Abstract
Ankylosing spondylitis (AS) is frequently associated with inflammatory lesions of the spine and continuous fatigue stress fractures; however, an association with an intraspinal synovial cyst has not been previously reported. A 55-year-old man with a five year history of AS who presented with back pain and a right radiculopathy was admitted to the hospital. Five years previously, he underwent a percutaneous vertebroplasty for an osteoporotic L1 compression fracture, and was diagnosed with AS at that time. Plain radiographs showed aggravated kyphosis and a stress fracture through the ossified posterior element, below the prior vertebroplasty. Magnetic resonance images revealed a right foraminal cystic lesion at the L2-L3 level with effacement of the nerve root. A 1.6 cm cystic lesion that appeared to arise from the L2-L3 facet joint without direct communication was excised from the L2-L3 foramen. Pathological examination confirmed synovial cyst. The patient's symptoms resolved immediately after surgery except for a mild dysesthesia of the right leg. We report herein a rare case of foraminal synovial cyst associated with AS accompanying posterior element fracture with a review of literature.
Keywords: Synovial cyst, Ankylosing spondylitis
INTRODUCTION
Synovial cysts usually develop from the synovial capsule of the facet joints. Although their etiology is unclear, facet joint arthropathy and underlying spinal instability are known to be associated with the formation of synovial cysts and worsening symptoms1,7). Most intraspinal synovial cysts are located in the lower lumbar spine, where the greatest degree of movement is present4). In rare cases, they have also been described with inflammatory changes of the facet joints in association with rheumatoid arthritis and undifferentiated spondyloarthropathy2,3,6). However, there has been no report of intraspinal synovial cysts associated with ankylosing spondylitis (AS). We report a patient who developed a radiculopathy caused by foraminal synovial cyst associated with AS accompanying posterior element fracture.
CASE REPORT
A 55-year-old man with a five year history of AS was admitted to our institute with severe back pain and right thigh pain. Five years previously, he developed severe back pain after a light fall and the magnetic resonance imaging (MRI) revealed a fresh compression fracture at L1. The patient was diagnosed with AS at that time and underwent percutaneous vertebroplasty (Fig. 1). The lowest T-score on DEXA bone mineral density was -3.57 at that time. The patient presented with only mild back discomfort after the vertebroplasty. However, the back and thigh pain progressively worsened without any history of trauma for one month before re-admission. Ambulation was very limited and the patient was then admitted to the hospital again. On physical examination, there was no motor weakness but there was decreased sensation to pinprick in the right L2 dermatome. The results of the straight leg raising test and femoral stretch test were negative. Simple radiographs showed severe degenerative changes, spondylosis, aggravated kyphosis and a stress fracture through the ossified posterior segment, below the prior vertebroplasty (Fig. 2A). Computed tomography scanning confirmed the stress fracture (Fig. 2B). The MRI revealed a right foraminal cystic mass at the L2-L3 level with effacement of the nerve root (Fig. 3). The cyst's interior signal was isointense with the cerebrospinal fluid on T1-weighted images and hyperintense on T2-weighted sequences. Administration of gadolinium resulted in little enhancement of the cyst's wall. A right L2-L3 total facetectomy and posterolateral fusion were performed to remove the lesion (Fig. 4). During surgery, a 1.6 cm cystic lesion was identified in the neural foramen and dorsal to right L2 nerve root. The cyst was filled with a dark yellowish fluid and it was totally resected. On pathological examination, a fibroconnective tissue and synovial membrane was observed (Fig. 5). The patient's postoperative course was uneventful. The symptoms resolved immediately after surgery except for a mild dysthesia and be remained free of thigh pain 15 months after surgery.
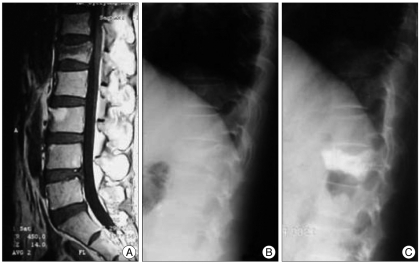
Fig. 1.
A 55-year-old man with an osteoporotic compression fracture. A and B : T1-weighted magnetic resonance image and simple lateral radiograph show a fresh compression fracture at the L1 level. C : Simple lateral radiograph shows good filling of bone cement after percutaneous vertebroplasty.
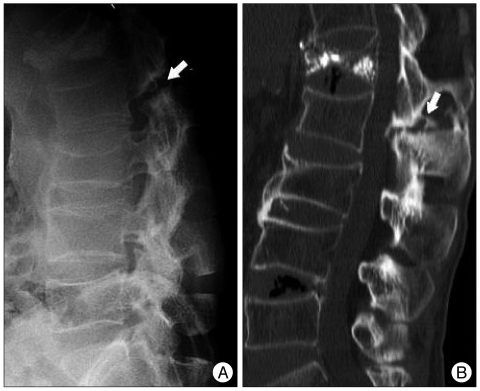
Fig. 2.
Five years later, a simple radiograph and computed tomographic scan show the transverse fracture. A : Simple radiograph shows the posterior element fracture through the facet joints below the prior vertebroplasty (arrow). B : Computed tomographic scan confirmed posterior element fracture (arrow).
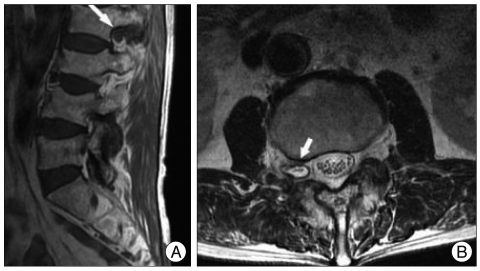
Fig. 3.
T1 weighted sagittal image and T2 weighted axial magnetic resonance images of the patient. A : T1 weighted sagittal image reveals hypointense lesion within L2 neural foramen (arrow). B : T2 weighted axial image shows hyperintense lesion at the right L2 neural foramen (arrow).
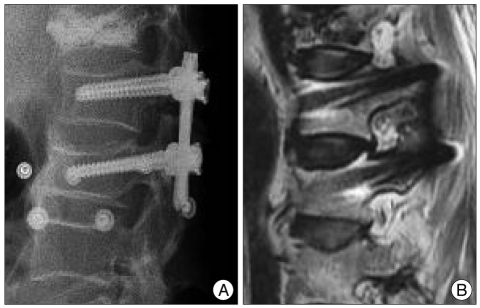
Fig. 4.
A and B : Posterolateral fusion was performed to remove the lesion and T1-weighted magnetic resonance image taken 2 months after operation shows complete removal of cystic lesion.
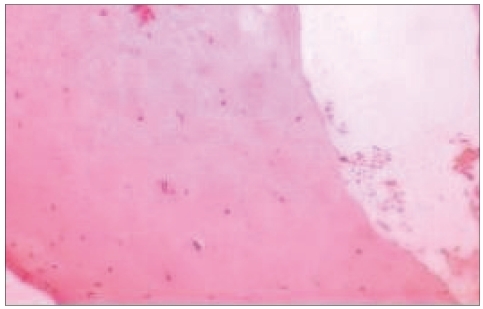
Fig. 5.
Microscopic findings of a surgical specimen show fibroconnective tissue and synovial membrane consistent with a synovial cyst. (H&E ×100)
DISCUSSION
Several theories have been suggested on the origin of synovial cysts. Most are contiguous with the facet joint capsule itself. Other theories suggest displaced cell rests of synovium, degeneration of the collagenous tissue of the joint capsule, or neoformation from articular tissue resulting from chronic irritation and inflammation1,7). Symptomatic synovial cysts of the facet joints in the lumbar spine have been the focus of study recently5,11). The most common cause reported is degenerative facet joint disease with hypertrophy and herniation of synovium through a tear of the capsule. Rarely, cysts have been observed to develop secondary to rheumatoid arthritis2,6,8,9). However, there have been no cases reported in association with AS; although Vergne et al.10) considered the possibility of this association. As the synovial fluid not only exists in the spinal canal, but also appears in ligament or tendons, there is possibility for it to be occured without attaching with facet joint. We, however, could not find any case which developed foraminal location at L2-L3 level. In this case, as the actual section of the facet joint was undefinable due to ankylosis of AS, we could not conclude whether the connection with facet joint exists or not, but considering the levels and location, in the case of synovial cyst that was not detected in the initial MRI taken 5 years ago, the possibility of formation of intraspinal synovial caused by chronic irritation by posterior segment fracture as the natural course of AS is worth taking into consideration. Although a casual relationship cannot be definitely established, spondylolisthesis was absent and there was no history of trauma. The occurrence of this finding in a patient with AS might be explained predominantly by an enthesitis rather than arthritis, which might make it less likely to cause a synovitis initially. A synovial cyst that develops from arthritis in a facet joint later in the course of the disease might not protrude through the ossified periarticular ligaments. Osteoporosis is a well-known complication of AS, and bone loss is the result of changes in the material and structural properties of bone; these changes lead to an increased risk of stress fractures. During the early course of AS, a simple osteoporotic compression fracture occurred after a minor injury in the patient reported here. Over time, with the chronic spinal inflammation the vertebrae likely fused together at the posterior segment fracture through the facet joints and appeared as chronic findings identified as sclerosis at the fracture margins along with pseudoarthrosis. This case showed sagittal imbalance as a consequence of the old compression fracture in the first lumbar vertebral body. Kyphosis secondary to a compression fracture indicates greater axial distraction stress or force loaded onto the posterior segment and the facet joint adjacent to the fracture level compared to normal spinal alignment. Finally, it is possible that the long-standing effects of repetitive stress caused by sagittal imbalance and the natural course of the increased vertebral stiffness were concentrated at the adjacent posterior element, through the facet joints and might have been contributing factors causing the stress fracture of the posterior element and the synovial cyst.
CONCLUSION
The findings of this case suggest that intraspinal synovial cysts may be associated with AS. It is important to aware of the natural course of AS and the possibility that continuous axial distraction stress can cause a posterior segment fracture and adjacent intraspinal synovial cyst.
References
- 1.Eyster EF, Scott WR. Lumbar synovial cysts : report of eleven cases. Neurosurgery. 1989;24:112–115. doi: 10.1227/00006123-198901000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Farrokh D. Lumbar intraspinal synovial cysts of different etiologies : diagnosis by CT and MR imaging. J Belge Radiol. 1998;81:275–278. [PubMed] [Google Scholar]
- 3.Finckh A, Gerster J, So AK. Association of spondylarthropathies with lumbar synovial cysts. Clin Rheumatol. 2003;22:67–69. doi: 10.1007/s10067-002-0656-3. [DOI] [PubMed] [Google Scholar]
- 4.Gadgil AA, Eisenstein SM, Darby A, Cassar Pullicino V. Bilateral symptomatic synovial cysts of the lumbar spine caused by calcium pyrophosphate deposition disease : a case report. Spine (Phila Pa 1976) 2002;27:E428–E431. doi: 10.1097/00007632-200210010-00024. [DOI] [PubMed] [Google Scholar]
- 5.Howington JU, Connolly ES, Voorhies RM. Intraspinal synovial cysts : 10-year experience at the Oschner Clinic. J Neurosurg. 1999;91:193–199. doi: 10.3171/spi.1999.91.2.0193. [DOI] [PubMed] [Google Scholar]
- 6.Jacob JR, Weisman MH, Mink JH, Metzger AL, Feldman GR, Dorfman HD, et al. Reversible cause of back pain and sciatica in rheumatoid arthritis : an apophyseal joint cyst. Arthritis Rheum. 1986;29:431–435. doi: 10.1002/art.1780290320. [DOI] [PubMed] [Google Scholar]
- 7.Kim SW, Lee SM. Cauda equina syndrome caused by bilateral facet cyst accompanying spinal stenosis. J Korean Neurosurg Soc. 2005;37:76–78. [Google Scholar]
- 8.Onofrio BM, Mih AD. Synovial cysts of the spine. Neurosurgery. 1988;22:642–647. doi: 10.1227/00006123-198804000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Pendleton B, Carl B, Pollay M. Spinal extradural benign synovial or ganglion cyst : case report and review of the literature. Neurosurgery. 1983;13:322–326. doi: 10.1227/00006123-198309000-00021. [DOI] [PubMed] [Google Scholar]
- 10.Vergne P, Bonnet C, Zabraniecki L, Bertin P, Moreau JJ, Treves R. Synovial cyst at the C1-C2 junction and spondylarthropathy. J Rheumatol. 1996;23:1438–1440. [PubMed] [Google Scholar]
- 11.Wait SD, Jones FD, Lonser RR, Lee KS. Symptomatic epidural hematoma caused by lumbar synovial cyst rupture : report of two cases and review of the literature. Neurosurgery. 2005;56:E1157. discussion E1157. [PubMed] [Google Scholar]