Abstract
Purpose/Objective:
To assess the correct position, attachment and effective suckling in the breastfeeding of infants as practiced by mothers attending hospitals at Benghazi.
Materials and Methods:
An observational, descriptive, cross-sectional study was done at AlJamahiriya and AlFateh Hospital in Benghazi, Libya, from November 2009 to February 2010. One hundred ninety-two mother-neonate units were observed for mother's and baby's position, attachment and effective suckling using WHO B-R-E-A-S-T- Feed observation form. Grading of positioning, attachment and suckling was done according to the score of various characteristics. Data thus collected were analyzed using software SPSS 11.5 version.
Results:
About 15% of the infants were about a week old (early neonatal period) and 85% were in the late neonatal period. There was poorer positioning among primipara (24.0%) than multipara (8.9–12.5%)mothers. Poorer attachment was also more evident among primipara (30.0%) compared to multipara (20.9%) mothers. Parity was significantly associated with poor position (P = 0.028) and attachment (P = 0.002). Poor attachment was related to cracked nipples and mastitis. Preterm and low birth weight were significantly associated with poor attachment and poor effective suckling. Poor suckling was more (42.8%) in the early neonatal period than late neonatal period (32.9%).
Conclusions and Recommendations:
Young (<20 years) and primipara mothers were more in need of support and guidance for appropriate breastfeeding techniques. It is recommended that each mother should be observed for mother's and infant's positioning and attachment at the onset of breastfeeding and if needed subsequent counseling should be given on correct positioning and attachment.
Keywords: Attachment (latch-on), breastfeeding practices, effective suckling, positioning
INTRODUCTION
Breastfeeding is one of the oldest practices, recommended in the ancient Hindu scriptures, Holy Quran and Biblical records.[1]
Breastfeeding confers short-term and long-term benefits on both child and mother, including helping to protect children against a variety of acute and chronic disorders. The review of studies from developing countries shows that infants who are not breastfed are 6–10 times more likely to die in the first few months of life than infants who are breastfed. Diarrhea and pneumonia are more common and more severe in children who are artificially fed, and are responsible for many of these deaths. Other acute infections, including otitis media, Haemophilus influenzae meningitis and urinary tract infection are less common and less severe in breastfed infants.[2]
Artificially fed children have an increased risk of longterm diseases with an immunological basis, including asthma and other atopic conditions, type 1 diabetes, celiac disease, ulcerative colitis and Crohn's disease.[2]
There has been an increasing concern in the recent years about the changing pattern of breastfeeding, particularly in societies in rapid transition. An earlier study in Benghazi in 1981 showed that only 54.8% of mothers breastfed for more than 6 months.[3] Regarding feeding practices, the rates of ever and exclusive breastfeeders till 4 months per 100 women were 83.2 and 49.1, respectively. The rate of breastfeeding for 6 or more months was 24.8 per 100 women.[4]
An interview survey of 200 mothers attending the emergency service of Al-Fateh Paediatric Hospital, Benghazi, showed that prelacteal feed was given to 18.5% of babies and breastfeeding was ever initiated in 90.5% (it also includes some cases from prelacteal fed babies who were breastfed). After 3 months, exclusive breastfeeding was continued in less than 30%, mixed feeding in 44–71% and supplementary feeding (with and without breastfeeding) in 65-97%.[1] At 3 months of age, 46.4% of the infants were exclusively breastfed, 27.0% were exclusively bottlefed, and 26.5% were fed by mixed methods.[5,6]
Effective breastfeeding is a function of the proper positioning of mother and baby and attachment of child to the mother's breast.[7] Studies conducted in North India reveal that there was “good attachment” in 42% mother-infant pairs and infants were held in “correct position” by 60% mothers.[8] A study in Bangladesh reported that correct breastfeeding position (74%) and good attachment (72.3%) as assessed by CHWs at late visits (67 days after delivery) were practiced by mothers.[9]
Positioning of the baby's body is important for good attachment and successful breastfeeding. Most difficulties can be avoided altogether if good attachment and positioning are achieved at the first and early feeds.[10] An effective sucking technique is considered important to establish breastfeeding, to ensure milk transfer, and to prevent breastfeeding problems.[7,11–16]
The baby's positioning and attachment to the breast during breastfeeding are fundamental toward the occurrence of different sorts of nipple trauma. A study conducted in Brazil showed that a greater proportion of primigests (first time pregnant) displayed nipple lesion (57.4%) followed by 54.9% of primipara (with one live birth) and 45.1% of multipara. Many studies indicate a statistically significant association between position and holding variables for causing nipple lesions, where newborns whose necks were bent, whose chins were held away from the breast and where lips were turned inward.[17] Improper suction is also described as a source of trauma which if corrected can become a protective factor.[7,14,15,17–21]
After review of literature it was found that, there is no documented study conducted in Benghazi on breastfeeding positioning of mother and baby, baby's attachment to breast and effective sucking. This study was, therefore, conducted with the objective of assessing the correct position, attachment and effective suckling in infant breastfeeding as practiced by mothers attending hospitals at Benghazi, Libya.
MATERIALS AND METHODS
This observational, cross-sectional study was conducted at AlJamahiriya and AlFateh hospitals in Benghazi, Libya, from November 2009 to February 2010. These two hospitals were selected since the majority of deliveries take place there and also for their proximity.
Two hundred fifteen mother–neonate (preterm and full-term) units were admitted to these hospitals during the study period. Fifteen mother–neonate units who had serious illnesses and/or neonatal malformations of palate/tongue were excluded from the study. A total of 200 mother–neonate units were included for the study, eight of which refused to participate. The remaining 192 mother–neonate units were observed for mother and baby's position, infant's mouth attachment and effective suckling during breastfeeding using WHO B-R-E-A-S-T- Feed observation form.[22] Informed verbal consent was obtained before data collection.
Six female medical interns were trained by the investigators to collect data and observe the positions of the mother and baby, infant's mouth attachment to breast and effective suckling by using video clips and hands on training and demonstration in the hospital. The information on the maternal characteristics like age, occupation, parity, breast problems, and baby's age, preterm/full term, birth weight, and any malformations was obtained using pre-designed and pre-tested questionnaire.
All six female medical interns also observed the breastfeeding process for 5 minutes and recorded the mother and infant's positioning, attachment to the breast and effective suckling as per WHO B-R-E-A-S-T Feed observation form. It was done by asking the mother to put her infant to the breast, if the infant had not been fed in the previous hour. If the infant had been fed during the last 1 hour, then the mother was asked when the infant would have the next feed and the observation assessment was planned accordingly.
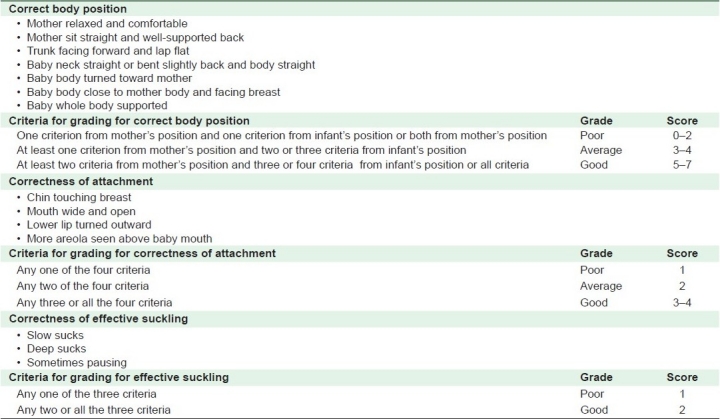
The following arbitrary scoring and grading system was developed and adopted to grade positioning (mother and infant), infant's mouth attachment and effective suckling during breastfeeding based on WHO criteria. Each criterion was assigned 1 point [Table 1].
Table 1.
Grading system for infant's mouth attachment and effective suckling during breastfeeding
The data were analyzed using software SPSS (11.5 version). The categorical variables are presented as percentages. Chi-squared test was used as test of significance and P value less than 0.05 was considered for the statistical significance.
RESULTS
Maternal characteristics
The present study revealed that the majority of the mothers were between 20 and 30 years of age (55.7%), followed by those who were more than 30 years (39.6%) and below 20 years (4.7%). Poor position (22.2%) and poor attachment (33.3%) were high among mothers aged less than 20 years as compared to other age groups (7.6–15.8% and 19.7–23.4%, respectively). However, there was no statistically significant association between the mother's age and poor position (P = 0.238) and attachment (P = 0.662) of babies to the breast during feeding [Table 2].
Table 2.
Maternal characteristics and position of mother and infant and attachment (latch-on) to breast during feeding
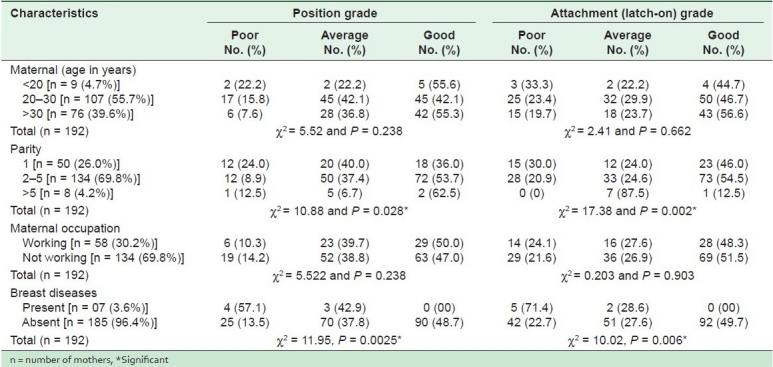
The majority of mothers were multipara (74.0%) and 26.0% were primipara. Among mothers with parity two or more low percentages of poor position (8.9–12.5%) and attachment (0–20.9%) were observed. A statistically significant association was found between parity and position (P = 0.028) and attachment (P = 0.002).
Only 30.2% were working mothers and 69.8% were nonworking. Although there was poorer positioning among nonworking (14.2%) than working mothers (10.3%), poor attachment was more in working (24.1%) than nonworking (21.6%) mothers. However, there was no significant association between maternal occupation and position (P = 0.238) and attachment (P = 0.903).
Breast diseases such as cracked nipples, mastitis, and sore nipples were more associated with poor position (57.1%) and attachment (71.4%). The findings were highly significant at P = 0.002 for position and P = 0.006 for attachment.
Infant characteristics
A total of 14.6% infants were less than 1 week old (early neonatal period) and 85.4% were between 7 and 28 days (late neonatal period) of age. All infants were observed for attachment to the breast and effective suckling [Table 3].
Table 3.
Attachment (latch-on) and effective suckling as per infant characteristics
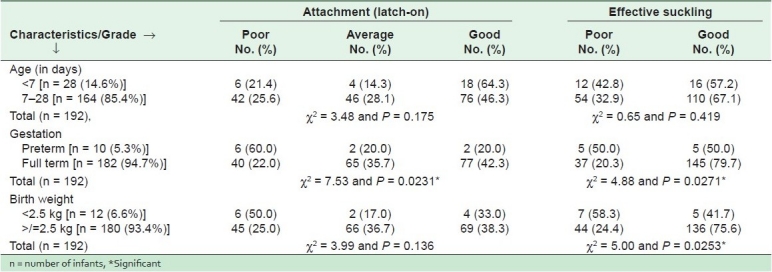
Suckling was poorer (42.8%) in the early neonatal period than the late neonatal period (32.9%). There was no statistically significant association between the age of the babies and attachment (P = 0.175) and effective suckling (P = 0.419) during breastfeeding.
Most of the neonates were full term (94.7%) and only 5.3% were preterm. Only 22% of total full-term babies had poorer attachment as compared to preterm babies (60.0%). The figures for poor suckling were 20.3% among full-term babies and 50.0% in preterm babies. These findings were statistically significant for attachment (P = 0.023) and effective suckling (P = 0.027).
Only 12 (6.6%) babies had birth weight less of than 2.5 kg (low birth weight as per WHO for developing countries) and the remaining 93.6% babies weighed more than 2.5 kg. Poor attachment (50.0%) and poor suckling (58.3%) were more in babies with low birth weight as compared to other groups (25.0% and 24.4%, respectively). There was no significant difference between the birth weight of infant and attachment (P = 0.136) to the breast, but statistically significant difference was observed for effective suckling (P = 0.025).
DISCUSSION
In the present study, younger mothers (<20 years) had poorer attachment as compared to older mothers, but age per se was not associated with position and attachment, which is primarily required for effective breastfeeding. Similar findings were also reported by Kronborg et al. (western Denmark) and Gupta et al. (North India).[23,24] Santo et al from Brazil also reported that adolescent mothers had poorer position[hazard ratio (HR) = 1.48, 95% CI 1.01-2.17] and poorer latch-on [HR = 1.29, 95% CI 1.06-1.58 for each unfavorable parameter].[25]
Our study results indicate that a majority (74.0%) of multiparous mothers had good position and attachment, which could be the result of their previous experience. Studies conducted by Coca et al. (Sao Paulo, Brazil) and Kronborg et al. (western Denmark) also reported that parity was significantly associated with effective breastfeeding (position and attachment).[17,23] However, Gupta et al. from North India did not find any statistically significant association.[24]
Our findings reveal that breast problems like cracked nipples, mastitis, and sore nipples were significantly associated with poor positioning and attachment which are essential for effective breastfeeding. Coca et al. (Sao Paulo, Brazil) reported that women whose infants were incorrectly positioned were 1.94 times at risk (95% CI 1006–3749) of developing nipple trauma compared with women whose infants were correctly positioned.[17]
Another study conducted at Brazil by Coca et al. confirmed that nursing mothers with turgid and/or engorged breasts were more likely to develop nipple injury (95% CI 4.48–33.78).[26] In their studies from Porto Alegre, Brazil, Tait et al. also identified nipple trauma as a disorder that resulted from incorrect positioning and latching-on in breastfeeding.[27,28] A study conducted by Carvalhaes from Brazil reported that breast engorgement makes it more difficult for newborn infants to latch-on correctly because of distension and edema of the nipple and areolar region.[29] Another study from Brazil reported that as per parity, the highest incidence of nipple trauma was found in primiparous women, which may be explained by inexperience in the breastfeeding technique.[30]
The present study indicates that preterm infants (<37 weeks of gestation) had poor attachment and suckling. Coca et al. did not find any association between weeks of gestation and strength of suckling.[26]
We observed that infants with low birth weight had poor attachment and poor effective suckling. Kronborg et al. and Coca et al. did not find any association between birth weight and nipple trauma (P = 0.41 and P = 0.22, respectively).[23,26]
Our study was able to demonstrate the association between mother-neonate characteristics and positioning, attachment and effective suckling in breastfeeding. Nevertheless, the use of a larger sample size may make it possible to identify the other risk factors.
CONCLUSION AND RECOMMENDATION
Young (<20 years) and primipara mothers need more support and guidance for appropriate breastfeeding techniques. It is recommended that each mother should be observed for mother's and infant's positioning and attachment at the onset of breastfeeding and if needed given counseling on correct positioning and attachment.
All Maternal and Child Health (MCH) care agencies should highlight and formulate a policy for successful and effective initiation of breastfeeding as a part of an integrated neonatal care.
Acknowledgments
The authors thank all the trained interns who were involved in collection of data from the hospitals. Special thanks are expressed for all the faculty of the Family & Community Medicine Dept. of University of Garyounis, and staff of the hospitals in Benghazi, Libya. Last but not the least, thanks to all the mothers & children who participated in the study.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
REFERENCES
- 1.Shembesh NM, Balo NN, Singh R. Breast-feeding and weaning patterns in Benghazi, Libyan Arab Jamahiriya. East Mediterr Health J. 1997;3:251–7. [Google Scholar]
- 2.Henderson P. WHO Press 20 Avenue Appia, 1211. Geneva 27, Switzerland: WHO Press, World Health Organization; 2009. Infant and young child feeding: Model chapter for textbooks for medical students and allied health professionals. Session 1- The importance of infant and young child feeding and recommended practices; pp. 5–6. [PubMed] [Google Scholar]
- 3.Abudejaja A, Singh R, Khan MA. Infant Feeding practices in north-eastern region of Libyan Arab Jamahiriya. Garyounis Med J. 1982;5:29–36. [Google Scholar]
- 4.Singh R, Mailud A, Sharma MP. Pattern of Breast Feeding and Weaning at Benghazi. Washington DC: Presented in 132nd meeting of American Public Health Association; 2004. [Google Scholar]
- 5.Bredan AS, Bshiwah SM, Kumar NS. Infant-feeding practices among urban Libya women. Food Nutr Bull (UNU) 1988;10:39–42. [Google Scholar]
- 6.Banapurmath CR, Nagaraj MC, Banapurmath S, Kesaree N. Breastfeeding practices in villages of central Karnataka. Indian Pediatr. 1996;33:477–9. [PubMed] [Google Scholar]
- 7.Dongre AR, Deshmukh PR, Rawool AP, Garg BS. Where and How Breastfeeding Promotion Initiatives Should Focus Its Attention? A Study from Rural Wardha. Indian J Community Med. 2010;35:226–9. doi: 10.4103/0970-0218.66865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sai M, Kishore S, Kumar P, Aggarwal AK. Breastfeeding Knowledge and Practices amongst Mothers in a Rural Population of North India: A community-based study. J Trop Pediatr. 2009;55:183–8. doi: 10.1093/tropej/fmn110. [DOI] [PubMed] [Google Scholar]
- 9.Mannan I, Rahman SM, Sania A, Seraji HR, Arifeen SE, Winch PJ, et al. Can early postpartum home visits by trained community health workers improve breastfeeding of newborns? J Perinatol. 2008;28:632–40. doi: 10.1038/jp.2008.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vinther T, Helsing E. Breastfeeding- how to support success, A practical guide for health workers. Copenhagen: World Health Organization, Regional Office for Europe; 1997. pp. 10–2. [Google Scholar]
- 11.Woolridge MW. Aetiology of sore nipples. Midwifery. 1986;2:172–6. doi: 10.1016/s0266-6138(86)80042-0. [DOI] [PubMed] [Google Scholar]
- 12.Neifert MR. Breastmilk transfer: Positioning, latch-on, and screening for problems in milk transfer. Clin Obstet Gynecol. 2004;47:656–75. doi: 10.1097/01.grf.0000136183.12304.96. [DOI] [PubMed] [Google Scholar]
- 13.Inch S. Breastfeeding problems: Prevention and management. Community Pract. 2006;79:165–7. [PubMed] [Google Scholar]
- 14.Blair A, Cadwell K, Turner-Maffei C, Brimdyr K. The relationship between positioning, the breastfeeding dynamic, the latching process and pain in breastfeeding mothers with sore nipples. Breastfeed Rev. 2003;11:5–10. [PubMed] [Google Scholar]
- 15.Weigert EM, Giugliani ER, França MC, Oliveira LD, Bonilha A, Espírito Santo LC, et al. The influence of breastfeeding technique on the frequencies of exclusive breastfeeding and nipple trauma in the first month of lactation. J Pediatr (Rio J) 2005;81:310–6. [PubMed] [Google Scholar]
- 16.Matthews MK. Experiences of primiparous breast-feeding mothers in the first days following birth. Clin Nurs Res. 1993;2:309–26. doi: 10.1177/105477389300200307. [DOI] [PubMed] [Google Scholar]
- 17.Coca KP, Gamba MA, Silva RS, Freitas V, Abrão AC. Does breastfeeding position influence the onset of nipple trauma? Rev Esc Enferm USP. 2009;43:442–8. doi: 10.1590/s0080-62342009000200026. [DOI] [PubMed] [Google Scholar]
- 18.Huml S. Sore nipples; a new look at an old problem through the eyes of a dermatologist. Pract Midwife. 1999;2:28–31. [PubMed] [Google Scholar]
- 19.Minchin MK. Positioning for breastfeeding. Birth. 1989;16:67–73. doi: 10.1111/j.1523-536x.1989.tb00864.x. [DOI] [PubMed] [Google Scholar]
- 20.Cadwell K. Latching-on and suckling of the healthy term neonate: Breastfeeding assessment. J Midwifery Womens Health. 2007;52:638–42. doi: 10.1016/j.jmwh.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 21.Narramore N. Supporting breastfeeding mothers on children's wards: An overview. Paediatr Nurs. 2007;19:18–21. doi: 10.7748/paed2007.02.19.1.18.c4441. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization. Breastfeeding counselling - a training course trainer's guide, part one, Sessions 5- observing a breastfeed. World Health Organization, CDD programme, UNICEF. 1993 WHO/CDR/93.4 UNICEF/NUT/93.2. [Google Scholar]
- 23.Kronborg H, Væth M. How Are Effective Breastfeeding Technique and Pacifier Use Related to Breastfeeding Problems and Breastfeeding Duration? Birth. 2009;36:34–42. doi: 10.1111/j.1523-536X.2008.00293.x. [DOI] [PubMed] [Google Scholar]
- 24.Gupta M, Aggarwal AK. Feasibility Study of IMNCI Guidelines on Effective Breastfeeding in a Rural Area of North India. Indian J Community Med. 2008;33:201–3. doi: 10.4103/0970-0218.42067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Santo LC, de Oliveira LD, Giugliani ER. Factors associated with low incidence of exclusive breastfeeding for the first 6 months. Birth. 2007;34:212–9. doi: 10.1111/j.1523-536X.2007.00173.x. [DOI] [PubMed] [Google Scholar]
- 26.Coca KP, Gamba MA, Silva RS, Abrão AC. Factors associated with nipple trauma in the maternity unit. J Pediatr (Rio J) 2009;85:341–5. doi: 10.2223/JPED.1916. [DOI] [PubMed] [Google Scholar]
- 27.Tait P. Nipple pain in breastfeeding women: Causes, treatment, and prevention strategies. J Midwifery Womens Health. 2000;45:212–5. doi: 10.1016/s1526-9523(00)00011-8. [DOI] [PubMed] [Google Scholar]
- 28.Weigert EM, Giugliani ER, França MC, Oliveira LD, Bonilha A, Espírito Santo LC, et al. The influence of breastfeeding technique on the frequencies of exclusive breastfeeding and nipple trauma in the first month of lactation. J Pediatr (Rio J) 2005;81:310–6. [PubMed] [Google Scholar]
- 29.Carvalhaes MA, Corrêa CR. Identification of difficulties at the beginning of breastfeeding by means of protocol application. J Pediatr (Rio J) 2003;79:13–20. [PubMed] [Google Scholar]
- 30.Shimoda GT, Silva IA, Santos JL. Characteristics, frequency and factors present in nipples damage occurence in lactating women. Rev Bras Enferm. 2005;58:529–34. doi: 10.1590/s0034-71672005000500006. [DOI] [PubMed] [Google Scholar]


