Abstract
We report the success rate and problems associated with conventional dacryocystorhinostomy (DCR) in failed cases of Trans-canalicular, laser-assisted DCR (TCLADCR). Out of 50 patients operated by the TCLADCR technique during the period 2005 – 2006, 33 patients had failure, which was confirmed on syringing of the nasolacrimal passage. Before considering them for conventional DCR, a thorough ear, nose, throat (ENT) examination was done by an ENT surgeon, to rule out a nasal pathology. All the patients were operated by the conventional standard DCR method at a medical college. While performing the surgery, the problems that came across were identified and noted. The success rate was found to be 91% in this study in a follow-up period of one year, with no major intra-operative problems. Conventional DCR is still a gold standard and should be considered as a procedure of choice in failed cases of TCLDCR.
Keywords: Conventional dacryocystorhinostomy, trans-canalicular laser-assisted dacryocystorhinostomy
External dacryocystorhinostomy (DCR), in which a communication is created between the lacrimal sac mucosa and nasal mucosa, is a widely acceptable treatment for nasolacrimal duct obstruction (NLDO).[1] The disadvantages of this procedure include scarring at the site of the incision, hemorrhage during the procedure, and disruption of the anatomy of the medial canthus.
With the introduction of endoscopic sinus surgery and lasers, trans-canalicular laser-assisted DCR (TCLADCR) has become another modality for treating NLDO. This procedure requires less time, with no hemorrhage, scar or suture. However, despite these advantages, the procedure may fail, as the small osteum is susceptible to blockage.
In this study we have tried to assess the difficulties that we came across, while performing conventional DCR in the failed cases of TCLADCR.
Materials and Methods
A total of 50 patients with distal NLDO, confirmed preoperatively by syringing of the nasolacrimal apparatus, underwent TCLADCR during the period 2005 – 2006. Blocked syringing and symptomatic epiphora of the nasolacrimal passage was seen in 33 patients postoperatively, after a follow up of six months. All these patients were subjected to the conventional DCR procedure after informed consent. All patients were seen by an ENT specialist for any nasal pathology. Thereafter, the patients were operated by a single surgeon under local infiltration anesthesia.
A J-shaped skin incision was made with a No. 15 blade over the sac area. The medial palpebral ligament was identified. The sac was separated from the lateral wall of the nose. In few cases, the sac was firmly adherent to the lacrimal bone and it was difficult to separate it from the bone. It was gently separated with the help of a lacrimal sac dissector. The periosteum overlying the lacrimal fossa and the area above it were elevated with a periosteum elevator. A previously made osteum was identified as a small depression in the lacrimal bone. The size of the osteum was measured by the caliper. The lacrimal bone, lacrimal crest, and the bone above the anterior lacrimal crest were removed with a bone punch to create an opening, 16 – 18 mm in size. A lacrimal probe of an appropriate size was passed through the lower canaliculas till it reached the lacrimal sac. In a few cases, the lacrimal probe failed to reach beyond the junction of the common canaliculas with the sac, identified as scarring at the junction of the common canaliculas into the sac (In these cases lacrimal intubation was performed). The lacrimal sac was opened in a longitudinal fashion to form anterior and posterior lacrimal flaps. The posterior flap was severed. The nasal mucosa was cut in a similar fashion. The posterior nasal mucosal flap was severed. The anterior nasal mucosa flap was sutured to the anterior lacrimal sac flap with 5-0 chromic-catgut. Fibers of the orbicularis were sutured with 5-0 chromic catgut. The skin was sutured with 6-0 prolene in a continuous fashion. Observations were made during each step and were noted. Data were entered in an excel sheet.
After 24 hours, the nasal pack was removed and syringing was done from the upper punctum to check the patency of the lacrimal passage. Postoperatively, patients were given Ibuprofen 400 mg and ofloxacin 400 mg tablets, twice a day, for five days, and local ofloxacin and dexamethasone eye drops for three weeks. The skin sutures were removed after seven days.
The patients were followed up after seven days, one month, six months, and one year. On every visit syringing was done. A successful outcome was defined as elimination of epiphora, absence of dacryocystitis, and negative syringing test result (i.e., unrestricted flow of irrigated saline to the nose) one year after surgery.
Result
The patients were in the age group of 30 to 60 years, (Mean age was 45.24, ± 9.947). There were18 males and 15 females.
Preoperatively all the patients had symptomatic epiphora and blocked syringing of the nasolacrimal passage. Mucocele was seen in five patients (15%) and three patients had a fistulous tract over the sac area (9%). Intraoperatively, blockage at the junction of the opening of the common canaliculas into the sac was seen in three patients. In these patients lacrimal intubation was done. A scarred osteum was seen in seven patients. The average size of the osteum was 4 × 4 mm. The osteotomy site made during TCLADCR was measured from the fundus of the sac with the help of a caliper. The osteum was situated 2 mm below the fundus of the sac in 21 patients (64%). No osteotomy site was seen in 10 patients (30%). The osteotomy site was 5 mm below the fundus of the sac in two patients (6%). Granuloma between the sac and the osteum identified during the separation of the sac from the bone was seen in two patients. Bleeding was not a major issue [Fig. 1]. In all patients it was not difficult to find out the details of the lacrimal sac, lacrimal bone, and nasal mucosa.
Figure 1.
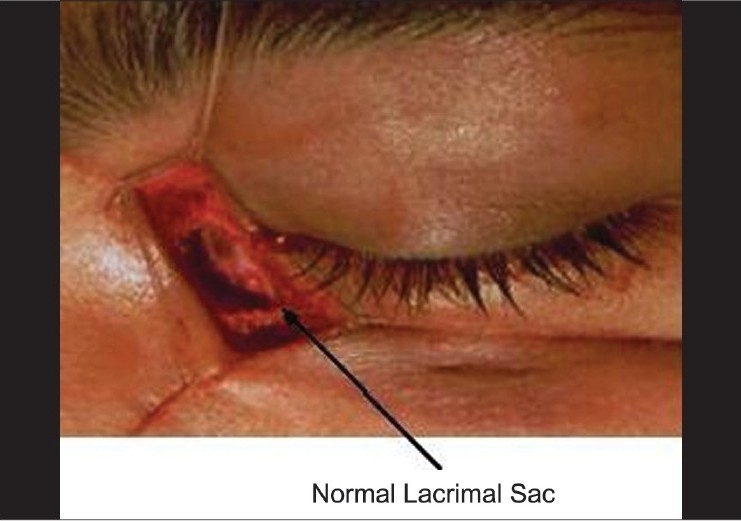
A normal lacrimal sac
Postoperatively blocked syringing because of scarred tissue at the osteum, which was confirmed on nasal endoscopy, was seen in three patients. Symptomatic and anatomic success was seen in 30 patients (91%), at one year.
Discussion
There have been many studies showing the success rate of trans-canalicular, laser-assisted dacryocystorhinostomy TCLADCR in a failed conventional DCR.[2,3] However, a study showing the success rate and problems associated and intra-operative findings in failed TCLADCR is lacking. A study done by the same author shows a success rate of TCLADCR without stenting of 34% (unpublished data), but no stenting was done during the procedure.
In this series of 33 cases of failed TCLADCR, re-operation by conventional DCR has had a success rate of 91%. This compares well with the success rate in the primary operated cases of NLDO.[1,4,5] Success in DCR surgery is compromised by a small osteum and blockage of the osteum by scarred tissue. Linberg et al. showed that an appropriately large osteotomy made during surgery can narrow down to a final size of approximately 2 mm due to tissue growth and scarring.[6] The success rate can be increased by the use of intra-operative mitomycin-C, an anti-proliferative agent placed over the anastomized posterior flaps and the osteotomy site.[7] The small osteotomy size compromises the success rate of TCLADCR. Many studies have reported a lower success rate of TCLADCR in the primary acquired cases of NLDO[8–10] as well as revision cases of failed conventional DCR.[11]
A failure in TLCDCR could be because of the improper osteotomy site. It is difficult to observe the site of osteotomy during TLCDCR. Placing it higher up in the sac can lead to ‘sumping,’ leading to fibrosis and granuloma formation at the osteotomy site. The osteotomy site was seen higher up in the bone in 21 (64%) cases. This site was 2 mm below the fundus of the sac. This was an interesting fact that was noted.
It is important not to fire a laser while negotiating the canalicular system. Inadvertent use of the laser can lead to damage at this site and the canalicular block. These patients require lacrimal intubation. Penetration of a laser in the sac and bone is very important. If the laser does not create an opening TCLADCR is likely to fail, as evidenced by 10 patients having no proper opening in the sac. In these patients, anatomy of the sac on the outer aspect and bone was not disturbed. This fact was not noticed while performing the TCLADCR. Making sac flaps and performing osteotomy was not a problem in any of the cases.
While performing conventional DCR in failed TCLADCR, bleeding and disturbed anatomy of the lacrimal sac was the main concern, but that was not a problem in any case. Patients (n = 3) having fistula between the sac and the skin had it excised during the surgery and it healed well postoperatively. Fistula was formed after an attack of acute dacryocystitis in failed cases of TCLADCR.
Conclusion
This study has shown the success rate of conventional DCR to the tune of 91% in failed cases of TCLADCR. Failure in TCLADCR was because of the small osteum and placement of the osteum at a higher level in the bone. Intra-operatively, there were no major problems encountered. One interesting fact noticed was the higher placement of the osteotomy site, which could have compromised the success rate in TCLADCR.
References
- 1.Tarbet KJ, Custer PL. External dacryocystorhinostomy: Surgical success, patient satisfaction and economic cost. Ophthalmology. 1995;102:1065–70. doi: 10.1016/s0161-6420(95)30910-4. [DOI] [PubMed] [Google Scholar]
- 2.Narioka J, Ohashi Y. Trans canalicular- endonasal semi-conductor diode laser-assisted revision surgery for failed external dacryocystorhinostomy. Am J Ophthalmol. 2008;146:60–8. doi: 10.1016/j.ajo.2008.02.028. [DOI] [PubMed] [Google Scholar]
- 3.Woo KI, Moon SH, Kim YD. Transcanalicular laser assisted revision of failed dacryocystorhinostomy. Ophthalmic Surg Lasers. 1998;29:451–5. [PubMed] [Google Scholar]
- 4.Sharma BR. Non endoscopic endonasal dacryocystorhinostomy versus external dacryocystorhinostomy. Kathmandu Univ Med J (KUMJ) 2008;6:437–42. doi: 10.3126/kumj.v6i4.1731. [DOI] [PubMed] [Google Scholar]
- 5.Tsirbas A, Davis G, Wormald PJ. Mechanical endonasal dacryocystorhinostomy versus external dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2004;20:50–6. doi: 10.1097/01.IOP.0000103006.49679.23. [DOI] [PubMed] [Google Scholar]
- 6.Linberg JV, Anderson RL, Bumsted RM, Barreras R. Study of intranasal osteum external dacryocystorhinostomy. Arch Ophthalmol. 1982;100:1758–62. doi: 10.1001/archopht.1982.01030040738005. [DOI] [PubMed] [Google Scholar]
- 7.Liao SL, Kao SC, Tseng JH, Chen MS, Hou PK. Results of intra operative mitomycin C application in dacryocystorhinostomy. Br J Ophthalmol. 2000;84:903–6. doi: 10.1136/bjo.84.8.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Piaton JM, Limon S, Ounnas N, Keller P. Trans canalicular endodacryocystorhinostomy using neodymium: YAG laser. J Fr Ophthalmol. 1994;17:555–67. [PubMed] [Google Scholar]
- 9.Dalez D, Lemagne JM. Transcanalicular dacryocystorhinostomy by pulse Holmium-YAG laser. Bull Soc Belge Ophthalmol. 1996;263:139–40. [PubMed] [Google Scholar]
- 10.Hong JE, Hatton MP, Leib ML, Fay AM. Endocanalicular laser dacryocystorhinostomy analysis of 118 consecutive surgeries. Ophthalmology. 2005;112:1629–33. doi: 10.1016/j.ophtha.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 11.Patel BC, Phillips B, McLeish WM, Flaharty P, Anderson RL. Trans-canalicular neodymium: YAG laser for revision of dacryocystorhinostomy. Ophthalmology. 1997;104:1191–7. doi: 10.1016/s0161-6420(97)30163-8. [DOI] [PubMed] [Google Scholar]


