Abstract
Aims:
This study was taken up with the aim to investigate the pattern of supraclavicular lymphadenopathy among patients presenting to our tertiary care institution, evaluate the diagnostic efficacy of fine needle aspiration cytology (FNAC), and analyze the diagnostic pitfalls.
Materials and Methods:
A total of 215 patients were subjected to FNAC of supraclavicular lymph nodes over a three-year period (August 2006 to July 2009). Since in 18 patients as either the aspirate was inadequate or the opinion was equivocal, we analyzed the remaining 197 cases.
Results:
Malignant pathology accounted for 79.7% (157/197) of the cases. These were mostly cases of metastatic squamous cell carcinoma (79/197, 40.1%), adenocarcinoma (47/197, 23.9%), small cell carcinoma (12/197, 6.1%) and lymphoma (10/197, 5%). There were 28 (14.2%) cases of tuberculosis. Out of these 197 patients, 92 patients were biopsied. The opinion based on FNAC was erroneous in 6 cases but corroborated with the final histopathology findings in the remaining 86 cases.
Conclusion:
FNAC is an excellent first line of investigation; and when used with a proper combination of experience and diligence, it can greatly reduce the number of errors.
Keywords: Fine needle aspiration cytology, metastatic carcinoma, supraclavicular lymph nodes
Introduction
Fine needle aspiration cytology (FNAC) of enlarged lymph nodes is a useful screening test. Studies in the past have shown metastatic malignancy to be a major cause of enlargement of supraclavicular lymph nodes.[1,2] In this study, we have attempted to analyze the pattern of presentation of supraclavicular lymphadenopathy and evaluate the diagnostic efficacy of FNAC in the assessment of these cases.
Materials and Methods
This prospective study was carried out over a period of three years (August 2006 to July 2009) at our tertiary care institute. A total of 215 patients with palpable supraclavicular lymph nodes were subjected to FNAC using a 22-G needle and a 10-mL disposable syringe. The slides were both air-dried and wet-fixed for May-Grünwald-Giemsa and Papanicolaou stains, respectively. Clinical details with regard to age, sex, site, size, duration, involvement of other lymph nodes and other investigations performed were recorded. In 92 patients, lymph node biopsy was performed. We compared the histopathological findings with the previous cytological impression. In 18cases, either the needle aspirate was inadequate or the cytological opinion was equivocal; hence the remaining 197 cases were analyzed.
The cases were divided into six groups, viz., reactive lymphoid hyperplasia, acute non-specific lymphadenitis, tuberculous lymphadenitis, metastatic malignancy, lymphoma, and a miscellaneous group showing features that did not conform to those of any of the earlier-mentioned groups. Cases with hematological malignancy were excluded.
Results
In this study, 215 patients were subjected to FNAC for supraclavicular lymph node enlargement. Among these patients, in 12 cases the aspirate was inadequate despite repeated attempts; and in 6 cases, the cytological impression was equivocal. Hence these 18 cases were excluded from the study, and the remaining 197 cases were analyzed.
The male-to-female ratio in the study was 1.3:1, and more patients had left-sided nodal enlargement (left:right : 1.2:1). The mean age at presentation was 53.3 years, being 45.1 years for male and female patients, respectively. The age at presentation ranged from 18 to 75 years. Malignant pathology accounted for 79.7% (157/197) of the cases. These were cases of metastatic squamous cell carcinoma (79/197, 40.1%), adenocarcinoma (47/197, 23.9%), small cell carcinoma (12/197, 6.1%), poorly differentiated carcinoma (8/197, 4.1%), and a single case of seminoma [Table 1] [Figure 1]. Besides these metastatic tumors, there were also cases of non-Hodgkin's lymphoma and Hodgkin's disease (6/197, i.e., 3%; and 4/197, i.e., 2%; respectively).
Table 1.
Proportion of different malignancies in the study
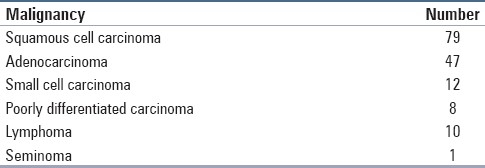
Figure 1.
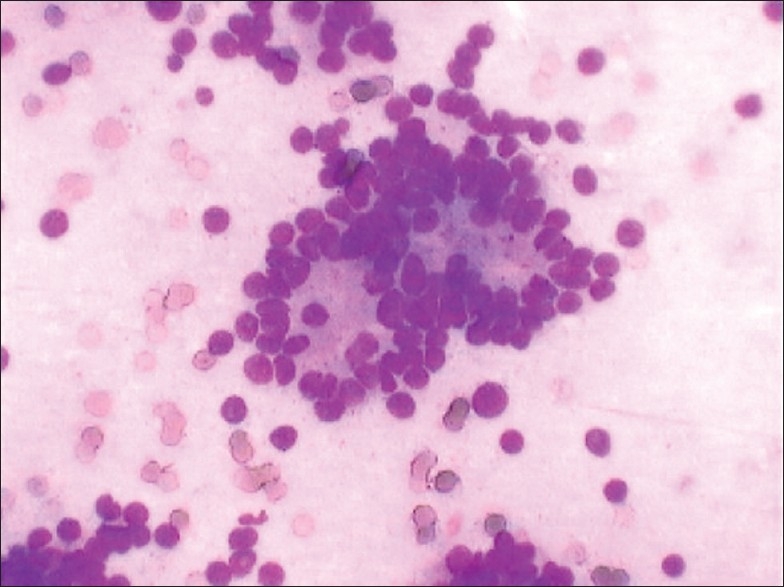
Metastatic deposit of prostatic adenocarcinoma in supraclavicular lymph node (MGG, ×400)
There were 28 (14.2%) cases of tuberculosis, majority of which involved patients up to 40 years of age [Table 2]. However, cases of malignancy were markedly predominant in patients above 30years age [Figure 2]. Reactive hyperplasia was diagnosed in 11 patients, while only three patients had acute non-specific lymphadenitis.
Table 2.
Comparison of tuberculous and malignant cases in different age groups
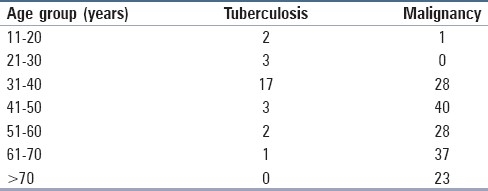
Figure 2.
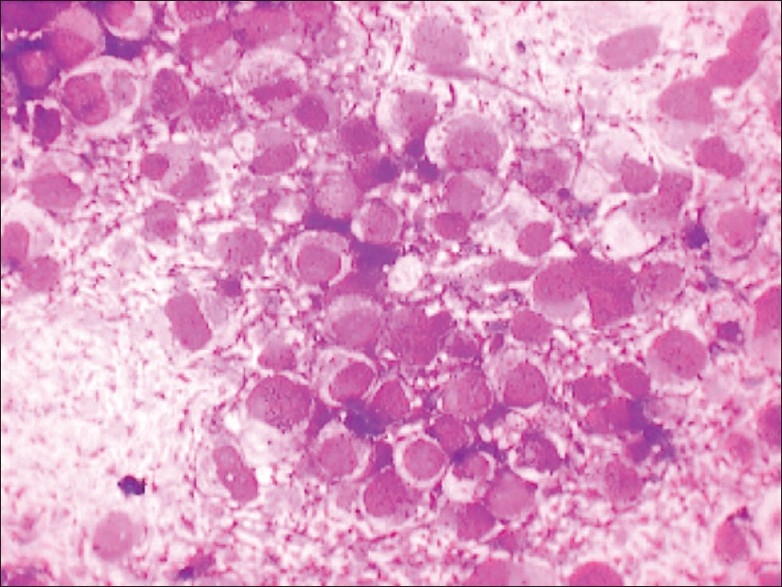
Metastatic deposit of seminoma in supraclavicular lymph node (MGG, ×400 )
Out of these 197 patients, 92 patients were biopsied. The opinion based on FNAC was erroneous in 6 cases but corroborated with the final histopathology findings in the remaining 86 cases.
Discussion
Fine needle aspiration cytology (FNAC) is used routinely as a first-line diagnostic test. The majority of studies reveal a malignant cause for palpable supraclavicular lymph nodes.[1,2] In our study, malignant pathology accounted for the majority of cases (157/197, 79.7%). Among these cases, 74.2% (147/197) were due to metastatic nodal involvement, while 5.1% (10/197) of cases were due to either Hodgkin's disease or non-Hodgkin's lymphoma. Palpable nodes with metastasis are significantly larger than non-palpable nodes with metastasis.[3] The incidence of malignancy rose steadily through the age groups to greater than 95% in patients above 60 years of age. Hence there is a pressing need for FNAC of enlarged supraclavicular lymph nodes in the elderly, which can provide an early clue to the diagnosis.
Lymphadenopathy in the supraclavicular region may be difficult to detect on clinical examination. The sensitivity of ultrasound for detecting nodes more than 1 cm in size is 16.7% higher than that of clinical examination. When compared with histological examination following surgical excision, the sensitivity and specificity of supraclavicular ultrasound are 91% and 94%, respectively, compared with 82% and 83% for clinical palpation; and importantly, ultrasound detects up to 50% of occult non-palpable metastases.[4]
Common primary sites included the lungs (65/147. 44.2%), breast (29/147, 19.7%), stomach (17/147, 11.6%) and oesophagus (5/147, 3.4%). In addition, there was one case each of nasopharyngeal carcinoma and seminoma, which showed metastasis to the supraclavicular nodes. In another 20% of the cases, the primary site could not be discerned. These findings corroborate with those of the earlier studies.[2,3,5]
Among the 79 cases of metastatic squamous cell carcinoma, 2 cases were erroneously reported as reactive hyperplasia. The other cases were successfully diagnosed despite some showing cystic degenerative changes. This underscores the importance of thorough sampling of the enlarged lymph node, which otherwise may lead to oversight. Given the limitations of FNAC, all suspicious lymph nodes should be biopsied following FNAC, even if the FNAC is reported to be normal or as demonstrating reactive changes only.[6] This is especially important as unusual cases in which microfilaria and tuberculosis were coexisting with metastatic adenocarcinoma have been reported in literature.[7,8]
Three cases of tuberculosis were initially missed out due to inadequate sampling. One case was reported as non-specific lymphadenitis, while 2 others were signed out as reactive hyperplasia.
The cases of metastatic tumors usually involved single lymph node groups. The case of nasopharyngeal carcinoma was an exception, involving both cervical and supraclavicular nodes. The aspirate from the supraclavicular node showed only few atypical cells. As this site is unusual for nasopharyngeal carcinoma to metastasize, we finally based our opinion on the cervical node aspirate and clinical findings.
The cases of lymphoma, on the other hand, involved other lymph node groups as well. A case of non-Hodgkin's lymphoma in a 55-year-old lady surprised us. This single enlarged supraclavicular lymph node was reported initially as reactive hyperplasia. However, when the node continued to enlarge and as more nodes cropped up in the cervical region after conventional antibiotic therapy, a lymph node biopsy was performed. The biopsy showed presence of peripheral T-cell lymphoma.
Conclusion
Based on our study, we feel that FNAC of palpable supraclavicular lymph nodes as a first line of investigation is a cost-effective procedure and is not only useful in the diagnosis of various lesions but can also help in deciding on appropriate management. Furthermore, the histological architecture from cell blocks can be correlated with cytology, and such material can be used for appropriate histochemical and immunomarker studies, which can be useful in enhancing the diagnosis.[1]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gupta RK, Naran S, Lallu S, Fauck R. The diagnostic value of fine needle aspiration cytology (FNAC) in the assessment of palpable supraclavicular lymph nodes: a study of 218 cases. Cytopathology. 2003;14:201–7. doi: 10.1046/j.1365-2303.2003.00057.x. [DOI] [PubMed] [Google Scholar]
- 2.Gupta N, Rajwanshi A, Srinivasan R, Nijhawan R. Pathology of supraclavicular lymphadenopathy in Chandigarh, north India:an audit of 200 cases diagnosed by needle aspiration. Cytopathology. 2006;17:94–6. doi: 10.1111/j.1365-2303.2006.00285.x. [DOI] [PubMed] [Google Scholar]
- 3.van Overhagen H, Brakel K, Heijenbrok MW, van Kasteren JH, van de Moosdjik CN, Roldaan AC, et al. Metastasis in supraclavicular lymph nodes in lung cancer: assessment with palpation, US, and CT. Radiology. 2004;232:75–80. doi: 10.1148/radiol.2321030663. [DOI] [PubMed] [Google Scholar]
- 4.Kumaran M, Benamore RE, Vaidhyanath R, Muller S, Richards CJ, Peake MD, et al. Ultrasound guided cytological aspiration of supraclavicular lymph nodes in patients with suspected lung cancer. Thorax. 2005;60:229–33. doi: 10.1136/thx.2004.029223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee J. Usefulness and limitations of fine needle aspiration cytology in adult cervical lymph node enlargement patients: An analysis of 342 cases. Tuberc Respir Dis. 2004;56:18–28. [Google Scholar]
- 6.Morris-Stiff Cr, Cheang P, Key S, Verghese A, Havard TJ. Does the surgeon still have a role to play in the diagnosis and management of lymphomas? World J Surg Oncol. 2008;4:6–13. doi: 10.1186/1477-7819-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kolte SS, Satarkar RN, Mane PM. Microfilaria concomitant with metastatic deposits of adenocarcinoma in lymph node fine needle aspiration cytology: A chance finding. J Cytol. 2010;27:78–80. doi: 10.4103/0970-9371.70759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wani BN, Jajoo SN. Ipsilateral axillary tubercular lymphadenopathy, contralateral osseous tuberculosis in a case of ductal carcinoma of breast. Indian J Cancer. 2008;45:182–4. doi: 10.4103/0019-509x.44671. [DOI] [PubMed] [Google Scholar]


