Abstract
In the National Longitudinal Study of Adolescent Health, a US longitudinal study of over 15,000 young adults, we examined the extent to which socioeconomic status is linked to systolic blood pressure, and whether biobehavioral risk factors mediate the association. Over 62% of the participants had systolic blood pressure >120 mmHg and 12% with systolic blood pressure >140 mmHg. Over 66% were classified as at least overweight (Body Mass Index>25 kg/m2), with over 36% meeting criteria for at least Class I obesity (Body Mass Index>30 kg/m2). Multivariate models showed that higher household income and being married were independently associated with lower systolic blood pressure. Higher body mass index, greater waist circumference, smoking, and higher alcohol intake were each independently associated with higher systolic blood pressure. Meditational analyses suggested that higher education level was associated with lower systolic blood pressure by way of lower body mass, smaller waist circumference, and lower resting heart rate. When these indirect effects were accounted for, education was not significantly associated with systolic blood pressure. In contrast, household income remained associated with systolic blood pressure even with control for all covariates. Results reinforce current public health concerns about rates of obesity and high blood pressure among young adults and suggest that disparities in education level and household income may play an important role the observed decrements in health. Identifying modifiable mechanisms that link socioeconomic status to systolic blood pressure using data from a large representative sample may improve risk stratification and guide the development of effective interventions.
Keywords: Systolic Blood Pressure, Socioeconomic Status, Education, Income, Body Mass Index, Biobehavioral Risk
Introduction
High blood pressure continues to be prevalent in the United States, conferring increased morbidity and mortality e.g.,1,2, and remains a significant economic burden on the health care system 3. Recently much attention has been paid in the scientific literature 4 and popular press 5 to substantial increases in the prevalence of biobehavioral risk factors for high blood pressure among young adults. Although advances in treatment of high blood pressure have apparently stabilized the rates of high blood pressure for the present 6, further elucidating how modifiable biobehavioral risk factors are related to high blood pressure may provide additional opportunities for maintaining or improving upon these advances in this population.
Modifiable biobehavioral risk factors for high blood pressure include body mass index (BMI), waist circumference, heart rate (HR), alcohol consumption, exercise, and smoking7. Lower socioeconomic status (SES) also has been associated with a poorer biobehavioral risk profile, and in turn with higher systolic blood pressure (SBP)8-10. Recent evidence from a French sample aged 30-7910 has shown that body shape, heart rate, and health behaviors may account for a sizable amount of the association between SES and SBP. In the present study we adopt the theoretical framework used in the French study10 to further examine the association between SES and SBP using data from a nationally representative sample of approximately 15,000 young adults in the U.S. Our aims are to assess the independent predictive association between SES indices, biobehavioral factors, and SBP and to examine these biobehavioral risk factors as possible mediators of the association between SBP and SES. We focus on SBP in the present study because SBP has been shown to be more important than diastolic blood pressure (DBP) with respect to health risk 11-13, and also possibly more responsive than DBP to changes in modifiable risk factors14. Results from the present study could improve risk stratification in clinical settings and inform interventions aimed at reductions in social disparities in health, and also further inform the generalizability of the association between SES and SBP across cultures and age cohorts.
Methods
Participants
The current study uses data from the Add Health study, a nationally representative sample of approximately 15,000 young adults that was designed to assess the effects of health-related behaviors during adolescence and into young adulthood. The study was reviewed and approved by the IRB at the University of North Carolina-Chapel Hill. Written consent was obtained for all data collection. The participants have been followed from grades 7 through 12 in 1995 through early adulthood in 2008in 4 waves of data collection15. Participants without SBP measures or survey sample weights were excluded, leaving a final sample of 14,299.
Measures
Demographic Measures
Age and marital status (yes/no) were recorded assessed at Wave IV. Race was constructed from a series of queries at Wave I.
Systolic Blood Pressure, Resting Heart Rate and Cardiac Medication use
Certified field interviewers measured respondents' resting, seated systolic and diastolic blood pressures (mmHg) and pulse rate (beats/minute).16 Following a five-minute seated rest, three serial measurements were performed at 30-second intervals using a factory calibrated, Microlife BP3MC1-PC-IB oscillometric blood pressure monitor (MicroLife USA, Inc.; Dunedin, FL); and SBP was constructed as the average of measures 2 and 3 and are highly reliable17. Cardiac medication status was assessed at the Wave IV in-home interview.
BMI and Waist Circumference
Height, weight, and waist circumference were assessed at Wave IV. BMI was calculated as BMI = weight (kg) / height (m2). BMI was modeled in its continuous form in our primary analyses, but for descriptive purposes also was reported in categories: BMI < 25 = normal weight; 25-29.9 = overweight; 30-34.5 = obese class I; 35-39.5 = obese class II; > 40 = morbidly obese 18. Waist circumference was measured to the nearest 0.5 cm at the superior border of the iliac crest. 16
Physical Exercise, Alcohol Consumption, and Smoking Behavior
Exercise was represented by a yes/no variable that assessed regular (on a weekly basis) participation in any bouts of physical activity such as walking or strenuous sports19. Alcohol Consumption was defined as follows: 0 = non-drinker; 1 = occasional drinker, drink 2 or fewer days of the week; 2 = light, drink 5-7 days per week and 2 or fewer drinks (1 or fewer if female); 3 = moderate, drink 5 - 7 days per week, 3 drinks for males, 2 drinks for females; 4 = heavy, drink 5 -7 days per week, more than 3 drinks for males, more than 2 for females. Smoking was coded yes/no indicating current daily smoking. All of the above variables were assessed at Wave IV, concurrent with the SBP measurement.
Individual and Parental Education
Education was coded as the highest level reported (at Wave IV for respondent, Wave I for parent), as follows: 1= some high school or less; 2 = graduated high school; 3 = some college or vo-tech; 4 = bachelor's degree; 5 = some graduate school or more. Participants completing G.E.D.s were grouped in the lower level of education class 20.
Financial Strain, Home Ownership, Built Environment, and Household Income
Income, Financial Strain, and Home Ownership were assessed at Wave IV. Financial strain was derived from 6 questions that assessed whether individuals reported the inability to pay bills, buy food, etc. A “Built Environment” measure (rated by the field interviewer) was the sum of two Likert-type items assessed at Wave I regarding how well the building in which the respondent lived was maintained, and the surrounding buildings were maintained. The summed score had a possible range of 2-8 with higher scores reflecting poorer maintenance. Annual household income was assessed using ordered categories. In order to create an ordinal income measure, we assigned the midpoint value to each category, resulting in the 13 values ranging from $2,500 to ≥$150,000.
Statistical analysis
Sample characteristics were described as median (interquartile range) for continuous variables and frequency (percent) for categorical measures. Analyses were carried out using SAS version 9.2 (Cary, NC), R software (http://cran.r-project.org), and Mplus21. Statistical models were weighted using grand sample weights and adjusted for individual school membership. We first conducted a series of linear regression models estimating the independent associations between the predictor variables and SBP, first adjusted for only age, gender, and cardiac medication, and then adjusted for all predictors under study, a “full” model. To capture nonlinearity for several variables we used a piecewise regression or “hockey stick” approach.
We then estimated a path model in which the associations between respondent education and household income on SBP were mediated by the biobehavioral variables. Significance tests were two-sided and a value of p < 0.05 was considered “significant.”
Further details on the above assessments and statistical analyses can be found in the data supplement: http://hyper.ahajournals.org
Results
Table 1 shows the unweighted sample characteristics. The majority of participants were white females, with mean age of 29 years. Median SBP was 123.5 mmHg and median BMI was 27.6. About 3.7% of the sample was taking some form of cardiac medication. Over 62% of the participants had SBP > 120 mmHg and 12% with SBP > 140. Over 66% were classified as at least overweight (BMI 25-29.9).
Table 1. Descriptive Statistics (N=14,299).
| Background Variable | N | Median or percent | Interquartile range or frequency |
|---|---|---|---|
| SBP, mmHg | 14,299 | 123.5 | 115.0, 132.5 |
| Age, years | 14,299 | 29.0 | 28.0, 30.0 |
| Male | 14,299 | 47% | 6,713 |
| Race | 14,288 | ||
| Hispanic | 16% | 2,221 | |
| Black | 22% | 3,091 | |
| Asian | 6% | 914 | |
| Native. American | 2% | 257 | |
| Other | 1% | 125 | |
| White | 54% | 7,680 | |
| Cardiac Medication | 14,299 | 4% | 523 |
| Financial Strain | 14,292 | 25% | 3,525 |
| Married | 14,282 | 50% | 7,189 |
| Annual Household Income ($US × 1000) | 13,368 | 62.5 | 33.0, 87.5 |
| Own Home | 14,276 | 41% | 5,822 |
| Built Environment (scale 2-8, best to worst) | 14,131 | 3.0 | 2.0, 4.0 |
| Respondent Education | 14,295 | ||
| < High School | 8% | 1,108 | |
| High School | 16% | 2,296 | |
| Some College | 44% | 6,315 | |
| College | 20% | 2,814 | |
| Post-graduate | 12% | 1,762 | |
| Parent Education | 14,079 | ||
| < High School | 15% | 2,141 | |
| High School | 23% | 3,212 | |
| Some College | 29% | 4,113 | |
| College | 18% | 2,582 | |
| Post-graduate | 14% | 2,031 | |
| Heart Rate (pulse) beats/minute | 14,218 | 73.5 | 66.0, 81.5 |
| Body Mass Index (kg/m2) | 14,160 | 27.6 | 23.7, 32.8 |
| Waist Circumference (cm) | 14,241 | 95.0 | 86.0, 107.0 |
| Alcohol Use | 14,201 | ||
| Never | 27% | 3,887 | |
| Occasional | 62% | 8,758 | |
| Light | 3% | 425 | |
| Moderate | 2% | 336 | |
| Heavy | 6% | 795 | |
| Exercise | 14,288 | 85% | 12,114 |
| Smoking | 14,183 | 22% | 3,059 |
N represents the number of non-missing cases
Note. Values are unweighted
Predictors of SBP
Among the background variables, African American race/ethnicity, male sex, age, and taking cardiac medication were positively associated with higher SBP (See Table 2). Adjusting only for age, gender, and cardiac medication, financial strain, built environment, alcohol intake, tobacco smoking, BMI, resting heart rate, and waist circumference were associated with SBP, while higher respondent and parental education, owning a home, being married, regular exercise and annual household income were inversely associated with SBP.
Table 2. Unstandardized regression coefficients from regression models.
| Initial model (Age, Gender, Medication Adjusted) |
Full Model (All potential predictors under study) |
|||
|---|---|---|---|---|
| Predictor | Regression coefficient | 95% Confidence Limits | Regression coefficient | 95% Confidence Limits |
| Background Factors | ||||
| Race | ||||
| Hispanic | 0.21 | -0.61, 1.03 | -0.49 | -1.29, 0.30 |
| African American | 2.14‡ | 1.39, 2.92 | 1.14 † | 0.39, 1.89 |
| Asian | -0.80 | -2.12, 0.52 | 0.73 | -0.52, 1.98 |
| Native American | 1.40 | -0.11, 2.91 | 0.48 | -0.95, 1.91 |
| Other | -2.43 | -4.57, -0.30 | -1.37 | -3.42, 0.67 |
| Caucasian (reference) | -- | |||
| Age (10 years) | 2.38† | 0.77, 4.00 | 1.93* | 0.38, 3.48 |
| Male | 9.90‡ | 9.49, 10.30 | 9.07‡ | 8.65, 9.49 |
| Cardiac Medication | 6.72‡ | 5.65, 7.78 | 4.17‡ | 3.15, 5.20 |
| SES Indices | ||||
| Married | -1.52‡ | -1.96, -1.08 | -1.21‡ | -1.66, -0.77 |
| HH Income (50K) | -0.90‡ | -1.10, -0.51 | -0.35* | -0.66, -0.04 |
| Own Home | -0.80‡ | -1.22, -0.35 | 0.09 | -0.35, 0.54 |
| Financial Strain | 0.50* | 0.02, 0.98 | -0.42 | -0.90, 0.07 |
| Parent's Education | ||||
| No High School (reference) | -- | -- | ||
| High School | 0.24 | -0.46, 0.94 | 0.21 | -0.47, 0.86 |
| Vocational | -0.32 | -1.01, 0.37 | -0.23 | -0.90, 0.44 |
| College | -1.22† | -2.00, -0.45 | -0.33 | -1.10, 0.44 |
| At least some post-grad | -1.32† | -2.18, -0.46 | -0.23 | -1.11, 0.64 |
| Participant's Education | ||||
| No High School (reference) | -- | -- | ||
| High School | 0.45 | -0.39, 1.29 | 0.06 | -0.74, 0.86 |
| Vocational | -0.46 | -1.22, 0.30 | -0.69 | -1.44, 0.05 |
| College | -1.22† | -2.09, -0.36 | -0.21 | -1.11, 0.69 |
| At least some post-grad | -1.40† | -2.36, -0.44 | 0.11 | -0.88, 1.11 |
| Built Environment | 0.26† | 0.12, 0.40 | 0.05 | -0.09,0.19 |
| Biobehavioral Factors | ||||
| Regular Exercise | -0.91† | -1.50, -0.32 | -0.56* | -1.12, -0.002 |
| Alcohol Intake | ||||
| None (reference) | -- | |||
| Occasional | 0.43 | -0.06, 0.92 | 0.88‡ | 0.39, 1.36 |
| Light | -0.12 | -1.38, 1.14 | 1.47* | 0.22, 2.73 |
| Moderate | 3.73‡ | 2.30, 5.15 | 5.31‡ | 3.92, 6.70 |
| Heavy | 3.92‡ | 2.99, 4.85 | 4.51‡ | 3.62, 5.41 |
| Current Smoking | 0.53* | 0.03, 1.02 | 0.61* | 0.11, 1.11 |
| BMI < 32(per one unit) | 0.82‡ | 0.77, 0.87 | 0.65‡ | 0.56, 0.74 |
| BMI ≥ 32 (per one unit) § | -0.52‡ | -0.61, -0.43 | -0.42‡ | -0.54, -0.30 |
| Resting heart rate < 72 (per 10 beats/minute) | 0.95‡ | 0.54, 1.36 | 0.09 | -0.30, 0.49 |
| HR ≥ 72 (per 10 beats/minute) § | 0.38 | -0.21, 0.97 | 0.53 | -0.03, 1.09 |
| Waist circumference < 100 cm (per 10 cm) | 0.32‡ | 0.30, 0.35 | 0.91‡ | 0.50, 1.32 |
| Waist ≥ 100 (per 10 cm) § | -0.16‡ | -0.20, -0.12 | -0.57* | -1.10, -0.05 |
Values in parentheses next to continuous predictors represent points of comparison along regression line. For example, for the first set of models reported in column two, each $50,000 increase in annual income is associated with about a 0.90 mmHg reduction in SBP.
p = 0.05; † p = 0.01; ‡ p = 0.001
Coefficients involving BMI, waist circumference, and heart rate are from a linear piecewise (hockey stick) estimate in which the regression slope is allowed to bend once at an inflection point. This procedure generates two coefficients for each variable, each coefficient representing the two different slope regions. For example, in column 1, the coefficient for waist circumference < 100 (second column) is about 0.32, which is the regression slope for individuals whose waist circumferences is 100 cm or less. The coefficient for waist circumference ≥ 100 represents the change in that slope for individuals whose waist circumference is greater than 100 cm. Above 100 cm, the slope is -0.16 less steep than the slope for waist circumference less than 100 cm, i.e., the slope for waist circumference beyond 100 cm is 0.33 + (-0.16) = 0.14.
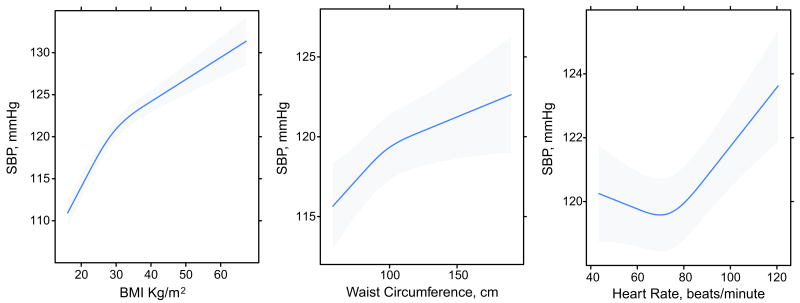
In the fully adjusted model, the background variables age, male sex, cardiac medication use, and African American race remained significantly, positively associated with SBP. Annual income and being married maintained their significant negative association with SBP, while moderate and heavy alcohol intake remained strongly associated with higher SBP. Cigarette smoking also was associated with higher SBP. Strong, independent associations were observed for BMI and waist circumference (See Figure 1), with higher values corresponding to higher SBP. Higher resting heart rate also was also associated with higher SBP, although the p-value was 0.06.
Figure 1.
Predicted SBP as a function of BMI, waist circumference, and resting heart rate for a typical participant (White, female, unmarried, unmedicated, with some college education, and average values of remaining covariables). Shaded area represents 95% confidence intervals for regression estimate.
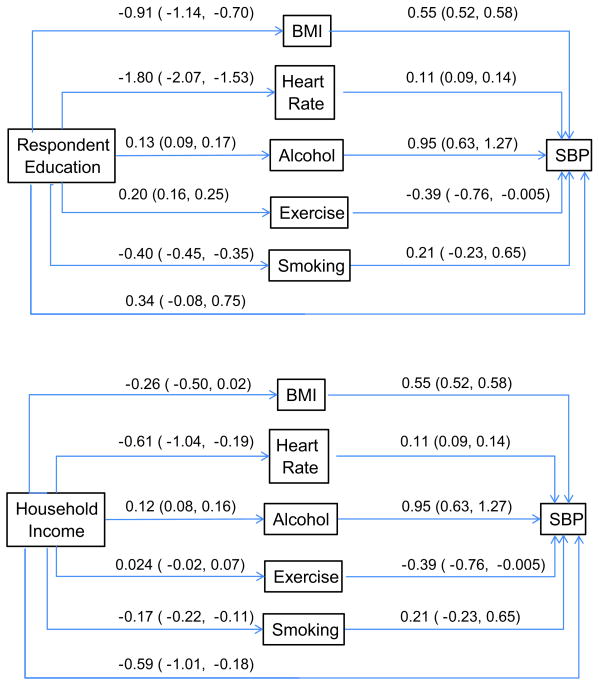
Mediation path model results are displayed in Figure 2. Estimates for respondent education (upper panel) and household income (lower panel) were produced from a single model that included all variables simultaneously, but are separated in the figure for presentational clarity. Higher levels of respondent education were associated with lower BMI, lower resting heart rate, less smoking, and more frequent exercise. Higher education level was associated with greater alcohol intake. The indirect effects of respondent education through BMI and through resting heart rate were statistically significant (see Table S2, http://hyper.ahajournals.org). For every one category increase in education, there was roughly a 0.5 mmHg decrease in SBP by way of BMI, and a 0.2 mmHg decrease by way of resting heart rate. In contrast, for every one level increase in education, there also was a 0.13 mmHg increase in SBP by way of alcohol intake. The indirect effects of education through exercise and smoking were not statistically significant. Waist circumference and BMI were not simultaneously modeled due to their strong correlation. We therefore re-estimated the primary path model replacing BMI with the waist measure. In this model, education was inversely associated with waist circumference (unstandardized path coefficient = -2.71, 95% CI = -3.20, -2.26). The unstandardized indirect effect for education via waist was -0.64 (95% CI = -0.76, -0.53)1. The overall indirect effect of education across the entire set of biobehavioral variables was -0.91 (95% CI = -1.19, -0.63). Finally, after accounting for all the indirect effects via biobehavioral mediators, the direct effect of respondent education on SBP was no longer statistically significant. Combining the direct effect with all indirect effects yielded a total effect for education on SBP of -0.59 (95% CI = -0.91, -0.26).
Figure 2.
Results of path model estimating indirect effects from education and income to SBP by way of biobehavioral variables. Values are unstandardized path weights with 95% confidence limits. Weights can be interpreted in original metric of the variable. Linearity was assumed for all associations. Results were estimated simultaneously from the same model, but separated here for presentational clarity.
Higher household income was associated with lower resting heart rate and higher alcohol intake (See Figure 2). In contrast to respondent education, although the specific indirect effects of income by way of alcohol and resting heart rate were statistically significant (see bottom section of Table S2), the total indirect effect was not. Moreover, the direct effect was statistically significant, with each $50,000 increase associated with a decrease in SBP of about 0.61 mm Hg. The total effect of household income on SBP was -0.74 (95% CI = -1.19, -0.29) and statistically significant. As with BMI, waist circumference was inversely associated with SBP [unstandardized path coefficient = -1.71 (95% CI = -2.43, -1.03)]. The unstandardized indirect effect of household income on SBP via waist circumference was also significant [-0.41 (95% CI = -0.54, -0.24)].
Discussion
A striking number of these young adults displayed clinically relevant elevations in both SBP and BMI. Among the most noteworthy findings from the conventional regression model was that the only SES indices that only income and marital status remained significantly related to SBP after adjustment for biobehavioral risk factors and other SES indicators. Our findings regarding the mediating path from education level to SPB by way of BMI, resting heart rate, and alcohol consumption are consistent with those of Chaix et al.10 However, our findings diverge from the French study in that we did not find that the total effect of education level on SBP was accounted for by these indirect biobehavioral mediators. This discrepancy may be the result of cultural differences between French and American cultures, the younger age of our sample and/or our larger sample size. In addition, the availability of government-sponsored health care in France, for example, could have buffered the SBP-raising effects of lower household income there. Another intriguing possibility is that the recent economic recession resulted in loss of jobs and diminished household income among Add Health participants at just about the time the Wave IV data collection was under way, thereby potentiating the impact of such a recent reduction in household income on SBP. Supporting this possibility is the recent report 22 that there was an increase in acute MI rates during the stock market decline of October, 2008, to April, 2009.
Our findings may have important implications for approaches to prevention of high blood pressure. Mediation of the low education association with SBP via increased BMI and waist circumference is consistent with the long-recognized importance of steps to decrease BMI and central obesity in any cardio-preventive program. The independent effect of lower heart rate to mediate the effects of both low education and household income on SBP points to the importance of also identifying interventions that can reduce resting heart rate. One such intervention is aerobic exercise, which is also long-recognized as an important cardio-preventive measure.
Finally, the emergence of smoking, being married, and increased alcohol consumption as independent correlates of SBP point to the importance of smoking cessation and limiting alcohol consumption as potentially important preventive approaches. The salutatory effects of marriage and social support in general have been widely studied e.g.,23 with the majority of findings being consistent with ours.
The cross-sectional nature of this study precludes conclusions regarding causality and the present findings may generalize only to individuals 24 to 32 years of age. In addition, as with any observational study, unmeasured factors may have significantly contributed to the present associations. For example, genetic profiles could be associated with socioeconomic status, as well as SBP.
Perspectives
We have shown that indices of lower SES are associated with increased SBP and that increased BMI and waist circumference and higher resting heart rate are significant mediators of these associations. These findings strengthen the case that lower SES is a risk factor for cardiovascular disease and that increased BMI and central obesity are important mediators of this effect. Interventions that promote weight loss and reduce resting heart rate have the potential to reduce the impact of low SES on SBP, especially among young adults which will further reduce the cardiovascular health burden of the US population as they age into middle and older adulthood.
Supplementary Material
Acknowledgments
Jon Hussey, PhD provided helpful commentary on the initial drafts of this manuscript.
Sources of Funding: This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01 HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). This research was also supported by Grant Number P01 HL36587 from the National Heart Lung and Blood Institute.
Footnotes
Disclosures: None.
The primary path model also specified indirect effects of education on SBP by way of household income and biobehavioral variables; these associations were all trivial in magnitude and not statistically significant.
References
- 1.Crews DC, Plantinga LC, Miller ER, Hedgeman SR, Saydah SH, Williams DE, Powe NR Centers for Disease Control and Prevention Cronic Kidney Disease Surveillance Team. Prevalence of chronic kidney diesease in persons with undiagnosed or prehypertension in the United States. Hypertension. 2010;55:1102–1109. doi: 10.1161/HYPERTENSIONAHA.110.150722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Falkner B, Lurbe E, Schaefer F. High blood pressure in childern: clinical and health policy implications. J Clin Hypertens. 2010;12:261–276. doi: 10.1111/j.1751-7176.2009.00245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hammond RA, Levine R. The economic impact of obesity in the United States. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 2010;3:285–295. doi: 10.2147/DMSOTT.S7384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CDC, Centers for Disease Control and Prevention. US Obesity Trends. 2009. [Google Scholar]
- 5.Reuters. 2010 http://www.reuters.com/article/idUSTRE6A35SO20101104)
- 6.Yoon SS, Ostchega Y, Louis T. Recent trends in the prevalence of high blood pressure and its treatment and control, 1999-2008. Services US Department of Health and Human Services: National Center for Health Statistics. Data brief No. 48. 2010 [PubMed] [Google Scholar]
- 7.Niskanen L, Laaksonen DE, Nyyssonen K, Punnonen K, Valkonen VP, Fuentes R, Tuomainen TP, Salonen R, Salonen JT. Inflammation, abdominal obesity, and smoking as predictors of hypertension. Hypertension. 2004;44:859–865. doi: 10.1161/01.HYP.0000146691.51307.84. [DOI] [PubMed] [Google Scholar]
- 8.Metcalf PA, Scragg RR, Schaaf D, Dyall L, Black PN, Jackson RT. Comparison of different markers of socieoconomic status with cardiovascular disease and diabetes risk factors in the Diabetes, Heart and Health Survey. N Z Med J. 2008;121:45–56. [PubMed] [Google Scholar]
- 9.Manuck SB, Phillips JE, Gianaros PJ, Flory JD, Muldoon MF. Subjective socioeconomic status and presence of the metabolic syndrome in midlife community volunteers. Psychosom Med. 2010;72:35–45. doi: 10.1097/PSY.0b013e3181c484dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chaix B, Bean K, Leal C, Thomas F, Harvard S, Evans D, Jego B, Pannier B. Individual/neighborhood social factors and blood pressure in the RECORD Cohort Study: Which risk factors explain the associations? Hypertension. 2010;55:769–775. doi: 10.1161/HYPERTENSIONAHA.109.143206. [DOI] [PubMed] [Google Scholar]
- 11.Kim JH, Jittiwat J, Ong WY, Farooqui AA, Jenner AM. Changes in cholesterol biosynthetic and transport pathways after excitotoxicity. J Neurochem. 2010;112:34–41. doi: 10.1111/j.1471-4159.2009.06449.x. [DOI] [PubMed] [Google Scholar]
- 12.Ong AD. Pathways linking positive emotion and health later in life. Current Directions in Psychological Science. 2010;19:358–362. [Google Scholar]
- 13.Bobrovskaya L, Damanhuri HA, Ong LK, Schneider JJ, Dickson PW, Dunkley PR, Goodchild AK. Signal transduction pathways and tyrosine hydroxylase regulation in the adrenal medulla following glucoprivation: an in vivo analysis. Neurochem Int. 2010;57:162–167. doi: 10.1016/j.neuint.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 14.Mather M, Carstensen LL. Aging and attentional biases for emotional faces. Psychol Sci. 2003;14:409–415. doi: 10.1111/1467-9280.01455. [DOI] [PubMed] [Google Scholar]
- 15.Harris CM, Halpern CT, Whitsel AE, Hussey DJ, Tabor JW, Entzel PP, Udry JR. The National Longitudinal Study of Adolescent Health Research Design. 2009 http://www.cpc.unc.edu/projects/addhealth/design.
- 16.Entzel PP, Whitsel AE, Richardson A, Tabor JW, Hallquist S, Hussey DJ, Halpern CT, Harris KM. Add Health Data Guides: Wave IV cardiovascular and anthropometric documentation. 2009. [Google Scholar]
- 17.Nguyen QC, Tabor JW, Entzel PP, Lau Y, Suchindran C, Hussey JM, Halpern CT, Harris KM, Whitsel AE. Discordance in National Estimates of Hypertension Among Young Adults. Epidemiology. doi: 10.1097/EDE.0b013e31821c79d2. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.WHO. Technical Report Series 894. Obesity: Preventing and Managing the Global Epidemic. Geneva, Switzerland: 2000. [PubMed] [Google Scholar]
- 19.Harris KM. An integrative approach to health. Demography. 2010;47:1–22. doi: 10.1353/dem.0.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perreira KM, Harris KM, Lee D. Making it in America: High school completion by immigrant and native youth. Demography. 2006;43:511. doi: 10.1353/dem.2006.0026. [DOI] [PubMed] [Google Scholar]
- 21.Muthen LK, Muthen BO. Mplus User's Guide. Third Edition. Los Angeles: CA: Muthen & Muthen; 1998-2004. [Google Scholar]
- 22.Fiuzat M, Shaw LK, Thomas L, Felker GM, O'Connor CM. United States stock market performance and acute myocardial infarction rates in 2008-2009 (from the Duke Databank for Cardiovascular Disease) Am J Cardiol. 2010;106:1545–1549. doi: 10.1016/j.amjcard.2010.07.027. [DOI] [PubMed] [Google Scholar]
- 23.Brummett BH, Barefoot JC, Siegler IC, Clapp-Channing NE, Lytle BL, Bosworth HB, Williams RB, Mark DB. Characteristics of socially isolated patients at elevated risk for cardiac mortality. Psychosomatic Medicine. 2001;62:790–795. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.