, et al. Output of neurogliaform cells to various neuron types in the human and rat cerebral cortex. Frontiers in Neural Circuits. 2007;1, article 4 doi: 10.3389/neuro.04.004.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Tamás G, Lörincz A, Simon A, Szabadics J. Identified sources and targets of slow inhibition in the neocortex. Science. 2003;299(5614):1902–1905. doi: 10.1126/science.1082053. [DOI] [PubMed] [Google Scholar]
- 235.Olah S, Fule M, Komlosi G, et al. Regulation of cortical microcircuits by unitary GABA-mediated volume transmission. Nature. 2009;461(7268):1278–1281. doi: 10.1038/nature08503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Biagini G, Panuccio G, Avoli M. Neurosteroids and epilepsy. Current Opinion in Neurology. 2010;23(2):170–176. doi: 10.1097/WCO.0b013e32833735cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Pellock JM, Hrachovy R, Shinnar S, et al. Infantile spasms: a U.S. consensus report. Epilepsia. 2010;51(10):2175–2189. doi: 10.1111/j.1528-1167.2010.02657.x. [DOI] [PubMed] [Google Scholar]
- 238.Price CJ, Cauli B, Kovacs ER, et al. Neurogliaform neurons form a novel inhibitory network in the hippocampal CA1 area. The Journal of Neuroscience. 2005;25(29):6775–6786. doi: 10.1523/JNEUROSCI.1135-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Simon A, Olah S, Molnar G, Szabadics J, Tamas G. Gap-junctional coupling between neurogliaform cells and various interneuron types in the neocortex. The Journal of Neuroscience. 2005;25(27):6278–6285. doi: 10.1523/JNEUROSCI.1431-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Zsiros V, Maccaferri G. Electrical coupling between interneurons with different excitable properties in the stratum lacunosum-moleculare of the juvenile CA1 rat hippocampus. The Journal of Neuroscience. 2005;25(38):8686–8695. doi: 10.1523/JNEUROSCI.2810-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Cauli B, Tong XK, Rancillac A, et al. Cortical GABA interneurons in neurovascular coupling: relays for subcortical vasoactive pathways. The Journal of Neuroscience. 2004;24(41):8940–8949. doi: 10.1523/JNEUROSCI.3065-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Cauli B, Hamel E. Revisiting the role of neurons in neurovascular coupling. Frontiers in Neuroenergetics. 2010;2, article 9 doi: 10.3389/fnene.2010.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Anderson S, Mione M, Yun K, Rubenstein JLR. Differential origins of neocortical projection and local circuit neurons: role of Dlx genes in neocortical interneuronogenesis. Cerebral Cortex. 1999;9(6):646–654. doi: 10.1093/cercor/9.6.646. [DOI] [PubMed] [Google Scholar]
- 244.Anderson SA, Marín O, Horn C, Jennings K, Rubenstein JLR. Distinct cortical migrations from the medial and lateral ganglionic eminences. Development. 2001;128(3):353–363. doi: 10.1242/dev.128.3.353. [DOI] [PubMed] [Google Scholar]
- 245.Corbin JG, Nery S, Fishell G. Telencephalic cells take a tangent: non-radial migration in the mammalian forebrain. Nature Neuroscience. 2001;4(1):1177–1182. doi: 10.1038/nn749. [DOI] [PubMed] [Google Scholar]
- 246.Miyoshi G, Fishell G. GABAergic interneuron lineages selectively sort into specific cortical layers during early postnatal development. Cerebral Cortex. 2011;21(4):845–852. doi: 10.1093/cercor/bhq155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Porteus MH, Bulfone A, Liu JK, Puelles L, Lo LC, Rubenstein JLR. DLX-2, MASH-1, and MAP-2 expression and bromodeoxyuridine incorporation define molecularly distinct cell populations in the embryonic mouse forebrain. The Journal of Neuroscience. 1994;14(11):6370–6383. doi: 10.1523/JNEUROSCI.14-11-06370.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Pleasure SJ, Anderson S, Hevner R, et al. Cell migration from the ganglionic eminences is required for the development of hippocampal GABAergic interneurons. Neuron. 2000;28(3):727–740. doi: 10.1016/s0896-6273(00)00149-5. [DOI] [PubMed] [Google Scholar]
- 249.Kohwi M, Petryniak MA, Long JE, et al. A subpopulation of olfactory bulb GABAergic interneurons is derived from Emx1- and Dlx5/6-expressing progenitors. The Journal of Neuroscience. 2007;27(26):6878–6891. doi: 10.1523/JNEUROSCI.0254-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Casarosa S, Fode C, Guillemot F. Mash1 regulates neurogenesis in the ventral telencephalon. Development. 1999;126(3):525–534. doi: 10.1242/dev.126.3.525. [DOI] [PubMed] [Google Scholar]
- 251.Fogarty M, Grist M, Gelman D, Marín O, Pachnis V, Kessaris N. Spatial genetic patterning of the embryonic neuroepithelium generates GABAergic interneuron diversity in the adult cortex. The Journal of Neuroscience. 2007;27(41):10935–10946. doi: 10.1523/JNEUROSCI.1629-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Wonders CP, Taylor L, Welagen J, Mbata IC, Xiang JZ, Anderson SA. A spatial bias for the origins of interneuron subgroups within the medial ganglionic eminence. Developmental Biology. 2008;314(1):127–136. doi: 10.1016/j.ydbio.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Flames N, Pla R, Gelman DM, Rubenstein JLR, Puelles L, Marín O. Delineation of multiple subpallial progenitor domains by the combinatorial expression of transcriptional codes. The Journal of Neuroscience. 2007;27(36):9682–9695. doi: 10.1523/JNEUROSCI.2750-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Xu Q, Guo L, Moore H, Waclaw RR, Campbell K, Anderson SA. Sonic hedgehog signaling confers ventral telencephalic progenitors with distinct cortical interneuron fates. Neuron. 2010;65(3):328–340. doi: 10.1016/j.neuron.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Sousa VH, Miyoshi G, Hjerling-Leffler J, Karayannis T, Fishell G. Characterization of Nkx6-2-derived neocortical interneuron lineages. Cerebral Cortex. 2009;19(supplement 1):i1–i10. doi: 10.1093/cercor/bhp038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Grigoriou M, Tucker AS, Sharpe PT, Pachnis V. Expression and regulation of Lhx6 and Lhx7, a novel subfamily of LIM homeodomain encoding genes, suggests a role in mammalian head development. Development. 1998;125(11):2063–2074. doi: 10.1242/dev.125.11.2063. [DOI] [PubMed] [Google Scholar]
- 257.Liodis P, Denaxa M, Grigoriou M, Akufo-Addo C, Yanagawa Y, Pachnis V. Lhx6 activity is required for the normal migration and specification of cortical interneuron subtypes. The Journal of Neuroscience. 2007;27(12):3078–3089. doi: 10.1523/JNEUROSCI.3055-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Zhao Y, Flandin P, Long JE, Cuesta MD, Westphal H, Rubenstein JLR. Distinct molecular pathways of development of telencephalic interneuron subtypes revealed through analysis of Lhx6 mutants. Journal of Comparative Neurology. 2008;510(1):79–99. doi: 10.1002/cne.21772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Andäng M, Hjerling-Leffler J, Moliner A, et al. Histone H2AX-dependent GABAA receptor regulation of stem cell proliferation. Nature. 2008;451(7177):460–464. doi: 10.1038/nature06488. [DOI] [PubMed] [Google Scholar]
- 260.LoTurco JJ, Owens DF, Heath MJS, Davis MBE, Kriegstein AR. GABA and glutamate depolarize cortical progenitor cells and inhibit DNA synthesis. Neuron. 1995;15(6):1287–1298. doi: 10.1016/0896-6273(95)90008-x. [DOI] [PubMed] [Google Scholar]
- 261.Heck N, Kilb W, Reiprich P, et al. GABA-A receptors regulate neocortical neuronal migration in vitro and in vivo. Cerebral Cortex. 2007;17(1):138–148. doi: 10.1093/cercor/bhj135. [DOI] [PubMed] [Google Scholar]
- 262.Tyzio R, Represa A, Jorquera I, Ben-Ari Y, Gozlan H, Aniksztejn L. The establishment of GABAergic and glutamatergic synapses on CA1 pyramidal neurons is sequential and correlates with the development of the apical dendrite. The Journal of Neuroscience. 1999;19(23):10372–10382. doi: 10.1523/JNEUROSCI.19-23-10372.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Hennou S, Khalilov I, Diabira D, Ben-Ari Y, Gozlan H. Early sequential formation of functional GABAA and glutamatergic synapses on CA1 interneurons of the rat foetal hippocampus. European Journal of Neuroscience. 2002;16(2):197–208. doi: 10.1046/j.1460-9568.2002.02073.x. [DOI] [PubMed] [Google Scholar]
- 264.Delpire E. Cation-chloride cotransporters in neuronal communication. News in Physiological Sciences. 2000;15(6):309–312. doi: 10.1152/physiologyonline.2000.15.6.309. [DOI] [PubMed] [Google Scholar]
- 265.Rivera C, Voipio J, Payne JA, et al. The K+/Cl− co-transporter KCC2 renders GABA hyperpolarizing during neuronal maturation. Nature. 1999;397(6716):251–255. doi: 10.1038/16697. [DOI] [PubMed] [Google Scholar]
- 266.Li H, Tornberg J, Kaila K, Airaksinen MS, Rivera C. Patterns of cation-chloride cotransporter expression during embryonic rodent CNS development. European Journal of Neuroscience. 2002;16(12):2358–2370. doi: 10.1046/j.1460-9568.2002.02419.x. [DOI] [PubMed] [Google Scholar]
- 267.Manent JB, Demarque M, Jorquera I, et al. A noncanonical release of GABA and glutamate modulates neuronal migration. The Journal of Neuroscience. 2005;25(19):4755–4765. doi: 10.1523/JNEUROSCI.0553-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Bortone D, Polleux F. KCC2 expression promotes the termination of cortical interneuron migration in a voltage-sensitive calcium-dependent manner. Neuron. 2009;62(1):53–71. doi: 10.1016/j.neuron.2009.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Wang DD, Kriegstein AR. GABA regulates excitatory synapse formation in the neocortex via NMDA receptor activation. The Journal of Neuroscience. 2008;28(21):5547–5558. doi: 10.1523/JNEUROSCI.5599-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Wang DD, Kriegstein AR. Blocking early GABA depolarization with bumetanide results in permanent alterations in cortical circuits and sensorimotor gating deficits. Cerebral Cortex. 2011;21(3):574–587. doi: 10.1093/cercor/bhq124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Cancedda L, Fiumelli H, Chen K, Poo MM. Excitatory GABA action is essential for morphological maturation of cortical neurons in vivo. The Journal of Neuroscience. 2007;27(19):5224–5235. doi: 10.1523/JNEUROSCI.5169-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Cossart R. The maturation of cortical interneuron diversity: how multiple developmental journeys shape the emergence of proper network function. Current Opinion in Neurobiology. 2010;21(1):160–168. doi: 10.1016/j.conb.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 273.Hensch TK, Fagiolini M, Mataga N, Stryker MP, Baekkeskov S, Kash SF. Local GABA circuit control of experience-dependent plasticity in developing visual cortex. Science. 1998;282(5393):1504–1508. doi: 10.1126/science.282.5393.1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Fagiolini M, Fritschy JM, Low K, Mohler H, Rudolph U, Hensch TK. Specific GABAA circuits for visual cortical plasticity. Science. 2004;303(5664):1681–1683. doi: 10.1126/science.1091032. [DOI] [PubMed] [Google Scholar]
- 275.Yazaki-Sugiyama Y, Kang S, Cteau H, Fukai T, Hensch TK. Bidirectional plasticity in fast-spiking GABA circuits by visual experience. Nature. 2009;462(7270):218–221. doi: 10.1038/nature08485. [DOI] [PubMed] [Google Scholar]
- 276.Harauzov A, Spolidoro M, DiCristo G, et al. Reducing intracortical inhibition in the adult visual cortex promotes ocular dominance plasticity. The Journal of Neuroscience. 2010;30(1):361–371. doi: 10.1523/JNEUROSCI.2233-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Crépel V, Aronov D, Jorquera I, Represa A, Ben-Ari Y, Cossart R. A parturition-associated nonsynaptic coherent activity pattern in the developing hippocampus. Neuron. 2007;54(1):105–120. doi: 10.1016/j.neuron.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 278.Allène C, Cattani A, Ackman JB, et al. Sequential generation of two distinct synapse-driven network patterns in developing neocortex. The Journal of Neuroscience. 2008;28(48):12851–12863. doi: 10.1523/JNEUROSCI.3733-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Ben-Ari Y, Cherubini E, Corradetti R, Gaiarsa JL. Giant synaptic potentials in immature rat CA3 hippocampal neurones. Journal of Physiology. 1989;416:303–325. doi: 10.1113/jphysiol.1989.sp017762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Bonifazi P, Goldin M, Picardo MA, et al. GABAergic hub neurons orchestrate synchrony in developing hippocampal networks. Science. 2009;326(5958):1419–1424. doi: 10.1126/science.1175509. [DOI] [PubMed] [Google Scholar]
- 281.Lundorf MD, Buttenschon HN, Foldager L, et al. Mutational screening and association study of glutamate decarboxylase 1 as a candidate susceptibility gene for bipolar affective disorder and schizophrenia. American Journal of Medical Genetics Part B. 2005;135(1):94–101. doi: 10.1002/ajmg.b.30137. [DOI] [PubMed] [Google Scholar]
- 282.Batista-Brito R, MacHold R, Klein C, Fishell G. Gene expression in cortical interneuron precursors is prescient of their mature function. Cerebral Cortex. 2008;18(10):2306–2317. doi: 10.1093/cercor/bhm258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.DeFelipe J. Cortical interneurons: from Cajal to 2001. Progress in Brain Research. 2002;136:215–238. doi: 10.1016/s0079-6123(02)36019-9. [DOI] [PubMed] [Google Scholar]
- 284.Rakic P. Evolution of the neocortex: a perspective from developmental biology. Nature Reviews Neuroscience. 2009;10(10):724–735. doi: 10.1038/nrn2719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.DeFelipe J. Types of neurons, synaptic connections and chemical characteristics of cells immunoreactive for calbindin-D28K, parvalbumin and calretinin in the neocortex. Journal of Chemical Neuroanatomy. 1997;14(1):1–19. doi: 10.1016/s0891-0618(97)10013-8. [DOI] [PubMed] [Google Scholar]
- 286.DeFelipe J, Alonso-Nanclares L, Arellano JI. Microstructure of the neocortex: comparative aspects. Journal of Neurocytology. 2002;31(3–5):299–316. doi: 10.1023/a:1024130211265. [DOI] [PubMed] [Google Scholar]
- 287.Letinic K, Zoncu R, Rakic P. Origin of GABAergic neurons in the human neocortex. Nature. 2002;417(6889):645–649. doi: 10.1038/nature00779. [DOI] [PubMed] [Google Scholar]
- 288.Rakic S, Zecevic N. Emerging complexity of layer I in human cerebral cortex. Cerebral Cortex. 2003;13(10):1072–1083. doi: 10.1093/cercor/13.10.1072. [DOI] [PubMed] [Google Scholar]
- 289.Yu X, Zecevic N. Dorsal radial glial cells have the potential to generate cortical interneurons in human but not in mouse brain. The Journal of Neuroscience. 2011;31(7):2413–2420. doi: 10.1523/JNEUROSCI.5249-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Lindsay S, Sarma S, Martínez-de-la-Torre M, et al. Anatomical and gene expression mapping of the ventral pallium in a three-dimensional model of developing human brain. Neuroscience. 2005;136(3):625–632. doi: 10.1016/j.neuroscience.2005.06.093. [DOI] [PubMed] [Google Scholar]
- 291.Sarma S, Kerwin J, Puelles L, et al. 3D modelling, gene expression mapping and post-mapping image analysis in the developing human brain. Brain Research Bulletin. 2005;66(4–6):449–453. doi: 10.1016/j.brainresbull.2005.05.022. [DOI] [PubMed] [Google Scholar]
- 292.Jakovcevski I, Mayer N, Zecevic N. Multiple origins of human neocortical interneurons are supported by distinct expression of transcription factors. Cerebral Cortex. 2011;21(8):1771–1782. doi: 10.1093/cercor/bhq245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Zecevic N, Hu F, Jakovcevski I. Interneurons in the developing human neocortex. Developmental Neurobiology. 2011;71(1):18–33. doi: 10.1002/dneu.20812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.DSM-IV. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC, USA: American Psychiatric Association; 1994. [Google Scholar]
- 295.Elvevag B, Goldberg TE. Cognitive impairment in schizophrenia is the core of the disorder. Critical Reviews in Neurobiology. 2000;14(1):1–21. [PubMed] [Google Scholar]
- 296.Cohen JR, Elvevåg B, Goldberg TE. Cognitive control and semantics in schizophrenia: an integrated approach. American Journal of Psychiatry. 2005;162(10):1969–1971. doi: 10.1176/appi.ajp.162.10.1969. [DOI] [PubMed] [Google Scholar]
- 297.Qin ZH, Zhang SP, Weiss B. Dopaminergic and glutamatergic blocking drugs differentially regulate glutamic acid decarboxylase mRNA in mouse brain. Molecular Brain Research. 1994;21(3-4):293–302. doi: 10.1016/0169-328x(94)90260-7. [DOI] [PubMed] [Google Scholar]
- 298.Gierdalski M, Jablonska B, Smith A, Skangiel-Kramska J, Kossut M. Deafferentation induced changes in GAD67 and GluR2 mRNA expression in mouse somatosensory cortex. Molecular Brain Research. 1999;71(1):111–119. doi: 10.1016/s0169-328x(99)00153-9. [DOI] [PubMed] [Google Scholar]
- 299.Woo RS, Li XM, Tao Y, et al. Neuregulin-1 enhances depolarization-induced GABA release. Neuron. 2007;54(4):599–610. doi: 10.1016/j.neuron.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 300.Volk DW, Pierri JN, Fritschy JM, Auh S, Sampson AR, Lewis DA. Reciprocal alterations in pre- and postsynaptic inhibitory markers at chandelier cell inputs to pyramidal neurons in schizophrenia. Cerebral Cortex. 2002;12(10):1063–1070. doi: 10.1093/cercor/12.10.1063. [DOI] [PubMed] [Google Scholar]
- 301.Maldonado-Avilés JG, Curley AA, Hashimoto T, et al. Altered markers of tonic inhibition in the dorsolateral prefrontal cortex of subjects with schizophrenia. American Journal of Psychiatry. 2009;166(4):450–459. doi: 10.1176/appi.ajp.2008.08101484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Cobb SR, Buhl EH, Halasy K, Paulsen O, Somogyi P. Synchronization of neuronal activity in hippocampus by individual GABAergic interneurons. Nature. 1995;378(6552):75–78. doi: 10.1038/378075a0. [DOI] [PubMed] [Google Scholar]
- 303.Smalley SL, Tanguay PE, Smith M, Gutierrez G. Autism and tuberous sclerosis. Journal of Autism and Developmental Disorders. 1992;22(3):339–355. doi: 10.1007/BF01048239. [DOI] [PubMed] [Google Scholar]
- 304.Smalley SL. Autism and tuberous sclerosis. Journal of Autism and Developmental Disorders. 1998;28(5):407–414. doi: 10.1023/a:1026052421693. [DOI] [PubMed] [Google Scholar]
- 305.Sebat J, Lakshmi B, Malhotra D, et al. Strong association of de novo copy number mutations with autism. Science. 2007;316(5823):445–449. doi: 10.1126/science.1138659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Kumar RA, Karamohamed S, Sudi J, et al. Recurrent 16p11.2 microdeletions in autism. Human Molecular Genetics. 2008;17(4):628–638. doi: 10.1093/hmg/ddm376. [DOI] [PubMed] [Google Scholar]
- 307.Marshall CR, Noor A, Vincent JB, et al. Structural variation of chromosomes in autism spectrum disorder. American Journal of Human Genetics. 2008;82(2):477–488. doi: 10.1016/j.ajhg.2007.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Weiss LA, Shen Y, Korn JM, et al. Association between microdeletion and microduplication at 16p11.2 and autism. The New England Journal of Medicine. 2008;358(7):667–675. doi: 10.1056/NEJMoa075974. [DOI] [PubMed] [Google Scholar]
- 309.State MW. The genetics of child psychiatric disorders: focus on autism and tourette syndrome. Neuron. 2010;68(2):254–269. doi: 10.1016/j.neuron.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Lim S, Naisbitt S, Yoon J, et al. Characterization of the Shank family of synaptic proteins: multiple genes, alternative splicing, and differential expression in brain and development. Journal of Biological Chemistry. 1999;274(41):29510–29518. doi: 10.1074/jbc.274.41.29510. [DOI] [PubMed] [Google Scholar]
- 311.Chubykin AA, Liu X, Comoletti D, Tsigelny I, Taylor P, Südhof TC. Dissection of synapse induction by neuroligins: effect of a neuroligin mutation associated with autism. Journal of Biological Chemistry. 2005;280(23):22365–22374. doi: 10.1074/jbc.M410723200. [DOI] [PubMed] [Google Scholar]
- 312.Dölen G, Carpenter RL, Ocain TD, Bear MF. Mechanism-based approaches to treating fragile X. Pharmacology and Therapeutics. 2010;127(1):78–93. doi: 10.1016/j.pharmthera.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 313.Brooks-Kayal A. Epilepsy and autism spectrum disorders: are there common developmental mechanisms? Brain and Development. 2010;32(9):731–738. doi: 10.1016/j.braindev.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 314.Yasuhara A. Correlation between EEG abnormalities and symptoms of autism spectrum disorder (ASD) Brain and Development. 2010;32(10):791–798. doi: 10.1016/j.braindev.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 315.de Lanerolle NC, Kim JH, Robbins RJ, Spencer DD. Hippocampal interneuron loss and plasticity in human temporal lobe epilepsy. Brain Research. 1989;495(2):387–395. doi: 10.1016/0006-8993(89)90234-5. [DOI] [PubMed] [Google Scholar]
- 316.Marco P, Sola RG, Pulido P, et al. Inhibitory neurons in the human epileptogenic temporal neocortex: an immunocytochemical study. Brain. 1996;119(4):1327–1347. doi: 10.1093/brain/119.4.1327. [DOI] [PubMed] [Google Scholar]
- 317.Wittner L, Magloczky Z, Borhegyi Z, et al. Preservation of perisomatic inhibitory input of granule cells in the epileptic human dentate gyrus. Neuroscience. 2001;108(4):587–600. doi: 10.1016/s0306-4522(01)00446-8. [DOI] [PubMed] [Google Scholar]
- 318.Jansen LA, Peugh LD, Ojemann JG. GABAA receptor properties in catastrophic infantile epilepsy. Epilepsy Research. 2008;81(2-3):188–197. doi: 10.1016/j.eplepsyres.2008.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Cohen I, Navarro V, Clemenceau S, Baulac M, Miles R. On the origin of interictal activity in human temporal lobe epilepsy in vitro. Science. 2002;298(5597):1418–1421. doi: 10.1126/science.1076510. [DOI] [PubMed] [Google Scholar]
- 320.Khalilov I, Holmes GL, Ben-Ari Y. In vitro formation of a secondary epileptogenic mirror focus by interhippocampal propagation of seizures. Nature Neuroscience. 2003;6(10):1079–1085. doi: 10.1038/nn1125. [DOI] [PubMed] [Google Scholar]
- 321.Sloviter RS. Decreased hippocampal inhibition and a selective loss of interneurons in experimental epilepsy. Science. 1987;235(4784):73–76. doi: 10.1126/science.2879352. [DOI] [PubMed] [Google Scholar]
- 322.Sloviter RS. Permanently altered hippocampal structure, excitability, and inhibition after experimental status epilepticus in the rat: the “dormant basket cell” hypothesis and its possible relevance to temporal lobe epilepsy. Hippocampus. 1991;1(1):41–66. doi: 10.1002/hipo.450010106. [DOI] [PubMed] [Google Scholar]
- 323.Lowenstein DH, Thomas MJ, Smith DH, McIntosh TK. Selective vulnerability of dentate hilar neurons following traumatic brain injury: a potential mechanistic link between head trauma and disorders of the hippocampus. The Journal of Neuroscience. 1992;12(12):4846–4853. doi: 10.1523/JNEUROSCI.12-12-04846.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Buckmaster PS, Jongen-Rêlo AL. Highly specific neuron loss preserves lateral inhibitory circuits in the dentate gyrus of kainate-induced epileptic rats. The Journal of Neuroscience. 1999;19(21):9519–9529. doi: 10.1523/JNEUROSCI.19-21-09519.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Dinocourt C, Petanjek Z, Freund TF, Ben-Ari Y, Esclapez M. Loss of interneurons innervating pyramidal cell dendrites and axon initial segments in the CA1 region of the hippocampus following pilocarpine-induced seizures. Journal of Comparative Neurology. 2003;459(4):407–425. doi: 10.1002/cne.10622. [DOI] [PubMed] [Google Scholar]
- 326.de Lanerolle NC, Kim JH, Williamson A, et al. A retrospective analysis of hippocampal pathology in human temporal lobe epilepsy: evidence for distinctive patient subcategories. Epilepsia. 2003;44(5):677–687. doi: 10.1046/j.1528-1157.2003.32701.x. [DOI] [PubMed] [Google Scholar]
- 327.Andrioli A, Alonso-Nanclares L, Arellano JI, DeFelipe J. Quantitative analysis of parvalbumin-immunoreactive cells in the human epileptic hippocampus. Neuroscience. 2007;149(1):131–143. doi: 10.1016/j.neuroscience.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 328.DeFelipe J. Chandelier cells and epilepsy. Brain. 1999;122(10):1807–1822. doi: 10.1093/brain/122.10.1807. [DOI] [PubMed] [Google Scholar]
- 329.Arellano JI, Muñoz A, Ballesteros-Yáñez I, Sola RG, DeFelipe J. Histopathology and reorganization of chandelier cells in the human epileptic sclerotic hippocampus. Brain. 2004;127(1):45–64. doi: 10.1093/brain/awh004. [DOI] [PubMed] [Google Scholar]
- 330.Sayin U, Osting S, Hagen J, Rutecki P, Sutula T. Spontaneous seizures and loss of axo-axonic and axo-somatic inhibition induced by repeated brief seizures in kindled rats. The Journal of Neuroscience. 2003;23(7):2759–2768. doi: 10.1523/JNEUROSCI.23-07-02759.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.van Vliet EA, Aronica E, Tolner EA, Lopes da Silva FH, Gorter JA. Progression of temporal lobe epilepsy in the rat is associated with immunocytochemical changes in inhibitory interneurons in specific regions of the hippocampal formation. Experimental Neurology. 2004;187(2):367–379. doi: 10.1016/j.expneurol.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 332.Palm L, Blennow G, Brun A. Infantile spasms and neuronal heterotopias: a report on six cases. Acta Paediatrica Scandinavica. 1986;75(5):855–859. doi: 10.1111/j.1651-2227.1986.tb10302.x. [DOI] [PubMed] [Google Scholar]
- 333.Jellinger K. Neuropathological aspects of infantile spasms. Brain and Development. 1987;9(4):349–357. doi: 10.1016/s0387-7604(87)80106-7. [DOI] [PubMed] [Google Scholar]
- 334.Vinters HV, de Rosa MJ, Farrell MA, Genton P, Portera-Sanchez A, Benninger CK. Neuropathologic study of resected cerebral tissue from patients with infantile spasms. Epilepsia. 1993;34(4):772–779. doi: 10.1111/j.1528-1157.1993.tb00460.x. [DOI] [PubMed] [Google Scholar]
- 335.Hayashi M. Neuropathology of the limbic system and brainstem in West syndrome. Brain and Development. 2001;23(7):516–522. doi: 10.1016/s0387-7604(01)00310-2. [DOI] [PubMed] [Google Scholar]
- 336.Riikonen R. Long-term outcome of patients with West syndrome. Brain and Development. 2001;23(7):683–687. doi: 10.1016/s0387-7604(01)00307-2. [DOI] [PubMed] [Google Scholar]
- 337.Jansen LA, Peugh LD, Roden WH, Ojemann JG. Impaired maturation of cortical GABAA receptor expression in pediatric epilepsy. Epilepsia. 2010;51(8):1456–1467. doi: 10.1111/j.1528-1167.2009.02491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Claes L, Ceulemans B, Audenaert D, et al. De novo SCN1A mutations are a major cause of severe myoclonic epilepsy of infancy. Human Mutation. 2003;21(6):615–621. doi: 10.1002/humu.10217. [DOI] [PubMed] [Google Scholar]
- 339.Kanai K, Hirose S, Oguni H, et al. Effect of localization of missense mutations in SCN1A on epilepsy phenotype severity. Neurology. 2004;63(2):329–334. doi: 10.1212/01.wnl.0000129829.31179.5b. [DOI] [PubMed] [Google Scholar]
- 340.Kanai K, Yoshida S, Hirose S, et al. Physicochemical property changes of amino acid residues that accompany missense mutations in SCN1A affect epilepsy phenotype severity. Journal of Medical Genetics. 2009;46(10):671–679. doi: 10.1136/jmg.2008.060897. [DOI] [PubMed] [Google Scholar]
- 341.Ogiwara I, Miyamoto H, Morita N, et al. NaV1.1 localizes to axons of parvalbumin-positive inhibitory interneurons: a circuit basis for epileptic seizures in mice carrying an Scn1a gene mutation. The Journal of Neuroscience. 2007;27(22):5903–5914. doi: 10.1523/JNEUROSCI.5270-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Sherr EH. The ARX story (epilepsy, mental retardation, autism, and cerebral malformations): one gene leads to many phenotypes. Current Opinion in Pediatrics. 2003;15(6):567–571. doi: 10.1097/00008480-200312000-00004. [DOI] [PubMed] [Google Scholar]
- 343.Rusconi L, Salvatoni L, Giudici L, et al. CDKL5 expression is modulated during neuronal development and its subcellular distribution is tightly regulated by the C-terminal tail. Journal of Biological Chemistry. 2008;283(44):30101–30111. doi: 10.1074/jbc.M804613200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Dibbens LM, Feng HJ, Richards MC, et al. GABRD encoding a protein for extra- or peri- synaptic GABAA receptors is susceptibility locus for generalized epilepsies. Human Molecular Genetics. 2004;13(13):1315–1319. doi: 10.1093/hmg/ddh146. [DOI] [PubMed] [Google Scholar]
- 345.Chen Y, Lu J, Pan H, et al. Association between genetic variation of CACNA1H and childhood absence epilepsy. Annals of Neurology. 2003;54(2):239–243. doi: 10.1002/ana.10607. [DOI] [PubMed] [Google Scholar]
- 346.Burgess DL, Noebels JL. Single gene defects in mice: the role of voltage-dependent calcium channels in absence models. Epilepsy Research. 1999;36(2-3):111–122. doi: 10.1016/s0920-1211(99)00045-5. [DOI] [PubMed] [Google Scholar]
- 347.Talley EM, Solórzano G, Depaulis A, Perez-Reyes E, Bayliss DA. Low-voltage-activated calcium channel subunit expression in a genetic model of absence epilepsy in the rat. Molecular Brain Research. 2000;75(1):159–165. doi: 10.1016/s0169-328x(99)00307-1. [DOI] [PubMed] [Google Scholar]
- 348.Smits P, Li P, Mandel J, et al. The transcription factors L-Sox5 and Sox6 are essential for cartilage formation. Developmental Cell. 2001;1(2):277–290. doi: 10.1016/s1534-5807(01)00003-x. [DOI] [PubMed] [Google Scholar]
- 349.Smits P, Lefebvre V. Sox5 and Sox6 are required for notochord extracellular matrix sheath formation, notochord cell survival and development of the nucleus pulposus of intervertebral discs. Development. 2003;130(6):1135–1148. doi: 10.1242/dev.00331. [DOI] [PubMed] [Google Scholar]
- 350.Smits P, Dy P, Mitra S, Lefebvre V. Sox5 and Sox6 are needed to develop and maintain source, columnar, and hypertrophic chondrocytes in the cartilage growth plate. Journal of Cell Biology. 2004;164(5):747–758. doi: 10.1083/jcb.200312045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Baraban SC, Southwell DG, Estrada RC, et al. Reduction of seizures by transplantation of cortical GABAergic interneuron precursors into Kv1.1 mutant mice. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(36):15472–15477. doi: 10.1073/pnas.0900141106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Sebe JY, Baraban SC. The promise of an interneuron-based cell therapy for epilepsy. Developmental Neurobiology. 2011;71(1):107–117. doi: 10.1002/dneu.20813. [DOI] [PMC free article] [PubMed] [Google Scholar]


