Abstract
Background
Whether the higher coronary mortality in South Asians compared with White populations is due to a higher incidence of disease is not known. This study assessed cumulative incidence of chest pain in South Asians and Whites, and prognosis of chest pain.
Methods
Over seven phases of 18-year follow-up of the Whitehall-II study (9775 civil servants: 9195 White, 580 South Asian), chest pain was assessed using the Rose questionnaire. Coronary death/non-fatal myocardial infarction was examined comparing those with chest pain to those with no chest pain at baseline.
Results
South Asians had higher cumulative frequencies of typical angina by Phase 7 (17.0 versus 11.3%, P < 0.001) and exertional chest pain (15.4 versus 8.5%, P < 0.001) compared with Whites. Typical angina and exertional chest pain at baseline were associated with a worse prognosis compared with those with no chest pain in both groups (typical angina, South Asians: HR, 4.67 and 95% CI, 2.12–0.30; Whites: HR, 3.56 95% CI, 2.59–4.88). Baseline non-exertional chest pain did not confer a worse prognosis. Across all types of pain, prognosis was worse in South Asians.
Conclusion
South Asians had higher cumulative incidence of angina than Whites. In both, typical angina and exertional chest pain were associated with worse prognosis compared with those with no chest pain.
Keywords: circulatory disease, epidemiology, ethnicity
Introduction
South Asians in industrialized countries experience higher coronary heart disease mortality compared with native majority White populations, in cross-sectional1–5 and prospective studies.6 This may be either as a consequence of higher incidence of coronary disease in South Asian populations or a worse prognosis of already-manifested coronary disease. Angina is a common initial manifestation of coronary heart disease7 and a significant burden in primary care.8 Early identification of angina is important for the initiation of interventions to reduce the future risk of a more serious cardiac event.9 What is not known is whether South Asian ethnicity results in a higher incidence of stable angina.10
South Asian people may however report atypical features when presenting with acute chest pain11,12 and in a small cross-sectional study13 measurement of chronic angina using questionnaires was reported to be less consistent in South Asian people when compared with the presence of a doctor diagnosis. The higher prevalence of diabetes14 and cultural differences in the experience, interpretation and understanding of pain13 have been used to support a common clinical perception that chest pain is difficult to assess in South Asians.
We aimed to assess the cumulative incidence of typical angina and exertional and non-exertional chest pain in a healthy population of South Asian and White people, and assess the prognostic significance of chest pain on risk of subsequent coronary death or non-fatal myocardial infarction. We used the Whitehall-II prospective cohort study with detailed characterization of symptoms of chest pain using the Rose questionnaire at seven time points over 18 years of follow-up.
Methods
Participants
The Whitehall-II study is a prospective cohort of non-industrial civil servants in London aged 35–55 years recruited by invitation (1985–1988).15 The target population of the study was all London-based office staff of 20 civil service departments and with a response of 73%, the baseline cohort consisted of 10 308 people, 3413 women and 6895 men. A clinical examination and a self-completed questionnaire (within which the Rose questionnaire was embedded) were administered at Phase 1. Six further phases were conducted at regular time points over 18 years of follow-up with the odd numbered phases consisting of both a clinical examination and a questionnaire and the even numbered phases consisting of a questionnaire alone. By 18 years (Phase 7), retained follow-up for the whole cohort was 67%.
Ethnicity
Ethnicity was defined according to the Office for National Statistics 1991 census types. Participants self-reported their ethnicity at Phase 5, and where this was missing, observer-assigned ethnicity from Phase 1 was used. There was strong agreement between data on observer-assigned ethnicity and self-reported ethnicity—93% for South Asians and 99.3% for Whites. Of the participants, 580 participants were grouped as South Asian and 9195 were ascribed as White. We took South Asian to represent those of Indian, Sri Lankan, Pakistani and Bangladeshi ethnic origin.
Chest pain
At each of seven phases over 18 years follow-up, symptoms of stable angina pectoris were assessed using the seven-item Rose angina questionnaire (appendix). Chest pain was defined in three mutually exclusive groups:
‘typical angina’ if the pain was located over the sternum or in both the left chest and the left arm, was precipitated by exertion, caused the person to stop or slow down and went away in 10 minutes or less when they stood still;
‘exertional chest pain’, based on the ‘possible’ classification,16 being chest pain brought on by exertion but not satisfying the additional criteria, such as location and relation to rest, necessary for a diagnosis of typical angina;
‘non-exertional chest pain’ was defined as those complaining of chest pain that had no relation to exertion.
Of the 580 South Asian and 9195 White participants, the vast majority had data on chest pain at Phase 1 (577 South Asian participants and 9184 White participants). By 18 year follow-up at Phase 7, data on chest pain were available on 317 South Asian participants and 6268 White participants (41 South Asian participants and 525 White participants having died), and loss to follow-up through the successive phases was mostly as a result of not filling in the overall study questionnaire rather than not filling in the Rose angina section, with the response rate for the Rose angina questionnaire being very high (almost 100%) in those that returned the questionnaire. Though as expected those with missing follow-up data at Phase 7 had worse baseline risk factor profiles, these patterns did not differ by ethnic groups in likelihood ratio tests of interaction.
For prognostic analyses, baseline was defined as Phases 1–3, as angina is a relapsing and remitting symptom. Those with typical angina at either Phases 1, 2 or 3 were defined as baseline typical angina and baseline exertional chest pain was similarly defined using exertional chest pain at either Phases 1, 2 or 3 among those who had not already been classified as having typical angina. Baseline non-exertional chest pain again was defined as those who had not already been classified as having typical angina or exertional chest pain at one of the Phases 1, 2 or 3.
Risk factors
Standardized assessments were made of smoking, hypertension (blood pressure higher than or equal to 130/85 mmHg or on antihypertensive medication), total cholesterol, body mass index (BMI), self-reported diagnosis of diabetes and family history (in parents or siblings) of onset of coronary heart disease before age 55 years at Phase 1. Metabolic syndrome was defined by the 2001 National Cholesterol Education Program Adult Treatment Panel-III criteria at Phase 3 by the presence of three or more of central obesity, elevated fasting blood triglycerides, reduced blood HDL cholesterol, elevated blood pressure, elevated fasting glucose.17 Impaired glucose tolerance was defined as a fasting plasma glucose <7 mmol/l and postload glucose of ≥7.8 mmol/l (140 mg/dl) and <11.1 mmol/l. Civil service employment grade was used as a measure of socioeconomic position in three levels: senior administrative grades (high), middle-ranking executive officers (intermediate) and clerical and support staff (low).
Outcomes and follow-up
The outcome in prognostic analyses was the incidence of a combined endpoint of coronary death or non-fatal myocardial infarction between Phases 3 and 7. For each subject, the period of follow-up was up to the date when the subject was last seen in the study or their date of death, provided that the subject attended their last possible study phase prior to their death. Ninety-nine per cent of participants were flagged for mortality at the National Health Service Central Registry. Coronary death was defined by the International Classification of Diseases-Ninth Revision (ICD-9) codes 410–414 and ICD-10 codes I20–I25.18,19 Based on all available data (from questionnaire, study ECGs, hospital acute ECGs and cardiac enzymes), non-fatal myocardial infarction was defined using World Health Organization MONICA Project (multinational monitoring of trends and determinants in cardiovascular disease) criteria.20
Classification of non-fatal myocardial infarction was carried out blind to other study data independently by two trained coders, with adjudication by a third in the (rare) event of disagreement.
Statistical analysis
Cumulative incidence was estimated with 95% confidence intervals of those who complained of typical, exertional and non-exertional chest pain through the six phases of the study following phase 1. For baseline characteristics, continuous variables were presented as means with standard deviation and proportions as percentages. These baseline clinical and socio-demographic data were tabulated by ethnic group across types of chest pain, and tested for age-adjusted linear trend across the three positive chest pain categories, in South Asian participants and in White participants, using the Mantel–Haenszel chi-squared test for linear trend for proportions and the analysis of variance for trend for continuous variables. Allowance for multiple comparisons was made by using the Bonferroni correction so that statistical significance of the baseline characteristics was defined as those associations with a P-value ≤0.002 (=0.05/24).
The rates of incident coronary death or non-fatal myocardial infarction per 1000 person-years were examined comparing those with typical, exertional and non-exertional chest pain on at least one of the first three phases to those with no chest pain at any of these early stages, for each ethnic group. Cox's proportional hazards models were used to estimate hazard ratios (HR) and 95% confidence intervals for the chest pain categories and were adjusted for age and sex and additionally for hypertension, blood cholesterol, ex/current smoker, overweight (BMI >30), diabetes, living alone, family history and employment grade.
A separate model examined rates of incident coronary death or non-fatal myocardial infarction per 1000 person-years within each type of chest pain comparing South Asian with White participants. Adjusted Cox's proportional hazards models were again used. A likelihood ratio test was used to assess interaction between ethnicity and chest pain. The proportional hazards assumption was tested using Schoenfeld residuals and found to be not violated.
All analyses were performed using STATA (version 11; StataCorp, College Station, TX, USA).
Results
This study accumulated 153 750 person-years of follow-up. Irrespective of the type of chest pain, South Asian participants tended to be older, less likely to have smoked, more likely to be hypertensive and diabetic, more likely to live with a partner, have a higher prevalence of metabolic syndrome and be in lower employment grades of work than White participants (Table 1). Among both ethnic groups, there was an increasing prevalence of hypertension and higher cholesterol levels and trends towards more metabolic syndrome and higher body mass index with more typical chest pain, but no other similar trends were observed. In particular, neither glucose intolerance nor diabetes mellitus had a significant relationship with the presence/absence of chest pain or chest pain types, in both populations studied.
Table 1.
Baseline characteristics in each chest pain type comparing South Asian and White participants
| Ethnic group | Whole cohort | No chest pain | Non-exertional chest pain | Exertional chest pain | Typical angina | Pfor trend across chestpain types | |
|---|---|---|---|---|---|---|---|
| n | South Asian | 580 | 312 | 134 | 73 | 58 | |
| White | 9195 | 5444 | 2619 | 587 | 534 | ||
| Age in years, mean (SD) | South Asian | 45.65 (5.7) | 45.26 (6.0) | 45.71 (5.3) | 46.14 (5.7) | 47.14 (5.0) | 0.115 |
| White | 44.31 (6.1) | 44.36 (6.1) | 43.77 (5.9) | 44.70 (6.2) | 45.90 (6.1) | <0.001 | |
| Men | South Asian | 357 (61.6) | 183 (41.3) | 100 (74.6) | 45 (61.6) | 27 (46.6) | 0.482 |
| White | 6309 (68.6) | 3591 (66.0) | 2019 (77.1) | 387 (65.9) | 308 (57.7) | 0.726 | |
| Ex/current smoker | South Asian | 190 (33.0) | 96 (31.2) | 50 (37.6) | 28 (38.4) | 16 (27.6) | 0.758 |
| White | 4767 (52.3) | 2700 (50.1) | 1425 (54.8) | 334 (57.3) | 300 (56.9) | <0.001 | |
| Hypertensive | South Asian | 70 (12.1) | 32 (10.3) | 11 (8.2) | 10 (13.7) | 16 (27.6) | 0.002 |
| White | 714 (7.8) | 410 (7.5) | 168 (6.4) | 52 (8.9) | 83 (15.5) | <0.001 | |
| Cholesterol, mean (SD) in mmol/l | South Asian | 5.96 (1.2) | 5.90 (1.2) | 5.94 (1.2) | 5.95 (1.2) | 6.39 (1.5) | 0.052 |
| White | 5.97 (1.2) | 5.94 (1.2) | 5.94 (1.1) | 6.09 (1.2) | 6.19 (1.2) | <0.001 | |
| Hyperglycaemic | |||||||
| Diabetic | South Asian | 22 (3.8) | 9 (2.9) | 6 (4.6) | 4 (5.5) | 2 (3.5) | 0.464 |
| White | 61 (0.7) | 38 (0.7) | 14 (0.5) | 3 (0.5) | 6 (1.1) | 0.737 | |
| Impaired glucose tolerance | South Asian | 46 (7.9) | 25 (8.0) | 9 (6.7) | 7 (9.6) | 5 (8.6) | 0.784 |
| White | 561 (6.1) | 327 (6.0) | 157 (6.0) | 37 (6.3) | 40 (7.5) | 0.27 | |
| Metabolic syndrome | South Asian | 66 (15.9) | 34 (15.9) | 15 (14.7) | 6 (11.8) | 11 (23.4) | 0.516 |
| White | 754 (10.6) | 391 (9.5) | 214 (10.1) | 76 (16.2) | 73 (17.0) | <0.001 | |
| BMI, mean (SD) | South Asian | 24.44 (3.3) | 24.26 (3.4) | 24.64 (3.1) | 24.49 (2.9) | 24.84 (3.7) | 0.537 |
| White | 24.55 (3.5) | 24.42 (3.4) | 24.46 (3.2) | 25.16 (4.0) | 25.65 (4.0) | <0.001 | |
| Living with partner | South Asian | 487 (84.3) | 256 (82.6) | 118 (88.1) | 61 (83.6) | 50 (86.2) | 0.424 |
| White | 6766 (73.8) | 3995 (73.6) | 1987 (76.2) | 403 (69.0) | 375 (70.4) | 0.146 | |
| Family history | South Asian | 227 (39.1) | 115 (36.9) | 52 (38.8) | 32 (43.8) | 27 (46.6) | 0.106 |
| White | 3599 (39.1) | 2060 (37.8) | 1029 (39.3) | 247 (42.1) | 259 (48.5) | <0.001 | |
| Employment grade, low | South Asian | 290 (50.0) | 158 (50.6) | 55 (41.0) | 43 (58.9) | 32 (55.2) | 0.514 |
| White | 1733 (18.8) | 1095 (20.1) | 377 (14.4) | 124 (21.1) | 128 (24.9) | 0.703 | |
The categories of chest pain total 9184 White and 577 South Asian participants who had data on chest pain at Phase 1. The whole cohort comprises the 9195 White participants at Phase 1 and the 580 South Asian participants. Data are n (%) unless otherwise specified. Test for trend is age adjusted.
Incidence of different forms of chest pain by ethnic group
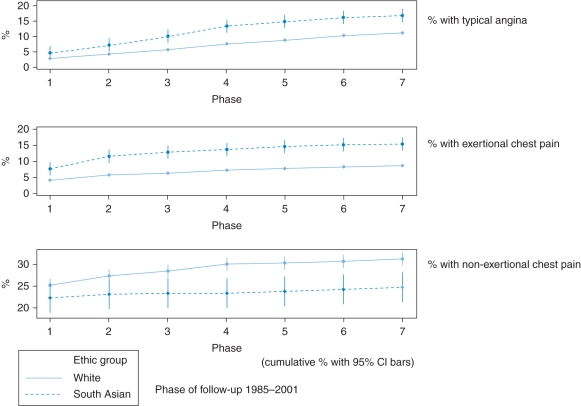
At Phase 1, South Asian participants had a higher prevalence of typical angina compared with White participants (4.8 versus 2.8%, P = 0.019) and exertional chest pain (7.8 versus 4.1%, P < 0.001) but not non-exertional chest pain (22.2 versus 25.2%, P = 0.085), as depicted in Fig. 1. By Phase 7, South Asian participants had higher cumulative frequencies of typical angina (17.0 versus 11.3%, P < 0.001) and exertional chest pain (15.4 versus 8.5%, P < 0.001) compared with White participants. For non-exertional chest pain, South Asian participants had a lower cumulative frequency (24.6 versus 31.3%, P = 0.001) compared with White participants.
Fig. 1.
Cumulative incidence of different types of chest pain by ethnic group over seven study phases.
Prognosis within ethnic groups of those with pain compared with those with no chest pain
In both South Asian and White participants, those with baseline typical angina and exertional chest pain had a worse prognosis for the long-term coronary outcome compared with those with no baseline chest pain. HR were similar in magnitude (in South Asian participants with typical angina adjusted: HR, 4.67 and 95% CI, 2.12–10.30; in White participants with typical angina adjusted: HR, 3.56 and 95% CI, 2.59–4.88, Table 2). Baseline non-exertional chest pain was not associated with a worse prognosis in either ethnic group.
Table 2.
Risk for coronary death and non-fatal myocardial infarction, comparing types of chest pain with those with no chest pain, and comparing South Asian with White participants by type of chest pain
| Study population | Ethnic group | n | Number of CHD events by Phase 7 | Rate/1000 person years (95% CI) |
HRs within ethnic groups compared with those with no chest pain |
HRs within types of pain for South Asian compared with White participants (95% CI) |
||
|---|---|---|---|---|---|---|---|---|
| Age and sex-adjusted | Adjusteda | Age- and sex adjusted | Adjusteda | |||||
| No chest pain | White | 5444 | 138 | 1.67 (1.42, 1.96) | 1 | 1 | 1 | 1 |
| South Asian | 312 | 15 | 3.44 (2.08, 5.71) | 1 | 1 | 1.92 (1.13, 3.28) | 1.58 (0.87, 2.86) | |
| Non-exertional chest pain | White | 2619 | 80 | 1.95 (1.57, 2.43) | 1.14 (0.86, 1.49) | 1.16 (0.88, 1.53) | 1 | 1 |
| South Asian | 134 | 9 | 4.68 (2.44, 9.00) | 1.24 (0.54, 2.84) | 1.34 (0.56, 3.22) | 2.10 (1.05, 4.20) | 2.17 (1.04, 4.53) | |
| Exertional chest pain | White | 587 | 41 | 4.56 (3.36, 6.19) | 2.71 (1.91, 3.84) | 2.34 (1.64, 3.32) | 1 | 1 |
| South Asian | 73 | 8 | 8.21 (4.11, 16.4) | 2.37 (1.01, 5.60) | 2.52 (1.02, 6.18) | 1.70 (0.79, 3.65) | 1.74 (0.75, 4.03) | |
| Typical angina | White | 534 | 59 | 7.49 (5.80, 9.66) | 4.32 (3.18, 5.87) | 3.56 (2.59, 4.88) | 1 | 1 |
| South Asian | 58 | 17 | 21.9 (13.6, 35.3) | 6.93 (3.40, 14.10) | 4.67 (2.12, 10.30) | 2.94 (1.71, 5.06) | 2.56 (1.36, 4.84) | |
The study population of the whole cohort represents those at Phase 1.
The study populations of the types of chest pain represent those who complained of these pains at Phases 1, 2 or 3. The types are mutually exclusive, as those with exertional chest pain excluded those who had complained of typical angina at one of the Phases 1, 2 or 3, and baseline non-exertional chest pain excluded those who had complained of typical angina or exertional chest pain at one of the Phases 1, 2 or 3.
CHD event: incident coronary death or non-fatal myocardial infarction.
aAdjusted for age, sex, hypertension, blood cholesterol, ex/current smoker, overweight, diabetes, living alone, family history and employment grade.
Prognosis within types of pain for South Asian compared with White participants
Among those with typical angina at baseline, South Asian participants had a worse long-term prognosis than White participants: HR, 2.56 and 95% CI, 1.36–4.84, Table 2). The South Asian population also had a worse long-term prognosis than the White population in those with non-exertional chest pain, and there was a similar trend in those with exertional chest pain and no chest pain. Across all types of chest pain, the rates of CHD events were higher in South Asian participants. A likelihood ratio test revealed no interaction between ethnicity and chest pain (P = 0.720).
Discussion
Main finding of this study
We found a higher cumulative incidence of typical angina and exertional chest pain in South Asian participants compared with White participants, in a study of almost 10 000 people with detailed characterization of symptoms of stable angina using the Rose angina questionnaire at seven time points over 18 year follow-up. We found that in both South Asian and White participants, typical angina and exertional chest pain at baseline were strongly associated with increased rates of coronary events when compared with those with no chest pain, but non-exertional chest pain was not associated with future coronary events. Thus, the Rose angina questionnaire was similarly valid in predicting an adverse prognosis in South Asians as has been demonstrated in White populations.21
What is already known on this topic
South Asians experience higher coronary heart disease mortality compared with native majority White populations, and Whitehall-II has previously reported within the whole cohort that South Asian subjects had an increased prevalence of hypertension, diabetes and a high-risk lipid profile in spite of adjusting for socioeconomic class.22 South Asians have been reported as having atypical features when presenting with chest pain.
What this study adds
The principal clinical implication of our findings is that South Asians and Whites with typical pain as measured by the Rose questionnaire appear to have a similarly poor prognosis compared with those with no chest pain. The differing populations of chest pain did not significantly differ in their risk profile at baseline. Thus, differences in prognosis can thus be predicted by the type of chest pain as measured by the Rose questionnaire. This challenges the clinical assumption that symptoms in South Asians may not be predictive of outcomes. This provides further population-based evidence for the NICE (the UK National Institute for Health and Clinical Excellence) guidance on chest pain,23 which came out in March 2010. From a public health perspective, angina prevalence is not declining, in contrast to the marked decline observed in myocardial infarction24 and is increasingly the most common initial symptomatic manifestation of coronary disease.10 The inconsistent relationships between cardiovascular risk factors and the presence/absence of chest pain remind clinicians that at this early stage of disease, risk factors in both populations studied may not be a proxy for true angina. The presence of diabetes mellitus has similarly been reported to not be a strong predictor for serious coronary outcomes (e.g. nonfatal myocardial infarction and cardiac death) in patients at an early stage of the natural history of the disease (e.g. asymptomatic diabetes).25 Thus, clinicians should focus on the chest pain history over risk factor profile for assessment of prognosis at this early stage of cardiovascular disease.
We also found that South Asians had higher coronary death and non-fatal myocardial infarction rates than Whites irrespective of the presence and type of chest pain. This is consistent with the South Asian ethnicity per se being associated with a higher cardiovascular risk. However, we do not have data on clinical management over the period of follow-up, and in particular whether or not typical pain as measured by the Rose questionnaire was treated clinically as angina equitably across ethnic groups. This has important healthcare implications, as appropriate management can allay an adverse prognosis in high-risk groups such as South Asians. Recent data have reported that among people presenting with typical angina to a rapid access chest pain clinic, South Asians were no more likely than Whites to experience an adverse coronary outcome on long-term follow-up.26 Mortality rates following appropriate coronary angiography in a population with chronic angina have also been reported to be similar in South Asians and Whites.27
Limitations of this study
Whether the higher prevalence of diabetes in South Asians compared with whites influenced our findings is uncertain. Evidence for altered perception of angina in diabetes is mixed, with not all studies showing associations with silent ischaemia.28 The majority of patients with diabetes experience angina in the same way as those without diabetes29 and any increase in silent ischaemia that may have occurred among South Asians only strengthens our main finding of their enhanced susceptibility to angina. We further acknowledge that though we used 2001 National Cholesterol Education Program Adult Treatment Panel-III to define metabolic syndrome, the International Diabetes Federation definition considers ethnicity and may be more accurate for South Asians. We did, in spite of this, still find a higher prevalence of metabolic syndrome in South Asians. We appreciate also that South Asians develop complications of obesity at a lower threshold for body mass index than people of Europid origin, and that for a given BMI, a South Asian person carries more fat in the abdominal area. Thus, waist circumference would have been a more preferable measure in such ethnic group comparisons. We used BMI rather than waist circumference as it was more valid across both sexes in this study, with more data available; there was a high correlation between BMI and waist circumference across both ethnic groups.
We defined baseline angina using subjects' responses at Phases 1, 2 and 3. By Phase 3, the response rate was 71% among South Asians and 82% among Whites. Hence, it is possible that the likelihood of detection of chest pain and angina across these phases might have been marginally less in South Asians compared with Whites. However, the result of this differential detection would be that our estimates of the difference in the angina effects between the South Asians and Whites might be underestimated.
The Whitehall-II civil servants may not be representative of the general population. South Asians in the Whitehall-II study were mostly Indian (74% Indian, with 13% Sri Lankan, 10% Pakistani and 3% Bangladeshi). Overall as a group, Indian people have consistently been reported to have lower levels of smoking30 and higher levels of diabetes.31 As the prevalence of angina may be higher in Pakistani men than Indian and Bangladeshi men,14 these results from Whitehall-II may underestimate the cumulative incidence of angina in South Asian populations. However, evidence that our findings are likely to be robust comes from a multi-centre chest pain clinic study, in which assessment of chest pain by a cardiologist showed similar prognostic validity in South Asians and Whites.26 Similar social and ethnic differences in other incident forms of coronary heart disease have been shown in other general population studies.6
Although our study is, to the best of our knowledge, the only prospective population-based study comparing incident angina and non-fatal myocardial infarction in Whites and South Asians, it is a small study with wide confidence intervals and thus there is the inherent possibility of type II errors. Finally, though loss to follow-up was 33% by 18 years, the biggest driver to loss of follow-up for chest pain data was loss of the overall study questionnaire, as part of the overall attrition within the Whitehall-II cohort study, and not specifically of loss of follow-up of the Rose angina section of the study questionnaire. Though those with missing follow-up data had a worse cardiovascular risk profile at rest as might be expected, this did not differ by ethnic group.
Conclusions
In summary, we have demonstrated here that South Asians have a higher incidence of typical angina over long-term follow-up compared with Whites, but that they did not have a higher incidence of chest pain that was non-exertional in nature. Typical angina was associated with a worse prognosis for coronary death and non-fatal myocardial infarction in both South Asians and Whites. Further work is required to further highlight the prognostic significance of early chest pain symptoms in ethnic groups at high risk of serious coronary outcomes, through larger studies and valid and careful measurement of angina.
Contributors
M.J.Z. and H.H. had the idea for the study; M.J.Z. did all statistical analyses, wrote the first draft, incorporated comments from all co-authors and is the guarantor. M.J.S. and M.S. were involved in further analysis. M.G.M. set up the cohort. E.B., A.D.T. and M.G.M. were involved in the discussion and interpretation. H.H. contributed to the first draft and analysis, and was involved in the discussion and interpretation. All authors participated in the discussion and interpretation of the final results and contributed to the final paper.
Funding
This work was supported by grants from the Medical Research Council; British Heart Foundation; Health and Safety Executive; Department of Health; National Heart Lung and Blood Institute (HL36310), US, NIH; National Institute on Aging (AG13196), US, NIH; Agency for Health Care Policy Research (HS06516) and the John D and Catherine T MacArthur Foundation Research Networks on Successful Midlife Development and Socioeconomic Status and Health. M.J.Z. was supported by a BHF Clinical PhD Studentship. M.S. is supported by a post-doctoral award from the Department of Health. M.M. is supported by an MRC research professorship.
Acknowledgements
We thank all participating civil service departments and their welfare personnel and establishment officers; the Occupational Health and Safety Agency; the Council of Civil Service Unions; all participating civil servants in the Whitehall-II study; and all members of the Whitehall-II Study Team. The Whitehall-II Study Team comprises research scientists, statisticians, study coordinators, nurses, data managers, administrative assistants and data entry staff, who make the study possible. We thank Tarani Chandola for critically reviewing the manuscript.
Ethical approval: Each phase of the Whitehall-II study has received ethical approval from the research ethics committee of UCL Hospitals.
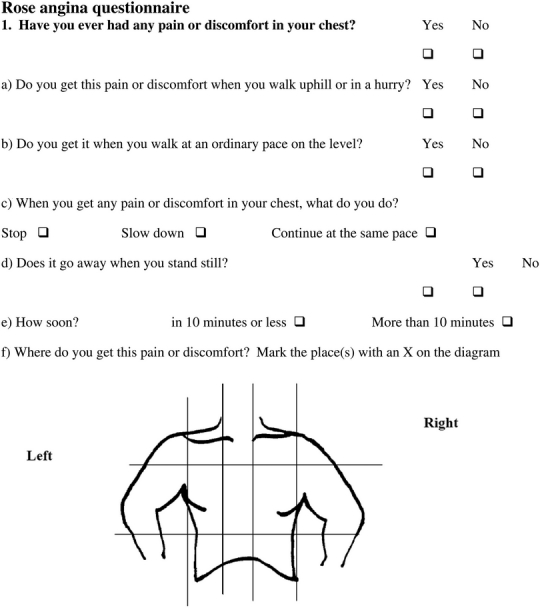
Appendix: Rose angina questionnaire
References
- 1.Harding S, Rosato M, Teyhan A. Trends for coronary heart disease and stroke mortality among migrants in England and Wales, 1979–2003: slow declines notable for some groups. Heart. 2008;94(4):463–70. doi: 10.1136/hrt.2007.122044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wild SH, Fischbacher C, Brock A, et al. Mortality from all causes and circulatory disease by country of birth in England and Wales 2001–2003. J Public Health (Oxf) 2007;29(2):191–8. doi: 10.1093/pubmed/fdm010. [DOI] [PubMed] [Google Scholar]
- 3.Fischbacher CM, Steiner M, Bhopal R, et al. Variations in all cause and cardiovascular mortality by country of birth in Scotland, 1997–2003. Scott Med J. 2007;52(4):5–10. doi: 10.1258/rsmsmj.52.4.5. [DOI] [PubMed] [Google Scholar]
- 4.Sheth T, Nair C, Nargundkar M, et al. Cardiovascular and cancer mortality among Canadians of European, south Asian and Chinese origin from 1979 to 1993: an analysis of 1.2 million deaths. CMAJ. 1999;161(2):132–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Palaniappan L, Wang Y, Fortmann SP. Coronary heart disease mortality for six ethnic groups in California, 1990–2000. Ann Epidemiol. 2004;14(7):499–506. doi: 10.1016/j.annepidem.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 6.Forouhi NG, Sattar N, Tillin T, et al. Do known risk factors explain the higher coronary heart disease mortality in South Asian compared with European men? Prospective follow-up of the Southall and Brent studies, UK. Diabetologia. 2006;V49(11):2580–8. doi: 10.1007/s00125-006-0393-2. doi:10.1007/s00125-006-0393-2. [DOI] [PubMed] [Google Scholar]
- 7.Hemingway H, McCallum A, Shipley M, et al. Incidence and prognostic implications of stable angina pectoris among women and men. JAMA. 2006;295(12):1404–11. doi: 10.1001/jama.295.12.1404. [DOI] [PubMed] [Google Scholar]
- 8.McCormick A, Fleming D, Charlton J. Morbidity Statistics from General Practice. Fourth National Study, 1991–1992. London: HMSO: Royal College of General Practitioners, Office of Population Censuses and Surveys, Department of Health; 1995. [Google Scholar]
- 9.Cannon CP, Steinberg BA, Murphy SA, et al. Meta-analysis of cardiovascular outcomes trials comparing intensive versus moderate statin therapy. J Am Coll Cardiol. 2006;48(3):438–45. doi: 10.1016/j.jacc.2006.04.070. [DOI] [PubMed] [Google Scholar]
- 10.Hemingway H, Langenberg C, Damant J, et al. Prevalence of angina in women versus men: a systematic review and meta-analysis of international variations across 31 countries. Circulation. 2008;117(12):1526–36. doi: 10.1161/CIRCULATIONAHA.107.720953. [DOI] [PubMed] [Google Scholar]
- 11.Barakat K, Wells Z, Ramdhany S, et al. Bangladeshi patients present with non-classic features of acute myocardial infarction and are treated less aggressively in east London, UK. Heart. 2003;89(3):276–9. doi: 10.1136/heart.89.3.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Teoh M, Lalondrelle S, Roughton M, et al. Acute coronary syndromes and their presentation in Asian and Caucasian patients in Britain. Heart. 2007;93(2):183–8. doi: 10.1136/hrt.2006.091900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fischbacher CM, Bhopal R, Unwin N, et al. The performance of the Rose angina questionnaire in South Asian and European origin populations: a comparative study in Newcastle, UK. Int J Epidemiol. 2001;30(5):1009–16. doi: 10.1093/ije/30.5.1009. [DOI] [PubMed] [Google Scholar]
- 14.Sproston K, Mindell J. Health Survey for England 2004. The Health of Minority Ethnic Groups. London: NatCen; 2006. [Google Scholar]
- 15.Marmot MG, Smith GD, Stansfeld S, et al. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991;337(8754):1387–93. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- 16.Cook DG, Shaper AG, MacFarlane PW. Using the WHO (Rose) angina questionnaire in cardiovascular epidemiology. Int J Epidemiol. 1989;18(3):607–13. doi: 10.1093/ije/18.3.607. [DOI] [PubMed] [Google Scholar]
- 17.Grundy SM, Becker D, Clark LT, et al. Third report of the National Cholesterol Education Program (NCEP). Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421. [PubMed] [Google Scholar]
- 18.World Health Organization. International Classification of Diseases, 10th revision. Geneva, World Health Organization; 1990. [Google Scholar]
- 19.World Health Organization. International Classification of Diseases, 9th revision. Geneva, World Health Organization; 1977. [Google Scholar]
- 20.Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, et al. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90:583–612. doi: 10.1161/01.cir.90.1.583. [DOI] [PubMed] [Google Scholar]
- 21.Graff-Iversen S, Selmer R, Lochen ML. Rose angina predicts 23-year coronary heart disease mortality in women and men aged 40–49 years. Heart. 2008;94(4):482–6. doi: 10.1136/hrt.2007.115931. [DOI] [PubMed] [Google Scholar]
- 22.Whitty CJ, Brunner EJ, Shipley MJ, et al. Differences in biological risk factors for cardiovascular disease between three ethnic groups in the Whitehall II study. Atherosclerosis. 1999;142(2):279–86. doi: 10.1016/s0021-9150(98)00239-1. [DOI] [PubMed] [Google Scholar]
- 23.National Institute for Health and Clinical Excellence. Chest pain of recent onset: assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin. 2010. http://guidance.nice.org.uk/CG95 . [PubMed]
- 24.Aitsi-Selmi A, Shipley M, Hemingway H. Stable angina pectoris: comparison of trends in symptoms and diagnosed cases of angina from 1991 to 2003 with trends in MI mortality. EJCPR. 2008;15:S25–6. (EuroPRevent Congress abstracts ) [Google Scholar]
- 25.Young LH, Wackers FJT, Chyun DA, et al. Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with Type 2 diabetes: the DIAD study: a randomized controlled trial. JAMA. 2009;301(15):1547–55. doi: 10.1001/jama.2009.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zaman MJ, Junghans C, Sekhri N, et al. Presentation of stable angina pectoris among women and South Asian people. CMAJ. 2008;179(7):659–67. doi: 10.1503/cmaj.071763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zaman MJ, Crook AM, Junghans C, et al. Ethnic differences in long-term improvement of angina following revascularization or medical management: a comparison between south Asians and white Europeans. J Public Health. 2009;31(1):168–74. doi: 10.1093/pubmed/fdn099. [DOI] [PubMed] [Google Scholar]
- 28.Falcone C, Nespoli L, Geroldi D, et al. Silent myocardial ischemia in diabetic and nondiabetic patients with coronary artery disease. Int J Cardiol. 2003;90(2–3):219–27. doi: 10.1016/s0167-5273(02)00558-2. doi:10.1016/S0167-5273(02)00558-2. [DOI] [PubMed] [Google Scholar]
- 29.Kelion AD, Al-Housni MB, Hutchings F. Are diabetic patients less likely to feel angina than nondiabetic controls for a given extent of myocardial ischaemia? Nucl Med Commun. 2010;31(8):741–5. doi: 10.1097/mnm.0b013e32833c3130. [DOI] [PubMed] [Google Scholar]
- 30.Erens B, Primatesta P, Prior G. Health Survey for England. The Health of Minority Ethnic Groups 1999. London: TSO; 2001. [Google Scholar]
- 31.Oldroyd J, Banerjee M, Heald A, et al. Diabetes and ethnic minorities. Postgrad Med J. 2005;81(958):486–90. doi: 10.1136/pgmj.2004.029124. [DOI] [PMC free article] [PubMed] [Google Scholar]