Abstract
We report a rare case of keratoconus with granular dystrophy with a follow-up of two decades, documenting the sequential presentation of two diseases confirmed by histology and genetic studies. A 13-year-old boy was diagnosed in 1988 with keratoconus in both eyes (BE) based on slit-lamp biomicroscopy findings of corneal ectasia in BE accompanied by Fleischer's ring, Vogt's striae, a small, old, healed hydrops. The left eye (LE) had central corneal thinning and scar in the central area involving the mid and posterior stroma secondary to healed hydrops. Penetrating keratoplasty (PKP) was advised. The boy was lost to follow-up till 1991 and presented with white, dot-like opacities in the central cornea in the RE only, suggestive of granular corneal dystrophy. Similar findings of white, dot-like opacities were noted in the LE in 1995 and the patient subsequently underwent PKP in BE. Histopathology of corneal buttons confirmed the presence of patchy, crystal-like orange deposits, which stained bright red with Masson's trichrome. Mutational analysis of the TGFBI gene in patient's DNA revealed a heterozygous mutation corresponding to a change in Arg555Trp in the keratoepithelin protein. Granular dystrophy recurred after 8 years in the RE.
Keywords: Bilateral keratoconus, granular dystrophy, late occurrence
Introduction
Keratoconus is a noninflammatory, usually bilateral progressive thinning of the cornea leading to ectasia, Fleischer's ring, Vogt's striae, and scarring with irregular astigmatism resulting in poor visual acuity. Sometimes patients may present as corneal hydrops.[1] Keratoconus is also known to coexist with other ocular conditions such as corneal dystrophies, retinitis pigmentosa, and Leber's congenital amaurosis.[1–6] There are few reports that discuss the association of granular dystrophy (GCD) with keratoconus.[2–5] We report a rare case of bilateral keratoconus where the patient later developed GCD in both eyes and underwent bilateral penetrating keratoplasty (PKP).
Case Report
A 13-year-old boy was seen at our institute in 1988 for diminution of vision of 3 years’ duration in both eyes (BE). The visual acuity was counting fingers at 3 m in the right eye (RE) and 20/50 in the left eye (LE) with a –1.00 DS/–4.00 D Cyl at 90°. Slit-lamp examination revealed corneal ectasia with the presence of Fleischer's ring, Vogt's striae, a small healed rupture of Descemet's membrane in the RE suggestive of old hydrops with scarring in the central cornea of the RE, and central corneal thinning with ectasia and central corneal scar in the central area involving the mid and posterior stroma secondary to healed hydrops in the LE. Lenses were clear. The fundus was within normal limits in both eyes. With a diagnosis of keratoconus in both eyes and healed hydrops in BE, he was advised to undergo PKP in the RE. There was no history of consanguinity. There was no family history of keratoconus or corneal dystrophy.
Subsequently, the child was lost to follow-up until 1991 when he presented with diminution of vision in BE. The best spectacle-corrected visual acuity (BSCVA) at this time was unchanged in the RE and reduced to 20/80 in the LE. In addition to previous findings, white, dot-like opacities were noted in the central cornea in the RE. The intervening areas were clear and the limbus was spared. The features were typical of GCD [Fig. 1]. The LE showed increased scarring and Vogt's striae without these opacities. PKP was advised; however, the boy was again lost to follow-up. Subsequently, he visited our institute in 1995 with complaints of blurred vision. The visual acuity was stable. The RE corneal findings were unchanged while the LE showed increased scarring secondary to an episode of hydrops with multiple granular white dots in the superficial and mid stroma with clear areas in between, sparing the limbus [Fig. 2].
Figure 1.
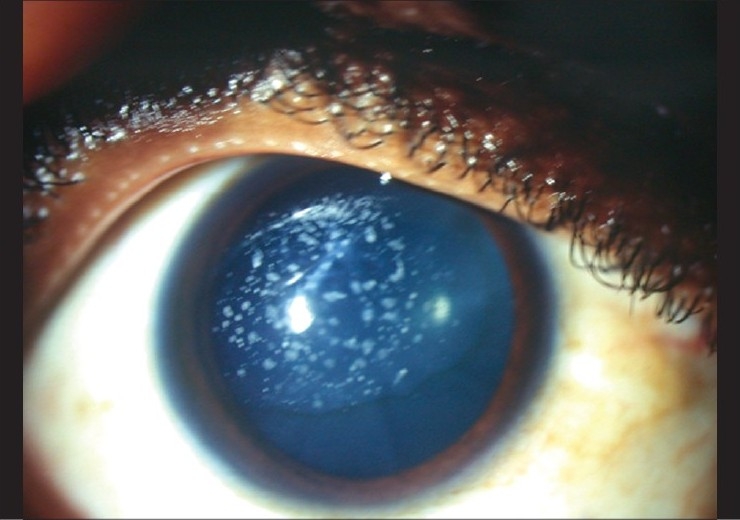
Right eye – the diffuse photomicrograph shows the Fleischer's ring and multiple flakes in the central cornea within the cone with clear areas in between and limbus is spared. This photograph was taken at the age of 17 years
Figure 2.
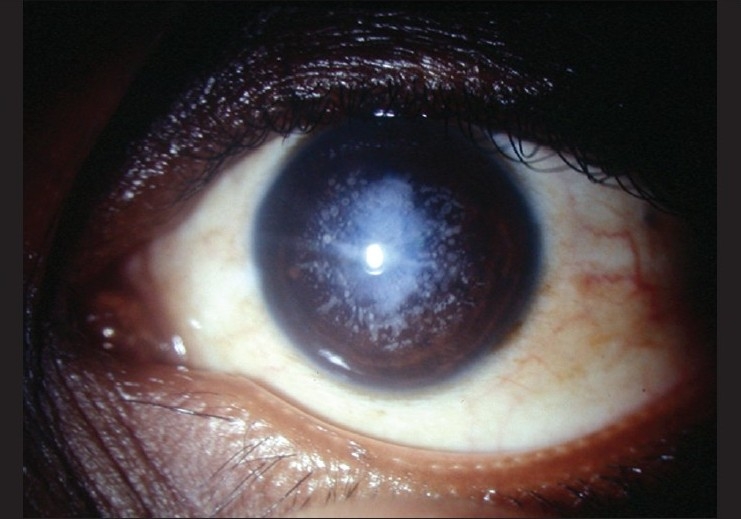
The flakes typical of granular corneal dystrophy as seen in the left eye of the patient with a dense scar posthydrops. This photograph was taken at the age of 21 years
Keratometry (Bausch and Lomb) readings were: RE: >52D, LE 52D @ 180, 50D @ 90°. At the age of 21 years, i.e., in 1996, PKP was done in the RE. The postoperative course in this eye was uneventful till the follow-up in 2002. Intraocular pressure was normal, at 16 mmHg. The sutures were removed intermittently depending on the amount of astigmatism and loose sutures, if any, under the cover of topical corticosteroids and antibiotics. BSCVA in the RE was 20/25 with a –1.50 DS/–3.00 D Cyl at 100. The lens was clear in BE. As vision in the LE dropped further, PKP was done for the LE in 2002. There was a wound leak on the first postoperative day, so resuturing was done. He was lost to follow-up 1 month after PKP, and presented 7 years later with complaints of blurring of vision of 4 months’ duration. BSCVA was 20/30 in the RE with a –5.75 D Cyl at 125° and 20/40 with a –0.25 DS/–5.00D Cyl at 120° in the LE. The RE graft showed the presence of anterior stromal flakes with clear areas in between [Fig. 3]. There were a few buried sutures. The LE graft was clear. Intraocular pressures were 15 and 8 mmHg in RE and LE, respectively. Lens in the RE was clear, while the LE lens showed posterior subcapsular cataract. Fundus examination was within normal limits. A diagnosis of recurrence of GCD in the RE graft was made.
Figure 3.
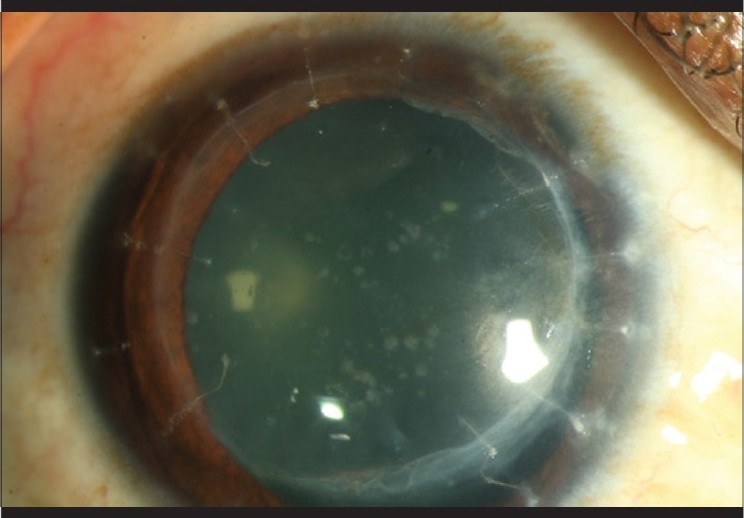
The flakes can be seen in the center of the graft with clear areas in between suggestive of the recurrence of granular corneal dystrophy. Note the buried sutures
Histopathology and mutational analysis
Histologic studies of the corneal button confirmed the presence of patchy granular deposits which stained bright red with Masson's trichrome [Fig. 4a]. On staining with Perl's stain, intracytoplasmic bluish staining was seen in the basal cells, a characteristic feature of keratoconus [Fig. 4b]. Analysis of the patient's leukocyte DNA for mutation in the transforming growth factor-beta-induced (TGFBI/BIGH-3) gene showed a heterozygous mutation corresponding to a change of Arg555Trp (arginine-555 to tryptophan) in the keratoepithelin protein. Genomic DNA was isolated from blood leukocytes using the standard procedure. Individual exons of the TGFBI gene were amplified with primers designed by us, specific to flanking intron sequences. Polymerase chain reaction (PCR) products were screened using single-strand confirmation polymorphism followed by sequencing. This patient was involved in a previous genetic study on dystrophies in Indians. This mutation is characteristic of GCD type I in different populations across the world including Indians.[7,8]
Figure 4.
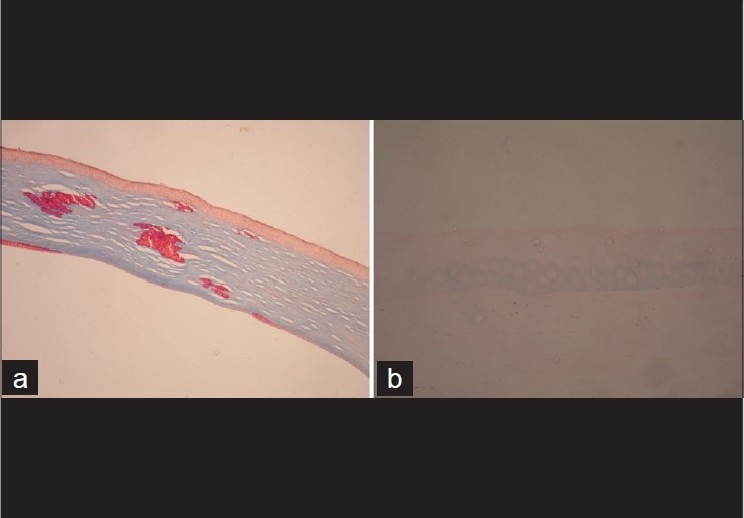
(a) Section of the cornea shows bright-red crystalline deposits in the stroma characteristic of granular dystrophy. (b) The basal cells show intracytoplasmic Prussian blue reaction with Perl's stain, confirming the presence of iron deposits, a characteristic feature of keratoconus
Discussion
The co-occurrence of keratoconus and corneal dystrophy though rare has been reported in the literature.[2–5] Our case is unique in that it documents the long-term (two-decade) follow-up, starting with the diagnosis of keratoconus followed by asymmetric presentation of GCD with recurrence after PKP. Wollensak et al. had reported that incidence of keratoconus conjointly with GCD may be higher with GCD as a presenting diagnosis, since it is difficult to diagnose keratoconus in early stages especially when it is associated with other diseases.[4] In contrast, our case presented first with features of keratoconus and subsequently with clinical features of GCD. Patients who had combined GCD and keratoconus are reported to be between 15 and 21 years of age.[3,4] Our case presented with keratoconus at the age of 13 and with GCD at the age of 17, with asymmetric presentation. The diagnosis of coexisting keratoconus with dystrophy is very important as visual acuity can be improved with RGP lenses. While coexistence has been reported, this particular chronology with a long follow-up is reported by us for the first time. If the patient presents at a stage when both keratoconus and GCD coexist, the management would be PKP or deep anterior lamellar keratoplasty, but if only a single diagnosis of granular corneal dystrophy is made and if the opacities are superficial, then the patient is likely to undergo phototherapeutic keratectomy (PTK). Though GCD is slow to recur and PTK can be repeated without the risk of ectasia, one should rule out keratoconus before proceeding with PTK in eyes with GCD if visual acuity is unexplained by corneal findings. Performing corneal topography or a trial with a rigid contact lens may help rule out keratoconus. In summary, we present a rare case of a patient with keratoconus who on long-term follow-up showed features of GCD and subsequently underwent penetrating keratoplasty.
Acknowledgments
We are grateful to Ms. Banu for her support.
References
- 1.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Sassani JW, Smith SG, Rabinowitz YS. Keratoconus and bilateral lattice-granular corneal dystrophies. Cornea. 1992;11:343–50. doi: 10.1097/00003226-199207000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Vajpayee RB, Snibson GR, Taylor HR. Association of keratoconus with granular corneal dystrophy. Aust N Z J Ophthalmol. 1996;24:369–71. doi: 10.1111/j.1442-9071.1996.tb01610.x. [DOI] [PubMed] [Google Scholar]
- 4.Wollensak G, Green WR, Temprano J. Keratoconus associated with corneal granular dystrophy in a patient of Italian origin. Cornea. 2002;21:121–2. doi: 10.1097/00003226-200201000-00026. [DOI] [PubMed] [Google Scholar]
- 5.Cremona FA, Ghoshesh FR, Rapuano CJ, Eagle RC, Jr, Hammersmith KM, Laibson PR, et al. Keratoconus associated with other corneal dystrophies. Cornea. 2009;28:127–35. doi: 10.1097/ICO.0b013e3181859935. [DOI] [PubMed] [Google Scholar]
- 6.Igarashi S, Makita Y, Hikichi T, Mori F, Hanada K, Yoshida A. Association of keratoconus and Avellino corneal dystrophy. Br J Ophthalmol. 2003;87:367–8. doi: 10.1136/bjo.87.3.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Munier FL, Korvatska E, Djemaï A, Le Paslier D, Zografos L, Pescia G, et al. Kerato-epithelin mutations in four 5q31-linked corneal dystrophies. Nat Genet. 1997;15:247–51. doi: 10.1038/ng0397-247. [DOI] [PubMed] [Google Scholar]
- 8.Chakravarthi SV, Kannabiran C, Sridhar MS, Vemuganti GK. TGFBI gene mutations causing lattice and granular corneal dystrophies in Indian patients. Invest Ophthalmol Vis Sci. 2005;46:121–5. doi: 10.1167/iovs.04-0440. [DOI] [PubMed] [Google Scholar]


