Abstract
Background:
Trigeminal neuralgia typically involves nerves supplying teeth, jaws and face of older females. Though the etiology is usually obscure, different treatment modalities have been tried for it viz. medicinal treatment, injection alcohol, peripheral neurectomy, rhizotomy, and microvascular decompression etc. Transcutaneous electric nerve stimulation (TENS) is an emerging and promising option for management of such patients.
Aims and Design:
The present study was designed with an aim to study the efficacy of TENS in management of trigeminal neuralgia.
Materials and Methods:
The study was conducted on 30 patients of trigeminal neuralgia confirmed by diagnostic nerve block. They were given bursts of TENS for 20-40 days over the path of the affected nerve and subsequently evaluated at 1 month and 3 month intervals by visual analogue scale (VAS), verbal pain scale (VPS), a functional outcome scales for main daily activities like sleep, chewing, talking, or washing face.
Results:
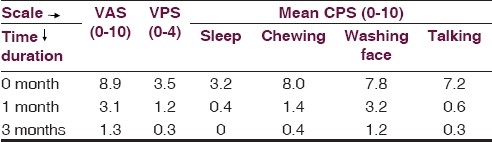
The results showed that, on VAS, the score decreased from 8.9 (Pre TENS) to 3.1 at 1 month and 1.3 at 3 months, and on VPS, the score decreased from 3.5 (Pre TENS) to 1.2 at 1 month and 0.3 at 3 months. Similarly, a considerable decrease in scores was seen on functional outcome scale for different activities. No side effects like irritation or redness of skin were seen in any of the patients.
Conclusions:
Thus, TENS was found to be a safe, easily acceptable, and non-invasive outdoor patient department procedure for management of trigeminal neuralgia.
Keywords: Trigeminal neuralgia, transcutaneous electric nerve stimulation, visual analogue scale
Introduction
Trigeminal neuralgia, also known as Tic Douloureux, Trifacial neuralgia, or Fothergill's disease typically involves the nerves supplying teeth, jaws, face and associated structures. Its etiology is as much a mystery today as it has been for several centuries. Periodontal diseases, traumatogenic occlusion, degeneration of nerves of deciduous teeth, circulatory insufficiency of trigeminal ganglion, multiple sclerosis, pressure of dilated and tortuous arteries in vicinity of trigeminal ganglion or age related brain sagging have been blamed from time to time as causative factors.[1,2]
The diseases, typically involves older females aged >35 years and usually involves right half of the face. It is typically characterized by excruciating paroxysms of pain in the lips, gums, cheeks, or chin and rarely in distribution of ophthalmic division of the 5th nerve. The pain seldom lasts for a few seconds or a minute, but may be so intense, stabbing or lancinating that the patient winces, hence the term ‘tic’. However, the spasmodic contraction of facial muscles is not seen. The paroxysms tend to recur frequently, both during day and night. The early pain has been termed “Pretrigeminal neuralgia” by Mitchell[3] and described as dull aching or burning or resembling a toothache. The later pain may be so severe that many sufferers have attempted suicide to put an end to their torment. Another characteristic feature is the trigger zones which precipitate an attack when touched. These are common on vermilion border of lips, alae of nose, cheeks, around the eyes and tongue. Any touch or movement of these parts like washing or shaving of face, brushing the teeth exposure to a draft of air or simply an act of eating or smiling may precipitate the pain.
Many treatment modalities have been described for trigeminal neuralgia from time to time. These include drug therapy (carbamazepine, phenytoin, baclofen, gabapantane),[2] peripheral techniques viz injection of alcohol,[4,5] phenol, streptomycin and lignocaine,[6] neurectomies,[7] peripheral radio frequency thermolysis,[8] and removal of jaw cavities.[9] Neurosurgery includes radiofrequency thermocoagulation of trigeminal ganglion,[10] glycerol injections,[11] posterior fossa surgery, either microvascular decompression[12] or partial rhizotomy.[13] Other methods tried are cryoanalgesia,[14] Gamma knife radiosurgery, cyber knife radiosurgery, transcranial magnetic stimulation over motor cortex, and deep brain stimulation.[15] All of these have their own positive and negative aspects. An ideal treatment is the one that causes no morbidity and preserves the normal sensation of the face. Such a sensation preserving absolutely safe and permanently successful treatment does not yet exist. Transcutaneous electric stimulation of trigeminal nerve is an emerging and promising option for treatment of trigeminal neuralgia. By definition, any stimulating device which delivers electric currents across the intact surface of the skin is TENS. Since it is non-invasive, least expensive, and safe technique with minimal morbidity, it may prove to be an excellent option for trigeminal neuralgia.
Materials and Methods
The present study was conducted on a total of 30 patients of trigeminal neuralgia who came to the department of Oral and Maxillofacial Surgery of this institute between the periods January 2010-December 2010. They were diagnosed by the classical display of paroxysmal pain viz. stabbing character lasting for seconds to minutes, rapidly provokable by gentle stimulation over trigger zone, confinement to distribution of branches of trigeminal nerve, being strictly unilateral at a particular paroxysm and without any sensory or motor loss in the affected region. The diagnosis was further confirmed by a diagnostic nerve block with 2% lignocaine which gave a complete relief to the symptoms.
They were treated with transcutaneous electric stimulation of the affected nerve. The patients on medicinal treatment, showing intolerance to drugs and patients with recurrent pain after neurectomy or peripheral alcohol injection were included. However, the pain due to other odontogenic causes or related to other specialities’ like of otolaryngology, neurology, ophthalmology or psychiatry; patients with cardiac pacemakers and pregnancy were excluded.
These patients were given continuous bursts of current for 20 minutes daily for 20-40 days over the path of the affected nerve with a portable transcutaneous electric nerve stimulation machine by Waves technologic, New Delhi. Out of the two electrodes, one was applied to the cutaneous area of the distribution of the affected nerve and other was applied to temple to complete the circuit. Pre TENS doses of carbamazepine were tapered off in the next 2-3 weeks. Patients were subsequently evaluated at 1 month and 3 months intervals for pain by visual analogue scale (VAS) (0-10), verbal pain scale (VPS) (0-4), category point scale (CPS) or functional outcome scale for main daily activities viz. sleep, chewing, talking or washing face (0-10 for each activity).
After the specific management, they were followed up till December 2010. The results were recorded on a predesigned proforma. They were scrutinized, tabulated, and analyzed and are being reported here.
Results
The study was conducted on 30 patients (M:F = 12:18), all more than 50 years of age. Majority of patients had involvement of inferior alveolar nerve followed by infraorbital nerve [Table 1]. The results of the various methods of pain evaluation are shown in Table 2 which depicts extremely promising results as indicated by a decrease in all the scores of the different scales, both at 1 month and 3 months post TENS. No side effects like irritation or redness of the skin were seen in any of the patients. It indicates the efficacy of this safe and non invasive technique in the management of trigeminal neuralgia. However, a longer follow up of patients is still required.
Table 1.
Incidence of different nerves involved
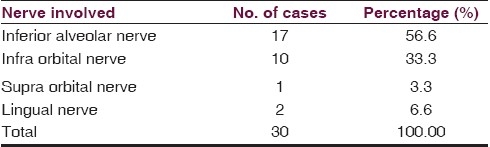
Table 2.
Mean scores of different scales at intervals of 0, 1, and 3 months
Discussion
Wall and Sweet[16] were pioneers to promote the use of TENS for the treatment of chronic pain. Later on, it was successfully used for the pain of knee osteoarthritis, rib fractures, phantom limb pain, neuropathic pain syndromes etc. Oncel et al.,[17] found TENS more effective than non-steroidal anti-inflammatory drugs (NSAIDS) or placebo in patients with uncomplicated minor rib fractures. Fong et al.,[18] advocated that the use of TENS could decrease the use of pethidine for first stage analgesia.
The analgesic mechanism of TENS involves gate control theory, physiological block, and endogenous pain inhibitory systems:
Gate control theory: According to this theory, substantia gelatinosa of spinal cord acts as a gate control system. Activation of large myelinating fibres subserving touch, pressure, vibration is thought to facilitate pre synaptic inhibition of substantia gelatinosa cells in the dorsal horn, thus, reducing pain transmission.[19]
As the frequency of stimulation increases, conduction decreases resulting in physiological block.
Basbaum and Field[20] proposed that there is a neural network including midbrain, medulla and spinal cord levels that monitors and modulates the activity of pain transmitting neurons. Woolf et al.,[21] demonstrated that peripheral electrical stimulation could also excite naloxone dependent anti nociceptive mechanisms, i.e., endogenous opioid systems operating both at spinal and supraspinal levels.
Advavtages of TENS
No Prostaglandins inhibition, since TENS controls pain by gate control mechanism.
Rapid and timely inhibition of pain at peak progression.
No adverse effects of drugs
Non invasive
Short term treatment for 20-40 days as compared with long term medicinal treatment.
No need for surgical intervention.
Doesn’t need much expertise.
Can be used at home with portable machine.
Equally effective in post neurectomy and post injection alcohol neuralgia.
Summary and Conclusions
TENS should be considered as safe, simple, and reusable first line of treatment for many pain conditions including trigeminal neuralgia, specially, in a rural set up where technical expertise for surgical treatment is lacking and in patients in whom there are seen adverse drug reactions or they are not willing to take medicinal treatment, or cannot afford expensive surgical intervention.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Shafer WG, Hine MK, Levy BM. A textbook of oral pathology. 4th Ed. Philadelphia: W.B. Saunders Co; 1983. Diseases of the nerves and muscles; pp. 854–6. [Google Scholar]
- 2.Beal MF, Hauser SL. Trigeminal neuralgia, bell's palsy and other cranial nerve disorder. In: Fauci AS, Brownwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, et al., editors. Harrisons's Principles of Internal Medicine. 17th ed. Vol. 2. New York: McGraw Hill Co; 2008. pp. 2583–4. [Google Scholar]
- 3.Mitchell RG. Pretrigeminal neuralgia. Br Dent J. 1980;149:167. doi: 10.1038/sj.bdj.4804480. [DOI] [PubMed] [Google Scholar]
- 4.Grant FC. Alcohol injction in the treatment of major trigeminal neuralgia. J Am Med Assoc. 1936;107:771. [Google Scholar]
- 5.Horrax G, Poppen JL. Trigeminal neuralgia. Experience with, and treatment employed in 468 patients during the past 10 years. Surg Gynaecol Obstet. 1935;61:394. [Google Scholar]
- 6.Sokolovic M, Todorovic L, Stajcic ZN, Petrovic J. Peripheral streptomycin/lidocaine injections in the treatment of idiopathic trigeminal neuralgia. J Maxillofacial Surg. 1986;14:8. doi: 10.1016/s0301-0503(86)80249-1. [DOI] [PubMed] [Google Scholar]
- 7.Grantham EG, Segerberg LH. An evaluation of palliative surgical procedures in trigeminal neuralgia. J Neurosurg. 1952;9:390. doi: 10.3171/jns.1952.9.4.0390. [DOI] [PubMed] [Google Scholar]
- 8.Gregg JM, Small EW. Surgical management of trigeminal pain with radiofrequency lesions of peripheral nerves. J Oral Maxillofacial Surg. 1986;44:122. doi: 10.1016/0278-2391(86)90194-1. [DOI] [PubMed] [Google Scholar]
- 9.Ratner EJ, Pearson P, Kleinman DJ, Shklar G, Socransky SS. Jawbone cavities and trigeminal neuralgia and atypical facial neuralgia. Oral Surg. 1979;48:3. doi: 10.1016/0030-4220(79)90229-9. [DOI] [PubMed] [Google Scholar]
- 10.Mittal B, Thomas DG. Controlled thermocoagulation in trigeminal neuralgia. J Neurol Neurosurg Psych. 1986;49:932. doi: 10.1136/jnnp.49.8.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lunsford LD, Bennett MH. Percutaneous retrogasserian glycerol rhizotomy for tic douloureux: Part 1. Neurosurg. 1984;14:424. doi: 10.1227/00006123-198404000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Jannetta PJ. Microsurgical approach to the trigeminal nerve for tic douloureux. Prog Neurol Surg. 1976;7:180. [Google Scholar]
- 13.Piatt JH, Jr, Wilkins RH. Treatment of tic douloureux and hemifacial spasm by posterior fossa exploration: Threrapeutic implications of the various neurovascular relationships. Neurosurgery. 1984;14:462–71. doi: 10.1227/00006123-198404000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Lloyd JW, Barnard JD, Glynn CJ. Cryoanalgesia: A new approach to the pain relief. Lancet. 1976;2:932. doi: 10.1016/s0140-6736(76)90893-x. [DOI] [PubMed] [Google Scholar]
- 15.Toda K. Operative treatment of trigeminal neuralgia: Review of current techniques. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:788–805. doi: 10.1016/j.tripleo.2008.05.033. [DOI] [PubMed] [Google Scholar]
- 16.Wall PD, Sweet WH. Temporary abolition of pain in man. Science. 1967;155:108–9. doi: 10.1126/science.155.3758.108. [DOI] [PubMed] [Google Scholar]
- 17.Oncel M, Sencan S, Yildiz H, Kurt N. Transcutaneous electric nerve stimulation for pain management in patients with uncomplicated minor rib fractures. Eur J Cardiothorac Surg. 2002;22:13–7. doi: 10.1016/s1010-7940(02)00206-3. [DOI] [PubMed] [Google Scholar]
- 18.Fong LH, Irene LY, Grace GY. A Pilot study on the use of transcutaneous Electric Nerve stimulation Machine for First-stage Analgesiain a teaching Hospital. Hongkong J Gynae Obstet Med. 2008;8:9–12. [Google Scholar]
- 19.Melzack R, Wall PD. Pain mechanisms: A new Theory. Science. 1965;150:971–8. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- 20.Basbaum AI, Fields HL. Endogenous pain control mechanisms: Review and hypothesis. Annu Rev Neurosci. 1984;7:309–38. doi: 10.1146/annurev.ne.07.030184.001521. [DOI] [PubMed] [Google Scholar]
- 21.Woolf CJ, Mitchell D, Barrett GD. Antinociceptive effect of peripheral segmental electrical stimulation in the rat. Pain. 1980;8:237–52. doi: 10.1016/0304-3959(88)90011-5. [DOI] [PubMed] [Google Scholar]


