Abstract
Aims:
The aim of this study was to compare demographics, clinical manifestations, associated systemic and ocular factors, severity and activity of patients with unilateral thyroid eye disease (U-TED) versus bilateral thyroid eye disease (B-TED).
Materials and Methods:
In a cross-sectional study, all patients with Graves’ hyperthyroidism and primary hypothyroidism seen in an endocrinology clinic were included from September 2003 to July 2006. Demographics, complete eye examination, severity score (NOSPECS, total eye score), and clinical activity score were recorded and compared in the B-TED and U-TED groups of patients.
Results:
From 851 patients with thyroid disorders, 303 (35.6%) had TED. Thirty-two patients (32/ 303, 10.56%) were found to have U-TED. Patients with U-TED (mean age 31.6 ± 11.6 years) were significantly younger than patients with B-TED (mean age 37.7 ± 14.7 years). Monovariate analysis (Chi-square and independent sample t-test) showed a significantly higher severity score in B-TED (U-TED 4.09±4.05, B-TED: 6.7±6.3; P= 0.002) and more activity score in B-TED (U-TED= 1.03±0.96, B-TED: 1.74±1.6, P= 0.001). However, multivariate analysis did not show any significant difference between the two groups in terms of age, gender, type of thyroid disease, duration of thyroid disease and TED, severity and activity of TED, smoking habit, and presentation of TED before or after the presentation of thyroid disease (0.1<P<1).
Conclusion:
This study did not find any significant difference between U-TED and B-TED in relation to the demographics, type of thyroid disease, associated findings, and severity and activity of TED.
Keywords: Graves’ ophthalmopathy, thyroid eye disease, unilateral
Thyroid eye disease (TED) is an inflammatory orbital disease of autoimmune origin with the potential to cause severe functional and psychosocial effects. Orbital involvement is usually bilateral but may be highly asymmetric in a minority of patients.[1] Persistent unilateral involvement may occur.[2–12] However, some reports suggest that clinically unilateral disease may, at last, bilateralize[2,3] or is bilateral from the onset, though not clinically apparent.[4]
It is unclear if the severity and activity of TED are different in patients who have unilateral TED (U-TED) versus bilateral TED (B-TED). We performed a cross-sectional study on patients with different thyroid disorders between 2003 and 2006. The aim of this study was to compare the demographics and clinical manifestation, especially severity and activity scores of TED in patients who presented with U-TED versus B-TED.
Materials and Methods
In a cross-sectional study, all patients with different thyroid disorders who visited a referral endocrinology clinic (Tehran University Institute of Endocrinology) between September 2003 and July 2006 were included.
Two general practitioners were initially trained to screen the thyroid disorder patients with regard to any signs and/or symptoms of TED. A special data sheet was completed for each patient in the eye plastic clinic (Rassoul Akram Hospital). Patients with any symptoms and/or signs of TED were referred to the TED clinic for further evaluation.
Diagnosis of thyroid dysfunction was based on clinical examination and hormone level and in some cases thyroid gland scan and sonography. Antibodies’ tests were not available in the beginning but anti-thyroid peroxidase antibody was checked since 2005 when it became available. Antibody titers were not used for the definition of thyroid gland disease as hypo- versus hyperthyroid. They were checked (when available) in order to assess the autoimmunity in the setting of thyroid disease.
Diagnosis of TED was clinical and based on thyroid disorder associated with one of the following signs: eyelid retraction and/or lag, proptosis, restrictive myopathy, dysthyroid optic neuropathy, fluctuating eyelid edema and/ or erythema, conjunctival chemosis and/ or diffuse redness, caruncular edema. Orbital imaging was requested for all cases with U-TED to look for other orbital pathologies and selected B-TED to mainly look for the signs of optic neuropathy. Findings on imaging, however, were not considered for the diagnosis of TED as we aimed to compare clinical unilateral versus B-TED. U-TED was considered when there was a diagnosis of TED in one eye but no clinical sign in the other eye.
A special TED form was completed for each subject which included different sections regarding thyroid gland disorder; associated systemic diseases including autoimmune diseases such as systemic lupus erythematosus and rheumatoid arthritis, diabetes mellitus, myasthenia gravis, and cardiovascular diseases; medications’ history; eye symptoms at presentation of TED; visual function tests including best corrected visual acuity, optic disc, color vision, and visual field; intraocular pressure (IOP) in primary and up-gaze; Hertel exophthalmometry; eyelid examination; ocular motility examination; slit-lamp examination; and findings on orbital imaging. The examination ended by recording Mourits’ clinical activity score[7] (CAS) and NOSPECS severity score.[8]
NOSPECS stands for no TED sign (N), only eyelid sign (O), soft tissue involvement (S), proptosis (P), extra-ocular motility restriction (E), corneal involvement (C), and sight loss (S). The NOSPECS severity score has six classes (N=0, O=1, S=2, P=3, E=4, C=5, and S=6) and four grades with increasing severity (0, 1, 2, and 3) for each class. This was used to calculate the total eye score (TES) which ranged from 0 to 63 (the higher the score the worse the severity). The score of each class was equal to the number of class multiplied by the number of grade at each class. For example, a patient with grade 2 of proptosis has a score of 6 in the P class (2× 3= 6). TES was the sum of all the scores in the six classes. In case of asymmetric severity and/or activity scores, the worst score was considered for the management and analysis. Open-angle glaucoma was defined as more than 21 mmHg of IOP in primary gaze associated with glaucomatous optic disc changes and/ or visual field defect.
Ethics committee approval (eye research center ethics committee) and consent form were obtained. Data were entered and analyzed with software SPSS (Version 16, Chicago).
Independent sample t-test was used for comparing the means between the two groups and Chi-square test was used to compare the nonparametric variables in the two groups. Multivariate binary regression analysis was used to analyze the significant variables found in the monovariate analyses.
Results
There were 851 patients with Graves’ hyperthyroidism and primary hypothyroidism. TED was clinically found in 303 patients (303/851, 35.6%). The majority of them (280/303, 92.4%) had Graves’ hyperthyroidism and 23 (7.5%) had primary hypothyroidism. Mean age was 37.06 ± 14.53 (range: 9-80 years). There were 201 (201/303, 66.3%) females.
The majority of patients (271/303, 89.4%) presented with B-TED and 10.5% (32/303) with U-TED. Mean age (31.6 ± 11.6) of U-TED was significantly lower than mean age (37.7±14.7) of B-TED. Male/ female ratio was 1:1.8 in the B-TED and 1:4 in U-TED (P= 0.059). Associated systemic diseases (diabetes mellitus, cardiovascular diseases, autoimmune diseases) were present in only two patients (2/32, 6.2%) with unilateral involvement but in 43 patients (43/271, 15.8%) with B-TED (P=0.03). Open-angle glaucoma was found in two patients (58 and 54 years old) with U-TED (2/32, 6.2%) and in 16 (16/271, 5.9%) with B-TED (P= 0.5). There were significantly more severity and activity scores in the B-TED group [Table 1].
Table 1.
Monovariate analysis of different variables in 32 patients with unilateral and 271 with bilateral thyroid eye disease
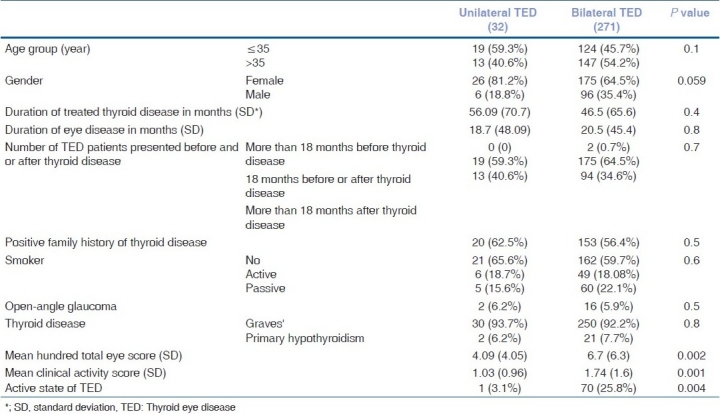
Gender, age groups (before and after age 35), duration of thyroid disease, duration of TED, time interval between TED and thyroid disease, family history of thyroid disease, smoking habit, frequency of open-angle glaucoma, and type of thyroid disorder were not significantly different between the two groups in a monovariate analysis [Table 1].
Significant differences between the two groups regarding the mean age, associated systemic diseases, severity and activity scores in monovariate analysis [Table 1] were re-analyzed. However, a multivariate binary regression analysis of the significant variables showed that none of them was independently significant between the two groups (0.9 <P<1). Patients with U-TED showed different severity of TED [Fig. 1].
Figure 1.
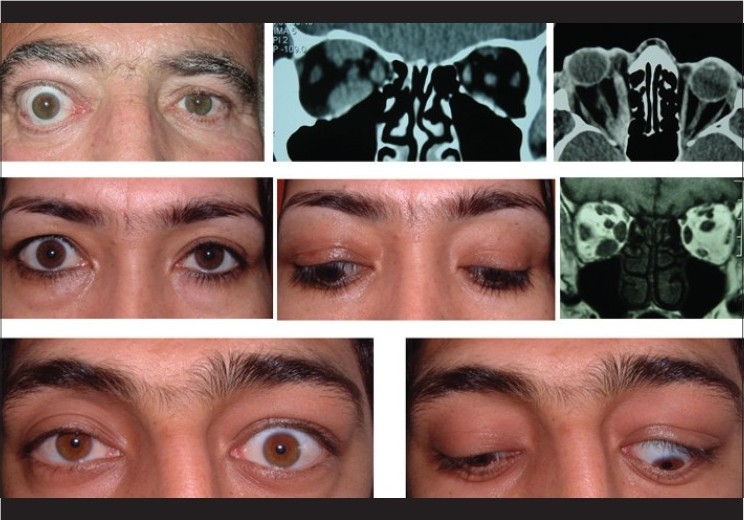
Top photos show a patient with unilateral thyroid optic neuropathy and coronal and axial computerized tomography (CT) scan demonstrating an apical crowding. Middle photos show a patient with unilateral thyroid extra-ocular myopathy and coronal CT scan demonstrating muscles’ enlargement. Bottom photos show a patient with unilateral thyroid eyelid retraction
Comparing unilateral versus B-TED in the female patients, there was no significant difference in activity (P= 0.136) or severity score (P=0.065). Accordingly, the male group with unilateral- versus B-TED did not show a significant difference in activity (P= 0.083) or severity score (P=0.451).
Discussion
The usual presentation of TED is bilateral involvement which may be asymmetric. U-TED has been reported in 9-15% of patients with TED.[1,4,5] Change from unilateral to B-TED has been reported in almost half of the patients,[2,4–6] which may take as long as seven years.[3] We did a cross-sectional study and found over 10% (32/303) unilateral presentation in patients with different grades of TED. Annunziate et al.,[13] recently reported a prevalence of 10.12% for unilateral or asymmetrical TED in their center. High prevalence of U-TED in our study may be attributed to the definition of TED which might have included patients with asymmetric TED. Patients might have forgotten to report conjunctival and eyelid edema on the side of less involvement. Furthermore, a mild degree of eyelid retraction or proptosis might not have been detected because of more prominent signs on the other side. There might also be cases with radiologically asymmetric B-TED who were clinically considered as U-TED in this study. Also, because this study was from a university hospital, it is possible that the numbers reported may over-represent the real prevalence of B-TED, as it is likely that referrals to our clinic are more common for patients with atypical TED presentation rather than typical symmetric TED.
The mean age of presentation in our study was 37.06 years which is lower than other studies.[4,9,10] This may generally reflect the younger population of the region of this study or ethnic difference. Our univariate analysis showed a significantly younger mean age in the U-TED group. However, multivariate binary regression re-analysis did not show any significance in this regard. Moreover, age group analysis [Table 1] did not show a significant difference between the two groups. Whereas, others[4,5,10] have reported that unilateral involvement is more often seen among older patients.
Parallel to previous studies,[1,9,10] we found female preponderance in both unilateral and B-TED. Although, the female to male ratio was higher in patients with bilateral than U-TED, this difference was not significant.
Our study found that type of thyroid disorder was not significantly different between unilateral and B-TED (P=0.8). Eckstein et al.,[11] however, reported a significantly more asymmetric TED in patients with hypothyroid and euthyroid TED.[12]
Although monovariate analysis showed that B-TED had significantly more severity and activity scores, multivariate binary regression re-analysis did not show any independent factor significantly different between the two groups. Others[2,4] also found that the severity and activity of TED are the same in unilateral and B-TED. It has been shown that U-TED may present with optic neuropathy as an initial manifestation.[12] Therefore, U-TED should not be considered as a mild and low-grade form of TED.
Our data on age, the interval between the onset of thyroid disease and eye disease, duration of thyroid and eye disease, eye changes, and smoking habits indicate that patients with U-TED, most probably, belong to the same population as those with bilateral eye disease. This would be against the concept that asymmetric TED is a less severe form of TED.[1,11,14] However, it has been shown that less than half of the cases with unilateral presentation may eventually develop bilateral disease.[2,4,6]
It seems that TED should be viewed in the box of different orbital inflammatory syndromes (OIS) in which different types of predominantly unilateral involvement, such as idiopathic OIS, and bilateral involvement, like TED, could be observed. There may be orbital structural differences that result in asymmetric blood flow, lymphatic drainage, or tissue distensibility.[1] Whether there are more (number or sensitive) receptors for the auto-antibodies in one orbital tissue is a subject of future studies. In fact, the systemic nature of TED (like ocular and orbital metastasis of cancers) makes it difficult to explain why pure unilateral disease would occur at all. It could be a matter of time to switch from unilateral to bilateral TED. If and how many will have developed B-TED in different time intervals are the subjects of future studies. The possibility of asymmetric clinical presentation of TED or subclinical TED instead of U-TED is an open question which needs a further long-term cohort study.
In conclusion, we did not find any significant difference between U-TED and B-TED with regards to the demographics, type of thyroid disease, associated findings, and severity and activity of TED.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Soroudi AE, Goldberg RA, McCann JD. Prevalence of asymmetric exophthalmos in Grave's orbitopathy. Ophthalmic Plast Reconstr Surg. 2004;20:224–5. doi: 10.1097/01.iop.0000124675.80763.5a. [DOI] [PubMed] [Google Scholar]
- 2.Daumerie Ch, Duprez Th, Boschi A. Long-term multidisciplinary follow-up of unilateral thyroid-associated orbitopathy. Eur J Intern Med. 2008;19:531–6. doi: 10.1016/j.ejim.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 3.Kalmann R, Mourits MP. Late recurrence of unilateral Graves’ orbitopathy on the contralateral side. Am J Opthalmol. 2002;5:7727–9. doi: 10.1016/s0002-9394(02)01390-9. [DOI] [PubMed] [Google Scholar]
- 4.Wiersinga WM, Smit T, Van der Graag R, Mourits M, Korneef L. Clinical presentation of Graves’ ophthalmopathy. Ophthalmic Res. 1989;21:73–82. doi: 10.1159/000266782. [DOI] [PubMed] [Google Scholar]
- 5.Lumegra G, Prummel MF, Baldeschi L. Unilateral Graves Orbitopathy: A case control and retrospective follow up study. Türk Jem . 2004;8(Suppl-1):63. [Google Scholar]
- 6.Perrild H, Feldt-Rusmussen U, Bech K, Ahlgren P, Hansen JM. The differential diagnosis problems in unilateral euthyroid Graves’ ophthalmopathy. Acta Endocrinol (Copenh) 1984;106:471. doi: 10.1530/acta.0.1060471. [DOI] [PubMed] [Google Scholar]
- 7.Mourits MP, Koornneef L, Wiersinga WM, Prummel MF, Berghout A, van der Gaag R. Clinical criteria for assessment of disease activity in Graves’ ophthalmopathy: A novel approach. Br J Ophthalmol. 1989;73:639–44. doi: 10.1136/bjo.73.8.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Werner SC. Modification of the classification of the eye changes of Graves’ disease: recommendations of the Ad Hoc Committee of the American Thyroid Association. J Clin Endocr Metab. 1977;44:203–4. doi: 10.1210/jcem-44-1-203. [DOI] [PubMed] [Google Scholar]
- 9.Bartley GB. The epidemiologic characteristics and clinical course of ophthalmopathy associated with autoimmune thyroid disease in Olmsted County, Minnesota. Trans Am Ophthalmol Soc. 1994;92:477–588. [PMC free article] [PubMed] [Google Scholar]
- 10.Kendler DL, Lippa J, Rootman J. The initial clinical characteristics of Graves’ orbitopathy vary with age and sex. Arch Ophthalmol. 1993;111:197–201. doi: 10.1001/archopht.1993.01090020051022. [DOI] [PubMed] [Google Scholar]
- 11.Eckstein AK, Loesch C, Glowacka D, Schott M, Mann K, Esser J, Morgenthaler NG. Euthyroid and primarily hypothyroid patients develop milder and significantly more asymmetric Graves’ ophthalmopathy. Br J Ophthalmol. 2009;93:1052–6. doi: 10.1136/bjo.2007.137265. [DOI] [PubMed] [Google Scholar]
- 12.Arslan E, Yavaşoğlu I, Cildağ BM, Kocatürk T. Unilateral optic neuropathy as the initial manifestation of euthyroid Graves’ disease. Intern Med. 2009;48:1993–4. doi: 10.2169/internalmedicine.48.2372. [DOI] [PubMed] [Google Scholar]
- 13.Annunziate CC, Kim SJ, Oh SR, Chokthaweesak W, Korn BS, Kikkawa DO. Unilateral and asymmetric thyroid related orbitopathy: Clinical characteristics and results of orbital decompression. ASOPRS fall symposium. 2009 Oct; poster 27. [Google Scholar]
- 14.Bartalena L, Pinchera A, Marcocci C. Management of Graves’ ophthalmopathy. Reality Perspect Endocr Rev. 2000;21:168–99. doi: 10.1210/edrv.21.2.0393. [DOI] [PubMed] [Google Scholar]


