Abstract
Although anxiety is one of the most prominent psychiatric complaints of methamphetamine (MA) users, little is known about the association between anxiety disorders and treatment outcomes in this population. Using data from 526 adults in the largest psychosocial clinical trial of MA users conducted to date, this study examined psychiatric, substance use, and functional outcomes of MA users with concomitant anxiety disorders 3 years after treatment. Anxiety disorders were associated with poorer alcohol and drug use outcomes, increased health service utilization, and higher levels of psychiatric symptomatology, including suicidality. Addressing anxiety symptoms and syndromes in MA users may be helpful as a means of optimizing treatment outcomes.
Anxiety is one of the most common psychiatric symptoms reported among methamphetamine (MA) users.1,2 Anxiety symptoms commonly emerge both during MA intoxication3 and withdrawal,4 although the extent to which such symptoms persist following cessation of MA use remains largely unknown. The observation of anxiety symptomatology in this population may be explained, in part, by activation of the sympathetic nervous system via alpha receptor stimulation, a putative MA-specific mechanism.3 Although prevalence rates of anxiety have not been well studied in MA using populations, a few investigations established that over three quarters of amphetamine users5 and nearly 40% of treatment-seeking MA users6 reported anxiety symptoms and a history of anxiety disorders, respectively. Likewise, significant rates of anxiety-stimulant use disorder comorbidity were demonstrated in a recent national epidemiological study, in which 39% of individuals with amphetamine use disorders were found to have a lifetime history of anxiety disorders.7
Although relatively few studies have documented the clinical course of MA users with concomitant psychiatric illness, prior work in alcohol and opiate users suggests that psychiatric and substance use disorder comorbidity worsens clinical prognosis and treatment outcomes.8,9,10 In stimulant users, diagnosis-specific studies are limited but have yielded mixed findings regarding the association between psychiatric disorders and treatment outcomes, with some studies suggesting poorer post-treatment substance use outcomes in subjects with psychiatric diagnoses relative to those without concomitant psychiatric illness11,12 and others demonstrating no significant difference in post-treatment substance use between individuals with and without psychiatric diagnoses.13,14 To date, little is known about the effects of anxiety disorders in particular on functional impairment or post-treatment health, psychiatric, or substance use outcomes in MA users.
In a recent study of MA-dependent adults three years after treatment, the presence of psychiatric illness was associated with poorer treatment and functional outcomes.12 More than one quarter of subjects met criteria for a current anxiety disorder, and anxiety disorders were associated with poorer MA use outcomes at 3-year follow-up. In this same cohort of MA users, the purpose of the current investigation was to characterize the relationship of anxiety disorders with post-treatment substance use frequency and diagnoses as well as health and functional outcomes. We hypothesized that the presence of an anxiety disorder would be associated with greater psychiatric, medical and functional impairment relative to MA users without anxiety disorders and that concomitant anxiety would be associated with poorer alcohol and other substance use outcomes.
Methods
Participants
The present study included 526 MA dependent adults who participated in the Methamphetamine Treatment Project (MTP), a randomized, controlled trial of psychosocial treatments for MA dependence described elsewhere.15 MTP participants were treatment-seeking, MA dependent adults (age 18 or over) recruited upon entry to outpatient drug treatment programs ranging from 8 to 16 weeks in duration in California, Montana, and Hawaii. To be included in the study, participants were required to meet DSM-IV criteria for MA dependence, be current MA users (having used MA within one month prior to treatment admission unless in a constrained environment, e.g., jail), a resident of the same geographic area as the treatment facility, English language proficient, and able to provide informed consent. Individuals were excluded if they: exhibited medical or psychiatric impairment that warranted hospitalization or other primary treatment, required medical detoxification from any substance of abuse, had been enrolled in another treatment program within the past 30 days; and/or had medical, legal, housing, or transportation problems precluding their safety or ability to participate in treatment. Although the inclusion and exclusion criteria may have restricted the range of functional disability in the sample, participant characteristics were consistent with stimulant using cohorts previously studied in psychosocial clinical trials.15, 16
The follow-up interview was completed an average of 3.1 years after treatment completion (SD=0.48) and consisted of a medical examination, a psychiatric diagnostic interview, a psychosocial interview, and administration of self-report questionnaires. Of the 587 participants who were interviewed for the follow-up study, 61 did not complete the psychiatric diagnostic component of the interview for various reasons, including: having moved out of the area, constraints due to incarceration, inability to schedule a convenient appointment, and/or declining this portion of the assessment. Thus, the final sample included 526 participants. After providing a complete description of the study to the subjects, informed consent was obtained. All procedures were performed in accord with the standards of the Committee of Human Experimentation of UCLA.
Procedures
Trained interviewers conducted face-to-face assessments with participants at baseline, treatment discharge, and approximately 3 years after discharge. The Addiction Severity Index (ASI) 17 was administered at all assessments and provided composite scores in seven functional domains (alcohol, drug, psychiatric, medical, legal, family, employment).
The Life Experience Timeline interview (LET),18 a measure adapted from the Natural History Interview19 was used to quantify MA use in the follow-up period. Using the LET, substance use history is gathered using a month-by-month timeline approach that links substance use to important life events.
At 3-year follow-up, The Mini-International Neuropsychiatric Interview (MINI),20 a brief structured diagnostic interview for assessing DSM-IV and ICD-10 psychiatric disorders was administered to provide anxiety, alcohol, and other substance use disorder diagnostic information. All interviewers were trained to criterion on the MINI using standardized procedures including didactic instruction, practice interviews, and direct observation.
Statistical Analysis
For all statistical tests, alpha was set at the 0.05 level. Primary outcome measures included treatment adherence and frequency of MA use during follow-up. Treatment adherence was a continuous variable indicating the number of weeks of scheduled treatment during which the participant attended.
Mixed model repeated measures analyses with main effects of time and anxiety disorder diagnosis and the interaction among these variables were used to compare ASI scores for those with and without anxiety disorders across baseline, treatment-end and 3-year follow-up.
Results
The original MTP sample (N=1016) was compared with the subset of participants who were included in the current investigation (N=526) by using t-tests and chi-square tests for age, education, gender, marital status, route of MA administration, employment, and baseline ASI composite scores. In all analyses, there were no significant differences between the patients in the current study and the original MTP sample.
Demographic characteristics of the original MTP sample are described elsewhere.1,16 At 3-year follow-up, the sample was 68% Caucasian, 2% African American, 12% Asian, and 14% Hispanic, with an average age of 36.2 (SD=8.0); 76% completed high school and 4% had college education and/or beyond. More than half (60%) of the participants were female. Regarding employment, 60% were working full-or part-time and 32% were unemployed; 4% were students, 2% were retired and 2% were in a controlled environment. Forty-seven percent were never married, 37% were divorced or separated, and 16% were married. At the baseline (i.e., pretreatment) assessment, participants reported using MA an average of 12 days out of the past 30 (SD=9.6). The preferred route of administration was smoking (62%), followed by i.v.-injecting (28%) and intranasal use (10%). There were no differences in demographic or substance use characteristics among those who completed the psychiatric assessment (n=526) relative to those who did not (n=61).
Participants with current (23.4%; N=123) and past (8.1%; N=43) anxiety disorders were compared on age, education, gender, marital status, route of MA administration, employment, and baseline MA use frequency and ASI composite scores. For each analysis, there were no significant differences between the patients with current and past anxiety disorders. Thus, current and past anxiety disorders were collapsed to form a single category indicating the presence of any anxiety disorder.
Of the 526 participants, 26.2% (N=138) met criteria for a current or past anxiety disorder at 3-year follow-up. The most common current disorder reported was Generalized Anxiety Disorder (12.3%; n=65), followed by Social Anxiety Disorder (8.5%; n=45), Post-Traumatic Stress Disorder (5.8%; n=31), Panic Disorder (2.6%; n=14), and Agoraphobia (2.6%; n=14). Self-reported MA use frequency during the follow-up period was significantly higher among those with (M=16.4 months, SD=1.2) versus without (M=13.3 months, SD=0.7) anxiety disorders. Likewise, participants with an anxiety disorder evidenced poorer treatment adherence relative to those without this diagnosis in terms of the number of scheduled weeks of treatment attended (M=6.25 vs. M=7.60, t=2.29, df=524, p=0.02), and were significantly more likely to meet criteria for alcohol- (OR=1.8, 95% C.I., 1.1–2.9) and other substance dependence (OR=2.2, 95% C.I., 1.5–3.3) at 3-year follow-up..
Those with an anxiety disorder had significantly greater odds of having been hospitalized within the 12 months prior to the 3-year follow-up interview relative to those without this diagnosis (Odds Ratio [OR]==1.8, 95% Confidence Interval [C.I.], 1.1–3.4) and had more than triple the odds of having attempted suicide once or more in their lifetime (OR=3.1, 95% C.I., 2.1–4.7).
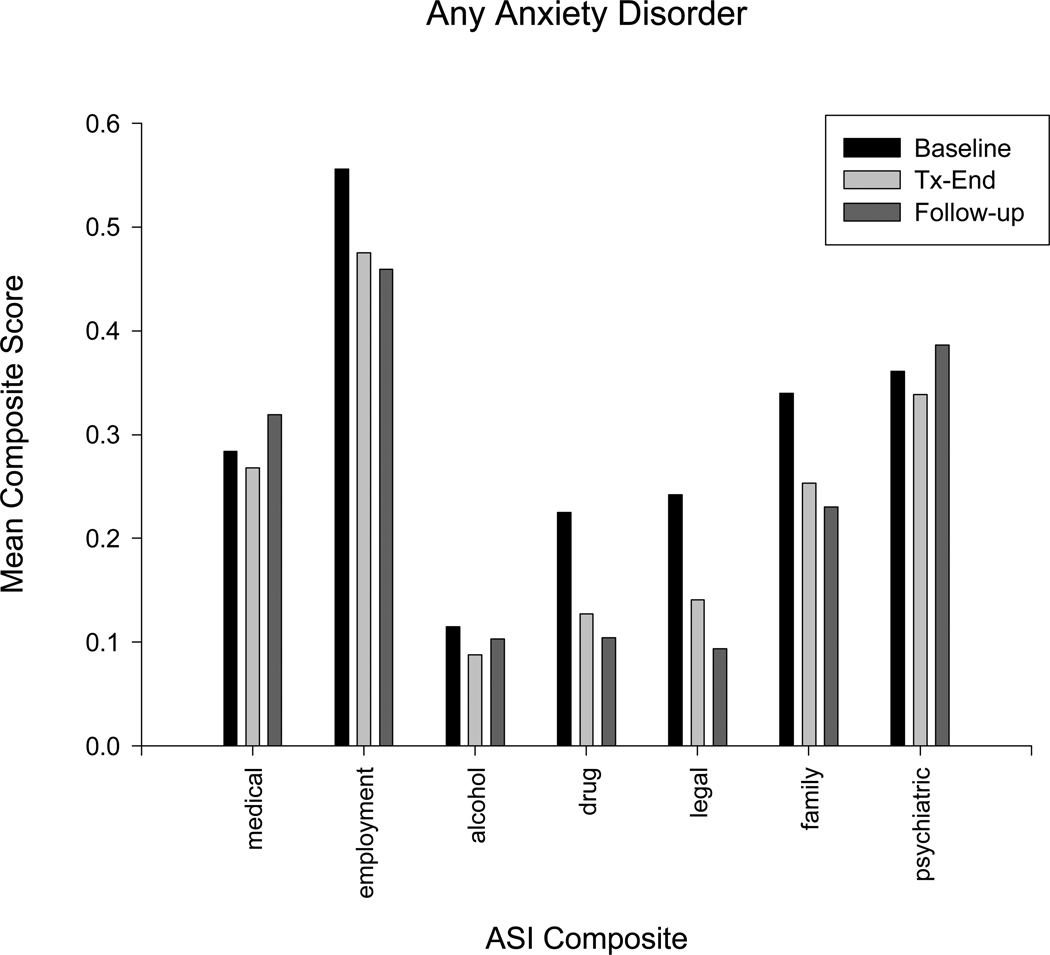
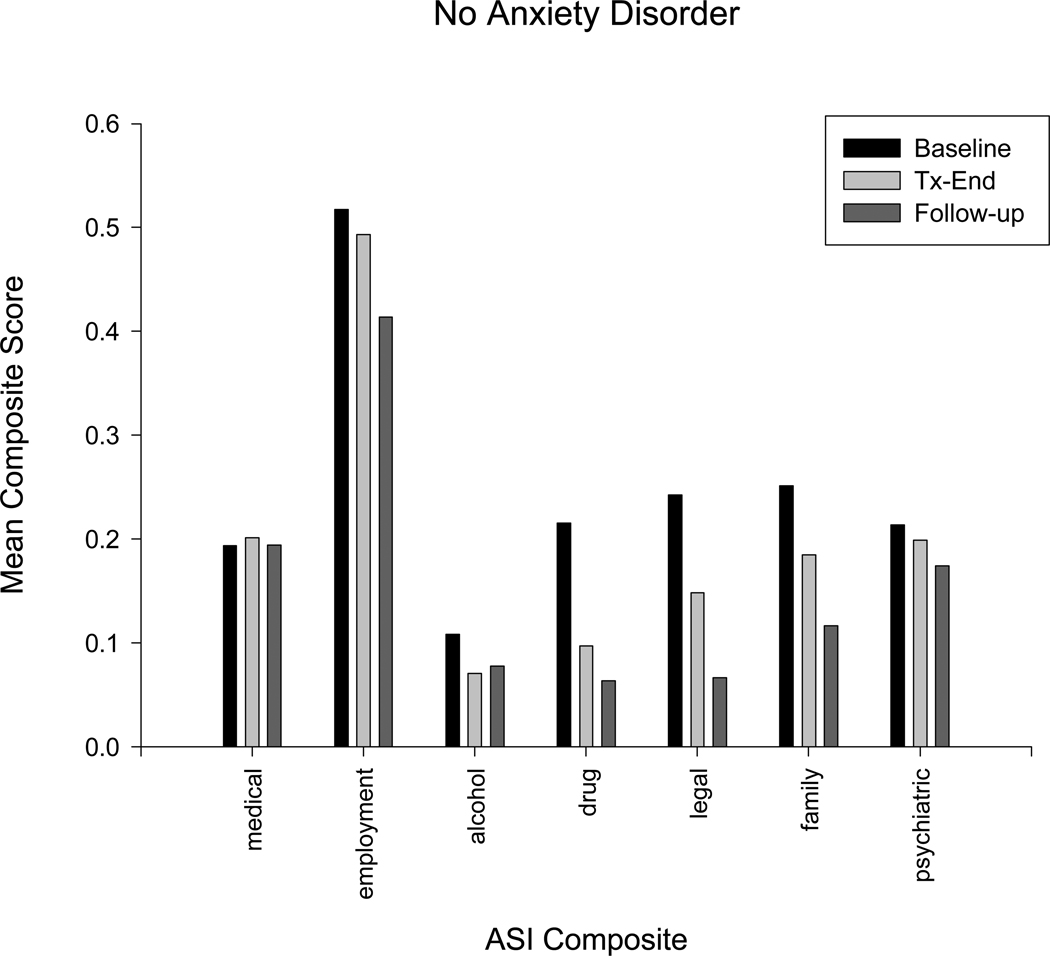
ASI composite scores at baseline, discharge and follow-up for those with and without anxiety disorders are plotted in Figures 1 and 2, respectively, and the results of mixed model linear regressions testing the effects of time, anxiety disorder diagnosis, and their interaction on ASI scores are provided in Table 1. Controlling for demographics, pre-treatment MA use frequency and route of MA administration, these analyses revealed a main effect of anxiety disorder on the family and medical severity composites, indicating higher levels of impairment on these indices overall among those with an anxiety disorder, and a significant time×diagnosis interaction on two of the remaining five ASI composites (drug and psychiatric). These interactions indicated that the group with an anxiety disorder diagnosis reported problems of significantly greater severity over time in these areas.
Figure 1.
Mean Addiction Severity Index (ASI) scale scores as a function of time among MA dependent adults with anxiety disorders at 3-year follow-up (N=138).
Figure 2.
Mean Addiction Severity Index (ASI) scale scores as a function of time among MA dependent adults without anxiety disorders at 3-year follow-up (N=388).
Table 1.
Changes in psychosocial, psychiatric, and substance-related impairment among MA dependent adults at 3-year follow-up: linear mixed-effects models
| Scale | Anxiety Diagnosis |
Time |
Anxiety Diagnosis × Time |
|||
|---|---|---|---|---|---|---|
| β | p | β | p | β | p | |
| Addiction Severity Index | ||||||
| Psychiatric Composite | 0.11 | <0.001 | −0.01 | <0.001 | 0.01 | 0.03 |
| Medical Composite | 0.08 | <0.001 | 0.00 | 0.51 | 0.00 | 0.59 |
| Employment Composite | 0.00 | 0.88 | −0.02 | <0.001 | 0.00 | 0.46 |
| Alcohol Composite | 0.01 | 0.59 | −0.01 | <0.001 | 0.00 | 0.23 |
| Drug Composite | 0.01 | 0.42 | −0.03 | <0.001 | 0.01 | 0.02 |
| Legal Composite | −0.01 | 0.80 | −0.04 | <0.001 | 0.01 | 0.12 |
| Family Composite | 0.06 | <0.01 | −0.03 | <0.001 | 0.00 | 0.83 |
Discussion
This is the first study to examine the relationship between anxiety disorders and both substance use and functional outcomes in MA-dependent adults. In this study, comorbid anxiety disorders were observed in more than one-quarter of MA users, a prevalence rate higher than those reported in both the general population21 and in other stimulant users.22,23 Though findings are consistent with prior literature demonstrating the elevated frequency of anxiety symptoms, relative to other psychiatric complaints in MA users,1 the prevalence rates of anxiety disorders and clinical course of MA users with such comorbidity have not been well-studied to date.
Although the prognostic implications of comorbid psychiatric illness on substance use outcomes have been inconsistent in prior studies,24, 25 results of the present investigation are consistent with that of a series of recent studies of MA users from this same cohort with concomitant affective disorders,26 in demonstrating that those with coexisting anxiety disorders evidenced more frequent MA use after treatment. Moreover, those with anxiety comorbidity evidenced greater likelihood of meeting criteria for alcohol and other substance use disorders at 3-year follow-up relative to participants without anxiety disorders. Nevertheless, given that diagnostic criteria for these disorders were only assessed at a single time point, coupled with the absence of data from the diagnostic instrument used to establish the independence of anxiety symptomatology from substance use, the causal relationships between anxiety and SUDs could not be fully elucidated. Thus, whether participants were at greater risk for alcohol and substance use disorders as a result of their anxiety disorder or vice versa remains unclear and is an important area for future research.
Consistent with extant literature demonstrating impairments in functional outcomes associated with psychiatric-SUD comorbidity,27 MA users with anxiety disorders evidenced poorer post-treatment functioning across multiple domains relative to those without anxiety disorders, with greater overall medical and family problem severity and a declining course of illness over time in drug- and psychiatric-related problem domains. Likewise, individuals with anxiety disorders were more likely to have been hospitalized in the year prior to their follow-up assessment and to have attempted suicide in their lifetime. These findings are consistent with a growing body of literature supporting an association between anxiety symptoms28 and disorders29 and suicidality. Additionally, an association between psychiatric-SUD comorbidity and increased risk of suicide has been demonstrated in prior literature,30,31 and the present study extends previously reported findings in this same cohort of MA-dependent adults in which individuals with a prior history of depression or psychiatric admissions were more likely to have attempted suicide,32 suggesting that anxiety may be an additional risk factor.
This study had several potential limitations. First, the MINI diagnostic interview was performed at a single time point after treatment, thereby limiting the ability to characterize the effects of treatment on anxiety disorders or to fully elucidate the clinical course of anxiety in this population. Second, because the MINI does not distinguish substance-induced from substance-independent disorders, the differential effects of substance-induced versus primary disorders on clinical course and treatment outcomes could not be determined. Lastly, given that participants with severe Axis I disorders warranting inpatient treatment were excluded from this study, the prevalence rates of anxiety disorders were likely underestimated in this study.
Findings from the current investigation underscore the importance of identifying and addressing anxiety disorders among treatment-seeking MA users. These results replicate and extend prior reports demonstrating that anxiety in MA users is a significant and clinically relevant psychiatric concern and provide evidence that co-occurring anxiety disorders in MA users are associated with greater overall impairment, healthcare utilization and poorer treatment adherence and outcomes. As such, addressing psychiatric and substance use disorders concurrently in an integrated fashion may improve outcomes in this population. Further research is warranted to investigate the temporal relationship between anxiety and MA use disorders and to further elucidate the clinical course and prognostic implications of anxiety disorders in MA users.
Acknowledgements
The authors would like to thank the treatment and research staff at the participating community-based center sites, as well as acknowledge the support of the study investigators in each region. The research presented in this paper was supported by NIDA Grant 1K23DA020085 awarded to S. Glasner-Edwards and by the Methamphetamine Abuse Treatment – Special Studies (MAT-SS) contract 270-01-7089 and grants numbers TI 11440–01, TI 11427–01, TI 11425–01, TI 11443–01, TI 11484–01, TI 11441–01, TI 11410–01 and TI 11411–01, provided by the Center for Substance Abuse Treatment (CSAT), Substance Abuse and Mental Health Services Administration (SAMHSA), US Department of Heath and Human Services. The opinions expressed in this publication are solely those of the authors and do not reflect the opinions of the government.
*Methamphetamine Treatment Project Corporate Authors: M. Douglas Anglin, Ph.D., Joseph Balabis, B.A., Richard Bradway, Alison Hamilton Brown, Ph.D., Cynthia Burke, Ph.D., Darrell Christian, Ph.D., Judith Cohen, Ph.D., M.P.H., Florentina Cosmineanu, M.S., Alice Dickow, B.A., Melissa Donaldson, Yvonne Frazier, Thomas E. Freese, Ph.D., Cheryl Gallagher, M.A., Gantt P. Galloway, Pharm.D., Vikas Gulati, B.S., James Herrell, Ph.D., M.P.H., Kathryn Horner, B.A., Alice Huber, Ph.D., Martin Y. Iguchi, Ph.D., Russell H. Lord, Ed.D., Michael J. McCann, M.A., Sam Minsky, M.F.T., Pat Morrisey, M.A., M.F.T., Jeanne Obert, M.F.T., M.S.M., Susan Pennell, M.A., Chris Reiber, Ph.D., M.P.H., Norman Rodrigues, Jr., Janice Stalcup, M.S.N., Dr.P.H., S. Alex Stalcup, M.D., Ewa S. Stamper, Ph.D., Janice Stimson, Psy.D., Sarah Turcotte Manser, M.A., Denna Vandersloot, M.Ed., Ahndrea Weiner, M.S., M.F.T., Kathryn Woodward, B.A., Joan Zweben, Ph.D.
References
- 1.Zweben JE, Cohen JB, Christian D, et al. Psychiatric symptoms in methamphetamine users. Am J Addict. 2004;13(2):181–190. doi: 10.1080/10550490490436055. [DOI] [PubMed] [Google Scholar]
- 2.Darke S, Kaye S, McKetin R, Duflou J. Major physical and psychological harms of methamphetamine use. Drug and Alcohol Review. 2008;27:253–262. doi: 10.1080/09595230801923702. [DOI] [PubMed] [Google Scholar]
- 3.Cruickshank CC, Dyer KR. A review of the clinical pharmacology of methamphetamine. Addiction. 2009;104:1085–1099. doi: 10.1111/j.1360-0443.2009.02564.x. [DOI] [PubMed] [Google Scholar]
- 4.McGregor C, Srisurapanont M, Jittiwutikarn J, Laobhripatr S, Wongtan T, White JM. The nature, time course and severity of methamphetamine withdrawal. Addiction. 2005;100(9):1320–1329. doi: 10.1111/j.1360-0443.2005.01160.x. [DOI] [PubMed] [Google Scholar]
- 5.Hall W, Hando J, Darke S, Ross J. Psychological morbidity and route of administration among amphetamine users in Sydney, Australia. Addiction. 1996;91(1):81–87. doi: 10.1046/j.1360-0443.1996.9118110.x. [DOI] [PubMed] [Google Scholar]
- 6.McKetin R, Ross J, Kelly E, Baker A, Lee N, Lubman DI, Mattick R. Characteristics and harms associated with injecting versus smoking methamphetamine among methamphetamine treatment entrants. Drug Alcohol Rev. 2008;27(3):277–285. doi: 10.1080/09595230801919486. [DOI] [PubMed] [Google Scholar]
- 7.Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67(2):247–257. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- 8.Rounsaville BJ, Kosten TR, Weissman MM, Kleber HD. Prognostic significance of psychopathology in treated opiate addicts. A 2.5-year follow-up study. Arch Gen Psychiatry. 1986;43(8):739–745. doi: 10.1001/archpsyc.1986.01800080025004. [DOI] [PubMed] [Google Scholar]
- 9.Rounsaville BJ, Dolinsky ZS, Babor TF, Meyer RE. Psychopathology as a predictor of treatment outcome in alcoholics. Arch Gen Psychiatry. 1987;44(6):505–513. doi: 10.1001/archpsyc.1987.01800180015002. [DOI] [PubMed] [Google Scholar]
- 10.Verheul R, Van den Brink W, Hartgers C. Personality disorders predict relapse in alcoholic patients. Addict Behav. 1998;23(6):869–882. doi: 10.1016/s0306-4603(98)00065-3. [DOI] [PubMed] [Google Scholar]
- 11.McKay JR, Pettinati HM, Morrison R, Feeley M, Mulvaney FD, Gallop R. Relation of depression diagnoses to 2-year outcomes in cocaine-dependent patients in a randomized continuing care study. Psychol Addict Behav. 2002;16(3):225–235. [PubMed] [Google Scholar]
- 12.Glasner-Edwards S, Mooney LJ, Marinelli-Casey P, Hillhouse M, Ang A, Rawson RA. Psychopathology in methamphetamine dependent adults 3 years after treatment. Drug and Alcohol Review. doi: 10.1111/j.1465-3362.2009.00081.x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown RA, Monti PM, Myers MG, Martin RA, Rivinus T, Dubreuil ME, Rohsenow DJ. Depression among cocaine abusers in treatment: relation to cocaine and alcohol use and treatment outcome. Am J Psychiatry. 1998;155(2):220–225. doi: 10.1176/ajp.155.2.220. [DOI] [PubMed] [Google Scholar]
- 14.Tate SR, Brown SA, Unrod M, Ramo DE. Context of relapse for substance-dependent adults with and without comorbid psychiatric disorders. Addict Behav. 2004;29(9):1707–1724. doi: 10.1016/j.addbeh.2004.03.037. [DOI] [PubMed] [Google Scholar]
- 15.Rawson RA, Marinelli-Casey P, Anglin MD, Dickow A, Frazier Y, Gallagher C, Galloway GP, Herrell J, Huber A, McCann MJ, Obert J, Pennell S, Reiber C, Vandersloot D, Zweben J. A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction. 2004;99(6):708–717. doi: 10.1111/j.1360-0443.2004.00707.x. [DOI] [PubMed] [Google Scholar]
- 16.Rawson R, Huber A, Brethen P, Obert J, Gulati V, Shoptaw S, Ling W. Methamphetamine and cocaine users: differences in characteristics and treatment retention. J Psychoactive Drugs. 2000;32(2):233–238. doi: 10.1080/02791072.2000.10400234. [DOI] [PubMed] [Google Scholar]
- 17.McLellan AT, Luborsky L, Woody GE, O'Brien CP. An improved diagnostic evaluation instrument for substance abuse patients. The Addiction Severity Index. J Nerv Ment Dis. 1980;168(1):26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Hillhouse M, Marinelli-Casey P, Rawson R. The LET (Life Experience Timeline): A new instrument for collecting time-anchored natural history data; Poster Presented at the 67th annual meeting of the College on Problems of Drug Dependence; Florida: Orlando; 2005. [Google Scholar]
- 19.Nurco DN, Bonito AJ, Lerner M, Balter MB. Studying addicts over time: methodology and preliminary findings. Am J Drug Alcohol Abuse. 1975;2:183–196. doi: 10.3109/00952997509002733. [DOI] [PubMed] [Google Scholar]
- 20.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59 Suppl 20:22–33. quiz 34–57. [PubMed] [Google Scholar]
- 21.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bourdon KH, Rae DS, Locke BZ, Narrow WE, Regier DA. Estimating the prevalence of mental disorders in U.S. adults from the Epidemiologic Catchment Area Survey. Public Health Rep. 1992;107(6):663–668. [PMC free article] [PubMed] [Google Scholar]
- 23.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen psychiatry. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 24.Carroll KM, Power ME, Bryant K, Rounsaville BJ. One-year follow-up status of treatment-seeking cocaine abusers. Psychopathology and dependence severity as predictors of outcome. J Nerv Ment Dis. 1993;181(2):71–79. doi: 10.1097/00005053-199302000-00001. [DOI] [PubMed] [Google Scholar]
- 25.McNamara C, Schumacher JE, Milby JB, Wallace D, Usdan S. Prevalence of nonpsychotic mental disorders does not affect treatment outcome in a homeless cocaine-dependent sample. The American Journal of Drug and Alcohol Abuse. 2001 Feb;27(1):91–106. doi: 10.1081/ada-100103120. [DOI] [PubMed] [Google Scholar]
- 26.Glasner -Edwards S, Marinelli-Casey P, Gonzales R, Hillhouse M, Ang A, Rawson RA. Depression among methamphetamine users: association with outcomes from the Methamphetamine Treatment Project at 3-year follow-up. Journal of Nervous & Mental Disease. 2009;197:225–231. doi: 10.1097/NMD.0b013e31819db6fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ritsher JB, McKellar JD, Finney JW, Otilingam PG, Moos RH. Psychiatric comorbidity, continuing care and mutual help as predictors of five-year remission from substance use disorders. J Stud Alcohol. 2002;63(6):709–715. doi: 10.15288/jsa.2002.63.709. [DOI] [PubMed] [Google Scholar]
- 28.Diefenbach GJ, Woolley SB, Goethe JW. The association between self-reported anxiety symptoms and suicidality. J Nerv Mental Dis. 2009;197(2):92–97. doi: 10.1097/NMD.0b013e318196127c. [DOI] [PubMed] [Google Scholar]
- 29.Sareen J, Houlahan T, Cox BJ, Asmundson GJ. Anxiety disorders associated with suicidal ideation and suicide attempts in the National Comorbidity Survey. J Nerv Ment Dis. 2005;193:450–454. doi: 10.1097/01.nmd.0000168263.89652.6b. [DOI] [PubMed] [Google Scholar]
- 30.Dalton EJ, Cate-Carter TD, Mundo E, Parikh SV, Kennedy JL. Suicide risk in bipolar patients: the role of co-morbid substance use disorders. Bipolar Disord. 2003;5(1):58–61. doi: 10.1034/j.1399-5618.2003.00017.x. [DOI] [PubMed] [Google Scholar]
- 31.Schneider B, Georgi K, Weber B, Schnabel A, Ackermann H, Wetterling T. Risk factors for suicide in substance-related disorders. Psychiatr Prax. 2006;33(2):81–87. doi: 10.1055/s-2005-866858. [DOI] [PubMed] [Google Scholar]
- 32.Glasner-Edwards S, Mooney LJ, Marinelli-Casey P, Hillhouse M, Ang A, Rawson RA. The Methamphetamine Treatment Project Corporate Authors: Risk factors for suicide attempts in methamphetamine dependent patients. The American Journal on Addictions. 2008;17(1):24–27. doi: 10.1080/10550490701756070. [DOI] [PubMed] [Google Scholar]