Abstract
Background
More physician years in practice have been associated with less frequent guideline adherence, but it is unknown whether years in practice are associated with patient outcomes.
Methods
We examined all inpatients on the teaching service of an urban hospital from 7/1/02 through 6/30/04. Admissions were assigned to attending physicians quasi-randomly. Years in practice was defined as the number of years the attending physician held a medical license. We divided physicians into 4 groups (0–5, 6–10, 11–20, and > 20 years in practice), and used negative binomial and logistic regression to adjust for patient characteristics and estimate associations between years in practice and length-of-stay, readmission, and mortality.
Results
59 physicians and 6,572 admissions were examined. Though the four inpatient groups had similar demographic and clinical characteristics, physicians with more years in practice had longer mean lengths-of-stay (4.77, 5.29, 5.42, and 5.31 days for physicians with 0–5, 6–10, 11–20, and >20 years in practice respectively, p = 0.001). After adjustment, inpatients of physicians with more than 20 years in practice had higher risk for both in-hospital mortality (OR = 1.71, 95% CI: 1.06–2.76) and 30-day mortality (OR = 1.51, 95% CI: 1.06–2.16) than inpatients of physicians with 0–5 years in practice.
Conclusion
Inpatient care by physicians with more years in practice is associated with higher risk of mortality. Quality of care interventions should be developed to maintain inpatient skills for physicians.
Keywords: Physician Experience, Length-of-stay, Outcomes, Hospital Medicine
INTRODUCTION
It is difficult to measure whether quality of care changes over the course of a physician’s career. More years in practice among physicians have been associated with decreased medical knowledge1–3 and less frequent adherence to standards of care,4–6 but these measures do not assess quality of care. Because efforts to measure associations between physician years in practice and patient outcomes have had conflicting results7–11 and often compared dissimilar patient groups,12, 13 it is unknown how physician years in practice affect the most appropriate measures of quality: patient outcomes.
Recognizing a public interest in maintaining quality care, the American Board of Internal Medicine has required that internists initially boarded after 1989 recertify every ten years. Although internists with many years in practice are exempt from internal medicine recertification, there are few data to support this policy and little is known about whether physicians exempt from recertification continue to offer high quality care.
A necessary component of high quality care is efficient management of complex medical inpatients. Over the last twenty years, the complexity of diagnostic work-ups and treatment plans associated with inpatient care has increased,14 while average length-of-stay has decreased.15 Internists who trained in the current era of high inpatient acuity and rapid turnover may feel more comfortable caring for inpatients than those who trained earlier.
Several other physician attributes have been associated with patient outcomes, including care by hospitalists (inpatient specialists), which has been associated with both shorter length-of-stay,16–19 and lower mortality.16, 17 More inpatient experience has also been associated with shorter length-of-stay and lower mortality.16 However, it is unknown whether more years in practice adversely affect either length-of-stay or outcomes of care.
Our objective was to determine the effect of physician years in practice on length-of-stay and three patient outcomes (30-day readmission, in-hospital mortality, and 30-day mortality) on the teaching service of an academic teaching hospital. We hypothesized that more physician years in practice are associated with longer length-of-stay and higher mortality.
METHODS
Study Setting, Design, and Population
Study Setting
Weiler Hospital is a 381-bed hospital that is one of two hospitals comprising Montefiore Medical Center, the primary teaching site of the Albert Einstein College of Medicine of Yeshiva University. We examined all admissions to Weiler Hospital’s general medical teaching service from 7/1/02 through 6/30/04.
Study Design
We used a quasi-experimental design to take advantage of a naturally occurring experiment occurring at Weiler. Patients are assigned to one of six identical teams at the time of admission by the admitting resident. Each team consists of one attending, one senior resident, two interns, one sub-intern, and a third-year medical student. Patients assigned to hospitalist-run non-teaching teams were excluded. Although teaching team assignment appears random, because concealed allocation does not occur we consider this a quasi-randomized design.18, 20
Study Population
Because we suspected that attending physicians might behave differently with their established patients in ways that could confound our analysis, we excluded inpatients with prior contact with the attending physician to whose team they were assigned. In addition, because many patients had more than one admission during the study period, we have used the term admission rather than patient to describe our unit of analysis.
Outcome Variables
Our outcome variables were: length-of-stay, 30-day readmission, and in-hospital and 30-day mortality. Length-of-stay was analyzed as a continuous variable and, although not normally distributed, is reported as a mean (as has been done previously).16, 18, 21, 22 Readmission was defined as an admission for any reason, within 30 days of discharge, to either of the two hospitals captured in Montefiore’s Clinical Information System. Readmission outside Montefiore occurs rarely (1.9% of discharges). Readmission, in-hospital and 30-day mortality were analyzed as dichotomous variables.
Outcome and other admission-level data (described below) were extracted using Clinical Looking Glass,™ a quality improvement health care surveillance software.23 Mortality data were obtained from the social security death registry.
Major Independent Variable
The major independent variable was the number of years in practice of the attending physician to whom the admission was assigned. This was defined as the time elapsed from the date of New York State licensure to the date of admission, and categorized a priori into four groups: 0–5 years, 6–10 years, 11–20 years, and >20 years.
The analyses were then repeated with physician years in practice defined as years since medical school graduation. To maintain four similarly sized groups, the groups were: 0–7 years, 8–12 years, 13–22 years, and > 22 years in practice.
Date of licensure and year of medical school graduation were obtained from the New York State Physician Profile Website.24
Physician-level Covariates
In addition to number of years in practice, we considered two other covariates to assess physician-level confounding: (1) whether or not the attending physician was a hospitalist (a physician who devotes more than 50% time to inpatient care), and (2) inpatient experience. To quantify inpatient experience, we calculated the total number of admissions for each physician over the two-year study period. We then dichotomized at the physician median (84 admissions) to categorize physicians as high or low inpatient volume.
Admission-level covariates
We included the following admission-level covariates: demographic characteristics, insurance, number of admissions within the previous 90 days, admission albumin, diabetes diagnosis, DRG-weight, and primary discharge diagnosis (ICD-9 code). Albumin and DRG-weight (a numeric billing code summarizing the total utilization associated with the admission) were used as surrogates for overall illness severity.16, 18, 25–28
We also used two common risk adjustment tools (Charlson score29 and Elixhauser30) to measure overall co-morbidity. Charlson score was analyzed as both a continuous variable, and dichotomized at the admission median (median score = 1). Admissions were thus defined as complex (Charlson >1) or less complex (Charlson ≤1).
ICD-9 codes were grouped into diagnosis clusters using the Healthcare Cost and Utilization Project of the Agency for Healthcare Research and Quality system.31
Statistical Analysis
Admission groups
First, the four admission groups were constructed based on years in practice of the physician (0–5 years, 6–10 years, 11–20 years, or >20 years). Then, patient characteristics were compared, using analysis of variance, Kruskal-Wallis, or chi-square tests.
Physician years in practice and length-of-stay
To assess univariate association between physician years in practice and length-of-stay, we used Somers’ D as a rank-based test,32 with standard errors robust to clustering of admissions within physicians. We repeated this analysis with and without truncation of length-of-stay to the mean plus three standard deviations (24 days), to assess the influence of long length-of-stay outliers, and including only the first admission for each patient, to assess the influence of patients returning for several admissions.
We then assessed the association between physician years in practice and length-of-stay after adjusting for both physician-level and admission-level covariates, using a multivariate negative binomial regression model. Negative binomial regression is appropriate when the dependent variable (e.g. length-of-stay), is skewed and overdispersed. To determine if the association between years in practice and length-of-stay is consistent among physicians with different levels of inpatient volume, we also examined how interactions between years in practice and inpatient volume affected length-of-stay. Because we observed a significant interaction, we performed a post-hoc analysis, stratified by physician inpatient volume.
Physician years in practice and clinical outcomes: readmission and mortality
To assess the association between physician years in practice and the dichotomous outcomes of readmission and both in-hospital and 30-day mortality, we initially compared rates of these outcomes between the four admission groups, using chi-square tests.
Before constructing multivariate models, we first determined that the physician random effect did not improve the model according to Akaike’s information criterion,33 so further analyses ignored heterogeneity among physicians. We therefore constructed multivariate logistic regression models to assess the independent impact of physician years in practice on 30-day readmission, inpatient mortality, and 30-day mortality, after adjusting for both physician-level and admission-level covariates. Similar models were constructed for each outcome. We initially chose variables for multivariate analysis that were significantly different between the four admission groups, then added other variables, keeping those with a Wald-statistic p < 0.20. Variables were excluded from our models if they were not associated with the outcome, or were co-linear with other independent variables. Variables that were measurable only at the time of discharge (i.e. DRG-weight, ICD-9 code) may reflect the outcome of care rather than an attribute of the admission, and thus were not included in multivariate analyses.
To assess whether the observed association between physician years in practice and mortality was similar among admissions of different complexity, we performed a second post-hoc analysis stratified by the Charlson co-morbidity score: complex admissions (Charlson score >1) and less complex admissions (Charlson score ≤1).
STATA/IC software, version 10.0,34 was used for all analyses. Montefiore’s IRB approved the study.
RESULTS
Admission groups
From 7/1/02 through 6/30/04 there were 9,047 admissions to Weiler’s general medical teaching service. Of these, 2,465 were patients with a previous encounter with the attending physician to whose team they were assigned, and significant data were missing on 10 admissions, leaving a study sample of 6,572. This included 2,483 admissions (37.8%) assigned to physicians with 0–5 years in practice, 1,659 (25.2%) to physicians with 6–10 years in practice, 1,139 (17.3%) to physicians with 11–20 years in practice, and 1,291 (19.6%) to physicians with >20 years in practice.
The four admission groups were similar with respect to age, sex, race, insurance, proportion with diabetes, albumin level, Charlson score, Elixhauser diagnoses, and DRG-weight. The mix of ICD-9 diagnoses was similar between the four groups. (Table 1).
Table 1.
Characteristics of Patients Grouped by Physician Years in Practice
| Years in practice | All | 0–5yrs | 6–10yrs | 11–20yrs | >20yrs | |
|---|---|---|---|---|---|---|
| No. of patients | (n=6572) | (n=2483) | (n=1659) | (n=1139) | (n=1291) | |
| No. of doctors | (n=59) | (n=14) | (n=12) | (n=14) | (n=19) | p value |
| Demographic Characteristics | ||||||
| Age- mean ± SD | 63.4 ± 18.1 | 64.0 ± 18.0 | 62.9 ± 17.7 | 63.8 ± 18.4 | 62.4 ± 18.4 | 0.03 |
| Male- no.(%) | 2732 (41.6) | 1012 (40.9) | 721 (42.1) | 475 (41.3) | 524 (42.3) | 0.82 |
| Race-Ethnicity No. (%) | 0.25 | |||||
| White | 1519 (23.1) | 558 (22.6) | 382 (22.3) | 284 (24.7) | 295 (23.8) | |
| Black | 1935 (29.4) | 729 (29.5) | 526 (30.7) | 340 (29.6) | 340 (27.5) | |
| Hispanic | 2370 (36.1) | 915 (37.0) | 588 (34.4) | 406 (35.3) | 461 (37.2) | |
| Unknown/Other | 748 (11.4) | 271 (11.0) | 216 (12.6) | 119 (10.4) | 142 (11.5) | |
| Insurance No. (%) | 0.53 | |||||
| Self-Pay | 73 (1.1) | 25 (1.0) | 19 (1.1) | 13 (1.1) | 16 (1.3) | |
| Medicaid | 2483 (37.8) | 936 (37.9) | 652 (38.1) | 422 (36.7) | 473 (38.2) | |
| Medicare | 2573 (39.2) | 976 (39.5) | 636 (37.2) | 478 (41.6) | 483 (39.1) | |
| Commercial | 1440 (21.9) | 534 (21.6) | 404 (23.6) | 236 (20.5) | 266 (21.5) | |
| Clinical Characteristics | ||||||
| Diabetes no. (%) | 2289 (34.8) | 838 (33.9) | 607 (35.4) | 424 (36.9) | 420 (33.9) | 0.28 |
| Prior Admit no. (%) | 1603 (24.4) | 630 (25.5) | 420 (24.5) | 260 (22.6) | 293 (23.7) | 0.27 |
| Albumin mean ± SD | 3.82 ± 0.67 | 3.81 ± 0.67 | 3.80 ± 0.69 | 3.82 ± 0.66 | 3.86 ± 0.68 | 0.12 |
| DRG-weight (median) | 0.90 | 0.90 | 0.90 | 0.92 | 0.90 | 0.84 |
| Charlson score | 1.98 ± 2.07 | 1.97 ± 2.03 | 1.98 ± 2.06 | 2.01 ± 2.11 | 1.97 ± 2.11 | 0.89 |
| # Elixhauser co-morbidities | 2.44 ± 1.56 | 2.45 ± 1.56 | 2.46 ± 1.58 | 2.49 ± 1.59 | 2.35 ± 1.50 | 0.28 |
| Diagnosis† No. (%) | ||||||
| Acute MI | 355 (5.4) | 134 (5.4) | 87 (5.1) | 63 (5.5) | 71 (5.7) | 0.89 |
| Acid-Peptic Disease | 146 (2.2) | 65 (2.6) | 28 (1.6) | 19 (1.7) | 34 (2.8) | 0.05 |
| Anemia | 68 (1.0) | 25 (1.0) | 15 (0.9) | 14 (1.2) | 14 (1.1) | 0.82 |
| Arrhthmia | 197 (3.0) | 71 (2.9) | 43 (2.5) | 40 (3.5) | 43 (3.5) | 0.33 |
| Asthma | 379 (5.8) | 158 (6.4) | 92 (5.4) | 60 (5.2) | 69 (5.6) | 0.40 |
| Coronary Artery Disease, no Infarct | 331 (5.0) | 122 (4.9) | 87 (5.1) | 46 (4.0) | 76 (6.1) | 0.12 |
| Congestive Heart Failure | 581 (8.8) | 212 (8.6) | 158 (9.2) | 111 (9.7) | 100 (8.1) | 0.49 |
| Acute CVA | 81 (1.2) | 32 (1.3) | 22 (1.3) | 14 (1.2) | 13 (1.1) | 0.93 |
| Cellulitis | 128 (2.0) | 58 (2.4) | 34 (2.0) | 20 (1.7) | 16 (1.3) | 0.16 |
| Chest Pain | 587 (8.9) | 197 (8.0) | 162 (9.5) | 123 (10.7) | 105 (8.5) | 0.04 |
| Complications: Surgery | 87 (1.3) | 30 (1.2) | 23 (1.3) | 12 (1.0) | 22 (1.8) | 0.41 |
| Diabetic Complications | 237 (3.6) | 75 (3.0) | 68 (4.0) | 39 (3.4) | 55 (4.4) | 0.13 |
| Enteritis | 135 (2.1) | 54 (2.2) | 33 (1.9) | 23 (2.0) | 25 (2.0) | 0.95 |
| Fluid/Electrolyte Disorders | 138 (2.1) | 53 (2.1) | 33 (1.9) | 19 (1.7) | 33 (2.7) | 0.35 |
| GI Bleeding | 160 (2.4) | 60 (2.4) | 41 (2.4) | 28 (2.4) | 31 (2.5) | 1.00 |
| HIV | 106 (1.6) | 40 (1.6) | 26 (1.5) | 19 (1.7) | 21 (1.7) | 0.98 |
| Hepatic Disease | 127 (1.9) | 47 (1.9) | 28 (1.6) | 18 (1.6) | 34 (2.8) | 0.11 |
| Neoplasm | 143 (2.2) | 50 (2.0) | 41 (2.4) | 26 (2.3) | 26 (2.1) | 0.86 |
| Pancreatitis | 61 (0.9) | 27 (1.1) | 17 (1.0) | 6 (0.5) | 11 (0.9) | 0.41 |
| Pneumonia | 428 (6.5) | 165 (6.7) | 108 (6.3) | 77 (6.7) | 78 (6.3) | 0.94 |
| Renal Failure | 129 (2.0) | 49 (2.0) | 37 (2.2) | 26 (2.3) | 17 (1.4) | 0.37 |
| SS Disease with Crisis | 32 (0.5) | 10 (0.4) | 11 (0.6) | 5 (0.4) | 6 (0.5) | 0.74 |
| Sepsis | 142 (2.2) | 44 (1.8) | 43 (2.5) | 21 (1.8) | 34 (2.8) | 0.15 |
| Syncope | 196 (3.0) | 78 (3.2) | 54 (3.2) | 38 (3.3) | 26 (2.1) | 0.24 |
| Thromboembolic Disease | 88 (1.3) | 36 (1.5) | 20 (1.2) | 17 (1.5) | 15 (1.2) | 0.81 |
| Urinary Tract Infection | 171 (2.6) | 80 (3.2) | 46 (2.7) | 22 (1.9) | 23 (1.9) | 0.03 |
| Other Diagnosis | 1339 (20.4) | 501 (20.3) | 355 (20.7) | 243 (21.2) | 240 (19.4) | 0.72 |
Years in practice = year of admission minus year granted New York State License
Continuous variables reported as mean ± standard deviation and groups compared using one-way ANOVA.
Categorical variables reported as number (percent) and compared using χ2.
Medians of age, DRG-weight, Charlson score, and number of Elixhauser co-morbidities compared using Kruskal-Wallis.
For zero-sum variables race-ethnicity and insurance, χ2 reported for whole group.
DRG-weight is a numeric summary measure of overall utilization used for billing.
Diagnoses grouped by ICD-9 code according to clinical classifications by the Agency for Healthcare Research and Quality, and collapsed into clinical categories.
Physician years in practice and length-of-stay
Univariate analysis (Table 2) revealed that mean length-of-stay was shortest (4.77 days) for admissions assigned to physicians with 0–5 years in practice, compared with 5.29 days for admissions to physicians with 6–10 years in practice, 5.42 days for admissions to physicians with 11–20 years in practice, and 5.31 days for admissions to physicians with >20 years in practice (cluster-robust p value = 0.001 for the difference between the groups). After truncating length-of-stay to reduce the effect of outliers, and restricting the analysis to first-admissions to eliminate the effect of multiple admissions per patient, more physician years in practice remained significantly associated with longer length-of-stay (p = 0.003).
Table 2.
Mean Length-of-Stay (LOS) Grouped by Physician Years in Practice
| Years in practice | 0–5years | 6–10years | 11–20years | >20years | |
|---|---|---|---|---|---|
| All admissions | |||||
| No. of patients | (n=2483) | (n=1659) | (n=1139) | (n=1291) | |
| No. of doctors | (n=14) | (n=12) | (n=14) | (n=19) | p value* |
| LOS, mean ± SD, days | 4.77 ± 6.32 | 5.29 ± 6.47 | 5.42 ± 6.41 | 5.31 ± 5.72 | 0.001 |
| Truncated LOS†, mean ± SD, days | 4.53 ± 4.67 | 5.03 ± 4.79 | 5.16 ± 4.82 | 5.11 ± 4.57 | 0.001 |
| First admissions | |||||
| No. of patients | (n=1794) | (n=1282) | (n=895) | (n=949) | |
| No. of doctors | (n=14) | (n=12) | (n=14) | (n=19) | p value* |
| LOS, mean ± SD, days | 4.64 ± 6.30 | 5.30 ± 6.81 | 5.21 ± 5.98 | 5.13 ± 5.62 | 0.003 |
| Truncated LOS†, mean ± SD, days | 4.43 ± 4.65 | 4.99 ± 4.82 | 4.99 ± 4.59 | 4.94 ± 4.53 | 0.003 |
Years in practice = year of admission minus year granted New York State License
Rank-based testing using Somers' D robust to clusters of patients by physician
Length of stay was truncated at mean + 3 SDs (24 days).
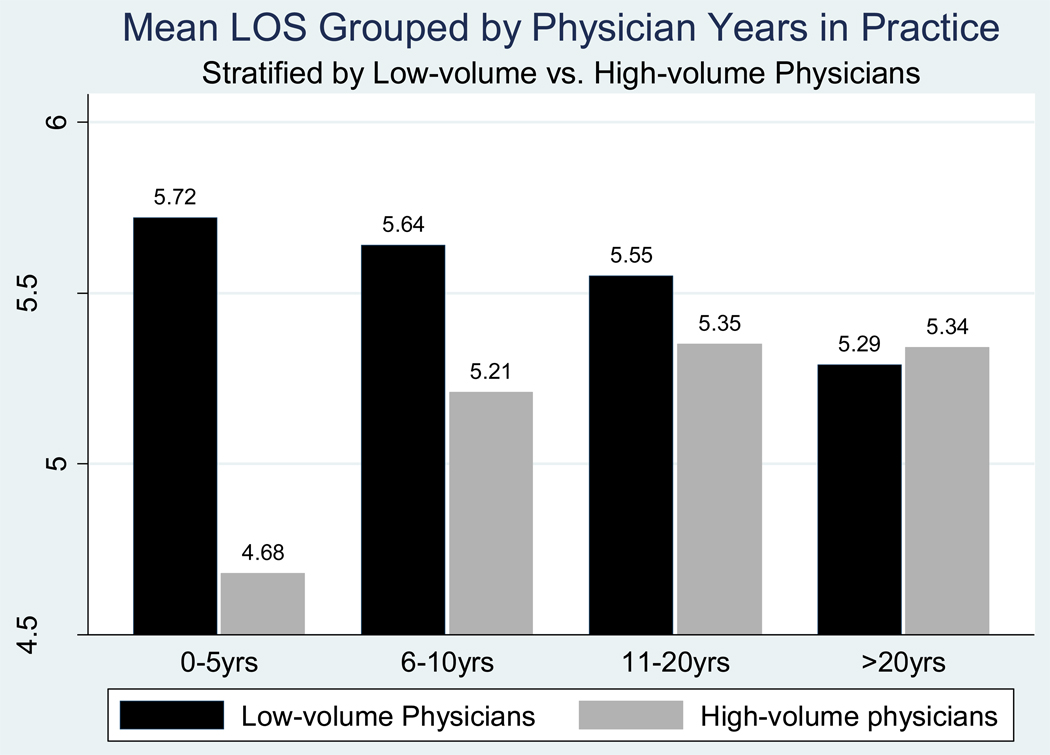
We also demonstrated that more physician years in practice affected length-of-stay differently, depending on whether the physician had high or low inpatient volume (Figure; p for interaction < 0.001). Among low volume physicians, we did not observe an association between years in practice and length-of-stay (p = 0.98). However, among high volume physicians, more years in practice was associated with longer length-of-stay (cluster-robust p value = 0.002 for the difference between the groups).
Figure.
After adjustment for admission-level covariates (sex, race/ethnicity, insurance, albumin, and Charlson co-morbidity score), more years in practice remained significantly associated with longer length-of-stay for physicians with high inpatient volume, but not for physicians with low inpatient volume. Because these analysis were performed using negative binomial regression and the results are reported as incidence rate ratios,35 we have included them in an appendix.
Years in practice and readmission and mortality rates
Social security mortality data were available for 97.7% of admissions. Univariate analysis revealed no significant differences in 30-day readmission, inpatient mortality, or 30-day mortality rates between the four groups. Multivariate associations between physician years in practice and both readmission and mortality rates are shown in Table 4, and also demonstrate no significant differences in 30-day readmission rates between the four groups. However, after adjustment for admission-level factors and whether the physician was a hospitalist, admissions assigned to physicians with >20 years in practice had a higher risk of both in-hospital mortality (OR = 1.71, 95% CI 1.06 – 2.76), and 30-day mortality (OR = 1.51, 95% CI: 1.06 – 2.16), compared to admissions assigned to physicians with 0–5 years in practice. When we repeated the multivariate analyses with physician years in practice defined based on years since medical school graduation, the results were similar.
We found that the increased mortality risk associated with more years in practice was limited to more complex admissions. Among less complex admissions (Charlson score ≤1), those assigned to physicians with more than 20 years in practice did not have a higher risk of in-hospital (OR 0.73, 95% CI 0.29 – 1.81) or 30-day mortality (OR 1.04, 95% CI 0.48 – 2.25) compared to those assigned to the 0–5 year group. However, among more complex admissions (Charlson score >1), we observed higher in-hospital (OR 2.34, 95% CI 1.30 – 4.31) and 30-day mortality (OR 1.75, 95% CI 1.13 – 2.70) for those assigned to physicians with more than 20 years in practice, compared to those assigned to the 0–5 year group.
DISCUSSION
We found a significant association between care by physicians with more years in practice and longer lengths of stay. In addition, after careful adjustment, we found significantly higher in-hospital and 30-day mortality in admissions cared for by physicians with the most years in practice. This finding persisted whether we defined years in practice as years since obtaining licensure, or years since medical school graduation. In post hoc analysis, we found that the mortality risk associated with being cared for by a physician with more years in practice was higher only among medically complex admissions.
Several studies have found an association between inpatient experience and shorter length-of-stay,16–19 but few have examined physician years in practice as a measure of experience. In our study, physicians with more years in practice had longer length-of-stay overall, but this association was not consistent among all physicians. Among high volume physicians, more years in practice was associated with longer length-of-stay; however, low-volume physicians showed the opposite effect: more years in practice was associated with shorter length-of-stay. As our study was not longitudinal, we were unable to determine if physician length-of-stay changes over time, or whether physician length-of-stay is relatively constant. If physician length-of-stay changes over time, there are several plausible explanations for the association between more years in practice and longer length-of-stay. High-volume physicians may suffer “burn-out” and become less efficient after years of inpatient practice, accounting for longer length-of-stay in later years. Low-volume physicians may need to acquire years of experience before they are able to offer efficient care, and their length-of-stay may therefore be long initially but shorter over time. If physician length-of-stay does not change over time, then it is possible that a physician’s length-of-stay reflects attention paid to length-of-stay during residency training. It is likely that physicians with the most years in practice trained earlier, when maintaining shorter length-of-stay was not a priority.
Although we found that admissions assigned to physicians with the most years in practice had higher mortality, this finding was not consistent among all admission groups. While we found no significant association between more physician years in practice and mortality in less medically complex admissions, we observed a significant association between more physician years in practice and higher mortality among medically complex admissions.
Because our study is not longitudinal we cannot determine if physician inpatient skills change over time, or remain relatively constant. It is possible that physician inpatient skills erode over time, resulting in worsening quality of care for complex hospitalized patients, and higher mortality. It is also possible that the knowledge and skills physicians acquire during their training remain intact, but that these clinical tools become less relevant to the care of complex inpatients as medical advances accumulate. Further research is needed to determine if interventions can close the gap in quality of care among physicians with many years in practice. One such intervention would be extension of recertification requirements to all physicians. Physicians with the highest mortality in this study (physicians with > 20 years in practice) are currently exempt from recertification.
Our study has some limitations. It is possible that unmeasured differences between patient groups resulted in residual confounding. In particular, older physicians are more likely to care for older, sicker, patients, with an increased risk of mortality but we minimized this effect by excluding patients with any prior relationship with the assigned physician. Because our four admission groups were so similar, we believe that our attempts to minimize selection bias were largely successful. To further minimize confounding, we adjusted for admission- and physician-level covariates, but did not assess use of specialty consultation, which may affect patient outcomes. Lastly, our data were drawn from a single institution, our sample of attending physicians is small (n = 59), and it may not represent all physicians.
In conclusion, in an urban teaching hospital, more years of physician experience are associated with longer length-of-stay and a higher risk of both in-hospital and 30-day mortality. Quality of care interventions should be developed to assist physicians to maintain inpatient skills throughout their careers, and that consideration should be given to the extension of recertification requirements to all physicians.
Supplementary Material
Table 3.
Readmission and Mortality Grouped By Physician Years in Practice
| Years in practice | 0–5 years | 6–10 years | 11–20 years | >20 years |
|---|---|---|---|---|
| No. of patients | (n=2483) | (n=1659) | (n=1139) | (n=1291) |
| No. of doctors | (n=14) | (n=12) | (n=14) | (n=19) |
| 30-Day Readmission | ref = 1.00 | 0.95 (0.82 – 1.10) | 0.92 (0.71 – 1.20) | 0.90 (0.71 – 1.13) |
| In-Hospital Mortality | ref = 1.00 | 1.14 (0.77 – 1.69) | 1.28 (0.83 – 2.00) | 1.71 (1.06 – 2.76) |
| 30-Day Mortality* | ref = 1.00 | 1.14 (0.90 – 1.46) | 1.11 (0.79 – 1.55) | 1.51 (1.06 – 2.16) |
Years in practice = year of admission minus year granted New York State License
Odds Ratios (95% confidence intervals) for events using 0–5 years experience as reference
Adjusted for age, sex, race-ethnicity, insurance, diabetes, admission albumin, Charlson co-morbidity score, prior admission, hospitalist physician
95% confidence intervals calculated using standard errors robust to clusters of patients by physician
30-day mortality taken from social security death registry using social security number matching.
Acknowledgements
We would like to thank Lori Ashton and Matthew Berger for programming support, and Phil Lief and Charles Hall for comments on the study design and analysis.
Financial support: This work was supported by the CTSA Grant UL1 RR025750 and KL2 RR025749 and TL1 RR025748 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and the Clinical Investigation Core of the Center for AIDS Research at the Albert Einstein College of Medicine and Montefiore Medical Center, funded by the National Institutes of Health (NIH P30 AI51519).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: the authors have no conflicts of interest to report
Reference List
- 1.Golden NH, Seigel WM, Fisher M, et al. Emergency contraception: pediatricians' knowledge, attitudes, and opinions. Pediatrics. 2001 February;107(2):287–292. doi: 10.1542/peds.107.2.287. [DOI] [PubMed] [Google Scholar]
- 2.Schroen AT, Detterbeck FC, Crawford R, Rivera MP, Socinski MA. Beliefs among pulmonologists and thoracic surgeons in the therapeutic approach to non-small cell lung cancer. Chest. 2000 July;118(1):129–137. doi: 10.1378/chest.118.1.129. [DOI] [PubMed] [Google Scholar]
- 3.Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005 February 15;142(4):260–273. doi: 10.7326/0003-4819-142-4-200502150-00008. [DOI] [PubMed] [Google Scholar]
- 4.Moride Y, Du Fort GG, Monette J, et al. Suboptimal duration of antidepressant treatments in the older ambulatory population of Quebec: association with selected physician characteristics. J Am Geriatr Soc. 2002 August;50(8):1365–1371. doi: 10.1046/j.1532-5415.2002.50357.x. [DOI] [PubMed] [Google Scholar]
- 5.Dhalla IA, Anderson GM, Mamdani MM, Bronskill SE, Sykora K, Rochon PA. Inappropriate prescribing before and after nursing home admission. J Am Geriatr Soc. 2002 June;50(6):995–1000. doi: 10.1046/j.1532-5415.2002.50252.x. [DOI] [PubMed] [Google Scholar]
- 6.Fehrenbach SN, Budnitz DS, Gazmararian JA, Krumholz HM. Physician characteristics and the initiation of beta-adrenergic blocking agent therapy after acute myocardial infarction in a managed care population. Am J Manag Care. 2001 July;7(7):717–723. [PubMed] [Google Scholar]
- 7.Norcini JJ, Kimball HR, Lipner RS. Certification and specialization: do they matter in the outcome of acute myocardial infarction? Acad Med. 2000 December;75(12):1193–1198. doi: 10.1097/00001888-200012000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Blanc PD, Trupin L, Earnest G, et al. Effects of physician-related factors on adult asthma care, health status, and quality of life. Am J Med. 2003 May;114(7):581–587. doi: 10.1016/s0002-9343(03)00053-6. [DOI] [PubMed] [Google Scholar]
- 9.O'Neill L, Lanska DJ, Hartz A. Surgeon characteristics associated with mortality and morbidity following carotid endarterectomy. Neurology. 2000 September 26;55(6):773–781. doi: 10.1212/wnl.55.6.773. [DOI] [PubMed] [Google Scholar]
- 10.Hartz AJ, Kuhn EM, Pulido J. Prestige of training programs and experience of bypass surgeons as factors in adjusted patient mortality rates. Med Care. 1999 January;37(1):93–103. doi: 10.1097/00005650-199901000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Katon W, Rutter CM, Lin E, et al. Are there detectable differences in quality of care or outcome of depression across primary care providers? Med Care. 2000 June;38(6):552–561. doi: 10.1097/00005650-200006000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Davidson W, Molloy DW, Bedard M. Physician characteristics and prescribing for elderly people in New Brunswick: relation to patient outcomes. CMAJ. 1995 April 15;152(8):1227–1234. [PMC free article] [PubMed] [Google Scholar]
- 13.Burns LR, Wholey DR. The effects of patient, hospital, and physician characteristics on length of stay and mortality. Med Care. 1991 March;29(3):251–271. doi: 10.1097/00005650-199103000-00007. [DOI] [PubMed] [Google Scholar]
- 14.2005–2006 Society of Hospital Medicine Survey: State of the Hospital Medicine Movement. 2006 [Google Scholar]
- 15.Baker DW, Einstadter D, Husak SS, Cebul RD. Trends in postdischarge mortality and readmissions: has length of stay declined too far? Arch Intern Med. 2004 March 8;164(5):538–544. doi: 10.1001/archinte.164.5.538. [DOI] [PubMed] [Google Scholar]
- 16.Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002 December 3;137(11):866–874. doi: 10.7326/0003-4819-137-11-200212030-00007. [DOI] [PubMed] [Google Scholar]
- 17.Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002 December 3;137(11):859–865. doi: 10.7326/0003-4819-137-11-200212030-00006. [DOI] [PubMed] [Google Scholar]
- 18.Southern WN, Berger MA, Bellin EY, Hailpern SM, Arnsten JH. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2007 September 24;167(17):1869–1874. doi: 10.1001/archinte.167.17.1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007 December;357(25):2589–2600. doi: 10.1056/NEJMsa067735. %20. [DOI] [PubMed] [Google Scholar]
- 20.Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002 January 23;287(4):487–494. doi: 10.1001/jama.287.4.487. [DOI] [PubMed] [Google Scholar]
- 21.Craig DE, Hartka L, Likosky WH, Caplan WM, Litsky P, Smithey J. Implementation of a hospitalist system in a large health maintenance organization: the Kaiser Permanente experience. Ann Intern Med. 1999 February 16;130(4 Pt 2):355–359. doi: 10.7326/0003-4819-130-4-199902161-00005. [DOI] [PubMed] [Google Scholar]
- 22.Bellet PS, Whitaker RC. Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges. Pediatrics. 2000 March;105(3 Pt 1):478–484. doi: 10.1542/peds.105.3.478. [DOI] [PubMed] [Google Scholar]
- 23.Clinical Looking Glass. Emerging Health Information Technology. New York: Yonkers; A quality improvement health care surveillance software 2009. [Google Scholar]
- 24.New York State Department of Health. New York State Physician Profile Website. www nydoctorprofile com 2008;Available at: URL: www.nydoctorprofile.com.
- 25.Hollenbeck BK, Miller DC, Taub DA, et al. The effects of adjusting for case mix on mortality and length of stay following radical cystectomy. J Urol. 2006 October;176(4 Pt 1):1363–1368. doi: 10.1016/j.juro.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 26.Wannamethee SG, Shaper AG, Lennon L, Whincup PH. Height loss in older men: associations with total mortality and incidence of cardiovascular disease. Arch Intern Med. 2006 December 11;166(22):2546–2552. doi: 10.1001/archinte.166.22.2546. [DOI] [PubMed] [Google Scholar]
- 27.Maraldi C, Volpato S, Kritchevsky SB, et al. Impact of inflammation on the relationship among alcohol consumption, mortality, and cardiac events: the health, aging, and body composition study. Arch Intern Med. 2006 July 24;166(14):1490–1497. doi: 10.1001/archinte.166.14.1490. [DOI] [PubMed] [Google Scholar]
- 28.Goldwasser P, Feldman J. Association of serum albumin and mortality risk. J Clin Epidemiol. 1997 June;50(6):693–703. doi: 10.1016/s0895-4356(97)00015-2. [DOI] [PubMed] [Google Scholar]
- 29.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 30.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998 January;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Clinical Classifications Software (CCS) 2005 [computer program] 2007 [Google Scholar]
- 32.Newson R. Confidence intervals for rank statistics: Somers' D and extensions. The STATA Journal. 2006;6(3):309–334. [Google Scholar]
- 33.Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19(6):716–723. [Google Scholar]
- 34.STATA Version 10.0. College Station, Texas: StataCorp; 2010. [Google Scholar]
- 35.Byers AL, Allore H, Gill TM, Peduzzi PN. Application of negative binomial modeling for discrete outcomes: a case study in aging research. J Clin Epidemiol. 2003 June;56(6):559–564. doi: 10.1016/s0895-4356(03)00028-3. [DOI] [PubMed] [Google Scholar]
- 36.Aujesky D, Stone RA, Kim S, Crick EJ, Fine MJ. Length of hospital stay and postdischarge mortality in patients with pulmonary embolism: a statewide perspective. Arch Intern Med. 2008 April 14;168(7):706–712. doi: 10.1001/archinte.168.7.706. [DOI] [PubMed] [Google Scholar]
- 37.Brotman DJ, Lindenauer PK. Length of stay and mortality in pulmonary embolism: high time for evidence-based discharge criteria. Arch Intern Med. 2008 April 14;168(7):683–684. doi: 10.1001/archinte.168.7.683. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.