Abstract
Sebaceous gland carcinoma usually arises from the meibomian or Zeis glands within the eyelid, but tumor arising primarily from the conjunctiva, especially bulbar conjunctiva, is a rarity. We hereby report a case of a 50-year-old female who presented with a painless mass in the inferior limbus, encroaching the cornea and hanging over the lower eyelid without involving it. Imprint cytology was suggestive of adenosquamous carcinoma. Management consisted of wide local excision, cryotherapy to tumor bed, and topical 5-fluorouracil (5-FU) 1% preoperatively and postoperatively. Histopathologic analysis was in favor of sebaceous gland carcinoma. This case suggests that although sebaceous gland carcinoma commonly originates as a lid tumor, it can present as a bulbar conjunctival mass. Topical 5-FU is a viable and efficient cost-effective alternative for neo-adjuvant and adjuvant treatment of sebaceous gland carcinoma.
Keywords: 5-Fluorouracil, bulbar conjunctiva, sebaceous carcinoma
Introduction
Sebaceous carcinoma is a very rare malignant tumor with an incidence of 3.2% among malignant tumors and 0.8% of all eyelid tumors. It originates primarily from the tarsal meibomian glands of the eyelids. In extremely rare cases, it may originate in glands of Zeis of the eyelashes or the sebaceous glands of the caruncle.[1] It usually extends locally to involve conjunctiva in most cases. Sebaceous carcinomas are reported to behave aggressively with a tendency to metastasize early and are associated with a significant mortality in most series.[2] Sebaceous carcinoma confined to the conjunctiva without involvement of eyelid is very rare. Extensive search of literature showed that only few such cases have been reported worldwide.[3–5]
We report a patient with sebaceous gland carcinoma limited to the bulbar conjunctiva without lid involvement. Diagnosis of sebaceous carcinoma is usually delayed because of its ability to masquerade as a variety of other conditions such as chalazion or chronic blepharoconjunctivitis, especially when it presents at an unusual site such as bulbar conjunctiva. A high index of suspicion is vital for early diagnosis and adequate treatment.
Case Report
A 50-year-old female presented with a painless, slow-growing mass in her left eye (OS) for the past 1 year. No previous ocular history was available. There was no history of trauma, medical treatment, or surgical intervention. The best corrected visual acuity in the right eye (OD) was 20/20 and in the left eye (OS) was 20/40. Intraocular pressure was normal in both eyes (OU). On examination, conjunctival hyperemia, chemosis, and discharge was noted OS. A mass measuring 20 mm × 16 mm was seen arising from inferior limbal area and extending over the bulbar conjunctiva to lower 1 mm of cornea [Figure 1]. The lower eyelid did not seem to be involved. Anterior segments were otherwise normal, and fundus examination was unremarkable OU. No lymphadenopathy was noted. Hemogram, liver and renal function tests, chest X-ray and ultrasonography of the abdomen were normal. Computed tomography (CT) of head and orbit did not show any invasion of adjacent soft tissue and bony structures.
Figure 1.

Gross appearance of tumor mass at inferior limbus of left eye, encroaching the cornea and hanging over lower eyelid without involving it
Imprint cytology of the mass showed malignant cells and glandular pattern suggestive of adenosquamous carcinoma [Figure 2]. Wide local excision was done followed by cryotherapy of the tumor bed with double freeze-thaw technique. Topical 5-fluorouracil (5-FU) 1% was used four times a day for 1 week preoperatively for chemoreduction and postoperatively for 1 month to treat any residual tumor and prevent recurrences. Histopathologic examination (HPE) of the excised mass showed cells with sebaceous differentiation with adenomatous component, indicated by the presence of foamy cytoplasm, and was suggestive of bowenoid type sebaceous carcinoma [Figure 3].
Figure 2.
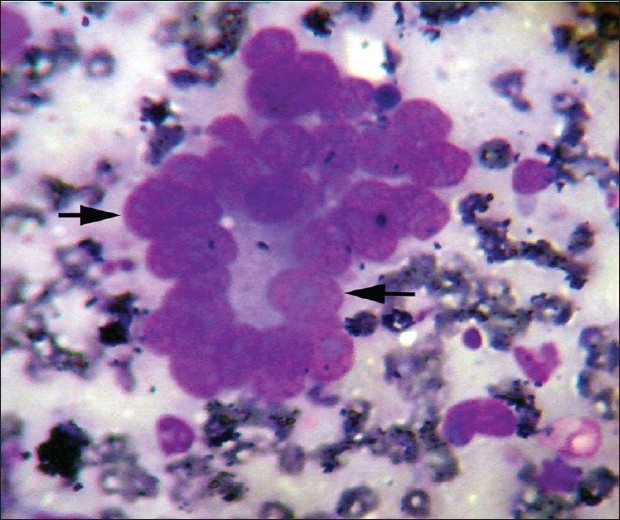
Imprint cytology showing clusters of atypical cells (arrows) with glandular pattern [May-Grünwald (MGG) stain; high magnification]
Figure 3.
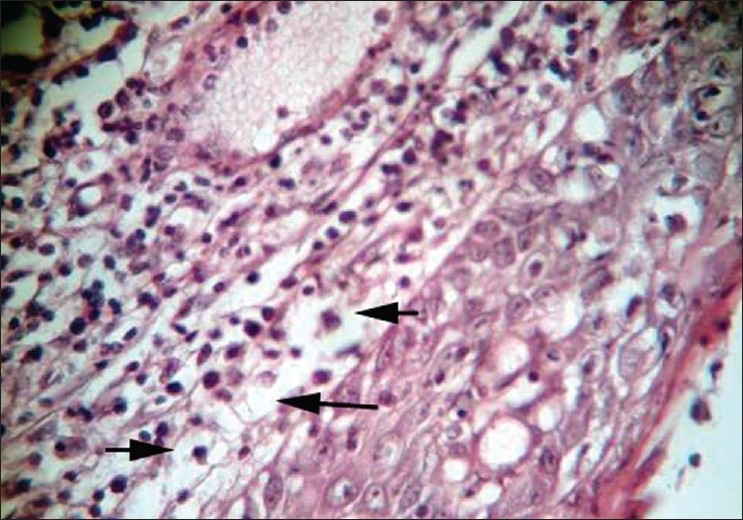
Photomicrograph of excised tissue showing atypical cells with vacuolated foamy cytoplasm suggestive of sebaceous differentiation (H and E stain; high magnification)
No recurrence was seen at 1-month follow-up. Conjunctival surface was healthy with no scar and adequate tear function. Macular grade opacity was seen in the lower peripheral part of cornea extending from 5-o’ clock to 7-o’ clock position [Figure 4]. The ocular movements were full in all gazes and the vision was same as that at presentation. Thereafter, the patient was followed up every 3 months for 1 year and six monthly for the next 1 year. The patient is currently both objectively and subjectively free from tumor recurrence, 2.5 years after treatment.
Figure 4.

Gross appearance 1 month after completion of treatment, showing healthy conjunctiva with macular grade corneal opacity in the lower peripheral part of cornea extending from 5-o’ clock to 7-o’ clock position
Discussion
Histogenesis of ocular sebaceous gland carcinoma is unknown; yet, prevailing opinion suggests that this tumor arises from a single pluripotent reserve cell rather than squamous metaplasis of adenocarcinoma. There are only few case reports or series of solitary conjunctival sebaceous carcinoma. Honavar and associates reported a case of a 33-year-old woman with sebaceous carcinoma confined to the palpebral conjunctiva.[4] Margo and Grossniklaus reported two cases of intraepithelial sebaceous carcinoma involving the tarsal and bulbar conjunctiva.[5]
Our case is unique in several respects. The perilimbal origin, involvement of cornea and bulbar conjunctiva and imprint cytology suggested adenosquamous carcinoma. Diagnosis of sebaceous carcinoma was through HPE of excised mass.
Histopathologically, sebaceous carcinoma may mimic squamous and basal cell carcinoma. Immunohistochemical staining profiling with antibodies like anti-epithelial membrane antigen (anti-EMA), BRST-1 (anti-BCA-225) and Cam-5.2 (anti-low molecular weight keratin) may help differentiate it from squamous and basal cell carcinoma when distinction by microscopy alone fails or is equivocal. Management consisted of wide local excision with cryotherapy of tumor bed and topical 5-FU was used both as neo-adjuvant and adjuvant treatment. Only one case of primary bulbar conjunctival sebaceous carcinoma has been reported where multiple small corneoscleral masses were seen with limbal ulceration and topical Mitomycin C was used when pagetoid spread was seen after surgery.[3] In our case, the mass was solitary, measuring 20 × 16 mm and involving cornea as well as bulbar conjunctiva. Absence of pagetoid spread may be attributed to the use of topical 5-FU before surgery and its continued use after surgery for 1 month.
Following treatment modalities have been described for malignant conjunctival tumors: Primary excisional biopsy, cryotherapy of tumor bed, eyelid and conjunctival reconstruction, topical chemotherapy, plaque radiotherapy and lastly orbital exenteration depending on the extent of tumor. Various chemotherapeutic drugs have been used: Mitomycin C, 5-FU and a-interferon.[6] 5-FU was chosen in our patient due to financial restraints and concerns regarding compliance to follow-up. Besides being inexpensive, 5-FU is stable in aqueous solution for 3–4 weeks and does not require refrigeration. It does not have epitheliotoxic effects and can be used before complete healing of corneal wounds unlike Mitomycin C.[7]
In conclusion, our patient is an evidence for the fact that though sebaceous gland carcinoma is a lid tumor, solitary bulbar conjunctiva involvement is possible, and should be kept as differential diagnosis in patients presenting with mass in bulbar conjunctiva with or without involvement of lid. Topical 5-FU is a cost-effective choice and allows ease of administration when used for neo-adjuvant and adjuvant treatment of sebaceous gland carcinoma.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Batsakis JG, Littler ER, Leahy MS. Sebaceous cell lesions of the head and neck. Arch Otolaryngol. 1972;95:151–7. doi: 10.1001/archotol.1972.00770080239012. [DOI] [PubMed] [Google Scholar]
- 2.Prioleau PG, Santa Cruz DJ. Sebaceous gland neoplasia. J Cutan Pathol. 1984;11:396–414. doi: 10.1111/j.1600-0560.1984.tb00397.x. [DOI] [PubMed] [Google Scholar]
- 3.Park SJ, Wee WR, Lee JH, Kim MK. Primary sebaceous carcinoma of the corneoscleral limbus with pagetoid recurrence. Korean J Ophthalmol. 2009;23:104–7. doi: 10.3341/kjo.2009.23.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Honavar SG, Shields CL, Maus M, Shields JA, Demirci H, Eagle RC, Jr, et al. Primary intraepithelial sebaceous gland carcinoma of the palpebral conjunctiva. Arch Ophthalmol. 2001;119:764–7. doi: 10.1001/archopht.119.5.764. [DOI] [PubMed] [Google Scholar]
- 5.Margo CE, Grossniklaus HE. Intraepithelial sebaceous neoplasia without underlying invasive carcinoma. Surv Ophthalmol. 1995;39:293–301. doi: 10.1016/s0039-6257(05)80106-7. [DOI] [PubMed] [Google Scholar]
- 6.Kim JW, Abramson DH. Topical treatment options for conjunctival neoplasms. Clin Ophthalmol. 2008;2:503–15. doi: 10.2147/opth.s1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yeatts RP, Ford JG, Stanton CA, Reed JW. Topical 5-fluorouracil in treating epithelial neoplasia of the conjunctiva and cornea. Ophthalmology. 1995;102:1338–44. doi: 10.1016/s0161-6420(95)30866-4. [DOI] [PubMed] [Google Scholar]


