Abstract
Background: How to improve treatment for negative symptoms is a continuing topic of debate. Suggestions have been made to advance psychological understanding of negative symptoms by focusing on the social cognitive processes involved in symptom formation and maintenance. Methods: Following the recommendations by the National Institute of Mental Health workshop on social cognition in schizophrenia, this study investigated associations between negative symptoms and various aspects of social cognition including Theory of Mind (ToM), attribution, empathy, self-esteem, and interpersonal self-concepts in 75 patients with schizophrenia spectrum disorders and 75 healthy controls. Results: Negative symptoms were significantly associated with difficulties in ToM, less readiness to be empathic, lower self-esteem, less self-serving bias, negative self-concepts related to interpersonal abilities, and dysfunctional acceptance beliefs. Different aspects of social cognition were mildly to moderately correlated and interacted in their impact on negative symptoms: Difficulties in ToM were associated with negative symptoms in persons with low but not in persons with medium or high levels of self-esteem. Taken together, the social cognition variables and their hypothesized interaction explained 39% of the variance in negative symptoms after controlling for neurocognition and depression. Conclusions: The results highlight the relevance of self-concepts related to social abilities, dysfunctional beliefs, and global self-worth alone and in interaction with ToM deficits for negative symptoms and thereby provide a helpful basis for advancing psychosocial interventions.
Keywords: negative symptoms, social cognition, theory of mind, self-esteem, self-concepts, neurocognition, depression
Introduction
Negative symptoms, defined as blunted affect, alogia, asociality, avolition, and anhedonia, are a key element of schizophrenia.1 It has been agreed that they constitute a distinct and important therapeutic domain.2 Nevertheless, the effectiveness of available interventions for negative symptoms is far from satisfactory: Cognitive-behavioral therapy (CBT) shows some impact on negative symptoms but the effect sizes are small.3 Even psychosocial approaches specifically developed to reduce negative symptoms have failed to produce convincing effects.4 The same holds true for pharmacological treatments5 of which some might even be producing adverse effects.6,7
How to improve treatment for negative symptoms is thus an ongoing topic of debate. Whereas the suggestions made by the National Institute of Mental Health-measurement and treatment research to improve cognition in schizophrenia (NIMH-MATRICS) group on negative symptoms2 focus largely on pharmacological research, others have suggested to broaden the perspective and include models from a range of domains, including cognitive models.8 Indeed, research on negative symptoms might benefit from the way in which the abundant research on positive symptoms has led to the identification of specific cognitive biases (eg, reasoning biases,9 attribution style,10 impaired self-worth11) and has thereby inspired the development of increasingly specific models and interventions for positive symptoms.12,13 An equally detailed understanding of the cognitive underpinnings of negative symptoms could advance the existing theoretical models14 and thereby facilitate the identification of further targetable domains for psychological treatments.
For a long time, the focus in negative symptoms has been on neurocognition due to its stronger association with negative than with positive symptoms15 and its potential to impact on work-related performance. However, even this association is small and treatments focusing on improving neurocognition have had little effect on negative symptoms.16,17 Therefore, recent interest has shifted toward social cognition2,18 and related aspects such as self-concepts, dysfunctional beliefs, attitudes, and expectancies14,19 that are more closely associated with negative symptoms and might act as mediators between neurocognition and social functioning.20–23
Social cognition generally refers to the “mental operations that underlie social interactions, including perceiving, interpreting, and generating responses to the intentions, dispositions, and behaviors of others” (Green et al18, page 1211). It includes a broad array of concepts such as Theory of Mind (ToM), social perception, social knowledge, attribution and emotional processing, self-perception, empathy, and other reasoning biases.18 Difficulties in social cognition are likely to impact on the ability and motivation to engage in interpersonal relationships.
The majority of studies on social cognition and negative symptoms have focused on ToM, which has been shown to be associated with negative symptoms and other symptoms of psychosis.24 For other domains, there are single studies, at the most, finding negative symptoms to be associated with less ability to empathize,25 a decreased sense of self-efficacy26, social discomfort20, more negative self-evaluations,27 and asocial beliefs28. Moreover, most studies have focused only on single aspects of social cognition and therefore do not provide information on which aspects of social cognition are most closely linked to negative symptoms or how different aspects of social cognition interrelate in their effect on negative symptoms. In particular, individuals who have problems in correctly deriving the intentions or emotions of others based on cues provided by the other person or the situation are left with more room for speculation. This room is more likely to be filled with negatively biased conclusions of being rejected and, as a consequence, to social withdrawal in persons with preexisting negative beliefs about themselves than in persons who see themselves in a positive light.
In order to identify aspects of social cognition whose improvement promises the strongest impact on negative symptoms, the NIMH workshop on definitions, assessments, and research options of social cognition in schizophrenia18 suggested to include a wider assessment of social cognition and to analyze the relationships between multiple aspects of social cognition and negative symptoms more closely. Following this suggestion, this study investigated the associations between negative symptoms and various aspects of social cognition, including the ability to infer intentions and emotions of other people, empathy, attribution style, self-esteem, interpersonal self-concepts, and dysfunctional beliefs. The first objective was to identify key domains of impairment in patients with negative symptoms by comparing them to healthy controls. Furthermore, we aimed to establish the strength of the associations between various aspects of social cognition, neurocognition, and negative symptoms. We were also interested in assessing how much variance in negative symptoms could be explained by social cognition over and above neurocognition and depression. Finally, we investigated the interplay between the more skill-related aspects of social cognition and beliefs by testing the assumption that difficulties in ToM will be more closely related to negative symptoms in persons with negative than in persons with positive self-concepts.
Method
Recruitment Procedure
A total of 75 patients were assessed. The majority of these were recruited in the pretreatment phase of an outpatient treatment project of the University of Marburg (n = 59). In order to broaden the range of patients with regard to symptom severity and remission status, additional patients were recruited (n = 16) in surrounding inpatient psychiatric hospitals. Inclusion criteria were Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, (DSM-IV) criteria for schizophrenia (n = 66) and schizoaffective disorder (n = 9). The diagnoses were assessed using the Structured Clinical Interview for DSM-IV (SCID)29 by diploma psychologists who were in training as clinical psychologists and who had been trained to administer the SCID in a 10-hour intensive course. The diagnoses were based on information from the SCID interview (duration 100 min), the positive and negative syndrome scale (PANSS) (duration 50 min), and patient records which were obtained from previous treatments. Exclusion criteria were the presence of cerebral damage or substance addiction.
Healthy control participants (n = 75) were recruited through leaflets and advertisements in local newspapers. They were selected to match the patient sample in regard to sex, age, and degree of education. Exclusion criteria for healthy controls were cerebral damage, acute mental disorder, or lifetime psychotic symptoms, assessed with SCID.
All participants were required to have sufficient German language skills to complete the assessments. They signed informed consent and were paid for participation. The study was approved for by the national ethics committee of the German Society of Psychology (DGPs).
Measures
Measures of Psychopathology.
PANSS30 was assessed and rated by clinical psychologists with certified training by the PANSS Institute or (in 9 cases) with close supervision from a certified rater. The interrater reliability (intra class correlations) for a subsample of 67 patients was 0.89, 0.74, and 0.78 for the PANSS positive, negative, and general score, respectively. We used the PANSS negative factor identified by van der Gaag et al.31 This factor includes the PANSS items N1 (blunted affect), N2 (emotional withdrawal), N3 (poor rapport), N4 (apathetic social withdrawal), N6 (lack of spontaneity), G7 motor retardation, and G16 (active social avoidance).
To control for symptoms of depression, we used the German version of the “Beck Depression Inventory.”32 The BDI is a widely used, reliable, and well-validated 4-point 21-item self-report questionnaire designed to assess the severity of depressive symptoms over the preceding week.
Measures of Social Cognition.
ToM was assessed by a movie task of social situations.33 Participants were asked to watch 4 movie sequences presenting complex social situations and answer questions about the protagonists’ intentions, thoughts, and emotions in an open-ended format. Two scores were derived from the task: an ability to infer intentions (ToM intentions: range: 0–8) and an ability to infer emotions (ToM emotions: range: 0–8). In each film, one point was given for ToM intentions if the participant only understood the literal meaning of the sequence, an additional point was given for understanding the indirect information (hint) provided by the protagonists. For ToM emotions, 1 point was given for identifying 1 type and 2 points were given for identifying 2 types of emotions. Two independent raters categorized the answers of the participants. The interrater reliability on a subsample of n = 10 was κ = 0.73. Both tasks have demonstrated sufficient convergent and discriminant validity in a previous study.33
In addition, a second-order false-belief task by Pickup and Frith (2001) was enacted with playing figures. In the task, participants were asked to infer a patient’s belief about the behavior of a second patient who is uninformed about the new location of the television in a hospital. Memory questions tested the general understanding of the tasks. Responses were scored by a trained rater.
Empathy was assessed with the Empathy Scale34 a 4-point 25-item Likert-scale designed to measure the self-perception of one’s ability to empathize with other persons. The readiness for empathy subscale assesses the preparedness to infer the perception and behavior of other persons in imagined situations, whereas the social concern subscale quantifies the tendency to experience empathic behavior in real-life situations. The authors report good validity and acceptable reliability.34
Attributional style was assessed using the Internal, Personal, and Situational Attributions Questionnaire (IPSAQ).35 The IPSAQ consists of 32-items describing 16 positive and 16 negative self-referent social situations. For each situation, participants are required to imagine experiencing the situation, write down the most probable cause for the situation, and then categorize this cause as being either internal (due to him or herself), external-personal (due to other person or persons), or situational (due to circumstances or chance). Three positive and 3 negative interdependent subscales can be calculated, representing the numbers of internal, external-personal, and situational attributions for positive and negative events. Cronbachs alpha for the subscales is between .61 and .76, and data confirming validity have been provided.35 We calculated the self-serving bias (SSB) as suggested by the authors by subtracting the number of internal attributions for negative events from the number of internal attributions for positive events (a positive score represents a SSB). Furthermore, we calculated an external-causation-bias by dividing the number of all external attributions by the number of all internal attributions, with higher scores indicating the tendency to attribute events to the external factors rather than to the self and thereby reflect a decreased self of self-causation.
A global sense of self-worth was assessed with a German version of the Rosenberg Self-Esteem Scale (RSE).36 The RSE is a widely used 4-point 10-item scale to assess current levels of global self-esteem. Good reliability and validity of the RSE has been confirmed.37
Interpersonal self-concepts were assessed with the Frankfurt Scales of Self-concept [Frankfurter Selbstkonzeptskalen (FSKN)].38 The FSKN is a reliable 7-point 78-item-questionnaire developed for a differentiated assessment of self-concepts. Psychometric properties have been studied in large samples of patients with schizophrenia finding good reliability of the subscales.39 For this study, we used the following subscales that assess interpersonal related self-concepts: the 10-item subscale assertiveness toward groups and significant others (FSKN-ST), which assesses whether the individual perceives him or herself as being assertive toward others; the 6-item subscale contact and interpersonal abilities (FSKN-KU), which assesses the extent to which a person experiences her or himself as someone who is skilled, relaxed, and confident in communicating with others; the 6-item subscale self-estimation-by-others, which assessed the self-concept of being respected, trusted, loved, and accepted by relevant others.
Other related dysfunctional beliefs were assessed with the subscale need for acceptance derived from the German version of the Dysfunctional Attitude Scale (DAS)-acceptance.40 The subscale assesses interpersonal vulnerability (eg, I am nothing if a person I love does not love me) and was computed in accord with the factors used by Grant and Beck.22
Measures of Intellectual Functioning and Neurocognition.
As an estimate of premorbid intelligence, we used the information subscale of the German version of the Wechsler Intelligence Scale—Revised (WAIS-R).41
We used the subtest Logical Memory I of the Wechsler Memory Scale-Revised (WMS-R)42 which requires recall of short prose passages as an indicator of immediate episodic memory capacity, the completion times in the Trail Making Test (TMT)43 Part A and B to assess information processing speed and the difference score between Part B and Part A as indicators of cognitive flexibility.
Analyses
t-Tests were used to test for group differences in social cognition and neurocognition. Pearson 2-tailed correlations were used to assess the associations between the indicators of social cognition and the negative symptom factor. Linear regression analyses (method: ENTER) was used to test for the combined predictive effect of social cognition on negative symptoms. All predictors were centered around the grand mean by subtracting the mean score from each case. Following a procedure described by Aiken and West44 interactions between predictors were included in the equation by adding the product of the interacting variables as a predictor in the final block. Post hoc plotting was used to interpret significant interactions by recasting the regression equation as the regression of the criterion on one predictor.
All variables were checked for normality within the patient sample: There was slight positive skewness for the negative symptom factor (S = 0.78, SE = 0.28), for the TMT-A (S = 1.6, SE = 0.28), and the TMT-B (S = 1.2, SE = 0.31) and slight negative skewness for the ToM-intentions score (S = −0.74, SE = 0.28). There was slight positive kurtosis for the DAS-acceptance score (K = 2.0, SE = .55), the TMT-A (K = 3.6, SE = 0.55), and TMT-B (K = 2.2, SE = 0.62) and slight negative kurtosis for the ToM second-order score (K = −1.9, SE = 0.55). All other variables were normally distributed.
Results
The sociodemographic characteristics of the patient and control samples are depicted in the top part of table 1. There were no differences between the samples with regard to gender, educational status, IQ, or age. The patient sample had a mean duration of psychosis of 10 years (SD = 8.1, range: 1–35), had experienced a mean of 4.3 (SD = 6.4, range: 0–35) previous hospitalizations, and had a mean General Assessment of Functioning score of 44.3 (SD = 12.8, range: 21–80). All patients but 3 were taking antipsychotic medication. The mean Chlorpromazine equivalent dose was 389.2 (SD = 689.9). The mean PANSS scores were 16.1 (SD = 5.0, range: 7–28) for the positive scale, 14.6 (SD = 4.8, range: 7–29) for the negative scale, and 34.2 (SD = 7.7, range: 19–53) for the general pathology scale. The mean negative factor score was 17.1 (SD = 6.3, range: 8–38). The mean score on the BDI was 17.0 (SD = 9.2) and 15 patients had a diagnosis of comorbid affective disorder.
Table 1.
Sample Characteristics of Schizophrenia Patients and Healthy Controls
| Patients (n = 75) | Controls (n = 75) | Statistics | |
| Mean (SD) | Mean (SD) | ||
| Sociodemographic characteristics | |||
| Sex (female/male) | 28/47 | 33/42 | χ2 (1) = 0.69 n.s. |
| Age | 33.9 (10.3) | 33.9 (11.4) | T148 = −.03 n.s. |
| Education in years | 14.9 (3.7) | 15.0 (4.1) | T143.7 = -1.4 n.s. |
| Intellectual functioning and neurocognitive performance | |||
| Verbal IQ (HAWIE) | 104.8 (19.0) | 109.5 (17.4) | T146.9 = −1.6 n.s. |
| Logical Memory I (WMS-R) | 25.8 (8.8) | 31.9 (7.7) | T108 = −3.8 (P ≤ .001) |
| TMT Part A | 32.2 (15.0) | 25.7 (9.0) | T119.3 = 3.2 (P ≤ .01) |
| TMT Part B | 61.5 (27.4) | 50.2 (23.8) | T131 = 2.5 (P ≤ .05) |
| TMT Part A-Part B | −30.8 (19.7) | −22.8 (16.2) | T109.4 = −2.5 (P ≤ .05) |
| Social cognition | |||
| Theory of Mind | |||
| Second order | 1.5 (1.4) | 2.22 (1.24) | T145.5 = −3.0 (P ≤ .01)** |
| Intentions | 5.5 (1.7) | 6.1 (1.3) | T133.4 = −2.4 (P ≤ .05) |
| Emotions | 3.8 (1.4) | 4.4 (1.3) | T147 = −2.4 (P ≤ .05)* |
| Empathy | |||
| Readinessa | 2.3 (.59) | 2.3 (.66) | T77 = 0.55 n.s. |
| Social concerna | 1.5 (.64) | 1.3 (.62) | T75 = 1.4 n.s. |
| Attribution | |||
| IPSAQ—SSB | 15.9 (24.3) | 27.5 (23.2) | T147 = −3.0 (P ≤ .01)** |
| IPSAQ—ECB | 8.9 (5.3) | 9.9 (3.7) | T131 = −1.3 n.s. |
| RSE | 18.5 (6.9) | 24.1 (4. 6) | T128.4 = −5.9 (P ≤ .001)** |
| Interpersonal concepts | |||
| FSKN—ST | 42.2 (12.1) | 54.0 (11.2) | T147 = −6.2 (P ≤ .001)** |
| FSKN—KU | 22.8 (5.1) | 26.0 (4.8) | T147 = −3.7 (P ≤ .001)** |
| FSKN—WA | 23.0 (5.9) | 27.4 (4.9) | T147 = −3. 7 (P ≤ .001)** |
| DAS–acceptance | 38.6 (7.5) | 45.1 (7.0) | T95 = −3.6 (P ≤ .001)** |
Note: HAWIE, Wechsler Intelligence Scale Revised; WMS-R, Wechsler Memory Scale Revised; TMT, Trail Making Test; RSE, Rosenberg self-esteem scale; FSKN, Frankfurt Scales of Self-concept; FSKN-ST, assertiveness toward groups and significant others; FSKN-KU, contact and interpersonal abilities; FSKN-WA, self-estimation-by-others; DAS-acceptance, Dysfunctional Attitudes Scale subscale to assess dysfunctional acceptance beliefs. IPSAQ-SSB, Internal, Personal, Situational Attributions Questionnaires—self-serving bias; IPSAQ-ECB, Internal, Personal, Situational Attributions Questionnaires—external-causation-bias.
The empathy subscales were completed by a subgroup of patients (n = 45).
**P ≤ .01, *P ≤ .05 after applying Bonferoni correction within each category.
The inpatients (n = 16) and outpatients (n = 59) did not differ in regard to age, gender of IQ, duration of disorder, or previous hospitalizations. However, the inpatients had less years of education than outpatients 12.8 vs 15.5 (P < .05) and a higher proportion of men (88% vs 56%, P < .05).
In the bottom part of table 1, the indicators of social cognition are depicted. As expected, the patients displayed more difficulties in each of the ToM tasks, although the group differences in the ability to infer intentions was no longer significant after Bonferoni correction. The patients showed significantly less SSB and—in line with this—revealed lower self-esteem on the RSE, more negative interpersonal self-concepts on all the FSKN subscales, and more dysfunctional acceptance beliefs than the healthy controls. No differences between the groups were found for the empathy scores.
In table 2, the 2-tailed Pearson correlation coefficients between the PANSS negative factor and each of the indicators of social cognition are depicted for the patient sample as well as the intercorrelations between the various aspects of social cognition and neurocognition. Negative symptoms were significantly associated with difficulties in the abilities to infer emotions and intentions, less readiness to be empathic, less SSB, lower self-esteem, negative self-concepts related to contact and interpersonal abilities, and dysfunctional acceptance beliefs. There were some substantial correlations between the RSE score, the interpersonal self-concepts, and dysfunctional acceptance beliefs. Other aspects of social cognition were either unrelated (eg, ToM and self-concepts) or showed only small associations (eg, ToM and empathy, ToM and attribution biases, self-concepts and attribution biases).
Table 2.
Intercorrelations Between Negative Symptoms, Social Cognition, and Neurocognition in Patients With Schizophrenia and Schizoaffective Disorder
| NEG | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
| ToM | ||||||||||||||||
| 1. Second order | −0.22 | |||||||||||||||
| 2. Intentions | −0.26* | 0.32** | ||||||||||||||
| 3. Emotions | −0.34** | 0.26* | 0.35** | |||||||||||||
| Empathy | ||||||||||||||||
| 4. Readinessa | −0.32* | 0.28 | −0.01 | 0.31* | ||||||||||||
| 5. Social concerna | −0.13 | 0.17 | 0.04 | 0.14 | 0.58** | |||||||||||
| Attribution biases | ||||||||||||||||
| 6. IPSAQ-SSB | −0.25* | 0.15 | −0.14 | 0.07 | 0.12 | 0.15 | ||||||||||
| 7. IPSAQ ECB | −0.08 | 0.29* | −0.21 | 0.04 | 0.10 | −0.08 | 0.38** | |||||||||
| Self-concept | ||||||||||||||||
| 8. RSE | −0.36** | 0.12 | −0.14 | 0.02 | −0.07 | −0.02 | 0.29* | 0.15 | ||||||||
| Interpersonal concepts | ||||||||||||||||
| 9. FSKN-ST | −0.12 | 0.07 | 0.03 | 0.06 | 0.01 | −0.01 | 0.10 | −0.04 | 0.55** | |||||||
| 10. FSKN-KU | −0.44** | 0.05 | 0.15 | 0.30** | 0.08 | −0.23 | 0.21 | 0.08 | 0.55** | 0.44** | ||||||
| 11. FSKN-WA | −0.35* | 0.02 | 0.13 | 0.01 | 0.01 | −0.08 | 0.06 | −0.15 | 0.52** | 0.41** | 0.42** | |||||
| 12. DAS–Acc | −0.23* | 0.19 | 0.16 | 0.08 | 0.01 | −0.08 | 0.12 | 0.16 | 0.45** | 0.34** | 0.45** | 0.46** | ||||
| Neurocognition | ||||||||||||||||
| 13. WMS-LM | −0.23 | 0.02 | 0.16 | 0.01 | 0.07 | 0.21 | 0.18 | 0.03 | 0.14 | 0.23 | 0.07 | 0.19 | 0.05 | |||
| 14. TMT-A | 0.25* | −0.18 | −0.12 | −0.15 | −0.19 | −0.18 | −0.13 | −0.12 | −0.10 | -0.13 | −0.15 | −0.07 | −0.05 | −0.29′ | ||
| 15. TMT-B | 0.19 | −0.05 | −0.19 | −04 | −0.25 | −0.21 | 0.12 | 0.19 | 0.13 | −0.19 | 0.02 | −0.12 | −0.14 | −0.28′ | 0.73** | |
| 16. TMT A-B | −0.03 | 0.01 | 0.18 | −0.11 | 0.22 | 0.17 | −0.13 | −0.20 | −0.24 | 0.11 | −0.15 | 0.03 | 0.07 | 0.19 | −0.33* | −0.89** |
Note: NEG, Negative Syndrome Factor assessed by the Positive and Negative Syndrome Scale; RSE, Rosenberg self-esteem scale; FSKN, Frankfurt Scales of Self-concept; FSKN-ST, assertiveness toward groups and significant others; FSKN-KU, contact and interpersonal abilities; FSKN-WA, self-estimation-by-others; DAS-Acc, Dysfunctional Attitudes Scale subscale to assess dysfunctional acceptance beliefs, WMS-LM, Wechsler Memory Scale, Subtest Logical Memory, TMT, Trail Making Test; TMT A-B, Difference Score between Part and Part B of the Trail Making Test. IPSAQ-SSB, Internal, Personal, Situational Attributions Questionnaires—self-serving bias; IPSAQ-ECB, Internal, Personal, Situational Attributions Questionnaires—external-causation-bias.
n = 53.
**P ≤ .01, *P ≤ .05.
As expected, the negative factor was also significantly correlated with processing speed (TMT-A). It was also associated with the BDI score (r = .30), indicating the need to control for the TMT-A score and depression in the further analyses. It was not, however, associated with the other TMT scores, the WMS or IQ.
For the regression model of social cognition on negative symptoms, we controlled for depression and the TMT-A score by entering them as predictors in step 1. In order to reduce multi-collinearity and retain an optimal ratio between the number of predictors and the number of participants, we restricted the number of variables entered in step 2 by selecting from within each category of social cognition the variable with the strongest association to negative symptoms: ToM emotions; empathy readiness, SSB, RSE self-esteem, and FSKN-KU. Due to the lower number of participants who completed the Empathy scale (n = 45), the regression model was based on a subgroup of 45 outpatients.
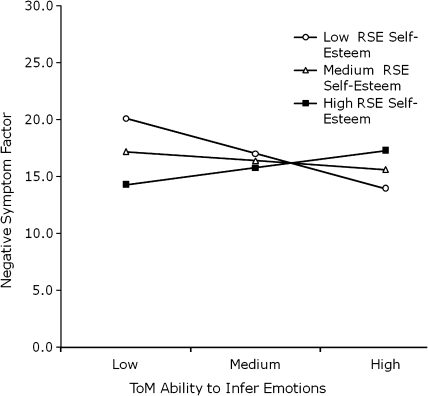
As can be seen in table 3, the TMT-A and BDI scores entered in step 1 explained a significant amount of variance (15%). The social cognition variables entered in step 2 led to a large and significant increase in the total explained variance to 41%. Based on the assumption that ToM and self-esteem will interact in predicting negative symptoms, the interaction term between ToM emotions and RSE was entered in step 3, which led to a further significant increase in total explained variance to 54%. Post hoc plotting was used to interpret the interaction term by equating simple slopes of the regression of ToM emotions on negative symptoms at the mean value of the RSE scale as well as 1 SD above and below. Thereby, we produced 3 regression slopes of ToM emotions on negative symptoms: one for persons with high self-esteem, one for persons in the medium range of the RSE scale, and one for persons with low self-esteem. The slope of each regression was then individually tested for significance.
Table 3.
Linear Regression Model of Negative Symptoms
| Predictors | Beta | P |
| Step 1 | ||
| TMT-A processing speed | .40 | .007 |
| BDI depression | .21 | .145 |
| Correlation R2=.15; F = 4.99; P = .011 | ||
| Step 2 | ||
| TMT-A processing speed | .27 | .036 |
| BDI depression | .22 | .211 |
| ToM emotions | −.23 | .150 |
| Empathy readiness | −.29 | .061 |
| IPSAQ self-serving bias | −.01 | .956 |
| RSE self-esteem | −.20 | .216 |
| FSKN-KU interpersonal self-concepts | −.07 | .599 |
| Correlation R2 =.41; change in R2 = .31; F = 5.28; significant change in F: P = .002 | ||
| Step 3 | ||
| TMT-A processing speed | .25 | .031 |
| BDI depression | .29 | .058 |
| ToM-emotions | −.13 | .370 |
| Empathy readiness | −.32 | .019 |
| IPSAQ self-serving bias | −.04 | .715 |
| RSE self-esteem | −.12 | .415 |
| FSKN-KU interpersonal self-concepts | −.29 | .047 |
| RSE × ToM emotions | .37 | .002 |
| Correlation R2 =.54; change in R2 = .12; F = 7.44; significant change in F: P = .002 | ||
Note: TMT, Trail Making Test; BDI, Beck Depression Inventory; ToM, Theory of Mind; IPSAQ, Internal, Personal, Situational Attributions Questionnaires; RSE, Rosenberg self-esteem scale; FSKN-KU, Frankfurt scales of self-concept, contact and interpersonal abilities; Beta = standardized β coefficients.
Figure 1 depicts the significant interaction between the ToM ability to infer emotions and the RSE in predicting negative symptoms. Difficulties in inferring emotions were associated with negative symptoms only in individuals with low self-esteem (slope = −2.13, t = −3.07, df = 41, P ≤ .01). The slope was nonsignificant in persons with medium levels of self-esteem (slope = −0.54, t = −0.92, df = 41) and in persons with high self-esteem (slope = 1.03, t = 1.24, df = 41).
Fig. 1.
Plot of the interaction between the Rosenberg self-esteem cale score and the ToM ability to infer emotions in predicting negative symptoms.
Discussion
Psychological explanations for the negative syndrome of psychosis have received little attention so far. This study therefore aimed to identify key domains of social cognition that are specifically relevant to negative symptoms.
In a large and heterogeneous sample of patients with regard to symptom severity, chronicity, and functioning, we found social cognitive variables not only to be significantly impaired in comparison to healthy controls but also to be directly associated with the severity of negative symptoms. Social cognition explained more than a third of the variance in negative symptoms over and above the impact of depression and neurocognition.
Once again, impairments in ToM proved to be linked to negative symptoms. It has been suggested to distinguish between cognitive perspective taking, inferring intentions, and affective ToM, with more overlap to the concept of empathy.45 We assessed both aspects of ToM finding the ability to infer emotions to be at least equally relevant to negative symptoms as the ability to infer intentions. Due to the cross-sectional nature of our study, we cannot draw conclusions with regard to causality. However, a recent study by Addington et al46 found impairments in facial affect recognition in a sample of persons at risk of psychosis which suggests that these difficulties precede the development of acute psychosis.
Empathy has been less frequently investigated in the context of psychosis. Although empathy was negatively associated with negative symptoms, over and above the impact of neurocognitive variables, we found no differences between patients and healthy control ratings of their empathetic skills. This is surprising as the samples differed in their abilities to infer emotions and seems to point to a discrepancy between self- and other estimated empathy as has been previously demonstrated by Bora and colleagues.47 Possibly, it is precisely this mismatch between the self- and other perception that leads to disappointing interpersonal experiences in which others do not respond as positively as expected.
The global perception of self as worthless, useless, and a failure (RSE) was also associated with negative symptoms. In accord with this, negative symptoms were inversely associated with the SSB and with the extent to which a person experiences themselves as skilled, relaxed, and confident in communicating with others (FSKN-KU) and respected, trusted, loved, and accepted by relevant others. The latter points to disturbances in close relationships and perceived social rank and fits in well with findings from Barrowclough and colleagues27 showing that the degree of perceived critical comments from family members predicted the presence and severity of negative symptoms. These associations are intuitive, as someone who has a low opinion of his or her interpersonal abilities and does not feel respected by others is not likely to expect social encounters to be successful and will be less motivated to engage in them. Dysfunctional acceptance beliefs, such as linking self-worth to the love and respect from others, are likely to further lower the threshold for disappointment by raising the standards for success. However, although it seems compelling to assume that negative self-concepts precede symptom formation, it is also possible that they arise as a consequence of psychosis. For example, patients' negative self-concepts with regard to social abilities might reflect that negative symptoms are not only acknowledged but also have began to seep into the concepts that the patients have of themselves. Furthermore, being labeled as “a schizophrenic” is likely to lead to loss of positive social feedback48 and enhance negative interpersonal self-concepts. In support of this, Birchwood et al49 found that social anxiety in schizophrenia was triggered by the anticipation of loss of social status. On the other hand, studies in ultrahigh-risk populations indicate that dysfunctional beliefs50 are already detectable before the beginning of an acute episode, which seems to imply a causal role in delusion formation. Most likely though both causal directions are relevant in a gradual process with negative self-concepts feeding into social avoidance and lack of positive social interactions reinforcing negative self-concepts.
The self-concept of being an assertive person (FSKN-ST) was not related to negative symptoms, suggesting that not all interpersonal self-concepts are relevant to negative symptoms. Also, and in contrast to Bentall et al26 who found low self-efficacy in patients with negative symptoms, we did not find a lack of perceived self-causation to be associated with negative symptoms. However, this may have been due to the different operationalizations of the construct.
Most interestingly, we found the ability to infer emotions to be only significantly associated with negative symptoms in persons with low self-esteem. This is intuitive because difficulties in ToM alone cannot convincingly explain why people withdraw socially. However, persons with ToM difficulties and a low opinion of themselves are going to be prone to negatively biased interpretations and therefore more likely to withdraw, which is likely to further stabilize negative self-concepts and negative symptoms. A noteworthy study by Bell et al20 also demonstrates that the interactions between skill-related deficits and self-conceptions are possibly more helpful to understanding symptoms than each potential predictor alone. They found effects of neurocognition on rehabilitation outcome to be mediated by social cognition and social discomfort, which suggests that poorer social cognition leads to social discomfort on the job which in turn leads to poorer rehabilitation outcomes.
Our findings feed into and advance the cognitive formulation of negative symptoms put forward by Rector et al14 who have suggested that low expectancies for pleasure, success and acceptance, and the perception of limited resources play a major role in the formation of negative symptoms. Subsequent work by this group and others has not only demonstrated the presence of dysfunctional performance beliefs (eg, If I fail partly, it is as bad as being a complete failure) to be associated with negative symptoms.51 Based on their assumption that specific attitudes and beliefs mediate the effect of impairment and behavior, Beck and colleagues19 have been accumulating evidence that points to indirect pathways from functional capacity over dysfunctional performance beliefs to negative symptoms. Hopefully, future research will further illuminate how the various aspects of social cognition, neurocognition, and other reasoning biases52 and their interactions impact on negative symptoms.
Some limitations need noting that might affect the generalizability of the findings. As it was, the assessments were lengthy and taxing for many patients. Therefore, priorities had to be set. Due to the focus on social cognition, rather than neurocognition, we only conducted a short screening of neurocognitive impairment. Possibly, neurocognition would have shown a stronger impact if we had used a larger neuro-psychological test-battery. Furthermore, for organizational reasons, part of the sample did not complete the empathy scale or the WMS so that some analyses are based on subsamples. We attempted to obtain a broad spectrum of severity by including inpatients and outpatients. This was an advantage in terms of the correlation analyses. However, in the light of findings showing ToM deficits to decrease with remission,53 the recruitment of patients from inpatients and outpatient settings raises the question of whether the outpatients might be accounting for the findings. On the other hand, this possibility could be disregarded because the correlations remained essentially the same when conducted for both samples and the regression analyses were based on the outpatient sample only. Despite the inclusion of inpatients, in regard to the severity of symptoms and functioning, the sample was not representative of patients with severe negative symptoms and the results cannot automatically be generalized to these patients. The PANSS positive, negative, and general scores were, however, comparable to those found in RCTs testing the effectiveness of CBT for psychosis eg,.54–56 Similarly, age, gender distribution, and length of disorder were comparable to those found in CBT intervention studies.57 Education data are difficult to compare across nations and—as Marburg is a typical university town—the sample could have been slightly biased towards those with higher education.
Taken together, the sample can be considered representative of samples of the help-seeking patients included in intervention studies testing the effect of CBT for psychosis.3,57 Therefore, the data obtained in this sample provide a helpful basis for developing interventions for these patients.
Conclusions
At times, it almost seems as if researchers and clinicians likewise have given up on negative symptoms. This might not only be due to discouraging effects in intervention studies but may also lie in the nature of the symptoms themselves. Patients in which they prevail are less active in seeking help and do not cause commotions that lead others to act on their behalf. Also, their suffering, although present, is often concealed due to the difficulties in expressing feelings, which impacts on the therapist-perceived alliance.58 Therefore, it is extremely important to improve the understanding of the processes involved in negative symptoms. The results of this study highlight the relevance of self-concepts related to social abilities, dysfunctional expectations, and global self-worth alone and in interaction with skill-related areas of impairment for negative symptoms and thereby provide a helpful basis for the further development of psychological therapy for patients with negative symptoms.
Funding
This work was supported by a grant to T.M.L. from the Deutsche Forschungsgemeinschaft (Li1298/3-1).
Acknowledgments
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1.Mäkinen J, Miettuden J, Isohanni M, Koponen H. Negative symptoms in schizophrenia. A review. Nord J Psychiatry. 2008;62:334–341. doi: 10.1080/08039480801959307. [DOI] [PubMed] [Google Scholar]
- 2.Kirkpatrick B, Fenton WS, Carpenter WT, Marder SR. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull. 2006;32:214–219. doi: 10.1093/schbul/sbj053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull. 2008;34:523–537. doi: 10.1093/schbul/sbm114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klingberg S, Wittorf A, Herrlich J, Wiedemann G, Buchkremer G, Wölwer W. Mainz, Germany. 2010: Kognitive Verhaltenstherapie bei Negativsymptomatik schizophrener Störungen—Ergebnisse zur Wirksamkeit in einer multizentrischen klinischen Studie. 28. Symposium der Fachgruppe für Klinische Psychologie und Psychotherapie der deutschen Gesellschaft für Psychologie. [Google Scholar]
- 5.Kirkpatrick B. Editor's introduction: theme issue on negative symptoms. Schizophr Bull. 2006;32:212–213. [Google Scholar]
- 6.Lewander T. Neuroleptics and the neuroleptic-induced deficit syndrome. Acta Psychiatr Scand. 1994;380:8–13. doi: 10.1111/j.1600-0447.1994.tb05825.x. [DOI] [PubMed] [Google Scholar]
- 7.Harrow M, Yonan CA, Sands JR, Marengo J. Depression in schizophrenia: are neuroleptics, akinesia or anhedonia involved? Schizophr Bull. 1994;20:327–338. doi: 10.1093/schbul/20.2.327. [DOI] [PubMed] [Google Scholar]
- 8.Tarrier N. Negative symptoms in schizophrenia: comments from a clinical psychology perspective. Schizophr Bull. 2006;32:231–233. doi: 10.1093/schbul/sbj051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garety P, Freeman D. Cognitive approaches to delusions: a critical review of theories and evidence. Br J Clin Psychol. 1999;38:113–154. doi: 10.1348/014466599162700. [DOI] [PubMed] [Google Scholar]
- 10.Bentall RP, Corcoran R, Howard R, Blackwood N, Kinderman P. Persecutory delusions: a review and theoretical integration. Clin Psychol Rev. 2001;21:1143–1192. doi: 10.1016/s0272-7358(01)00106-4. [DOI] [PubMed] [Google Scholar]
- 11.Lincoln TM, Mehl S, Ziegler M, Kesting M-L, Exner C, Rief W. Is fear of others linked to an uncertain sense of self. The relevance of self-worth, interpersonal self-concepts and dysfunctional beliefs to paranoia. Behav Ther. 2010;41:187–197. doi: 10.1016/j.beth.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 12.Kuipers E, Garety P, Fowler D, Freeman D, Dunn G, Bebbington P. Cognitive, emotional, and social processes in psychosis: refining cognitive behavioral therapy for persistent positive symptoms. Schizophr Bull. 2006;32:24–31. doi: 10.1093/schbul/sbl014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moritz S, Woodward TS. Metacognitive training in schizophrenia: from basic research to knowledge translation and intervention. Curr Opin Psychiatry. 2007;20:619–625. doi: 10.1097/YCO.0b013e3282f0b8ed. [DOI] [PubMed] [Google Scholar]
- 14.Rector NA, Beck AT, Stolar N. The negative symptoms of schizophrenia: a cognitive perspective. Can J Psychiatry. 2005;50:247–257. doi: 10.1177/070674370505000503. [DOI] [PubMed] [Google Scholar]
- 15.Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr Res. 2009;113:189–199. doi: 10.1016/j.schres.2009.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roder V, Mueller D, Mueser KT, Brenner HD. Integrated psychological therapy (IPT) for schizophrenia: is it effective? Schizophr Bull. 2006;32:81–93. doi: 10.1093/schbul/sbl021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McGurk S, Twamley EW, Sitzer DI, McHugi GJ, Mueser KT. A meta-Analysis of cognitive remediation in schizophrenia. Am J Psychiatry. 2007;164:1791–1802. doi: 10.1176/appi.ajp.2007.07060906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Green MF, Penn DL, Bentall R, et al. Social cognition in schizophrenia: an NIMH workshop on definitions, assessment, and research opportunities. Schizophr Bull. 2008;34:1211–1220. doi: 10.1093/schbul/sbm145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beck AT, Rector NA, Stolar N, Grant PM. Schizophrenia. Cognitive Theory, Research and Therapy. New York, NY: Guilford Press; 2009. [Google Scholar]
- 20.Bell M, Tsang HWH, Greig TC, Bryson GJ. Neurocognition, social cognition, perceived social discomfort, and vocational outcomes in schizophrenia. Schizophr Bull. 2009;35:738–747. doi: 10.1093/schbul/sbm169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McGlade N, Behan C, Hayden J, et al. Mental state decoding v. mental state reasoning as a mediator between cognitive and social function in psychosis. Br J Psychiatry. 2008;193:77–78. doi: 10.1192/bjp.bp.107.044198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grant PM, Beck AT. Defeatist beliefs as a mediator of cognitive impairment, negative symptoms, and functioning in schizophrenia. Schizophr Bull. 2009;35:798. doi: 10.1093/schbul/sbn008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horan WP, Rassovsky Y, Kern RS, Lee J, Wynn JK, Green MF. Further support for the role of dysfunctional attitudes in models of real-world functioning in schizophrenia. J Psychiatr Res. 2010;44:499–505. doi: 10.1016/j.jpsychires.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sprong M, Schothorst P, Vos E, Hox J, van Engeland H. Theory of mind in schizophrenia: meta-analysis. Br J Psychiatry. 2007;191:5–13. doi: 10.1192/bjp.bp.107.035899. [DOI] [PubMed] [Google Scholar]
- 25.Shamay-Tsoory SG, Shur S, Harari H, Levkovitz Y. Neurocognitive basis of impaired empathy in schizophrenia. Neuropsychology. 2007;21:431–438. doi: 10.1037/0894-4105.21.4.431. [DOI] [PubMed] [Google Scholar]
- 26.Bentall RP, Simpson PW, Lee DA, et al. Motivation and avolition in schizophrenia patients: the role of self-efficacy. Psychosis Psychol Soc Integr Approach. 2010;2:12–22. [Google Scholar]
- 27.Barrowclough C, Tarrier N, Humphreys L, Ward J, Gregg L, Andrews B. Self-esteem in schizophrenia: relationships between self-evaluation, family attitudes, and symptomatology. J Abnorm Psychol. 2003;112:92–99. [PubMed] [Google Scholar]
- 28.Grant PM, Beck AT. Asocial beliefs as predictors of asocial behavior in schizophrenia. Psychiatry Res. 2010;177:65–70. doi: 10.1016/j.psychres.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 29.Wittchen HU, Zaudig M, Fydrich T. Strukturiertes Klinisches Interview fuer DSM-IV. Goettingen, Germany: Hogrefe; 1997. [Google Scholar]
- 30.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 31.van der Gaag M, Hoffman T, Remijsen M, et al. The five-factor model of the positive and negative syndrome scale II: a ten-fold cross-validation of a revised model. Schizophr Res. 2006;85:280–287. doi: 10.1016/j.schres.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 32.Hautzinger M, Bailer M, Worall H, Keller F. Beck-Depressions-Inventar (BDI) Bern, Switzerland: Huber; 1995. [Google Scholar]
- 33.Mehl S, Rief W, Mink K, Lüllmann E, Lincoln TM. Social performance is more closely associated with Theory of Mind and autobiographical memory than with psychopathological symptoms in clinically stable patients with schizophrenia spectrum disorders. Psychiatry Res. 2010;178:276–283. doi: 10.1016/j.psychres.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 34.Leibetseder M, Laireiter A-R, Riepler A, Köller T. E-Skala: fragebogen zur Erfassung von Empathie - Beschreibung und psychometrische Eigenschaften. Zeitschrift für Differentielle und Diagnostische Psychologie. 2001;22:70–85. [Google Scholar]
- 35.Kinderman P, Bentall RP. A new measure of causal locus. The internal, personal and situational attributions questionnaire. Pers Individ Dif. 1996;20:261–264. [Google Scholar]
- 36.von Collani G, Herzberg PY. Eine revidierte Fassung der deutschsprachigen Skala zum Selbstwertgefühl nach Rosenberg. Zeitschrift für Differentielle und Diagnostische Psychologie. 2003;24:3–7. [Google Scholar]
- 37.Bosson JK, Swann WB, Pennebaker JW. Stalking the perfect measure of implicit self-esteem: the blind men and the elephant revisited? J Pers Soc Psychol. 2000;79:631–643. [PubMed] [Google Scholar]
- 38.Deusinger IM. Die Frankfurter Selbstkonzeptskalen. Göttingen, Germany: Hogrefe; 1986. [Google Scholar]
- 39.Bergemann N, Scheurer H. Altstötter-Gleich. Retest-Reliabilität und faktorenanalytische Dimensionalität der FSKN [Retest Reliability and Factor Dimensions of the Frankfurt Self-Concept Scales (FSKN)] Zeitschrift für Differentielle und Diagnostische Psychologie. 2002;23:367–380. [Google Scholar]
- 40.Hautzinger M, Luka U, Trautmann RD. Skala dysfunktionaler Einstellungen—Eine deutsche Version der Dysfunctional Attitude Scale. Diagnostica. 1985;31:312–323. [Google Scholar]
- 41.Wechsler D. Wechsler Adult Intelligence Test—Revised. New York, NY: Psychological Corporation; 1981. [Google Scholar]
- 42.Härting C, Markowitsch HJ, Neufeld H, Calabrese P, Deisinger K, Kessler J. Wechsler Gedächtnistest—Revidierte Fassung (WMS-R) Bern, Switzerland: Verlag Hans Huber; 2000. [Google Scholar]
- 43.Reitan RM. Trail Making Test. Manual for Administration and Scoring. South Tucson, AZ: Reitan Neuropsychology Laboratory; 1992. [Google Scholar]
- 44.Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. London, UK: Sage; 1991. [Google Scholar]
- 45.Koelkebeck M, Abdel-Hamid M, Ohrmann P, Brühne M. Theory of Mind bei Schizophrenien. Klinische und wissenschaftliche Aspekte. Fortschritte in Neurologie und Psychiatrie. 2008;76:573–582. doi: 10.1055/s-2008-1038250. [DOI] [PubMed] [Google Scholar]
- 46.Addington J, Penn D, Woods SW, Addington D, Perkins DO. Facial affect recognition in individuals at clinical high risk for psychosis. Br J Psychiatry. 2008;192:67–68. doi: 10.1192/bjp.bp.107.039784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bora E, Gökçen S, Veznedaroglu B. Empathic abilities in people with schizophrenia. Psychiatry Res. 2008;160:23–29. doi: 10.1016/j.psychres.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 48.Angermeyer MC, Dietrich S. Public beliefs about and attitudes towards people with mental illness: a review of population studies. Acta Psychiatr Scand. 2006;113:163–179. doi: 10.1111/j.1600-0447.2005.00699.x. [DOI] [PubMed] [Google Scholar]
- 49.Birchwood M, Trower P, Brunet K, Gilbert P, Iqbal Z, Jackson C. Social anxiety and the shame of psychosis. A study in first episode psychosis. Behav Ther Res. 2006;45:1026–1037. doi: 10.1016/j.brat.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 50.Perivoliotis D, Morrison AP, Grant PM, Beck AT. Negative performance beliefs and negative symptoms in individuals at ultra-high risk of psychosis: a preliminary study. Psychopathology. 2009;42:375–379. doi: 10.1159/000236909. [DOI] [PubMed] [Google Scholar]
- 51.Rector NA. Dysfunctional attitudes and symptom expression in schizophrenia: differential associations with paranoid delusions and negative symptoms. J Cogn Psychother. 2004;18:163–173. [Google Scholar]
- 52.Lincoln TM, Ziegler M, Mehl S, Rief W. The Jumping to Conclusions Bias in delusions: specificity and changeability. J Abnorm Psychol. 2010;199:40–49. doi: 10.1037/a0018118. [DOI] [PubMed] [Google Scholar]
- 53.Bora E, Yucel M, Pantelis C. Theory of mind impairment in schizophrenia: meta-analysis. Schizophr Res. 2009;109:1–9. doi: 10.1016/j.schres.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 54.Bechdolf A, Knost B, Kuntermann C, et al. A randomized comparison of group cognitive-behavioural therapy and group psychoeducation in patients with schizophrenia. Acta Psychiatr Scand. 2004;110:21–28. doi: 10.1111/j.1600-0447.2004.00300.x. [DOI] [PubMed] [Google Scholar]
- 55.Rector NA, Seeman MV, Segal Z. Cognitive therapy for schizophrenia: a preliminary randomised trial. Schizophr Res. 2003;63:1–11. doi: 10.1016/s0920-9964(02)00308-0. [DOI] [PubMed] [Google Scholar]
- 56.Valmaggia LR, Van der Gaag M, Tarrier N, Pijnenborg M, Sloof CJ. Cognitive-behavioural therapy for refractory psychotic symptoms of schizophrenia resistant to atypical medication. Br J Psychiatry. 2005;186:324–330. doi: 10.1192/bjp.186.4.324. [DOI] [PubMed] [Google Scholar]
- 57.Lincoln TM, Suttner C, Nestoriuc Y. Wirksamkeit kognitiver Interventionen in der Reduktion schizophrener Symptomatik. Eine Meta-Analyse. Psychol Rundsch. 2008;4:217–232. [Google Scholar]
- 58.Wittorf A, Jakobi U, Bechdolf A, et al. The influence of baseline symptoms and insight on the therapeutic alliance early in the treatment of schizophrenia. Eur Psychiatry. 2009;24:259–267. doi: 10.1016/j.eurpsy.2008.12.015. [DOI] [PubMed] [Google Scholar]