Abstract
Context:
Since the home is the primary source of exposure of children to second-hand smoke (SHS), measures to restrict smoking at home should be introduced to protect children from its adverse health consequences.
Aims:
Objectives of the study were to assess the level of awareness of rural Indian women on the health impacts of SHS on children and to look into the strategies they used to reduce children's exposure to SHS at home.
Materials and Methods:
A community-based cross-sectional study was conducted among 438 rural women using a survey questionnaire. Information on socio-demographic characteristics, knowledge on specific health effects of SHS on children, and attitude toward having a smoke-free home were collected. The perceived reasons that made it difficult to have smoke-free homes were also explored.
Results:
A total of 75.8% of women agreed that SHS was a serious health risk for children. Knowledge on health impacts of SHS on children identified asthma as the most common problem. Smoking by husbands (89.7%) was the major source of exposure to SHS at home. While 67.6% of women reported having taken measures to limit SHS exposure in their homes, only 12.8% of them had tried to introduce a complete ban on smoking at home. On a five-point evaluation scale, 73.3% of the women indicated a failure of their initiatives to have smoke-free homes.
Conclusions:
Women's initiatives to introduce restrictions on smoking at home had very limited success and did not produce an appreciable change in smoking behavior at home. Lack of empowerment of women in rural India probably rendered the interventional measures ineffective.
Keywords: Health risk, second-hand smoke, smoke-free home
INTRODUCTION
Although there is conclusive scientific evidence on health risks associated with exposure to SHS, the health of a large proportion of children across the world is being adversely affected as a result of exposure to SHS at home. An estimated 700 million children worldwide are exposed to second-hand tobacco smoke at home.[1] The global average of children with at least one parent who smokes is estimated as 43%.[2] To protect the nonsmokers’ right for a smoke-free environment, Article 8 of the WHO Framework Convention on Tobacco Control (FCTC) mandates the implementation of appropriate smoke-free measures by all countries that have ratified the global health treaty. Being party to the WHO FCTC, India has enacted and enforced legislation that prohibits smoking in public and work places. But legislation to ban smoking inside homes is unlikely. In India, 21.9% of children aged 13-15 years are exposed to SHS in their own homes[3] where their options to avoid the health risks resulting from it are limited. Measures to restrict smoking at home need to be introduced in order to protect children from the adverse health consequences of SHS. Information on how prevalent these practices are among women or the factors that influence such practices in rural India is very limited. This study was conducted to elicit the level of awareness of rural Indian women of the effects of SHS on health of children and to look into the strategies they use to make their homes smoke free.
MATERIALS AND METHODS
A community-based cross-sectional study was carried out among rural women attending a primary healthcare clinic organized by a district level nongovernment organization (NGO) in Nadia district of West Bengal, India. The clinics held thrice a week on specified days addressed the health needs of women and children of three neighboring villages. Women aged from 25 to 40 years, nonsmokers, having at least one child less than 10 years of age and is exposed to tobacco smoke at home, were eligible to participate in the study. The participants were interviewed at the clinic site by a trained social worker in the period from December 2007 to May 2008. Only one woman per household was interviewed. A pretested, semi-structured questionnaire was used to collect information on socio-demographic characteristics, smokeless tobacco habits, knowledge on specific health impacts of SHS on children, and initiatives taken by the participants to make their homes smoke free. The women who reported that they had taken some initiatives to restrict smoking at home were further asked about realistic measures introduced to have a smoke-free indoor environment. A five-point evaluation scale was used to assess their level of agreement or disagreement (1: strongly agree, 2: agree, 3: neither agree nor disagree, 4: disagree, 5: strongly disagree) to the following statement “I have made my home smoke free.” The perceived reasons that made it difficult to have a smoke-free home environment were also explored.
Data were entered in Microsoft Excel database and analyzed using was Epi-Info version 6 StatCalc. The characteristics of the study participants by socio-demographic variables were described. Frequency tables for each independent variable were generated and expressed as percentage of the total number of women that responded in a particular group. The chi-square test (χ2) was applied to compare the significant differences of observed frequencies among the groups.
RESULTS
A total number of 438 women participated in the study. The mean age of the respondents was 31.2 years. Hindus comprised 81.5% of the study participants, 68.3% of whom were homemakers. The literacy status was low with only 19.9% of the participants possessing a secondary level of education. The majority (85.6%) belonged to the low socio-economic group with a monthly income of <3000 Indian Rupees (INR). A total of 11.8% had the habit of consuming chewable tobacco. Smoking by husbands (89.7%) was the major source of exposure to SHS at home. A total of 75.8% of women agreed that exposure to SHS was harmful to children. Knowledge of the impact of SHS on the health of children indicated that asthma was the most widespread problem followed by other types of respiratory illnesses like bronchitis. No response was available in the ‘cot death’ and ‘middle ear infection’ categories.
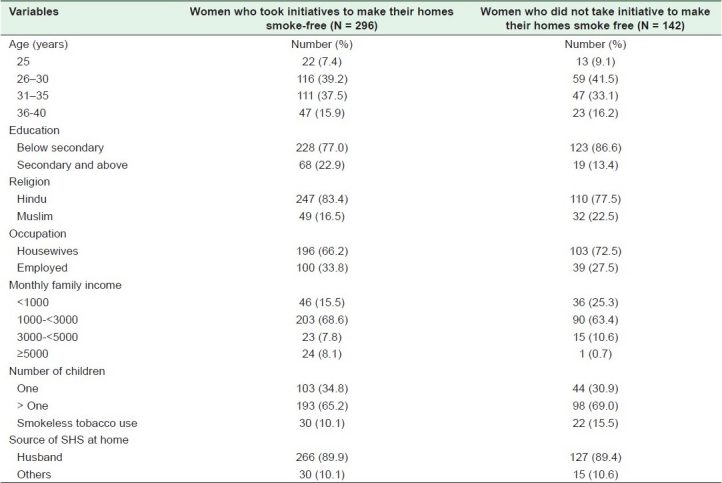
A total of 67.6% of the women reported having taken initiatives to restrict smoking at home. The characteristics of the respondents are given in Table 1. A significant difference was observed in educational levels (χ2 = 5.53; P = 0.018) and family income (χ2 = 5.99; P = 0.014) between the group who had tried to introduce restrictive measures on smoking at home and the group that had not (32.4%). Lower the education (illiterate and primary level) and family income (<3000 INR), less were the initiatives to introduce restrictions on smoking at home. Characteristics such as women's age, number of children, employment status, religion, habit of chewing tobacco, and number of rooms in each household did not differ significantly between the two groups.
Table 1.
Characteristics of the respondents (N = 438)
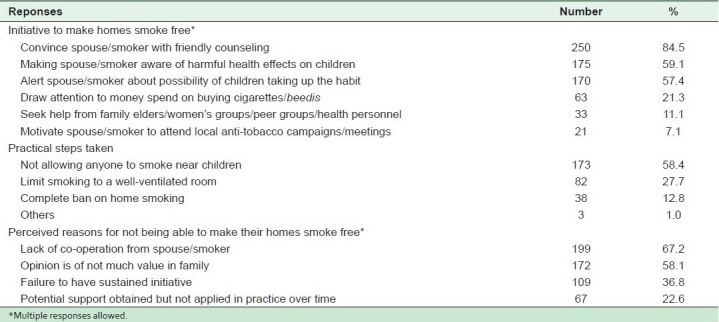
The women (N = 296) who took the initiative to introduce restrictions on smoking at home were asked what actions they had taken. The most frequent response was “convince spouse/smoker with friendly counseling.” The other commonly reported initiatives were that they made the spouse/smoker aware of the health effects of SHS on children and warned them of the possibility of children taking up the habit. When the women were asked to specify the practical steps taken to create a smoke-free indoor environment, 58.4% said that they did not allow anyone to smoke near children at home, and 27.7% responded that they limited smoking to a well-ventilated room. Only 38 (12.8%) women had tried to establish a complete ban on smoking at home. These women had a significantly higher level of education compared to the women who had tried to initiate other forms of restrictive measures on smoking at home (χ2 = 4.37; P = 0.036). Of the 292 available responses to the statement “I have made my home smoke free,” nearly half of them (49.3%, N = 144) strongly disagreed and 23.9% (N = 70) disagreed, indicating failure in their initiatives to have a smoke-free home. A total of 19.1% (N = 56) women neither agreed nor disagreed, as they were not able to decide on their level of achievement. Only 5.8% (N=17) women agreed and 1.7% (N = 5) strongly agreed to the statement that indicated achieving smoke-free homes. The most frequently reported reason for not being able to institute measures that limit SHS at home was the lack of co-operation from the spouse/smoker. Other important reasons stated were that women's opinion was not valued in the family, failure of a sustained initiative, and diminished practical support from spouse/smoker over time [Table 2].
Table 2.
Responses of surveyed women who took initiatives to make their homes smoke free (N = 296)
DISCUSSION
Since the home is the key source of exposure of children to SHS, restrictive policies on smoking at home are essential for the protection of children from its harmful health consequences. Many countries across the world have enforced comprehensive legislation prohibiting smoking in public places. The introduction of similar legislative measures inside homes is difficult because of diverse complex social and cultural issues. Adoption of voluntary restrictive behavior on smoking at home is the ideal way to protect children from exposure to SHS, but this may not always be feasible. Since women are the primary care givers and play a major role in promoting and protecting the health of children, it is important to look into their strategies of protecting children from the ill-effects of SHS in their own homes. There is little documentation on the implications of SHS initiatives and policies for subpopulations of women, such as those of lower socio-economic status, young women or those of particular ethno-cultural or marginalized groups.[4] To our knowledge, the present study is the first from India to explore the initiatives of rural Indian women to control exposure of SHS at home and the effectiveness of the adopted strategies in reducing exposure.
The low level of education of women and literacy on health matters is a key problem in rural India. Since women are responsible to a large extent for taking care of the health of family members, particularly children, it is essential to educate them on basic issues of healthcare. In our study area, the mentioned district NGO held regular promotion campaigns on health literacy among women as part of their awareness generation support services. The present study revealed that in spite of the low level of literacy of the participating women, the majority (75.8%) were aware of harmful effects of SHS on children, demonstrating the effectiveness of the campaign. Earlier studies have shown that heightened awareness of the harmful health effects of SHS was associated with bans on smoking in the house for both smokers and nonsmokers.[5,6] In our study, women's awareness of health risks of SHS did not necessarily translate into action for a smoking ban in their homes. A total of 67.6% mothers had tried to introduce some restrictive behavior on smoking at home, but only 12.8% of them had actually attempted to introduce a complete ban on home smoking. Deficiency in the depth of knowledge probably influenced the women to take action. Mothers were aware of only some of the health hazards caused by exposure to SHS on children like asthma and other respiratory illnesses. None were aware of other serious health consequences like sudden infant death syndrome (SIDS) and middle ear infections. The quality of knowledge about SHS effects is important, as attitude toward SHS depends on the depth of information available, as well as the emotional value of the information to the recipient, among other things.[7] Family income emerged to be a determinant of motivation for adopting restrictions on smoking behavior at home. The lower the family income (<3000 INR) the less were the initiatives to introduce restrictions on smoking at home. Similar results were found in one of the studies that indicated that families on low income were less likely to have smoke-free homes.[8]
Relationship issues within the family are important when considering implementation of smoke-free rules at home. Rural Indian women have little empowerment, and their role in the family is generally restricted to child care, looking after other family members and carrying out routine household chores. Even if they are able to comprehend the health risks of exposure to SHS, their capacity to implement smoke-free rules in the family may be limited. In the present study, women reported rather guarded efforts, with the majority saying that they had tried to convince their spouses/smoker with friendly counseling to restrict smoking in the presence of children. Household dynamics and elements of power and control in relationships need to be considered when designing sensitive tobacco reduction initiatives such as smoke-free homes.[9]
The educational level was an important factor in influencing action-taking behavior of women. Of the 67.6% of women who wanted to have smoke-free homes, only 12.8% of them had tried to enforce a “complete ban on home smoking.” These women had a significantly higher level of education compared to women who took partial restrictive measures on smoking at home. Action taking behavior is a complex matter and may be affected by knowledge about SHS, interest in the effects of SHS, ability to make plans for action, and ability to carry out the plans.[10] A majority of the women in our study belonged to the low socio-economic and low literacy group, and their efforts to have a smoke-free home were mostly limited to enforcing partial restrictions on smoking at home.
Considering the rural Indian scenario, initiatives taken by women to make their homes smoke-free were encouraging. However, evaluation of the level of achievement in actual practice showed a failure in the majority (73.3%) to enforce smoke-free rules. In the home, smoke-free policies may be ineffective or pose difficulties, because of economic and child care responsibilities, interpersonal dynamic and conflicts.[4] Our study explored the perceived barriers that precluded smoke-free home. It appeared that the lack of co-operation of the spouse/smoker was the major impediment to achieving the goal. Although some of them experienced temporary reduction in exposure to SHS at home, the lack of a sustained initiative to pursue the issue was an important reason for their failure. Many also felt that their opinion or suggestions on health issues were not valued in the family. Poor empowerment of rural India women coupled with low level of education was possibly responsible for such family interactions.
The major limitation of our study was the low sample size. The results may not be representative of the vast majority of rural population in India. Moreover, the study was a cross-sectional one that addressed the issue only once. Following up the same cohort could have revealed more important gender sensitive issues on enforcing smoke-free policies at home.
Although only a complete smoke-free home would provide the best protection to children, women's initiatives to introduce restrictive measures on smoking at home had limited success and did not lead to an appreciable change in behavior on smoking at home. Poor empowerment of women in rural India probably rendered the interventional measures ineffective. Since the home is the major source of exposure of SHS to children, women's initiatives toward a smoke-free home need to be evaluated, and targeted interventions with a focus on cultural attitudes designed. Comprehensive strategies along with appropriate educational campaigns and counseling aimed at modifying smoking behavior at home are suggested to protect children from harmful effects of SHS.
Acknowledgments
The authors gratefully acknowledge the co-operation of all the members and volunteers of the following Non Governmental Organizations -- Sreema Mahila Samity of district Nadia, West Bengal, and Saktipada Das Memorial Foundation of Kolkata, West Bengal.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
REFERENCES
- 1.Geneva: World Health Organization, Division of Non-communicable Disease, Tobacco Free Initiative; 1999. [Last accessed on 2011 Feb 15]. International Consultation on Environmental Tobacco smoke (ETS) and Child Health. Available from: http://www.who.int/tobacco/research/en/ets_report.pdf . [Google Scholar]
- 2.Warren CW, Jones NR, Peruga A, Chauvin J, Baptiste JP, Costa-de-Silva V, et al. Global Youth Tobacco Surveillance, 2000–2007. Morbidity and Mortality Weekly Report. Centers for Disease Control and Prevention. 2008;57(SS01):1–21. [PubMed] [Google Scholar]
- 3.Global Youth Tobacco Survey – India Factsheet. 2009. [Last accessed on 2011 Feb 15]. Available from: http://www.searo.who.int/LinkFiles/GYTS_India_Factsheet2009.pdf .
- 4.Lorraine JG, Natalie JH. Sex, gender, and second hand smoke policies, Implications for disadvantaged women. Am J Prev Med. 2009;37(2S):S131–7. doi: 10.1016/j.amepre.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 5.Kegler MC, Malcoe LH. Smoking restrictions in the home and car among rural Native American and White families with young children. Prev Med. 2002;35:334–42. doi: 10.1006/pmed.2002.1091. [DOI] [PubMed] [Google Scholar]
- 6.Pizacani BA, Martin DP, Stark MJ, Koepsell TD, Thompson B, Diehr P. Household smoking bans: Which households have them and do they work? Prev Med. 2003;36:99–107. doi: 10.1006/pmed.2002.1123. [DOI] [PubMed] [Google Scholar]
- 7.Blackburn C, Spencer N, Bonas S, Coe C, Dolan A, Moy R. Effect of strategies to reduce exposure of infants to environmental tobacco smoke in the home: Cross sectional survey. BMJ. 2003;327:257. doi: 10.1136/bmj.327.7409.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borland R, Yong HH, Cummings KM, Hyland A, Anderson S, Fong GT. Determinants and consequences of smoke-free homes: Findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(3S):iii42–50. doi: 10.1136/tc.2005.012492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greaves L, Kalaw C, Bottorff JL. Case studies of power and control related to tobacco use during pregnancy. Womens Health Issues. 2007;17:325–32. doi: 10.1016/j.whi.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Thomson G, Wilson N, Howden-Chapman P. Attitudes to, and knowledge of, second hand smoke in New Zealand homes and cars. N Z Med J. 2005;118:U1407. [PubMed] [Google Scholar]


