Abstract
Fragile X Syndrome (FXS), also known as Martin-Bell Syndrome, is a genetic abnormality found on the X chromosome.1,2 Individuals suffering from FXS display abnormalities in the expression of FMR1 - a protein required for typical, healthy neural development.3 Recent data has suggested that the loss of this protein can cause the cortex to be hyperexcitable thereby affecting overall patterns of neural plasticity.4,5
In addition, Fragile X shows a strong comorbidity with autism: in fact, 30% of children with FXS are diagnosed with autism, and 2 - 5% of autistic children suffer from FXS.6
Transcranial Magnetic Stimulation (a non-invasive neurostimulatory and neuromodulatory technique that can transiently or lastingly modulate cortical excitability via the application of localized magnetic field pulses 7,8) represents a unique method of exploring plasticity and the manifestations of FXS within affected individuals. More specifically, Theta-Burst Stimulation (TBS), a specific stimulatory protocol shown to modulate cortical plasticity for a duration up to 30 minutes after stimulation cessation in healthy populations, has already proven an efficacious tool in the exploration of abnormal plasticity.9,10
Recent studies have shown the effects of TBS last considerably longer in individuals on the autistic spectrum - up to 90 minutes.11 This extended effect-duration suggests an underlying abnormality in the brain's natural plasticity state in autistic individuals - similar to the hyperexcitability induced by Fragile X Syndrome.
In this experiment, utilizing single-pulse motor-evoked potentials (MEPs) as our benchmark, we will explore the effects of both intermittent and continuous TBS on cortical plasticity in individuals suffering from FXS and individuals on the Autistic Spectrum.
Keywords: Neuroscience, Issue 46, Transcranial Magnetic Stimulation, Theta-Burst Stimulation, Neural Plasticity, Fragile X, Autism
Protocol
1. Determine Resting Motor Threshold:
To begin, seat your subject in a comfortable chair.
Next, apply EMG surface electrodes over the first dorsal inerosseus muscle of the subject's right hand. (INSERT FIGURE1) If you are having trouble locating this muscle, ask the subject to make a pinching motion or to move his/her index finger back and forth - this should make the muscle easier to locate.
Place a ground electrode on the meaty portion of the subject's forearm.
Determine the location of the subject's left motor cortex. Although this area differs slightly for everyone, it will generally be around 3.5 cm rostrolateral of cranial vertex. Do not be afraid to explore a small grid around this region and adjust the angle of stimulation until finding the motor "hotspot".
Once you've found M1, starting at 50% power, begin single pulse stimulation to this region and measure the resultant evoked MEPs.
Adjust the power up or down until you are able to produce an MEP of greater than 50 μV on exactly 5 out of 10 consecutive pulses. This power level is the subject's resting motor threshold.
2. Determine Active Motor Threshold
Using the same electrode set-up as described above, ask the subject to pinch his/her right forefinger and thumb together using about 20% pressure.
While the subject holds this pinching position, begin single-pulse stimulation at 50% power over M1 and measure the resultant MEPs.
Adjust the power up or down until you are able to produce an MEP of greater than 200 μV on exactly 5 out of 10 consecutive pulses. This power level is the subject's active motor threshold.
3. Determine Baseline Mep
To determine a subject's baseline MEP amplitude, stimulate motor hotspot at 120% resting motor threshold with 10 single pulses.
Measure the MEP after each pulse.
Average the MEP values from three batches of 10 pulses.
4. Setting TMS Parameters
We will be utilizing standard Theta-Burst parameters: three pulses at 50 Hz at an intensity of 80% active motor threshold for 200 ms intervals.
To administer intermittent TBS, generate a two-second stim train (at the aforementioned parameters) followed by eight-seconds of no stimulation. Repeat for 190 seconds (a total of 600 pulses). iTBS has been shown to facilitate cortical activity.
To administer continuous Theta-Burst, generate an uninterrupted stim train (at the aforementioned parameters) for 47 seconds (a total of 600 pulses). cTBS has been shown to inhibit cortical activity.
5. Tms Stimulation
For this protocol, administer either iTBS or cTBS over the earlier established M1 motor hotspot.
6. Determine Post-stimulation MEP
Following TBS, as before, stimulate motor hotspot at 120% resting motor threshold with 10 single-pulses.
Average the batch of 10 MEP levels.
Collect new 10-pulse batch averages at 5 minutes, 10 minutes, 20, 30, 40, 50, 60, 75, 90, 105, and 120 minutes post-stimulation.
7. Representative Results
When utilizing an iTBS pattern, you should notice an increase in MEP values for a duration reflecting the subject's natural state of plasticity. Likewise, when utilizing a cTBS pattern, you should notice a decrease in MEP values for a duration reflecting the subject's natural state of plasticity.
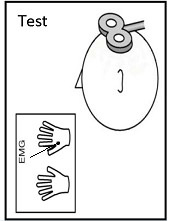 Figure 1. Diagram of electrode placement for MEP measurement.
Figure 1. Diagram of electrode placement for MEP measurement.
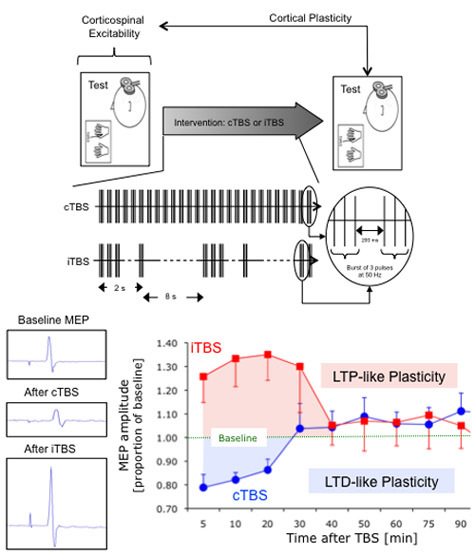 Figure 2. Diagram of the iTBS stimulation pattern.
Figure 2. Diagram of the iTBS stimulation pattern.
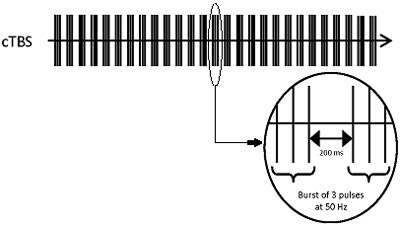 Figure 3. Diagram of the cTBS stimulation pattern.
Figure 3. Diagram of the cTBS stimulation pattern.
Discussion
Knowing that prolonged duration of TMS after-effects is reflective of atypical neural plasticity, studies such as this could serve to create better and more precise diagnostic protocols for Autism and related disorders.
Similarly, with more data, we may be able to find temporal biological markers for other neurological pathologies - including Fragile X syndrome. In this case, although there is not yet a therapeutic remediation option, early detection could help parents and educators determine best practices for their own child's unique developmental trajectory.
Disclosures
No conflicts of interest declared.
References
- Pfeiffer BE, Huber KM. The state of synapses in fragile x syndrome. Neuroscientist. 2009;15:549–567. doi: 10.1177/1073858409333075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Donnel WT, Warren ST. A decade of molecular studies of fragile x syndrome. Annual Review of Neuroscience. 2002;25:315–338. doi: 10.1146/annurev.neuro.25.112701.142909. [DOI] [PubMed] [Google Scholar]
- Tassone F, Hagerman RJ, Taylor AK, Mills JB, Wood S, Gane LW, Hagerman PJ. American Journal of Human Genetics. 1999;65:A493–A493. [Google Scholar]
- Hagerman RJ, Miller LJ, McGrath-Clarke J, Riley K, Goldson E, Harris SW, Simon J, Church K, Bonnell J, Ognibene TC, McIntosh DN. Influence of stimulants on electrodermal studies in fragile x syndrome. Microscopy Research and Technique. 2002;57:168–173. doi: 10.1002/jemt.10067. [DOI] [PubMed] [Google Scholar]
- Miller LJ, McIntosh DN, McGrath J, Shyu V, Lampe M, Taylor AK, Tassone F, Neitzel K, Stackhouse T, Hagerman RJ. Electrodermal response to sensory stimuli in individuals with fragile x syndrome: a preliminary report. American Journal of Medical Genetics. 1999;83:268–279. [PubMed] [Google Scholar]
- Hagerman RJ. Fragile X: perspectives from birth through aging. Biological Psychiatry. 2005;57:73s–73s. [Google Scholar]
- Pascual-Leone A, Davey M, Wassermann EM, Rothwell J, Puri B, editors. Handbook of Transcranial Magnetic Stimulation. London: Edward Arnold; 2002. [Google Scholar]
- Walsh V, Pascual-Leone A. Transcranial Magnetic Stimulation: A Neurochronometrics of Mind. Cambridge: MIT Press; 2005. [Google Scholar]
- Thickbroom GW. Transcranial magnetic stimulation and synaptic plasticity: experimental framework and human models. Experimental Brain Research. 2007;180:583–593. doi: 10.1007/s00221-007-0991-3. [DOI] [PubMed] [Google Scholar]
- Huang YZ, Edwards MJ, Rounis E, Bhatia KP, Rothwell JC. Theta burst stimulation of the human motor cortex. Neuron. 2005;45:201–206. doi: 10.1016/j.neuron.2004.12.033. [DOI] [PubMed] [Google Scholar]
- Oberman L, Eldaief MC, Gautam S, Fecteau S, Tormos JM. Abnormal Cortical Plasticity in Adults with Asperger's Syndrome. Forthcoming.


