Abstract
Background The excess risk of fatal and non-fatal cerebrovascular disease in people from low socioeconomic positions is only partially explained by conventional cerebrovascular risk factors. This has led to the suggestion that poor psychosocial work environments provide important additional explanatory power. However, little evidence is available for women.
Methods We examined whether job demands or job control contributed to the socioeconomic gradient in cerebrovascular disease among 48 361 women aged 18–65 years. Job demands, job control and behavioural risk factors were self-reported in 2000–2002; socioeconomic position (as indexed by occupational class) and all of the health measures were obtained from registers. The outcome was recorded hospitalization or death from cerebrovascular disease.
Results During a mean follow-up of 3.4 years, 124 women had a new cerebrovascular disease event. The risk was 2.3 (95% CI 1.3–3.9) times higher among women in low vs high socioeconomic positions. Adjustment for conventional risk factors, such as prevalent hypertension, coronary heart disease, diabetes, smoking, heavy alcohol consumption, physical inactivity and obesity, attenuated this excess risk by 23%. In contrast, adjustment for job demands and job control actually amplified the gradient by 36% suggesting a suppression effect.
Conclusions In this contemporary cohort of employed women, job demands—alone and in combination with job control—suppressed rather than explained socioeconomic differences in cerebrovascular disease.
Keywords: Socioeconomic status, psychosocial factors, risk factors, cerebrovascular disorders, cohort studies, stroke
Introduction
Socioeconomic gradients in cerebrovascular disease are evident among men and women,1–9 but their causes remain unclear.10 That the excess risk of cerebrovascular disease in people from low socioeconomic positions is only partially explained by conventional cerebrovascular risk factors—hypertension, smoking, physical inactivity and obesity—has led to the suggestion that poor psychosocial work environments provide important additional explanatory power.3,10–12 However, the only study to test this hypothesis among women found that high demands and low job control did not predict the onset of cerebrovascular disease over an 11-year follow-up and thus did not explain the association between socioeconomic position and cerebrovascular disease.12 This null finding does not necessarily refute the hypothesis: one would expect a dilution of effects when extended follow-up periods are used to assess effects of exposures that may change over time (the regression dilution bias). To examine more proximal effects on the cerebrovascular disease gradient among women, we assessed socioeconomic position, job demands and job control in a large cohort of female employees, and followed hospitalizations and deaths from cerebrovascular disease over a much shorter period of time, a mean of 3.4 years.
Methods
Study population
Data were taken from the ongoing Finnish Public Sector Study, which includes the entire personnel in government employment in 10 towns and 21 hospitals in Finland.13 A questionnaire on risk factors and health was sent to all of the 53 217 women (mean age 44.4 years, 26.6% with high socioeconomic position) in these organizations between 2000 and 2002; 38 391 (72%) responded. In 2004, a similar questionnaire was again sent to the female staff (70% responded) and we included in the present study those who did not respond to the first survey as well as those who were hired by the target organizations after the first survey—a further 14 254 women. Thus, the total number of respondents was 52 645. We excluded 4284 participants (8.1%) with missing data for one or more study variables (2248 lacked information on smoking, 1372 on body mass index, 1115 alcohol consumption, 1378 physical activity, 545 job demands, and 444 job control), leaving a total of 48 361 participants in the analytic sample. Their mean age was 43.5 years (range 18–65) and 27.2% were of high socioeconomic position; figures which closely resemble those for the original target population. Questionnaire data from this cohort were linked to records from national registers of drug reimbursement, hospitalization and mortality using the unique personal identification numbers assigned to all citizens in Finland. This linkage was successful to all participants. The Finnish Institute of Occupational Health Ethics Committee approved the study.
Socioeconomic position
Participants’ occupational titles from the employers’ records (a total of 1931 different five-digit occupational titles) were classified into high (upper non-manual including e.g. physicians, teachers); intermediate (lower non-manual, e.g. technicians, registered nurses); and low (manual, e.g. cleaners, maintenance workers) socioeconomic position (SEP) on the basis of Statistics Finland's existing occupational classification.14
Conventional risk factors
History of hypertension (International Classification of Diseases (ICD) ICD-9 codes 401–405; ICD-10 I10–I15), coronary heart disease (ICD-9 410–414, 427; ICD-10 I20–I25, I47–I49) and diabetes mellitus (ICD-9 250; ICD-10 E10–E14) at the time of questionnaire survey were ascertained from data on special reimbursement for treatment for these illnesses from the Social Insurance Institute Drug Reimbursement Register or from hospitalizations recorded in the National Hospital Discharge Register from January 1, 1990 onwards (criteria for hypertension: repeated blood pressure measurements >200 systolic or >105 diastolic, or >140 systolic or >95 diastolic with signs of complications or cardiovascular morbidity; Insulin-dependent diabetes: diagnosed by a specialist; Type 2 diabetes: disease specific symptoms and repeated blood (plasma) glucose levels >7.0 mmol/l; Coronary heart disease: presence of definite chronic angina, myocardial infarction or coronary artery bypass).
Using standard questionnaires, we requested current smoking status and regular weekly intake of beer, wine and spirits expressed in grams of alcohol. Physical activity was expressed as Metabolic Equivalent Task (MET)-hours per day. Body mass index (BMI, kg/m2) was computed from self-reported weight and height.
Job demands and job control
We used established questionnaire to assess job demands (three items, Cronbach's alpha = 0.75) and job control (nine items, Cronbach's alpha = 0.82).15 Scores from a five-point rating scale were summed and expressed as a percentage of the theoretical maximum (100 refers to the highest score for every item; 0 refers to the lowest score for every item). Neither natural nor clinical-based thresholds has been defined, so each scale was divided into low, middle and high exposure based on the tertile distribution in the total study population. Four quadrants of job strain were constructed by first division at the median and then cross-tabulation. This resulted in: low demands-high control (labelled ‘low strain’), low demands-low control (‘passive job’), high demands-high control (‘active job’), high demands-low control (‘high strain’).12
Cerebrovascular disease follow-up
Linkage to the National Hospital Discharge Register and the Statistics Finland Mortality Register provided a virtually complete follow-up for hospitalizations and death from cerebrovascular disease (ICD-9 430–438 and ICD-10 I6). Events that occurred after January 1, 1990 but before questionnaire completion determined history of cerebrovascular disease (112 cases). Each participant was followed until a cerebrovascular event, death or the end of the study, December 31, 2005, whichever came first; mean follow-up 3.4 years.
Statistical analysis
Associations of SEP, conventional risk factors, tertiles of job demands and job control, and quadrants of job strain with subsequent cerebrovascular events were examined using Cox proportional hazard models adjusted for age and cerebrovascular disease history, and, additionally, for other risk factors. P-value for linear trends between job demands, job control and cerebrovascular disease risk were obtained from models where these exposures were fitted as continuous variables. Change in the socioeconomic gradient after adjustments for conventional risk factors and psychosocial work characteristics was calculated with the formula:16
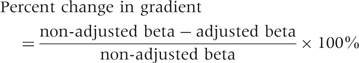 |
All the tests were two-tailed and the analyses were conducted using the SAS 9.1 program.
Results
Low SEP was associated with older age and less favourable levels for all risk factors with the exception of job demands, which were higher among high-SEP women (Table 1). During a mean follow-up of 3.4 years, 124 women had a cerebrovascular disease event (44 cerebral infarctions, 22 intracerebral haemorrhages, 33 subarachnoid haemorrhages, 25 non-specified or other cerebrovascular diseases). The rate of cerebrovascular disease events was 7.4 per 10 000 women per year.
Table 1.
Associations between socioeconomic position, conventional cerebrovascular risk factors and psychosocial work characteristics (n = 48 361)
| Socioeconomic position |
||||
|---|---|---|---|---|
| Baseline | High | Intermediate | Low | P-value |
| Numbers (%) | 13 158 (27.2) | 28 482 (58.9) | 6721 (13.9) | N/A |
| Age, year (mean) | 43.7 | 42.8 | 46.0 | <0.0001 |
| History of cerebrovascular disease (%)a | 0.16 | 0.21 | 0.27 | 0.34 |
| Conventional risk factorsa,b | ||||
| Diagnosed chronic hypertension (%) | 4.4 | 6.4 | 7.7 | <0.0001 |
| Diagnosed coronary heart disease (%) | 0.2 | 0.5 | 0.8 | <0.0001 |
| Diagnosed diabetes (%) | 0.7 | 1.0 | 1.3 | 0.0001 |
| Current smoking (%) | 10.1 | 17.1 | 29.2 | <0.0001 |
| Body mass index (kg/m2) | 24.0 | 24.9 | 25.7 | <0.0001 |
| Alcohol consumption (g/week) | 57.3 | 46.4 | 46.0 | <0.0001 |
| Physical activity, MET-hours per day | 4.5 | 4.7 | 4.4 | <0.0001 |
| Psychosocial work factors | ||||
| High job demandsc (%) | 31.9 | 26.8 | 26.1 | <0.0001 |
| Low job controlc (%) | 8.9 | 35.8 | 61.9 | <0.0001 |
| Low-strain jobd (%) | 33.1 | 21.6 | 10.4 | |
| Passive jobd (%) | 8.6 | 28.2 | 38.6 | |
| Active jobd (%) | 45.1 | 21.9 | 8.5 | |
| High-strain jobd (%) | 13.2 | 29.0 | 42.5 | <0.0001 |
aAge adjusted values. 112 women had a history of cerebrovascular disease.
bPrevalent diseases are obtained from hospitalisation records or reimbursement records.
c‘High’ refers to the proportion of those in the top tertile and ‘Low’ refers to the proportion of those belonging to the bottom tertile in the total population.
dThe four quadrants of job strain are low demands-high control (low strain), low demands-low control (passive job), high demands-high control (active job), high demands-low control (high strain).
Association of conventional and psychosocial risk factors with cerebrovascular disease
As expected, most of the conventional risk factors predicted subsequent cerebrovascular disease events (Table 2). High job demands were also associated with an increased risk of cerebrovascular disease events (hazard ratio 1.94, 95% CI 1.2–3.1, P for linear trend 0.004), but job control was not related to these events (P = 0.90). There was no multiplicative interaction between job demands and job control on cerebrovascular disease events (P for ‘demand * control’ interaction term = 0.48 in a model including the main effects). High demands combined with high control (i.e. active job) were associated with an increased risk of cerebrovascular disease events (hazard ratio 2.32, 95% CI 1.3–4.1 compared with low strain). The population attributable fraction for high job demands was large (14.9%).
Table 2.
Associations of conventional cerebrovascular risk factors, job demands and job control with subsequent cerebrovascular disease, adjusted for age and history of cerebrovascular disease
| Risk factor | No. of women (No. of events) | Hazard ratio (95% CI) |
|---|---|---|
| Diagnosed hypertension | ||
| No | 45 445 (98) | 1.00 |
| Yes | 2916 (26) | 2.44 (1.5–3.9) |
| Diagnosed coronary heart disease | ||
| No | 48 138 (120) | 1.00 |
| Yes | 223 (4) | 2.41 (0.8–6.8) |
| Diagnosed diabetes | ||
| No | 47 907 (124) | N/A |
| Yes | 454 (0) | |
| Current smoking | ||
| No | 40 186 (90) | 1.00 |
| Yes | 8175 (34) | 2.05 (1.4–3.1) |
| Alcohol consumption (g/week) | ||
| 0 (non-drinker) | 7362 (18) | 0.91 (0.5–1.5) |
| 1–210 (moderate) | 38 490 (97) | 1.00 |
| >210 (heavy) | 2509 (9) | 1.24 (0.6–2.5) |
| Physical activity, MET-hours per day | ||
| ≥2.0 (non-sedentary) | 36 880 (91) | 1.00 |
| <2.0 (sedentary) | 11 481 (33) | 1.08 (0.7–1.6) |
| Body mass index (kg/m2) | ||
| <18.5 (underweight) | 749 (1) | 0.87 (0.1–6.2) |
| 18.5–24.9 (normal) | 28 534 (61) | 1.00 |
| 25.0–29.9 (overweight) | 13 640 (36) | 1.04 (0.7–1.6) |
| ≥30 (obese) | 5438 (26) | 1.87 (1.2–3.0) |
| Job demands (tertiles)a | ||
| 1 (lowest) | 16 801 (29) | 1.00 |
| 2 | 17 975 (47) | 1.40 (0.9–2.2) |
| 3 (highest) | 13 585 (48) | 1.94 (1.2–3.1) |
| Job control (tertiles) | ||
| 3 (highest) | 15 512 (41) | 1.00 |
| 2 | 16 025 (44) | 1.21 (0.8–1.9) |
| 1 (lowest) | 16 824 (39) | 1.03 (0.7–1.6) |
| Job strain quadrants | ||
| Low strain | 11 209 (16) | 1.00 |
| Passive | 11 743 (29) | 1.57 (0.9–2.9) |
| Activea | 12 542 (45) | 2.32 (1.3–4.1) |
| High strain | 12 867 (34) | 1.62 (0.9–2.9) |
aAmong those with no history of cerebrovascular disease, the hazard ratio of future disease was 1.89 (95% CI: 1.1–3.1) for high vs low job demands and 2.22 (95% CI: 1.2–4.0) for active vs low-strain job.
Test of psychosocial explanations hypothesis
The risk of a future cerebrovascular event was 2.28 times higher among low SEP women than high SEP women (Table 3, upper panel). Adjustment for the conventional risk factors attenuated this excess risk by 23.1%. In contrast, this association was amplified by 27.7% after adjustment for job demands and job control, suggesting a suppression effect. This suppression effect was 35.7% when the adjustment made was for job strain quadrants instead of job demands and job control.
Table 3.
Contribution of conventional cerebrovascular disease risk factors, job demands and job control to the association between socioeconomic position and cerebrovascular disease
| Hazard ratio (95% CI), adjustment in addition to age and history of cerebrovascular disease |
||||
|---|---|---|---|---|
| Socioeconomic position | No. of participants (No. of events) | None | Conventional risk factorsa | Psychosocial work characteristicsb |
| Total cohort | ||||
| High | 13 430 (25) | 1.00 | 1.00 | 1.00 |
| Intermediate | 28 210 (67) | 1.38 (0.8–2.2) | 1.28 (0.8–2.1) | 1.60 (1.0–2.6) |
| Low | 6721 (32) | 2.28 (1.3–3.9) | 1.88 (1.1–3.2) | 2.86 (1.6–5.1) |
| Change in gradientc (%) | 0 | −23.1 | +27.7 | |
| Subpopulation with no history of cerebrovascular disease | ||||
| High | 13 409 (24) | 1.00 | 1.00 | 1.00 |
| Intermediate | 28 150 (62) | 1.36 (0.8–2.2) | 1.19 (0.74–1.92) | 1.54 (0.9–2.6) |
| Low | 6703 (27) | 2.01 (1.1–3.5) | 1.59 (0.90–2.80) | 2.38 (1.3– 4.4) |
| Change in gradientc (%) | 0 | −30.0 | +24.3 | |
aHypertension, coronary heart disease, diabetes, smoking, alcohol consumption, physical activity, and body mass index.
bJob demands and job control.
cCompared to low vs high socioeconomic position category in the age- and cerebrovascular-disease-history-adjusted model. Corresponding changes in the gradient after adjustment for job strain quadrants 35.7% for the total cohort and 28.6% for the subpopulation.
Repeating all the analyses in a cohort with no prior history of cerebrovascular disease at baseline (n = 48 262, 113 incident cerebrovascular events) largely replicated these findings: 30.0% attenuation in the SEP–cerebrovascular disease association after adjustment for conventional risk factors; amplification of 24.3 and 28.6%, respectively, after adjustment for job demands and job control and for quadrants of job strain (Table 3, lower panel).
The findings were also replicated in analyses using self-reported education (instead of occupational status) as the indicator of SEP. The age and cerebrovascular disease history adjusted hazard ratio for cerebrovascular disease for primary vs secondary (A level) education was 1.77 (95% CI 1.2–2.6). Adjustment for conventional risk factors reduced this effect by 25.7%. In contrast, the association was amplified by 16.2% after adjustments for job demands and job control and by 24.9% after adjustment for job strain quadrants.
Discussion
We found a marked socioeconomic gradient in cerebrovascular disease that was partially explained by a higher prevalence of conventional risk factors among women of low socioeconomic position. In this cohort, psychosocial work characteristics did not explain socioeconomic differences in cerebrovascular disease; controlling for job demands and job strain quadrants increased (rather than decreased) the gradient. While this result was counter to our expectations, the associations observed between the established risk factors, hypertension, smoking and obesity and cerebrovascular disease point to a degree of validity in our new findings.
It is assumed that the greater the attenuation of the gradient after adjustment for a given risk factor the greater the potential to reduce socioeconomic inequalities via interventions that target this factor.17 Our cerebrovascular risk factor measures were based on two data sources: (i) records from national health registers which have high coverage and specificity but do not include undiagnosed conditions and (ii) validated self-reported measures that may still be affected by reporting bias.18 In spite of possible misclassification of the risk factors, the 20–30% reduction in the cerebrovascular disease gradient following adjustment for conventional risk factors accords with the results from other studies suggesting that important reductions in inequalities will follow reductions in levels of hypertension, coronary heart disease, smoking, physical inactivity and obesity in low socioeconomic groups.10,19
Psychosocial factors have been found to be associated with both socioeconomic position and conventional risk factors,20–24 but evidence on the association between psychosocial factors and risk of cerebrovascular disease is mixed.12,25 It is not known whether the association between job demands and cerebrovascular disease observed in the present study was causal. Reverse causation remains an alternative explanation for our findings, because timing of the onset of cerebrovascular disease symptoms may vary, depending on the type of cerebrovascular disease.26 For example, symptoms of atherosclerosis, such as shortness of breath and chest pain may increase susceptibility to high demands and could occur long before manifest ischemic stroke.27 Confounding by socioeconomic position is a further possibility, but is an unlikely explanation for our findings as higher job demands were not associated with lower socioeconomic position in this cohort.
We found no support for the hypothesis that psychosocial characteristics, as indicated by job demands and job control, would explain socioeconomic differences in cerebrovascular disease among women. High job demands were more common among women of high than low socioeconomic positions. Thus, the socioeconomic gradient in cerebrovascular disease was amplified by adjustment for job demands. We used occupational group and educational level to measure socioeconomic position and the main findings were consistent across these two indicators of socioeconomic position.
If we assume that high job demands were a causal risk factor for cerebrovascular disease, what would the observed amplification of the gradient imply in terms of policy? The common ‘prescription’ to reduce socioeconomic inequalities in disease is to reduce differential exposure to risk factors between high and low socioeconomic groups. If prevention only reduced high demands, this would potentiate the gradient although it would reduce the absolute risk of cerebrovascular disease in the total population. Any strategy to reduce the gradient, i.e. the relative risk, would also need to target those risk factors more prevalent among low socioeconomic groups. 17,28
Further research is needed to examine whether the association between job demands and cerebrovascular disease is causal and whether the psychosocial explanations hypothesis will be refuted or confirmed in other populations and specific categories of cerebrovascular disease, such as subarachnoid haemorrhage, intracerebral haemorrhage and ischemic stroke.
Funding
Academy of Finland (projects 117604, 124322, 124271, and 129262) and participating organizations.
KEY MESSAGES.
Causes of the excess risk of cerebrovascular disease in women from low socioeconomic positions are not known.
In a cohort of over 48 000 Finnish women, there was a marked socioeconomic gradient in cerebrovascular disease.
This gradient was partially explained by a higher prevalence of hypertension, smoking and obesity among women of low socioeconomic position.
Job demands and job control did not explain the socioeconomic gradient although high job demands were associated with an increased risk of cerebrovascular disease events.
References
- 1.Steenland K, Hu S, Walker J. All-cause and cause-specific mortality by socioeconomic status among employed persons in 27 US states, 1984–1997. Am J Public Health. 2004;94:1037–42. doi: 10.2105/ajph.94.6.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huisman M, Kunst AE, Bopp M, et al. Educational inequalities in cause-specific mortality in middle-aged and older men and women in eight western European populations. Lancet. 2005;365:493–500. doi: 10.1016/S0140-6736(05)17867-2. [DOI] [PubMed] [Google Scholar]
- 3.Hart CL, Hole DJ, Smith GD. The contribution of risk factors to stroke differentials, by socioeconomic position in adulthood: the Renfrew/Paisley Study. Am J Public Health. 2000;90:1788–91. doi: 10.2105/ajph.90.11.1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jakovljevic D, Sarti C, Sivenius J, et al. Socioeconomic status and ischemic stroke: The FINMONICA Stroke Register. Stroke. 2001;32:1492–98. doi: 10.1161/01.str.32.7.1492. [DOI] [PubMed] [Google Scholar]
- 5.Peltonen M, Rosen M, Lundberg V, Asplund K. Social patterning of myocardial infarction and stroke in Sweden: incidence and survival. Am J Epidemiol. 2000;151:283–92. doi: 10.1093/oxfordjournals.aje.a010204. [DOI] [PubMed] [Google Scholar]
- 6.van Rossum CT, van de Mheen H, Breteler MM, Grobbee DE, Mackenbach JP. Socioeconomic differences in stroke among Dutch elderly women: the Rotterdam Study. Stroke. 1999;30:357–62. doi: 10.1161/01.str.30.2.357. [DOI] [PubMed] [Google Scholar]
- 7.Avendano M, Kunst AE, Huisman M, et al. Educational level and stroke mortality: a comparison of 10 European populations during the 1990s. Stroke. 2004;35:432–37. doi: 10.1161/01.STR.0000109225.11509.EE. [DOI] [PubMed] [Google Scholar]
- 8.Kim C, Eby E, Piette JD. Is education associated with mortality for breast cancer and cardiovascular disease among black and white women? Gend Med. 2005;2:13–18. doi: 10.1016/s1550-8579(05)80005-1. [DOI] [PubMed] [Google Scholar]
- 9.Singh GK, Siahpush M. Increasing inequalities in all-cause and cardiovascular mortality among US adults aged 25–64 years by area socioeconomic status, 1969–1998. Int J Epidemiol. 2002;31:600–13. doi: 10.1093/ije/31.3.600. [DOI] [PubMed] [Google Scholar]
- 10.Cox AM, McKevitt C, Rudd AG, Wolfe CD. Socioeconomic status and stroke. Lancet Neurol. 2006;5:181–88. doi: 10.1016/S1474-4422(06)70351-9. [DOI] [PubMed] [Google Scholar]
- 11.Tolonen H, Mahonen M, Asplund K, et al. Do trends in population levels of blood pressure and other cardiovascular risk factors explain trends in stroke event rates? Comparisons of 15 populations in 9 countries within the WHO MONICA Stroke Project. World health organization monitoring of trends and determinants in cardiovascular disease. Stroke. 2002;33:2367–75. doi: 10.1161/01.str.0000033131.27936.7f. [DOI] [PubMed] [Google Scholar]
- 12.Kuper H, Adami HO, Theorell T, Weiderpass E. The socioeconomic gradient in the incidence of stroke: a prospective study in middle-aged women in Sweden. Stroke. 2007;38:27–33. doi: 10.1161/01.STR.0000251805.47370.91. [DOI] [PubMed] [Google Scholar]
- 13.Kivimaki M, Lawlor DA, Davey Smith G, et al. Socioeconomic position, co-occurrence of behavior-related risk factors, and coronary heart disease: the Finnish Public Sector study. American Journal of Public Health. 2007;97:874–79. doi: 10.2105/AJPH.2005.078691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Statistics Finland. Classification of Occupations. Helsinki: Statistics Finland; 1987. [Google Scholar]
- 15.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The job content questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322–55. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 16.Hamer M. Mediation of the association between mortality risk and socioeconomic status. JAMA. 2006;296:763. doi: 10.1001/jama.296.7.763-a. [DOI] [PubMed] [Google Scholar]
- 17.Kivimaki M, Shipley MJ, Ferrie JE, et al. Best-practice interventions to reduce socioeconomic inequalities of coronary heart disease mortality in UK: a prospective occupational cohort study. Lancet. 2008;372:1648–54. doi: 10.1016/S0140-6736(08)61688-8. [DOI] [PubMed] [Google Scholar]
- 18.Macleod J, Davey Smith G, Heslop P, Metcalfe C, Carroll D, Hart C. Psychological stress and cardiovascular disease: empirical demonstration of bias in a prospective observational study of Scottish men. Br Med J. 2002;324:1247–51. doi: 10.1136/bmj.324.7348.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Donnan GA, Fisher M, Macleod M, Davis SM. Stroke. Lancet. 2008;371:1612–23. doi: 10.1016/S0140-6736(08)60694-7. [DOI] [PubMed] [Google Scholar]
- 20.Marmot MG, Davey Smith G, Stansfeld S, et al. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991;337:1387–93. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- 21.Hallqvist J, Diderichsen F, Theorell T, Reuterwall C, Ahlbom A. Is the effect of job strain on myocardial infarction risk due to interaction between high psychological demands and low decision latitude? Results from Stockholm Heart Epidemiology Program (SHEEP) Soc Sci Med. 1998;46:1405–15. doi: 10.1016/s0277-9536(97)10084-3. [DOI] [PubMed] [Google Scholar]
- 22.Kouvonen A, Kivimäki M, Virtanen M, Pentti J, Vahtera J. Work stress, smoking status, and smoking intensity: an observational study of 46,190 employees. J Epidemiol Community Health. 2005;59:63–69. doi: 10.1136/jech.2004.019752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kouvonen A, Kivimäki M, Cox SJ, Cox T, Vahtera J. Relationship between work stress and body mass index among 45,810 female and male employees. Psychosom Med. 2005;67:577–83. doi: 10.1097/01.psy.0000170330.08704.62. [DOI] [PubMed] [Google Scholar]
- 24.Chandola T, Britton A, Brunner E, et al. Work stress and coronary heart disease: what are the mechanisms? Eur Heart J. 2008;29:640–48. doi: 10.1093/eurheartj/ehm584. [DOI] [PubMed] [Google Scholar]
- 25.Toivanen S, Hemstrom O. Is the impact of job control on stroke independent from socioeconomic status?: a large-scale study of the Swedish working population. Stroke. 2008;39:1321–23. doi: 10.1161/STROKEAHA.107.495523. [DOI] [PubMed] [Google Scholar]
- 26.Silver FL, Kapral MK, Lindsay MP, Tu JV, Richards JA. International experience in stroke registries: lessons learned in establishing the Registry of the Canadian Stroke Network. Am J Prev Med. 2006;31(6 Suppl. 2):S235–37. doi: 10.1016/j.amepre.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 27.Macleod J, Davey Smith G. Psychosocial factors and public health: a suitable case for treatment? J Epidemiol Community Health. 2003;57:565–70. doi: 10.1136/jech.57.8.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singh-Manoux A, Nabi H, Shipley M, et al. The role of conventional risk factors in explaining social inequalities in coronary heart disease: the relative and absolute approaches to risk. Epidemiology. 2008;19:599–605. doi: 10.1097/EDE.0b013e3181761cdc. [DOI] [PMC free article] [PubMed] [Google Scholar]


