Abstract
Background: Ovarian cancer is generally diagnosed at an advanced stage where the case/fatality ratio is high and thus remains the most lethal of all gynecologic malignancies among US women 1,2,3. Serous tumors are the most widespread forms of ovarian cancer and 4,5 the Tg-MISIIR-TAg transgenic represents the only mouse model that spontaneously develops this type of tumors. Tg-MISIIR-TAg mice express SV40 transforming region under control of the Mullerian Inhibitory Substance type II Receptor (MISIIR) gene promoter 6. Additional transgenic lines have been identified that express the SV40 TAg transgene, but do not develop ovarian tumors. Non-tumor prone mice exhibit typical lifespan for C57Bl/6 mice and are fertile. These mice can be used as syngeneic allograft recipients for tumor cells isolated from Tg-MISIIR-TAg-DR26 mice.
Objective: Although tumor imaging is possible 7, early detection of deep tumors is challenging in small living animals. To enable preclinical studies in an immunologically intact animal model for serous ovarian cancer, we describe a syngeneic mouse model for this type of ovarian cancer that permits in vivo imaging, studies of the tumor microenvironment and tumor immune responses.
Methods: We first derived a TAg+ mouse cancer cell line (MOV1) from a spontaneous ovarian tumor harvested in a 26 week-old DR26 Tg-MISIIR-TAg female. Then, we stably transduced MOV1 cells with TurboFP635 Lentivirus mammalian vector that encodes Katushka, a far-red mutant of the red fluorescent protein from sea anemone Entacmaea quadricolor with excitation/emission maxima at 588/635 nm 8,9,10. We orthotopically implanted MOV1Kat in the ovary 11,12,13,14 of non-tumor prone Tg-MISIIR-TAg female mice. Tumor progression was followed by in vivo optical imaging and tumor microenvironment was analyzed by immunohistochemistry.
Results: Orthotopically implanted MOV1Kat cells developed serous ovarian tumors. MOV1Kat tumors could be visualized by in vivo imaging up to three weeks after implantation (fig. 1) and were infiltrated with leukocytes, as observed in human ovarian cancers 15 (fig. 2).
Conclusions: We describe an orthotopic model of ovarian cancer suitable for in vivo imaging of early tumors due to the high pH-stability and photostability of Katushka in deep tissues. We propose the use of this novel syngeneic model of serous ovarian cancer for in vivo imaging studies and monitoring of tumor immune responses and immunotherapies.
Protocol
1. Cell Culture
Before orthotopic injection, culture MOV1Kat cells, derived from DR26 tumors, in a T175 flask until they are 90% confluent. Plan to use 1 to 5 million cells per injection, which will require 1 or 2 T175 flasks.
On the day of the injection, harvest the cells and determine the cell number using a hemocytometer.
Once the cell concentration has been determined, pellet the cells by centrifugation for 5 minutes at 300 X g at room temperature.
Following the spin, resuspend the cells to have 1 million in 10 microliters of sterile PBS with 0.002 M EDTA
2. Pre-Surgery
Prior to surgery, fill up a 3/10cc insulin syringe with 1 million MOV1-Kat cells in 10 microliters of PBS EDTA.
Transfer an isofluorane anesthetized mouse to a heating pad. Add eye ointment to prevent eye dehydration. Then, immediately insert the animal's head into a nose cone system connected to an isoflurane vaporizer to deliver anesthesia throughout the surgery.
After disinfection of the injection site with alcohol swabs, subcutaneously inject 5 mg/kg of Ketoprofen, a pre-surgical analgesic, with a 3/10cc Insulin syringe.
Using clippers, shave the left caudal portion of the dorsum from the thoracolumbar junction to the base of the animal tail. Apply hair removal cream to completely remove the hair. Then, remove the excess with a wet paper towel.
Once the hair has been removed, sterilize the shaved area with povidone-iodine and alcohol swabs. Then, place a surgical drape around the area of incision.
3. Surgery
Just before surgery, adjust the isoflurane vaporizer levels to 1.5%.
Verify that the animal is completely anesthetized by pinching the foot pad.
Next, locate the spleen under the skin. Then using surgical scissors, make a dorsolateral incision 1-2 cm long on the top right of the spleen.
Dissect the retroperitoneum. The pad surrounding the mouse ovary will be observed. Use curved forceps to grasp and expose the fat pad surrounding the mouse ovary.
Hydrate the organ with some drops of sterile PBS.
Use curved forceps to grasp, retract...position...and then secure the ovary for injection
While firmly grasping the ovary with the forceps, inject 10 microliters of MOV1Kat tumor cells into the ovary. A firm grasp will prevent fluid regurgitation or leakage.
Immediately following injection, release the tension exerted by the forceps. The perforation in the ovary should spontaneously retract and close.
Using an absorbable Polyglycolic Acid suture attached to a needle, close the retro-peritoneum wound.
Release the animal from the nose cone.
Stretch the skin and seal the dorsolateral wound edges with few drops of tissue adhesive.
Finally, orally administer 100 microliters of antibiotics to the animal. Then place it back in its cage and monitor for recovery. Keep the animal on antibiotics in the drinking water for one week.
4. In vivo Imaging
One week after the orthotopic injection of MOV1Kat tumor cells, perform in vivo imaging. Begin by transferring an isofluorane anesthetized mouse to the imaging chamber.
Turn the isoflurane vaporizer level down to 2%.
Perform in vivo imaging according to the imaging system manufacturer's instructions. In this video, the Lumina system will be used.
To image, click the Living Image software desktop icon. Then, on the IVIS Acquisition Control Panel, select "Initialize". The instrument settings are analogous to a camera settings
On the acquisition Control Panel set up the instrument's acquisition parameters. For fluorescence, check "Fluorescent." Click the Photograph box to acquire a photograph with each image.
Next, set the exposure time as Auto. Under "Pixel binning or CCD resolution", check "Medium". Then Under F/stop or aperture, check the value of 2. Next, select the 535 excitation filter and the DsRed emission filter.
Under field of view, click on View B to image a single mouse.
Then, click on acquire to begin the image acquisition.
Once the image acquisition is complete, use the Region of Interest, or ROI, tool to measure of the signal. Click on the measurement icon to release the signal values and area.
Finally, click on "save" to save the image in the user folder
After the images have been saved, stop the administration of isoflurane and return the mouse to its cage. The mouse should wake up immediately.
5. Representative Results
-Using this protocol, the in vivo growth of an orthotopic ovarian cancer can be monitored for at least 3 weeks using a non-invasive procedure.
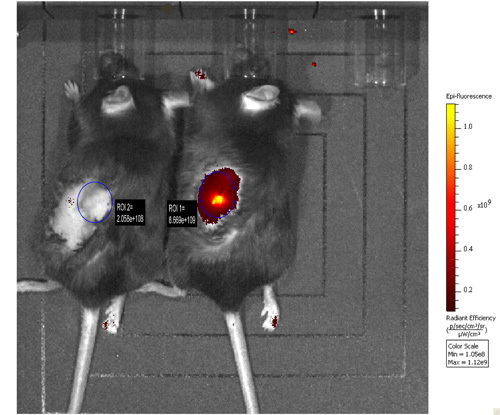 Figure 1. MOV1Kat cells, or PBS as negative control, were orthotopically injected into the ovary of non-tumor prone mice (right animal and left animal and respectively). In vivo imaging was performed 2 weeks later. The fluorescence emission generated by MOV1Kat cells engrafted in the ovary was measured and compared with that from negative control mouse.
Figure 1. MOV1Kat cells, or PBS as negative control, were orthotopically injected into the ovary of non-tumor prone mice (right animal and left animal and respectively). In vivo imaging was performed 2 weeks later. The fluorescence emission generated by MOV1Kat cells engrafted in the ovary was measured and compared with that from negative control mouse.
 Figure 2. Frozen sections of MOV1Kat ovarian tumors were stained with biotinylated anti-CD4 mAb followed by DAB substrate (dark brown) to detect tumor infiltrating lymphocytes (black arrow). Cells were counterstained with methyl-green to visualize cell nuclei (blue). Tumor cells (red arrows) were morphologically distinct from T cells. The slide appears magnified 40x.
Figure 2. Frozen sections of MOV1Kat ovarian tumors were stained with biotinylated anti-CD4 mAb followed by DAB substrate (dark brown) to detect tumor infiltrating lymphocytes (black arrow). Cells were counterstained with methyl-green to visualize cell nuclei (blue). Tumor cells (red arrows) were morphologically distinct from T cells. The slide appears magnified 40x.
Discussion
Surgery and Orthotopic injections
Orthotopic injection in ovarian bursa demands training and precision. Thus
In case of poor surgical experience, practice with cadavers first.
Use preferentially multiparous females (one or two litters) as they develop bigger ovaries over time which facilitates injection and increase survival to compare with nulliparous females.
Due to the small size of the mouse ovarian bursa, the use of the smallest available needle size is strongly encouraged.
In vivo imaging
Always use a reference for fluorescence, such as a 1.5 ml ependorf tube filled with 106 to 107 MOV1kat cells in 100 μl to 1ml of PBS.
Feed the animals with alfalfa-free diet to reduce fluorescence background.
Carefully shave the animal before in vivo imaging to reduce background.
Significance
This syngeneic model of serous ovarian cancer in immunocompetent animals that are orthotopically injected with Far-red fluorescent ovarian cancer cells (MOV1KAT) permits preclinical studies to evaluate novel strategies for imaging and therapy of early tumors, when the disease is still treatable, as well as in vivo monitoring of tumor immune responses and immunotherapies.
Disclosures
No conflicts of interest declared.
Acknowledgments
This work was supported by the NIH grant P01 AI 068730 (SNC, NS), the NIH grant CA016520/ TAPITMAT (NS), the private funding from the Claneil Foundation (NS), and the ovarian SPORE grant to FCCC and University of Pennsylvania (P50 CA83638) and the Fox Chase Cancer Center Core Grant (P30 CA06927) (DCC). The authors thank the excellent technical assistance of the Optical/Bioluminescence Core Facility directed by Dr. E.J. Delikatny at the University of Pennsylvania, Anthony Secreto from the Stem Cell and Xenograft Core directed by Dr. G. Danet-Desnoyers at the University of Pennsylvania Cancer Center for training SNC to orthotopic injection technique and Denada Dangaj at the University of Pennsylvania/ OCRC for assisting on the surgery.
References
- Etzioni R. The case for early detection. Nat Rev Cancer. 2003;3:243–252. doi: 10.1038/nrc1041. [DOI] [PubMed] [Google Scholar]
- Sasaroli D, Coukos G, Scholler N. Beyond CA125: the coming of age of ovarian cancer biomarkers. Are we there yet. Future Medicine. 2009;3:275–288. doi: 10.2217/bmm.09.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson GL. Assessing Lead Time of Selected Ovarian Cancer Biomarkers: A Nested Case Control Study. J Natl Cancer Inst. 2010;102:26–38. doi: 10.1093/jnci/djp438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auersperg N, Wong AS, Choi KC, Kang SK, Leung PC. Ovarian surface epithelium: biology, endocrinology, and pathology. Endocr Rev. 2001;22:255–288. doi: 10.1210/edrv.22.2.0422. [DOI] [PubMed] [Google Scholar]
- Dubeau L. The cell of origin of ovarian epithelial tumours. Lancet Oncol. 2008;9:1191–1197. doi: 10.1016/S1470-2045(08)70308-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly DC. Female mice chimeric for expression of the simian virus 40 TAg under control of the MISIIR promoter develop epithelial ovarian cancer. Cancer Res. 2003;63:1389–1397. [PubMed] [Google Scholar]
- Hensley H. Magnetic resonance imaging for detection and determination of tumor volume in a genetically engineered mouse model of ovarian cancer. Cancer Biol Ther. 2007;6 doi: 10.4161/cbt.6.11.4830. [DOI] [PubMed] [Google Scholar]
- Deliolanis NC. Performance of the red-shifted fluorescent proteins in deep-tissue molecular imaging applications. J Biomed Opt. 2008;13 doi: 10.1117/1.2967184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman RM. A better fluorescent protein for whole-body imaging. Trends Biotechnol. 2008;26 doi: 10.1016/j.tibtech.2007.10.006. [DOI] [PubMed] [Google Scholar]
- Shcherbo D. far-red fluorescent protein for whole-body imaging. Nat Methods. 2007;4:741–746. doi: 10.1038/nmeth1083. [DOI] [PubMed] [Google Scholar]
- Fu X, Hoffman RM. Human ovarian carcinoma metastatic models constructed in nude mice by orthotopic transplantation of histologically-intact patient specimens. Anticancer Res. 1993;13:283–286. [PubMed] [Google Scholar]
- Kiguchi K. A patient-like orthotopic implantation nude mouse model of highly metastatic human ovarian cancer. Clinical & experimental metastasis. 1998;16:751–756. doi: 10.1023/a:1006537013317. [DOI] [PubMed] [Google Scholar]
- Bao R. Activation of cancer-specific gene expression by the survivin promoter. J Natl Cancer Inst. 2002;94:522–528. doi: 10.1093/jnci/94.7.522. [DOI] [PubMed] [Google Scholar]
- Connolly DC, Hensley HH. Xenograft and Transgenic Mouse Models of Epithelial Ovarian Cancer and Non Invasive Imaging Modalities to Monitor Ovarian Tumor Growth In situ -Applications in Evaluating Novel Therapeutic Agents. Current Protocols in Pharmacology. 2009;45:1–36. [PMC free article] [PubMed] [Google Scholar]
- Milne K. Systematic analysis of immune infiltrates in high-grade serous ovarian cancer reveals CD20, FoxP3 and TIA-1 as positive prognostic factors. PLoS ONE. 2009;4 doi: 10.1371/journal.pone.0006412. [DOI] [PMC free article] [PubMed] [Google Scholar]


