Abstract
Personalization of treatment is a current strategic goal for improving health care. Integrated treatment approaches such as psychiatric rehabilitation benefit from personalization because they involve matching diverse arrays of treatment options to individually unique profiles of need. The need for personalization is evident in the heterogeneity of people with severe mental illness and in the findings of experimental psychopathology. One pathway to personalization lies in analysis of the judgments and decision making of human experts and other participants as they respond to complex circumstances in pursuit of treatment and rehabilitation goals. Such analysis is aided by computer simulation of human decision making, which in turn informs development of computerized clinical decision support systems. This inspires a research program involving concurrent development of databases, domain ontology, and problem-solving algorithms, toward the goal of personalizing psychiatric rehabilitation through human collaboration with intelligent cyber systems. The immediate hurdle is to demonstrate that clinical decisions beyond diagnosis really do affect outcome. This can be done by supporting the hypothesis that a human treatment team with access to a reasonably comprehensive clinical database that tracks patient status and treatment response over time achieves better outcome than a treatment team without such access, in a controlled experimental trial. Provided the hypothesis can be supported, the near future will see prototype systems that can construct an integrated assessment, formulation, and rehabilitation plan from clinical assessment data and contextual information. This will lead to advanced systems that collaborate with human decision makers to personalize psychiatric rehabilitation and optimize outcome.
Keywords: ontology, rehabilitation, decision support
Two transcending realities emerge from contemporary schizophrenia research:
People with schizophrenia are quite heterogeneous with respect to strengths, disabilities, course of their illness, and the nature of their recovery.
Our array of treatment and rehabilitation methods and tools has become broad and diverse, including biological, cognitive, behavioral, and socioenvironmental approaches.
There are 2 simple but very important implications for treatment to achieve maximum effectiveness:
It must be broad enough and flexible enough to allow tailoring to individual patient needs.
It must be integrated in a comprehensive treatment array, delivered as part of a personalized rehabilitation regimen.
The US National Institute of Mental Health has put a strategic priority on research to enhance personalization of treatment.1 However, it can be surprisingly difficult to make the leap from our conventional research questions, which generally address “average” treatment effects in the “typical” patient, to questions of what treatment is best for which person, at what time. The difficulty is surprising because as clinical practitioners we take for granted that we and our patients make judgments and decisions throughout the course of treatment, based on the patient’s individual characteristics among other factors, but our research methods usually neutralize those individual considerations so that we can make inferences about specific treatments. From these methods, we learn how different treatments compare with respect to groups defined by our grouping variables but we learn little or nothing about how to personalize treatment within those groups.
The idea of personalization resonates with broader principles of evidence-based practice, but a commitment to evidence-based practice alone does not guarantee optimal personalization. Ultimately, a practice must be evidence based for a specific problem. The proliferation of treatment options reflects in part proliferation of treatment targets, diverging from symptoms to cognitive impairments, instrumental behaviors, skill deficits, social roles, and possibly in the near future biological processes. After a treatment becomes evidence based, it remains for the practitioner to identify the features of a particular patient’s presentation for which possible treatments are effective. In psychiatry, these targets are seldom if ever identified by diagnosis alone. Trial-and-error is arguably the most common method of selecting specific evidence-based treatments for specific patients. There is no question that systematic empirical trial-and-error (or more precisely, trial-and-assess outcome) is crucial in psychiatry. Personalization is advanced when science provides information that maximizes the probability of selecting treatments that will prove effective on the first trial.
One pathway toward personalization, reflected in current excitement about early intervention and first-episode approaches2,3 is to identify more homogeneous subgroups with high potential for responding to a specific, specially selected treatment array. Medication algorithms4 could represent another path to personalization, although so far medication algorithms have focused more on reducing costs and heterogeneity among practitioners than on matching individual characteristics with treatment options. Genome-based treatment selection5,6 may be another pathway, although so far it is more promise than reality.
There is yet another pathway to personalization, based on the deceptively simple idea that practitioners and patients do make individualized judgments and decisions. This is not such a platitude, as it may seem. We really do not understand very much about how practitioners make their decisions, especially in the clinical frontier of treating schizophrenia and related disorders. Our attempts at formalizing even seemingly straightforward decisions, for example in medication algorithms, have yielded disappointing results. There are reasons for this. Most generally, we know from the experimental psychology of judgment and decision making7 (JDM) that experts cannot always describe or articulate the rules and algorithms by which they operate. In mental health practice, even simple decisions are usually made in very complex contexts. In patients with multiple conditions or problems, as is the case with severe and disabling mental illness, even if a definable patient group is homogeneous in response to a specific treatment, it will be heterogeneous with respect to other treatments for other problems. As treatment options multiply, the complexity of personalization increases. Nevertheless, it is credible to presume that practitioners personalize treatment by making case-specific judgments and decisions, beyond initial grouping judgments (eg, making a psychiatric diagnosis). If we did not think so, we would not invest so heavily in their training, education, and regulation.
Conceptualizing personalization of treatment in terms of clinical JDM leads logically to a research and development agenda. If we could more fully understand the judgments and decisions involved in navigating the course of chronic, severe psychiatric conditions toward recovery, we could better educate and train practitioners to collect the needed information and make the best judgments and decisions. A more systematic accounting of clinical judgments and decisions, and the data on which they are based, would also enable better use of computer technology to support those decisions, as has been the case in other areas of health care.8–10
The research and development agenda can be validated by testing a simple hypothesis:
H1: A practitioner or treatment team continuously exercising JDM in response to data on patients’ status and treatment response, using systematic trial-and-assessment and selecting from an evidenced-based treatment array, produces better outcome than one guided only by group inclusion criteria (eg, diagnosis), unsystematic trials, and environmental exigencies (eg, institutional policy, availability of specific treatments).
However, the null hypothesis is neither trivial nor counterintuitive:
H0: It makes no difference—
most treatment effects are more generalized than specific;
more treatment is simply better;
a shot gun is still more cost-effective than a magic bullet.
So, in embarking on the JDM pathway to personalization, we have reason to seek some reassurance about it is potential. Do we really have reason to suspect that recovery in severe mental illness generates circumstances where personalized JDM would make a difference? Reassurance comes from 2 domains: (1) the nature of the severely mentally ill population, especially its heterogeneity and (2) findings of experimental psychopathology.
The Heterogeneity of the Population
Table 1 shows a list of characteristics of the broad population of people under the rubric of “severe and disabling mental illness” (hereafter, the term Serious Mental Illness or SMI will be used to denote this population). These characteristics, and presumably many more yet to be identified, produce an extremely heterogeneous population, even within diagnostic groups. There is no profile or combination of these problems that is unique or even “typical.” No combination or pattern is peculiar to SMI or even to schizophrenia. Since the disorder continues over the life span, the patient population includes people of all ages and developmental stages. Individual patients have unique combinations of multiple problems. Logically, multiple problems require multiple treatments, each treatment having its own considerations for tailoring to individual needs. Coordination and integration of multiple treatments logically requires simultaneous consideration of many factors, on a case-by-case basis.
Table 1.
Characteristics of “Severe and Disabling Mental Illness”
| • Schizophrenia spectrum diagnoses, often multiple diagnoses |
| Episodic psychosis, highly variable in severity, length, symptoms |
| • Neurocognitive deficits of variable type and severity |
| Frontal/executive and memory deficits of variable severity |
| Deficits in automatic (“gistful”) social cognition of variable severity |
| Emotional recognition deficits in some individuals |
| Theory of Mind deficits in some individuals |
| Context apprehension deficits of variable severity |
| • Adolescent or pre-adolescent onset in many individuals, with diverse developmental implications |
| Adolescent or preadolescent levels of moral cognition and social judgment in some individuals |
| Social/interpersonal skill deficits of variable severity |
| Independent living skill deficits of variable severity |
| • Multi-comorbidity in all possible combinations: |
| Substance abuse |
| Emotion dysregulation disorders (borderline syndrome) |
| Anxiety disorders |
| Depression |
| • Various personality disorder traits in all possible combinations |
There is growing consensus that integrated biopsychosocial models of schizophrenia and other severe mental illnesses are key to understanding its complex psychopathology and hence its treatment.11 We increasingly have the technology to target and treat impairments at all these various levels. Even in more homogeneous patient populations, integration of treatment across levels of human functioning is a major challenge. With heterogeneity, the difficulties increase exponentially.
The logical implications of patient heterogeneity for a JDM pathway to personalization are partially supported by empirical findings. Outcome research generally links the effectiveness of specific treatments to specific problems (eg, symptoms, cognitive impairments, skill deficits, family interactions), not diagnostic groups. However, it is notoriously more difficult to determine a treatment’s specificity than its effectiveness for any particular problem or outcome measure. There is thus still rational room for the skeptical view that until proven otherwise, there is not enough specificity of treatment effects in psychiatric rehabilitation to make personalization beneficial. Nevertheless, skepticism is inconsistent with what seems obvious to experienced practitioners that we continuously make important judgments and decisions, and not just about medication, based on patients’ unique characteristics and circumstances.
Experimental Psychopathology
The JDM pathway to personalization also draws upon the experimental psychopathology of schizophrenia, which tells us much about interactions between neurophysiological, cognitive, and behavioral processes over the course of the disorder. Whenever we identify a link between a measurable process and a measurable dimension of personal or social functioning, we identify a potential point at which a judgment or decision might helpfully be made. When there are individual differences among those processes and dimensions, we have taken a step toward personalization.
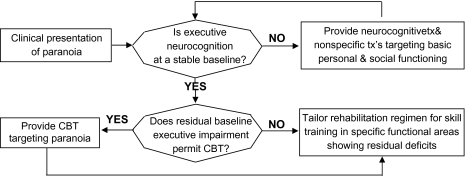
Here is an example of how psychopathology research can lead to JDM implications. A body of findings suggests that the clinical presentation of paranoia is mediated by neurocognitive and social cognitive factors,12 as cognitive and behavioral recovery progresses.13–16 Taken together, the findings collectively reveal sequential relationships relevant to treatment. Inferring from the sequences and time frames in the findings, a plausible narrative interpretation can be constructed as follows:
When paranoia is accompanied by deficits in executive cognitive functioning at the start of rehabilitation, improvement in executive cognition brings reduction of paranoia in some individuals (consistent with the familiar observation that paranoia can result from various kinds of generalized brain dysfunction). Neuropsychological assessment can determine whether there is executive impairment at the start of rehabilitation. If so, resources can be deployed primarily to address it, with the expectation of specific treatment effects from some modalities (eg, neurocognitive remediation,17,18) and nonspecific effects of others (eg, adhering to a daily routine, participating in low-demand social activities.19) Repeated assessments can confirm whether the executive impairments are responsive to treatment, within 30 to 60 days. If so, the focus of treatment on neurocognition should continue with a gradual increase in more demanding modalities that enhance cognitive recovery through nonspecific effects as well as specific effects on other areas requiring functional improvement (eg, replace low-demand social activities with social skills training). The combined effects of this regimen are expected to produce a recovery trajectory in personal and social behavioral functioning continuing at least 6 months before reaching baseline.
Repeated assessment can also indicate the degree of paranoia residual to neurocognitive recovery. The residual paranoia is associated with attributional processes, as opposed to executive impairments, and is a suitable target for specialized cognitive behavioral therapy (CBT) that directly addresses attributions and beliefs.20
When repeated assessment indicates executive functioning is near baseline (no improvement with intensive treatment over 30–60 days), expectations for further treatment response must be adjusted according to the severity of the residual deficit. Severe residual executive deficits compromise response to CBT and skill training. With or without paranoia, the environmental support required for severe residual executive deficits will be greater (executive deficits impair performance of many routine skills), and the living and occupational skill acquisition goals must be adjusted accordingly.
These interpretations can be summarized in a simple decision algorithm, shown in figure 1 in the form of a cybernetic information-processing diagram.
Fig. 1.
The course of paranoia as an information-processing algorithm
This is arguably an unusual use of psychopathology, where findings are usually meant to clarify the role of specific biological, psychological, and social processes in the etiology of disorders. The purpose of this example is to show that reasonable interpretations of research data can also lead to testable algorithms for clinical decision making. In this example, the algorithm logically could enhance outcome by identifying opportunities for exploiting spontaneous recovery, directing the sequence of specific interventions, preventing use of expensive options having low probability of benefit, and informing long-term treatment goals.
The example also shows that using even a simple algorithm may require a considerable amount of longitudinal data collection and processing, not only just for validation but also for routine clinical application. A set of algorithms comprehensive enough to even approach the scope of clinical issues involved in psychiatric rehabilitation would require exponentially more data processing. At this point, the JDM path to personalization encounters a key signpost: “Computer technology and the cybernetic sciences, collectively known as informatics, will play a crucial role in further progress.”
Clinical Decision Support Systems
Informatics plays a key role in personalization for 2 main reasons. First, the volume of data involved in JDM in psychiatric treatment and rehabilitation is so great that its management in clinical settings may only be possible through computerization. This is no surprise to computer scientists, who have seen similar realizations in many other areas of health care (if there is any surprise, it is that mental health technology can now generate such a volume of data). The second reason is that beyond passive management of clinical data for human consumption, computers can be helpful by participating in JDM. This in turn happens in 2 ways: (1) with computer modeling, we can better understand human JDM and (2) computers can complement human JDM by using their special nonhuman abilities.
The explosion of informatics in other areas of health care provides a vision of how similar developments in mental health could support personalization of treatment.21 Treatment and rehabilitation could be organized around a clinical decision support system (CDSS) in which humans and computers collaborate, contributing their respective abilities, to optimize decision making, and thus to optimize treatment outcome. This vision illuminates in turn the kind of technological and scientific work that lies ahead.
In the real world, humans engaged in clinical decision making use a large number of implicit algorithms, “fast and frugal heuristics,” and other probabilistic determinations.22 Formal representation and systematic use of all of them in a computer system requires not only extraordinary data management but also advanced software engineering technology. For a CDSS to truly participate in treatment personalization, as opposed to passive support of human judgments, comprehensive sets of elemental decision algorithms must be derived from research findings and clinical experience, integrated into the context of real world clinical practice, and coded in computer programs.23 For these reasons, development of computerized systems to support personalization in psychiatric rehabilitation requires extended, intensive, systematic interdisciplinary collaboration of experienced clinicians, rehabilitation researchers, computer scientists, engineers, and others.23
We do not have to envision a computer producing better treatment outcomes than humans. It would be enough for a human treatment team with a cyber member to produce better outcomes than a human treatment team without one. Along the way, the process of developing and improving intelligent and interactive CDDSs will teach us much about human JDM. This will in turn inform human training and education and will further improve computer emulation of human abilities.23 In this sense, advancing our understanding of human JDM and developing intelligent CDSSs proceed as 2 steps in a cyclic iterative process.
Evolution of CDSSs for Personalization of Psychiatric Treatment and Rehabilitation
We can foresee a stage-wise sequence by which increasingly intelligent CDSSs achieve the ability to participate collaboratively in clinical JDM:
“Stage I” is familiar to many who conduct research in clinical settings—systematic collection and management of clinical data pertinent to a particular research question or treatment outcome. Sophisticated multivariate analyses of the databases created by such systems have already identified numerous relationships between parameters of treatment and recovery that could represent key decision-making opportunities.14,15,24–27 However, such databases are typically designed and built to answer a narrow range of research questions, and the variables are selected accordingly. A stage I CDSS that includes the variables pertinent to assessing individual people, formulating their treatment plan, and tracking their progress in recoveryhas different design requirements.
“Stage II” includes a new set of variables, reflecting human judgments and decisions. “Medication prescriptions,” for example, reflect not only a particular treatment but also a JDM process that led to the prescription. Medication algorithms exploit that process. In rehabilitation, a “treatment plan” more comprehensively reflects multi-modal treatment selections and related decisions. “Dispositional events” such as legal determinations of competence, civil commitment, guardian directives, and transfer of patients between service settings also reflect human JDM. Inclusion of judgment and decision variables in the database greatly enhances our ability to retrospectively identify patient and context factors that influence human decisions. This informs how we choose variables for a more advanced CDSS.
In “stage III,” the data management system actually functions to support clinical decision making, by compiling data generated in the course of treatment and returning it to human decision makers in easily interpretable formats, in the time frame in which decisions must be made. However, the actual JDM remains exclusively human.
Commercially, available electronic medical records systems (EMRs) used in many health care settings include some decision information such as diagnosis (arguably a human judgment based on raw data about the patient) and physicians’ orders. Some EMRs manage raw clinical data as well, for example laboratory tests. In that sense, they are stage II systems. Some EMRs support some clinical activities in real time (mostly record keeping, not decision making) and in that sense have stage III capabilities. However, in mental health settings, much of the clinical data in an EMR is embedded in narrative reports, eg, social histories, evaluation reports, progress notes, etc. As a result, the data are not easily accessible for computer processing and real time decision making (sophisticated language-analytic software can analyze such data off line for research purposes, but processing sufficient for real time decision support lies in the future). On the other hand, EMRs usually include treatment plans and related documents required by practice standards and regulations. EMRs could evolve into stage III CDSSs by combining their prescription and treatment plan documenting capabilities with quantitative databases that increasingly include variables pertinent to psychiatric rehabilitation.
There are a few prototypal examples of stage III systems for psychiatric rehabilitation, each with its own limitations in scope and applicability. A system developed by Paul et al28–30 is built around a comprehensive treatment approach derived from social learning theory. It supports a token economy and an array of other psychosocial treatment modalities, it tracks behavioral functioning over time with an impressive level of precision, and it formats the data for human decision making in a clinical time frame. However, it has limited capacity to support personalized treatment, especially in the biological, cognitive, and socioenvironmental domains, and most decisions are driven by the treatment model, not case-wise data. A system developed by Young et al31 takes advantage of network capabilities and supports personalized treatment but is focused on drug treatment. A system developed by Spaulding et al32 supports personalization and encompasses the broad scope of treatment modalities in psychiatric rehabilitation, but like the Paul et al system, it was designed for a select subpopulation (extremely disabled patients in long-term inpatient or residential settings) pursuing a narrower range of recovery goals than the broader SMI population (ie, goals most immediately relevant to moving to less restrictive settings). None of these prototypes is capable of testing the key hypothesis.
In “stage IV,” the system actively participates in decision making. It uses algorithms to identify patterns in the data that may not be apparent or accessible to a human. It uses other algorithms that emulate human clinical judgment. It formulates hypotheses about possible treatment response and computes differential probabilities in ways that humans typically do not. It comments on and learns from the decisions of its human colleagues. It accesses public data sets and other information sources, informing the treatment team about new findings and developments the way Google informs us about the world in general. This is obviously a vision of the future, but it is a foreseeable future, and we already have the computer technology to build such a system. What we need is a fuller understanding of the course of illness and recovery, and a fuller accounting of the clinical decisions required in comprehensive integrated treatment and rehabilitation.
The R&D Agenda
A stage III CDSS can test the hypothesis that data-driven decision making enhances outcome, if it is sufficiently comprehensive. If that hypothesis can be supported, stage IV systems of increasing intelligence and sophistication would subsequently compete to produce the best possible outcome, as determined in comparative outcome trials. That process will extend through the foreseeable future, as we continue to improve our assessment methods and add new evidence-based practices to our treatment array.
Currently, there is no stage III CDSS comprehensive and reliable enough to provide a fair test of the key hypothesis. Until we can perform such a test, it is difficult to justify investing in development of stage IV capabilities. On the other hand, development of advanced cyber systems is not a linear process. In building a stage III system, we are confronted early on with the question of what data the system should include. What set of clinical and dispositional variables would be required to sufficiently represent and inform human JDM for this application? Our initial selections would be guided by a combination of theory, epistemology, and pragmatism. These selections reflect many of the human cognitive processes that must be emulated in an intelligent CDSS. In turn, articulation of the human processes further informs selection of variables. This pas de deux between content and process in cyber system development requires attention to both, even in development of less intelligent stage III systems.
In computer science and engineering, development of intelligent systems begins with a functional analysis of all the entities and activities in the environment in which the systems will operate. In the course of this analysis, development of a “domain ontology” begins. The domain ontology is the vocabulary that defines all the concepts, constructs, objects and variables, and their interrelationships, within an intelligent system’s scope of operation. Developing the domain ontology is a fundamental aspect of intelligent system design, but for complex applications, it is an exhaustive and time-consuming process. Fortunately, commercial software has evolved to assist in achieving the perfect consistency required for computerization.
As development proceeds, the system advances through stage III as the domain ontology incorporates variables into a database capable of tracking all the factors pertinent to all the decisions that must be made, the actions those decisions drive, and the consequences of the actions. Development reaches stage IV as the domain ontology becomes comprehensive enough to support “knowledge management” and “problem solving,” the algorithms by which the CDSS organizes its data and makes its own judgments and decisions.
The world of psychiatric rehabilitation has many similarities and overlaps with the worlds of general health care, conventional mental health services, physical rehabilitation, psychotherapy, and others. This can both inform and mislead design of a CDSS expressly for psychiatric rehabilitation. In the course of the pas de deux between content and process, between ontology and database development, and between computer scientist and clinical scientist-practitioner, some characteristics of psychiatric rehabilitation emerge as having especially salient implications for the ontology, knowledge management, and problem solving of a stage III and stage IV CDSS:
A Rehabilitation/Recovery Orientation
Psychiatric rehabilitation is based on precepts that are fundamentally different from those of conventional psychiatry. The condition of concern is not a disease to be cured but a disability to be overcome. Recovery is not simply elimination of the symptoms of the disease, but regaining a meaningful life, having friends, a meaningful occupational pursuit, hope for a better future, a sense of self. A stage III CDSS must recognize a broader array of treatment goals, or more properly, “recovery goals,” than in conventional psychiatric treatment of SMI. These goals are determined, at least in part, by the patient’s preferences and priorities, not by inference from a diagnosis or comparable designation. The centrality of recovery goals to rehabilitation is universally recognized, yet we know almost nothing about how people formulate such goals. Development of reliable measures of patient’s recovery goals, and their ability to formulate such goals, will be a rate-limiting factor in developing stage III systems. Developing a better understanding of how people formulate recovery goals, and methods for enhancing people’s ability to do so, will be a rate-limiting factor in development of stage IV systems capable of assisting with the goal-setting process.
The Biosystemic Model of Illness, Treatment, and Recovery
SMI is the result of semi-independent vulnerabilities and etiological processes that operate at physiological, neurocognitive, social-cognitive, behavioral, and socioenvironmental levels of organismic functioning. The characteristics listed in table 1, the sources of heterogeneity, are distributed across all those levels. Our treatment array increasingly targets processes at all levels. This is necessary because impairments and disabilites in SMI do not cascade from molecular causes in a way that makes focal treatment of the cascade’s origin an effective strategy (eg, as in infectious diseases). The complexity this produces is what necessitates personalization and integration of treatment.
A stage III CDSS must have an assessment repertoire capable of measuring functioning at all levels of biosystemic organization, especially specific impairments known to produce specific consequences. We arguably have clinical measures sufficient to meet this demand, but no single database has ever been constructed that is even presumed to include enough of them to support comprehensive treatment and rehabilitation. In the near future, rapid scientific developments may create new assessment domains, eg, the potential impact of genomics on the neurophysiological assessment that informs pharmacotherapy. One challenge for both stage III and stage IV systems will be to keep up with such advances and manage an increasingly diverse and extensive assessment repertoire. A stage IV system will need algorithms that weigh the influence of factors across all levels of functioning over time, like the example in figure 1. It will take a lot of effort to formulate and test a sufficient collection of such algorithms.
Patient Perspective and Involvement
Consistent with the principles of rehabilitation and recovery, the patient has a more central and active role in decision making than in conventional psychiatric treatment of SMI. This goes beyond setting goals, to detailed preferences about treatment options and trade-offs. Can we actually represent a patient’s personal perspective pertinent to psychiatric rehabilitation as an array of quantitative measures? A database for tracking all that information will be quite extensive, and no precedent or prototype exists. This will be a new challenge for stage III systems. For stage IV, we will need algorithms that can weigh these preferences against other factors, including the patient’s competence to make informed decisions, legal imperatives, and risks. In some cases, there will be conflict between patient preference and expectation of effectiveness. In others, patient preference may actually moderate treatment effectiveness. In still others, patient preference may decide between otherwise equivocal alternatives.
Functional Assessment and Analysis
In psychiatric rehabilitation, functional assessment and analysis supplant diagnosis as the operational link between assessment and treatment. Functional analysis is familiar to behaviorally oriented clinicians as a systematic process of identifying environmental and intrapersonal antecedents and consequences of behaviors of clinical interest, for the purpose of bringing them under therapeutic control. However, the functional-analytic approach is also applicable to antecedents, consequences, and behaviors at all levels of organismic functioning. A version of this approach has been formulated expressly for people with SMI undergoing rehabilitation and recovery.33 It can play a major role in understanding the nature of specific problems and selecting and shaping treatment.
Functional-analytic data are “idiographic,” meaning unique to the individual rather than a value on a scale equally applicable to all individuals. For example, the target behavior in a behavior change program is defined and described for a particular patient. Quantitative measures such as frequency or intensity can then be applied to the target behavior. Although behavior therapists have long been using sophisticated methods to track idiographic clinical data, these methods have not yet been incorporated in a CDSS sufficiently comprehensive for psychiatric rehabilitation. The stage III challenge will be to develop a database that includes both conventional (nomothetic) scalar variables and idiographic variables. The stage IV challenge will be to codify the principles of interpreting functional analytic data as computer algorithms and then to formulate algorithms that include idiographic and conventional scalar data in reaching judgments and decisions.
Functional assessment is distinct from functional analysis. The former uses conventional scalar measures to determine people’s ability to perform functional tasks, such as cooking, housekeeping, managing personal finances, and resolving interpersonal conflicts. Impairments in these domains are understood to be causally proximal to the disabilities of SMI. Stage III systems can take advantage of a well-developed assessment arsenal for functional abilities. The challenge for stage IV will be to develop algorithms that distinguish between functional impairments that result from problems in other areas, such as neurophysiological dysregulation or cognitive impairment, and those that result from skill deficits. This has obvious implications for treatment selection.
Problem-oriented “treatment planning” is an approach to health care documentation that resolves incompatibilities between traditional diagnosis-driven treatment and functionally driven psychiatric rehabilitation. It was introduced in the 1960s as a way to standardize medical record formats and persisted in psychiatry because of the notoriously weak relationship between diagnosis and treatment outcome. A comprehensive account of psychiatric rehabilitation34 has shown that a problem-oriented treatment planning approach can incorporate functional analytic methods and the principles of biosystemic psychopathology. Problem-oriented treatment plans will probably provide a key organizational format for stage III and stage IV systems.
The Hypothetico-Deductive Method
Case-wise application of the hypothetico-deductive method is arguably a feature of science-informed or evidence-based clinical practice in general. The complexity of problems confronted in psychiatric rehabilitation requires that this approach be applied even more aggressively than usual. For example, the clinician is often confronted with such questions as, “Is this particular behavior the result of acute psychosis, deficient social skills, or perverse institutional incentives to engage in inappropriate behavior?” The most reliable way to decide is to choose the highest probability alternative, treat accordingly, and evaluate the outcome. Better initial assessment may improve our chances of guessing correctly the first time, but we may never be able to eliminate the need for careful, systematic evaluation of treatment response. The main implication for level III development is that the database must include measures not just for making the initial formulation but also for tracking treatment response. These are not necessarily the same measures. For stage IV, the system must be able to design a data collection and analysis protocol, based on the initial hypothesis and expected treatment response and then monitor the data to determine, within a time frame specific to the hypothesized problem and the selected treatment, whether treatment is effective. If treatment is not effective, the stage IV algorithms must recycle the hypothetico-deductive process to find the next-best guess and formulate a new treatment trial.
Contextual Factors
Contextual factors often constrain clinical practice, although in conventional settings, these are usually annoyances to be managed through good administrative oversight. For example, if there is a need for a drug that is not in the formulary, the Formulary Committee should take care of that. In mental health, and especially in SMI services, contextual factors are more pervasively influential, and less amenable to solution through administrative means. Treatment decisions are influenced by institution or agency policy, local regulatory constraints, funding channels, civil commitment and competence laws, and most especially, limited treatment arrays. There is no precedent for including in a CDSS a database that represents the contextual factors that may impinge on JDM. A stage III system may have to rely on human understanding of local context until very advanced stages of development. Ultimately, though, a stage IV system will need to be able to access a reasonably complete set of that information, and use it at appropriate points in the rehabilitation and recovery process.
Conclusions
The momentum of the Information Age will inevitably drive development of increasingly sophisticated EMRs for mental health services. Multivariate research on the course of SMI is stimulating development of databases that capture increasingly comprehensive pictures of the course of illness, treatment, rehabilitation, and recovery.35 Increasingly, holistic theoretical accounts of SMI and rehabilitation11,35 are guiding joint development of databases and domain ontology. At some point in the near future we will cross the threshold where an outcome trial testing the contributions of a stage III CDSS will become feasible. There will follow a period of research establishing the particular circumstances and clinical settings in which clinical JDM is sufficiently complex that outcome benefits from cyber system support.
Support of the key hypothesis that JDM makes a difference will provide the scientific and economic incentive to build a stage IV CDSS. Psychopathologists and others will compete to formulate the most effective algorithms, based on clinical experience as well as empirical research. Clinical effectiveness will supplant construct validation as the criterion of success for intelligent systems. As science marches on, new findings and insights will produce increasingly intelligent systems, and they will play an increasingly important role in personalizing psychiatric rehabilitation and optimizing outcome.
Funding
National Institute of Mental Health (R24 MH073858)
Acknowledgments
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1.Insel TR. Translating scientific opportunity into public health impact: a strategic plan for research on mental illness. Arch Gen Psychiatry. 2009;66:128–133. doi: 10.1001/archgenpsychiatry.2008.540. [DOI] [PubMed] [Google Scholar]
- 2.Heinssen RK, Cuthbert BN, Breiling J, Colpe LJ, Dolan-Sewell R. Overcoming barriers to research in early serious mental illness: issues for future collaboration. Schizophr Bull. 2003;29:737–745. doi: 10.1093/oxfordjournals.schbul.a007043. [DOI] [PubMed] [Google Scholar]
- 3.Francey SM, Nelson B, Thompson A, et al. Who needs antipsychotic medication in the earliest stages of psychosis? A reconsideration of benefits, risks, neurobiology and ethics in the era of early intervention. Schizophr Res. 2010;119:1–10. doi: 10.1016/j.schres.2010.02.1071. [DOI] [PubMed] [Google Scholar]
- 4.Kashner TM, Rush AJ, Crismon ML, et al. An empirical analysis of cost outcomes of the Texas Medication Algorithm Project. Psychiatr Serv. 2006;57:648–659. doi: 10.1176/ps.2006.57.5.648. [DOI] [PubMed] [Google Scholar]
- 5.de Leon J. The future (or lack of future) of personalized prescription in psychiatry. Pharmacol Res. 2009;59:81–89. doi: 10.1016/j.phrs.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 6.de Leon J. Pharmacogenomics: the promise of personalized medicine for CNS disorders. Neuropsychopharmacology. 2009;34:159–172. doi: 10.1038/npp.2008.147. [DOI] [PubMed] [Google Scholar]
- 7.Goldstein WM, Hogarth RM, editors. Research on Judgment and Decision Making: Currents, Connections, and Controversies. Cambridge, UK: Cambridge University Press; 1997. [Google Scholar]
- 8.Abidi S. Breast ontology-based modeling of breast caccer follow-up clinical practice guideline fo providing clinical decision support. Twentieth IEEE International Symposium on Computer-based Medical Systems (CBMS ’07) 2007; Maribor, Slovenia. 542–547. [Google Scholar]
- 9.Brochhausen M, Weiler G, Cocos C, Stenzhorn H, Graf N, Drr M, Tsiknakis M. The ACGT master ontology on cancer—a new terminology source for oncological practice. In: Proceedings of the 21st IEEE International Symposium on Computer-based Medical Systems, 2008; Jyväskylä, Finland. 324–329. [Google Scholar]
- 10.Candelieri A, Conforti D, Perticone F, Scicqua A, Kawicka-Jaszcz K, Styczkiewicz K. Early detection of decompensation conditions in hear failurepatients by knowledge discovery: the HEARTFAID approaches. Comput Cardiol. 2008;35:893–896. [Google Scholar]
- 11.Roder V, Mueller D, Brenner HD, Spaulding W. Integrated Psychological Therapy for Schizophrenia. 2nd ed. London, UK: Hogrefe; 2010. [Google Scholar]
- 12.Peer J, Rothmann T, Penrod R, Penn D, Spaulding W. Social cognitive bias and neurocognitive deficit in paranoid symptoms: evidence for an interaction effect and changes during treatment. Schizophr Res. 2004;71:463–471. doi: 10.1016/j.schres.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 13.Peer J, Strachan E, Spaulding W. Heterogeneity in behavioral treatment response in severe mental illness. J Nerv Ment Dis. 2008;196:198–206. doi: 10.1097/NMD.0b013e318165c7d2. [DOI] [PubMed] [Google Scholar]
- 14.Peer JE, Spaulding WD. Heterogeneity in recovery of psychosocial functioning during psychiatric rehabilitation: an exploratory study using latent growth mixture modeling. Schizophr Res. 2007;93:186–193. doi: 10.1016/j.schres.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 15.Brekke J, Kay DD, Lee KS, Green MF. Biosocial pathways to functional outcome in schizophrenia. Schizophr Res. 2005;80:213–225. doi: 10.1016/j.schres.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 16.Spaulding W, Fleming S, Reed D, Sullivan M, Storzbach D, Lam M. Cognitive functioning in schizophrenia: implications for psychiatric rehabilitation. Schizophr Bull. 1999;25:275–289. doi: 10.1093/oxfordjournals.schbul.a033378. [DOI] [PubMed] [Google Scholar]
- 17.Bell MD, Weinstein A. Simulated job interview skill training for people with psychiatric disability: feasibility and tolerability of virtual reality training. Schizophr Bull. 2011;37:S91–S97. doi: 10.1093/schbul/sbr061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Medalia A, Saperstein A. The role of motivation for treatment success. Schizophr Bull. 2011;37:122–128. doi: 10.1093/schbul/sbr063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spaulding W, Poland J. Cognitive rehabilitation for schizophrenia: enhancing social cognition by strengthening neurocognitive functioning. In: Corrigan P, Penn D, editors. Social Cognition in Clinical Psychology. Washington, DC: American Psychological Association; 2001. pp. 217–248. [Google Scholar]
- 20.Haddock G, Tarrier N, Spaulding W, Yusupoff L, Kinney C, McCarthy E. Individual cognitive-behavior therapy in the treatment of hallucinations and delusions: a review. Clin Psychol Rev. 1998;18:821–838. doi: 10.1016/s0272-7358(98)00007-5. [DOI] [PubMed] [Google Scholar]
- 21.Deogun J, Spaulding W, Sahi S, Nolting J. Conceptual development of mental health ontologies. In: Ras ZW, Tsay L, editors. Advances in Intelligent Information Systems. New York, NY: Springer; 2010. [Google Scholar]
- 22.Katsikopoulos K, Pachur T, Machery E, Wallin A. From Meehl to fast and frugal heuristics (and back): New insights into how to bridge the clinical-actuarial divide. Theory Psychol. 2008;18:443–464. [Google Scholar]
- 23.Musen M. Technology for building intelligent systems: from psychology to engineering. In: Shuart B, Spaulding W, Poland J, editors. Modeling Complex Systems: Nebraska Symposium on Motivation. Vol 52. Lincoln, NE: University of Nebraska Press; 2007. [PubMed] [Google Scholar]
- 24.Kupper Z, Tschacher W. Symptom trajectories in psychotic episodes. Compr Psychiatry. 2002;43:311–318. doi: 10.1053/comp.2002.33501. [DOI] [PubMed] [Google Scholar]
- 25.McKibben C, Brekke J, Sires D, Jeste DV, Patterson TL. Direct assessment of functional abilities: relevance to persons with schizophrenia. Schizophr Res. 2004;72:53–67. doi: 10.1016/j.schres.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 26.Beck NC, Durrett C, Stinson J, Coleman J, Stuve P, Menditto A. Trajectories of seclusion and restraint use at a state psychiatric hospital. Psychiatr Serv. 2008;59:1027–1032. doi: 10.1176/ps.2008.59.9.1027. [DOI] [PubMed] [Google Scholar]
- 27.Gard DE, Fisher M, Garrett C, Genevsky A, Vinogradov S. Motivation and its relationship to neurocognition, social cognition, and functional outcome in schizophrenia. Schizophr Res. 2009;115:74–81. doi: 10.1016/j.schres.2009.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paul GL, editor. Observational Assessment Instrumentation for Service and Research—The Time-Sample Behavioral Checklist: Assessment in Residential Treatment Settings. Part 2. Champaign, IL: Research Press; 1988. [Google Scholar]
- 29.Paul GL, editor. Observational Assessment Instrumentation for Service and Research—The Staff-Resident Interaction Chronograph: Assessment in Residential Treatment Settings. Part 3. Champaign, IL: Research Press; 1988. [Google Scholar]
- 30.Paul GL, editor. Observational Assessment Instrumentation for Service and Research—The Computerized TSBC/SRIC Planned Access Observational Information System: Assessment in Residential Treatment Settings. Part 4. Champaign, IL: Research Press; 1988. [Google Scholar]
- 31.Young AS, Mintz J, Cohen AN, Chinman MJ. A network-based system to improve care for schizophrenia: the Medical Informatics Network Tool (MINT) J Am Med Inform Assoc. 2004;11:358–367. doi: 10.1197/jamia.M1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buican B, Spaulding W, Gordon B, Hindman T. Clinical decision support systems in state hospitals. In: Spaulding W, editor. The Role of the State Hospital in the 21st Century. Vol 84. San Francisco, CA: Jossey-Bass; 1999. pp. 99–112. [DOI] [PubMed] [Google Scholar]
- 33.Hunter RH, Wilkniss S, Gardner W, Silverstein SM. The Multimodal Functional Model–advancing case formulation beyond the ‘diagnose and treat’ paradigm: Improving outcomes and reducing aggression and the use of control procedures in psychiatric care. Psychol Serv. 2008;5:11–25. [Google Scholar]
- 34.Spaulding W, Sullivan M, Poland J. Treatment and Rehabilitation of Severe Mental Illness. New York, NY: Guilford; 2003. [Google Scholar]
- 35.Brekke J, Phillips E, Pancake L, Lewis A, Duke J. Implemetation practice and implementation research: a report from the field. Res Soc Work Pract. 2009;19:592. [Google Scholar]