Abstract
Background
The demographic shift toward an older population in the U.S. will result in a higher burden of coronary heart disease, but the increase has not been quantified in detail. We sought to estimate the impact of the aging U.S. population on coronary heart disease.
Methods
We used the Coronary Heart Disease Policy Model, a Markov model of the U.S. population aged 35–84 years, and U.S. Census projections to model the age structure of the population from 2010–2040.
Results
Assuming no substantive changes in risks factors or treatments, incident coronary heart disease is projected to increase by approximately 26%, from 981,000 in 2010 to 1,234,000 in 2040, and prevalent coronary heart disease by 47%, from 11.7 million to 17.3 million. Mortality will be affected strongly by the aging population; annual coronary heart disease deaths are projected to increase by 56% over the next 30 years, from 392,000 to 610,000. Coronary heart disease-related health care costs are projected to rise by 41% from $126.2 billion in 2010 to $177.5 billion in 2040 in the U.S. It may be possible to offset the increase in disease burden through achievement of Healthy People 2010/2020 objectives or interventions that substantially reduce obesity, blood pressure, or cholesterol levels in the population.
Conclusions
Without considerable changes in risk factors or treatments, the aging of the U.S. population will result in a sizeable increase in coronary heart disease incidence, prevalence, mortality, and costs. Health care stakeholders need to plan for future age-related health care demands of coronary heart disease.
Keywords: Aging, coronary heart disease, forecasting, Markov chains
The United States (U.S.) population is aging. The combination of the elevated birth rate during the “Baby Boom” and the increasing life expectancy will result in a doubling of the population aged 65 years and older from year 2010 to 2040,1 with the number of persons aged 65 and older increasing from 40 million in 2010, to 81 million in 2040.1, 2 Coronary heart disease is strongly associated with age and is the leading cause of death in the US.3 Because coronary heart disease disproportionately affects the elderly, this demographic shift will result in a considerable increase in burden of disease in the U.S. population. The first of the Baby Boomers will enter the Medicare population in 2011, so up-to-date projections of coronary heart disease burden are of special importance for public health planning. Quantitative estimates of the magnitude and distribution of disease are essential for appropriate preparedness strategies at both the provider and system levels, and in order to optimally target preventive efforts.
We aimed to provide a detailed projection of the impact of the aging U.S. population on coronary heart disease burden, based on a computer model that is representative of the U.S. population. The Coronary Heart Disease Policy Model is a simulation model that can account for the relationship of risk factors and changing demographics on the incidence, prevalence, and cost of coronary heart disease.4 Since its inception, the Model has been used to explain the decline in coronary heart disease mortality in the U.S. 5; to estimate the gains in life expectancy achievable by various risk factor interventions 6; to assess the cost-effectiveness of interventions to reduce cholesterol 7, 8, blood pressure9, 10, and smoking 11; and to analyze the public health impact of improvements in medical care.12, 13 Most recently, the Model has assessed the impact of current adolescent obesity on future rates of adult coronary heart disease,14 public policies to reduce passive tobacco exposure on coronary heart disease rates15, clinical guidelines for the use of statins 16, and the impact of dietary salt reductions 17. In 1987, the Model’s projections were published through 2010.4 In this analysis, we provide updated estimates of the impact of the aging U.S. population on the incidence, prevalence, mortality, and cost of coronary heart disease from 2010–2040. In addition, we estimate the extent to which achievement of national goals for risk factor improvement could offset the age-related increase in coronary heart disease burden.
Methods
Model
The Coronary Heart Disease Policy Model is a validated state-transition (Markov) model of the incidence, prevalence, mortality, and cost of coronary heart disease in U.S. residents aged 35 to 84 years.4 The model is composed of three components. First, the demographic-epidemiologic submodel estimates the incidence of coronary heart disease (cardiac arrest, myocardial infarction, angina, or coronary heart disease death) and death from other causes, based on age, sex, systolic blood pressure, smoking, high-density lipoprotein (HDL) cholesterol, and low-density lipoprotein (LDL) cholesterol, diabetes, and body-mass index (BMI). Second, the bridge submodel characterizes the initial coronary heart disease event and related events in the subsequent 30 days. Third, the disease-history submodel predicts the number of subsequent coronary heart disease events, revascularization procedures, and deaths among subjects with coronary heart disease, stratified according to age, sex, and history of coronary heart disease events. Modifiable components of the model include: population distributions, risk-factor levels, risk-factor coefficients, event rates, case fatality rates, costs, and quality of life adjustments.4 A more detailed description of the Model is given in the appendix.
Data Sources
In the present study, we used U.S. Census data and 2008 projections to estimate the demographic shift in the age structure of the population.2 Other data sources for the Model include the National Center for Health Statistics mortality data,18 the Framingham Heart Study for the association of risk factors with coronary heart disease,19, 20 and Olmsted County data for the incidence of myocardial infarction and cardiac arrest.21 The prevalence of coronary heart disease was estimated from the National Health Interview Survey,22 and the risk factor distributions were estimated from the National Health and Nutrition Examination Survey.23 Data from the National Hospital Discharge Survey were used to calculate rates of myocardial infarction, hospitalization due to cardiac arrest, revascularization procedures, and associated case-fatalities.24 We estimated coronary heart disease deaths, pre-hospital deaths due to cardiac arrest, and non-coronary heart disease deaths based on data from the U.S. Vital Statistics.18 Total health care costs and 30-day survival rates were based on data from Medicare.25 We estimated coronary heart disease costs based on California data,26 deflated by using cost-to-charge ratios,27 and the ratio of the U.S. national average costs to the California average.28 We then inflated to 2010 dollars by using the Bureau of Labor Statistics Consumer Price Index for Medical Care Costs.29
Simulations
We ran the main simulation from years 2010–2040 to reflect the changing age demographics of the U.S. population over these years. Age and sex specific risk factor distributions, event rates, case fatality rates, and costs per event were held constant across the simulation period in order to isolate the effect of the aging population. We estimated the absolute and relative annual excess (defined as increase above 2010 estimates) in coronary heart disease incidence (stable or unstable angina, myocardial infarction, cardiac arrest, and death), prevalence, mortality, and costs across 30 years. We present the annual number of events by ten year age categories.
We next explored how changes in risk factors and treatments might alter the projected increase in coronary heart disease incidence. We modeled the impact of achieving adherence to the major 2010/2020 Healthy People guidelines for risk factors in 2010, including a 10% reduction in the prevalence of hypertension, a 40% improvement in the control of hypertension, a 10% reduction in the prevalence of hypercholesterolemia, a 10% reduction in the mean level of cholesterol, a 10% reduction in the prevalence of obesity, a reduction of the prevalence of smoking to 12%, a 10% reduction in environmental exposure to smoke, and a 10% reduction in the rate of developing incident diabetes 30. For the cholesterol interventions, we modified LDL-cholesterol levels instead of total cholesterol in the Model. We explored the impact of lowering LDL-cholesterol and blood pressure to levels used in prevention guidelines.31 We also modeled the impact a linear 10% increase in BMI over 30 years, which is consistent with recently published trends32, as well as a 10% decrease in BMI over the simulation period. Finally, we modeled the impact of a hypothetical intervention that would reduce the in-hospital MI case-fatality rate by 25–50%, based on improvements in the survival of patients hospitalized for MI in the past 30 years.33, 34
Results
In 2010, an estimated 156 million adults age 35–84 years will be living in the US. This population is expected to increase by 28% to 200 million in 2040. The 65–84 year old population is expected to increase by 89% percent over this period, due to both the aging of Baby Boomers as well as their longer life expectancy. The increase in coronary heart disease will reflect this population growth: incidence, prevalence, mortality, and cost are all expected to increase monotonically over the next 30 years.
The number of incident coronary heart disease cases is projected to increase in parallel with the overall population growth by approximately 26% from 981,000 in 2010 to 1,234,000 in 2040 (Table 1). The number of incident cases is projected to remain fairly constant in persons under age 65 years because of the relatively smaller population growth in this subgroup. The largest increase in incident coronary heart disease events will be expected in persons 65 years and older, and the number of cases in 75–84 year olds will double in the next 30 years. Without a change in the risk factor distributions, the incidence rate is projected to remain fairly constant, at 680 per 100,000 person years in 2010 as compared with 710 per 100,000 person years in 2040.
Table 1.
Projected coronary heart disease Incidence, Prevalence, Mortality, and Cost in U.S. Adults Aged 35–84 years
| Year | Population | 2010 | 2020 | 2030 | 2040 |
|---|---|---|---|---|---|
| Incidence | Total | 981,000 | 1,128,000 | 1,212,000 | 1,234,000 |
| 35–64 years | 658,000 | 666,000 | 637,000 | 669,000 | |
| 65–84 years | 323,000 | 462,000 | 575,000 | 565,000 | |
| Prevalence | Total | 11,744,000 | 14,382,000 | 16,699,000 | 17,322,000 |
| 35–64 years | 5,662,000 | 6,949,000 | 7,107,000 | 7,634,000 | |
| 65–84 years | 6,082,000 | 7,433,000 | 9,592,000 | 9,688,000 | |
| Mortality | Total | 392,000 | 473,000 | 586,000 | 610,000 |
| 35–64 years | 106,000 | 122,000 | 118,000 | 125,000 | |
| 65–84 years | 286,000 | 351,000 | 468,000 | 485,000 | |
| Cost ($ Billions) | Total | 126.2 | 149.5 | 170.7 | 177.5 |
| 35–64 years | 69.7 | 79.5 | 80.5 | 86.4 | |
| 65–84 years | 56.5 | 70.0 | 90.2 | 91.1 |
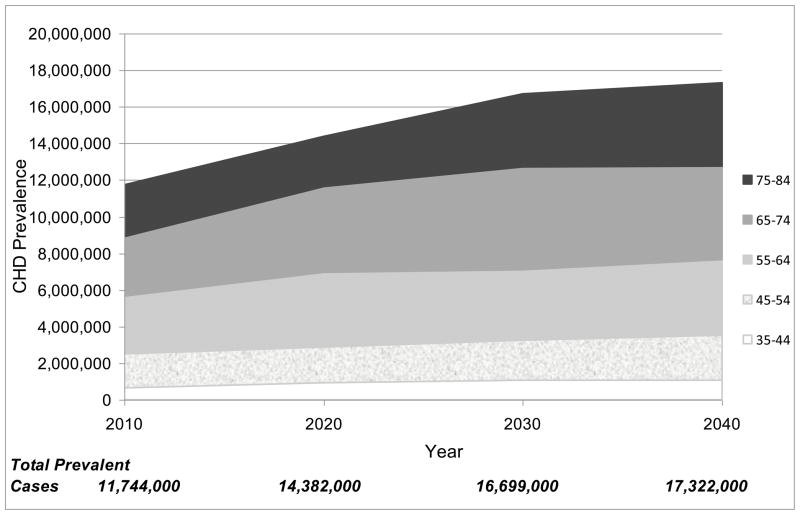
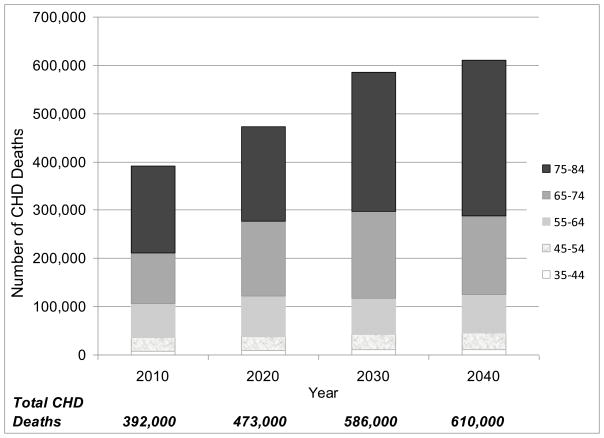
The number of prevalent coronary heart disease cases is also expected to increase as a result of the change in population demographics: the number of persons with prevalent coronary heart disease is expected to grow by 47% from 11.7 million to 17.3 million in 2040 (Table 1). As with incidence, the greatest growth in prevalence is expected to be in adults over 65 years of age (Figure 1). Coronary heart disease mortality will be impacted most strongly by the shift in age demographics, and coronary heart disease deaths are expected to increase by over 50% over the next 30 years (Figure 2). The number of deaths in adults age 65–84 years is projected to increase by two-thirds, due to the large increase in this segment of the population. The greater increase in coronary heart disease deaths compared with incidence or prevalence is because death disproportionately occurs at older ages; the increase in the number of older adults will affect mortality rates more strongly than it will affect incidence or prevalence rates.
Figure 1.
The absolute coronary heart disease prevalence by decade of age, from 2010 – 2040
Figure 2.
The absolute number of coronary heart disease deaths by decade of age, from 2010 – 2040.
U.S. coronary heart disease related health care costs in adults aged 35–84 are projected to rise by 41% over the next 30 years, from $126.2 billion in 2010 to $177.5 billion in 2040, based on year 2010 dollars. The annual cost of coronary heart disease per working-aged adult (20–64 years) is projected to rise by 24%, from $680 in 2010 to $840 in 2040. The proportion of costs associated with acute coronary heart disease care is projected to increase slightly over the next 30 years compared with costs due to chronic disease follow-up, from 48% in 2010 to 50% in 2040.
Effects of Potential Changes in Risk Factors or Treatment
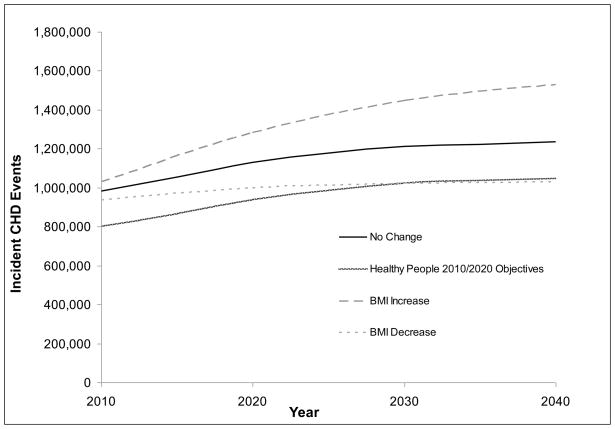
Immediate achievement of Healthy People 2010/2020 objectives for blood pressure, lipids, obesity, smoking, and diabetes could offset the increase in disease attributable to the aging population by over 70% in 2040 (Figure 3). In addition, a trend of a reduction in BMI by 10% over the next 30 years could offset the projected increase in incidence by approximately 80%. In contrast, a trend of increase in the average BMI of U.S. adults by 10% over the next 30 years would add to the burden of coronary heart disease, and could more than double the increase in incident cases by 2040 (Figure 3). If all Americans age 35–84 had a systolic blood pressure no higher than 140 mmHg, the projected incidence of coronary heart disease would be 1,130,000 new cases in 2040, or a 15% increase over 2010. Similarly, if all Americans had an LDL-cholesterol of <130 mg/DL, the projected incidence would be 1,151,000 in 2040, or a 17% increase over 2010. A 25–50% reduction in the in-hospital case-fatality for both first and recurrent MI in 2040 as compared with 2010 was projected to reduce mortality in 2040 by only 4–8%.
Figure 3.
The projected impact of changes in coronary heart disease risk factors on coronary heart disease incidence, from 2010–2040. Adherence to Healthy People 2010/2020 objectives include immediate improvements in blood pressure, LDL-cholesterol, obesity, smoking, and diabetes. BMI increase and decrease refers to a +/− 10% trend from 2010–2040.
Discussion
Unprecedented growth in the 65 years and older population in the U.S. is expected over the coming decades. This growth will result in a substantial increase in coronary heart disease incidence, prevalence, mortality, and cost. A quantitative estimate of the magnitude of this increase is essential information for stakeholders in the U.S. health care system, including patients, providers, training organizations, hospitals, health plans, governments, and industry.35, 36 Despite concern over the impact of the aging Baby Boomers on health care, few detailed quantitative estimates of the effect of the aging population on coronary heart disease burden have been published. Our study provides estimates that will inform researchers, providers, and policy makers as they plan to meet future age-related health care demands.
Our findings expand upon prior research that has demonstrated strong growth in coronary heart disease prevalence and mortality over the next several decades;37 Foot et al. estimated a 128.5% increase in coronary heart disease mortality and a 93% increase in coronary heart disease prevalence from 2000–2050. Our projections are slightly more conservative, and we provide detailed epidemiologic estimates that account for the distribution of age, gender, and risk factors in the U.S. population. As noted by prior studies, the aging population will impact the need for more focused efforts on primary, secondary, and tertiary prevention, as optimal treatment can lead to longer and higher quality of life in coronary heart disease patients. However, these preventive efforts will also increase the need for providers and services. The increased burden of disease will require more resources in hospitals, physicians, medical groups, training institutions, and public health departments.37 Physicians and non-physician clinicians are already in short supply. For example, the Council on Graduate Medical Education (COGME) has determined that the demand for physicians is expected to grow more than the supply over the next 10 years.35, 38 Although some of this burden will require more specialty providers to conduct procedure-based treatments, the majority of the burden is likely to fall on primary care physicians and geriatricians who manage the chronic care of patients living with coronary heart disease.
Risk factors and medical advances to prevent and treat coronary heart disease will certainly change in the next 30 years, and these changes are difficult to predict. Primary prevention gains would need to be substantial to offset the impact of the aging population. The achievement of optimistic, but feasible, improvements in risk factor control, consistent with Healthy People 2010/2020 objectives, could offset over 70% of the increase in coronary heart disease incidence due to the aging of the population. However, achievement of these goals would require these improvements across multiple domains, including a reversal of the trend of weight gain and increasing diabetes in the U.S. If the trend of increasing BMI continues at the same rate observed over the past few decades, the growing burden of coronary heart disease would be even worse. A prior study based on the Model demonstrated a substantial impact of current adolescent obesity on the future burden of coronary heart disease; Bibbins-Domingo et al. estimated an excess of at least 100,000 cases of coronary heart disease in 2035. 14 Conversely, improvements in BMI could offset the increase in coronary heart disease; a 10% reduction in BMI over the next 30 years would offset approximately 80% of the impact of the aging population, because of its beneficial effects on blood pressure, cholesterol, and diabetes. These simulations suggest that public health interventions to lower BMI through improved diet and physical activity should be a high priority. By comparison, a 25–50% reduction in in-hospital MI case fatality would have only a modest effect on coronary heart disease largely because the current survival rate is approximately 90% for a hospitalized first MI24. Taken together, these analyses suggest that substantial improvements from risk factor profiles would be necessary to offset the projected increase in coronary heart disease.
This increased burden of disease will likely tax the already struggling U.S. health care system. Medical expenditures have increased at a high rate for many years, and the future impact of population aging on health care costs is frequently cited as a source of concern in the literature and media.36, 39, 40 Our cost projections due to coronary heart disease events are similar to those reported by Martini et al.,36 who estimated a 44% increase in health care costs due to heart and vascular conditions from 2000–2050. Notably, heart and vascular conditions account for more medical care costs than any other category of disease.36 Population growth amongst working adults could help to offset these costs slightly, through increased tax revenue and other financial contributions. Although, the coronary heart disease costs per working adult aged 20–64 are projected to increase by 24% over the next 30 years. Economic growth will only augment the increase in health care costs; prior studies have demonstrated that economic expansion determines the ceiling for health care expenditures, and demand for services will continue to grow as patients desire and expect longer and healthier lives.35
The Model is tested and updated regularly to reflect changes in risk factor distributions, population estimates, risk factor associations, event rates, case-fatality rates, and costs, although these statistics are only estimates of what may occur in the future. Projections from any forecasting model should be viewed with caution, as there will always be unpredicted changes that can impact results. The prior projections from the Coronary Heart Disease Policy Model published in 1987 underestimated the prevalence of future coronary heart disease but overestimated incidence and mortality4, although the majority of the variation can be explained by a change in disease definition and by reductions in risk factors and advances in treatment (See appendix).
Our projections have limitations that should be considered when interpreting the findings. These estimates do not account for changes in the racial/ethnic structure of the population; though this could impact our estimates, the relationship between age and risk of coronary heart disease events does not likely differ greatly across racial/ethnic groups.. The timing and sustainability of the risk factor changes that were modeled were optimistic and could vary substantially in practice. Furthermore, there will likely be unexpected changes in risk factor profiles and health care technology that could affect our results. Improved therapies to treat coronary heart disease may decrease secondary events and mortality, but also increase the cost and prevalence of coronary heart disease. Finally, the model does not include incident events for adults over 85 years of age, who represent a growing proportion of the population of adults with coronary heart disease.
In conclusion, the demographic shift towards an increased number of older adults in the U.S. will have a substantial impact on coronary heart disease burden over the next 30 years. Stakeholders in the U.S. health care system should prepare for this growth by ensuring there are adequate resources to care for the high number of adults expected to be living with coronary heart disease as optimal treatment can lead to longer and higher quality of life in coronary heart disease patients. Future improvements in primary and secondary prevention may attenuate this burden of disease, although substantial changes would be necessary to offset the effect of the aging population.
Supplementary Material
Acknowledgments
This work was supported in part by the Swanson Family Fund, Tempe, AZ, and a grant-in-aid from the American Heart Association Western States Affiliate, Burlingame, CA (09GRNT2060096). Dr. Odden is supported by a Ruth L. Kirschstein National Research Service Award (T32HP19025). Dr. Moran is supported by an NIH/NHLBI Mentored Career Development Award (K08HL089675), and an Empire Clinical Research Program award from New York State, NY, NY.
Footnotes
All authors were involved in the design of the study, interpretation of data, and the writing of the manuscript. All authors have approved the final version. None of the authors have any conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. Trends in Aging - United States and Worldwide. MMWR. 2003;52:101–106. [PubMed] [Google Scholar]
- 2.U.S. Census Bureau. US Interim Projections by Age, Sex, Race, and Hispanic Origin 2008. Vol. 2009. 2008. [Google Scholar]
- 3.Heron M, Hoyert DL, Murphy SL, et al. Deaths: Final Data for 2006. National Vital Statistics Reports 2009. 57(14) [PubMed] [Google Scholar]
- 4.Weinstein MC, Coxson PG, Williams LW, et al. Forecasting coronary heart disease incidence, mortality, and cost: the Coronary Heart Disease Policy Model. Am J Public Health. 1987;77(11):1417–26. doi: 10.2105/ajph.77.11.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldman L. Cost-effectiveness perspectives in coronary heart disease. Am Heart J. 1990;119(3 Pt 2):733–9. doi: 10.1016/s0002-8703(05)80054-7. discussion 739–40. [DOI] [PubMed] [Google Scholar]
- 6.Tsevat J, Weinstein MC, Williams LW, et al. Expected gains in life expectancy from various coronary heart disease risk factor modifications. Circulation. 1991;83(4):1194–201. doi: 10.1161/01.cir.83.4.1194. [DOI] [PubMed] [Google Scholar]
- 7.Goldman L, Weinstein MC, Williams LW. Relative impact of targeted versus populationwide cholesterol interventions on the incidence of coronary heart disease. Projections of the Coronary Heart Disease Policy Model. Circulation. 1989;80(2):254–60. doi: 10.1161/01.cir.80.2.254. [DOI] [PubMed] [Google Scholar]
- 8.Prosser LA, Stinnett AA, Goldman PA, et al. Cost-effectiveness of cholesterol-lowering therapies according to selected patient characteristics. Ann Intern Med. 2000;132(10):769–79. doi: 10.7326/0003-4819-132-10-200005160-00002. [DOI] [PubMed] [Google Scholar]
- 9.Edelson JT, Weinstein MC, Tosteson AN, et al. Long-term cost-effectiveness of various initial monotherapies for mild to moderate hypertension. JAMA. 1990;263(3):407–13. [PubMed] [Google Scholar]
- 10.Phillips KA, Shlipak MG, Coxson P, et al. Health and economic benefits of increased beta-blocker use following myocardial infarction. JAMA. 2000;284(21):2748–54. doi: 10.1001/jama.284.21.2748. [DOI] [PubMed] [Google Scholar]
- 11.Tosteson AN, Weinstein MC, Williams LW, Goldman L. Long-term impact of smoking cessation on the incidence of coronary heart disease. Am J Public Health. 1990;80(12):1481–6. doi: 10.2105/ajph.80.12.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldman L, Phillips KA, Coxson P, et al. The effect of risk factor reductions between 1981 and 1990 on coronary heart disease incidence, prevalence, mortality and cost. J Am Coll Cardiol. 2001;38(4):1012–7. doi: 10.1016/s0735-1097(01)01512-1. [DOI] [PubMed] [Google Scholar]
- 13.Tice JA, Ross E, Coxson PG, et al. Cost-effectiveness of vitamin therapy to lower plasma homocysteine levels for the prevention of coronary heart disease: effect of grain fortification and beyond. JAMA. 2001;286(8):936–43. doi: 10.1001/jama.286.8.936. [DOI] [PubMed] [Google Scholar]
- 14.Bibbins-Domingo K, Coxson P, Pletcher MJ, et al. Adolescent overweight and future adult coronary heart disease. N Engl J Med. 2007;357(23):2371–9. doi: 10.1056/NEJMsa073166. [DOI] [PubMed] [Google Scholar]
- 15.Lightwood JM, Coxson PG, Bibbins-Domingo K, et al. Coronary heart disease attributable to passive smoking: CHD Policy Model. Am J Prev Med. 2009;36(1):13–20. doi: 10.1016/j.amepre.2008.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pletcher MJ, Lazar L, Bibbins-Domingo K, et al. Comparing impact and cost-effectiveness of primary prevention strategies for lipid-lowering. Ann Intern Med. 2009;150(4):243–54. doi: 10.7326/0003-4819-150-4-200902170-00005. [DOI] [PubMed] [Google Scholar]
- 17.Bibbins-Domingo K, Chertow GM, Coxson PG, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010;362(7):590–9. doi: 10.1056/NEJMoa0907355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.United States, 1999–2000. Atlanta: National Center for Health Statistics; 2007. Deaths for 358 Selected causes, by 5year age groups, race and sex. [Google Scholar]
- 19.Framingham Heart Study CD-ROM. Washington DC: Department of Health and Human Services; 2005. [Google Scholar]
- 20.Wilson PW, D’Agostino RB, Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–47. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 21.Roger VL, Jacobsen SJ, Weston SA, et al. Trends in the incidence and survival of patients with hospitalized myocardial infarction, Olmsted County, Minnesota, 1979 to 1994. Ann Intern Med. 2002;136(5):341–8. doi: 10.7326/0003-4819-136-5-200203050-00005. [DOI] [PubMed] [Google Scholar]
- 22.National Health Interview Survey datasets. Washtington, DC: National Center for Health Statistics; 2000. [Google Scholar]
- 23.National Health and Nutrition Examination Survey. Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 24.National Hospital Discharge Survey, 1996–2005. National Center for Health Statistics; [Google Scholar]
- 25.Centers for Medicare & Medicaid Services. Personal Health Care Spending by Type of Spending, Age Group, and Source of Payment Distribution, Calendar Year 1999. Centers for Medicare & Medicaid Services; 2000. [Google Scholar]
- 26.California Patient Discharge Data January 1 - December 31, 2000, Public Version A-24 (CD-ROM) Sacramento, California: Office of Statewide Health Planning and Development; 2001. [Google Scholar]
- 27.Office of Statewide Health Planning and Development. Hospital financial data for cost to charge ratio, CA inpatient discharge data hospital annual finanacial data, pivot profiles, 1999–2000. Sacramento, California: California Office of Statewide Health Planning and Development; 2008. [Google Scholar]
- 28.U.S. Census Bureau. Statistical Abstract of the United States. Average cost to community hospitals per patient, by state (Table 204) Washington, DC: Goverment Printing Office; 1998. [Google Scholar]
- 29.Bureau of Labor Statistics. Consumer Price Index. Washington, DC: Bureau of Labor Statistics; 2010. [Google Scholar]
- 30.Department of Health and Human Services. Healthy People 2020. Washington, D.C.: 2010. [Google Scholar]
- 31.Pearson TA, Blair SN, Daniels SR, et al. AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update: Consensus Panel Guide to Comprehensive Risk Reduction for Adult Patients Without Coronary or Other Atherosclerotic Vascular Diseases. American Heart Association Science Advisory and Coordinating Committee. Circulation. 2002;106(3):388–91. doi: 10.1161/01.cir.0000020190.45892.75. [DOI] [PubMed] [Google Scholar]
- 32.Ogden CL, Fryar CD, Carroll MD, Flegal KM Statistics NCfH. Advance data from vita and health statistics: no 347. 2004. Mean body weight, height, and body mass index, United States 1960–2002. [PubMed] [Google Scholar]
- 33.Floyd KC, Yarzebski J, Spencer FA, et al. A 30-year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2(2):88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McGovern PG, Jacobs DR, Jr, Shahar E, et al. Trends in acute coronary heart disease mortality, morbidity, and medical care from 1985 through 1997: the Minnesota heart survey. Circulation. 2001;104(1):19–24. doi: 10.1161/01.cir.104.1.19. [DOI] [PubMed] [Google Scholar]
- 35.Cooper RA. Weighing the evidence for expanding physician supply. Ann Intern Med. 2004;141(9):705–14. doi: 10.7326/0003-4819-141-9-200411020-00012. [DOI] [PubMed] [Google Scholar]
- 36.Martini EM, Garrett N, Lindquist T, Isham GJ. The boomers are coming: a total cost of care model of the impact of population aging on health care costs in the United States by Major Practice Category. Health Serv Res. 2007;42(1 Pt 1):201–18. doi: 10.1111/j.1475-6773.2006.00607.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Foot DK, Lewis RP, Pearson TA, Beller GA. Demographics and cardiology, 1950–2050. J Am Coll Cardiol. 2000;35(4):1067–81. doi: 10.1016/s0735-1097(00)00561-1. [DOI] [PubMed] [Google Scholar]
- 38.Council on Graduate Medical Education; Services USDoHaH. Reassessing Physician Workforce Policy Guidelines for the US 2000–2020. Washington, DC: 2003. [Google Scholar]
- 39.Halvorson GC. Credibility and creativity: a conversation with Kaiser Permanente’s George C. Halvorson . Health Aff (Millwood) 2004;23(4):133–42. doi: 10.1377/hlthaff.23.4.133. [DOI] [PubMed] [Google Scholar]
- 40.Rice DP, Fineman N. Economic implications of increased longevity in the United States. Annu Rev Public Health. 2004;25:457–73. doi: 10.1146/annurev.publhealth.25.101802.123054. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.