Abstract
OBJECTIVE
To quantify the impact of cash transfer and microfinance interventions on a selected list of tuberculosis (TB) risk factors and assess their potential role in supporting TB control.
DATA SOURCE
Published and unpublished references identified from clinical and social electronic databases, grey literature and web sites.
METHODS
Eligible interventions had to be conducted in middle- or low-income countries and document an impact evaluation on any of the following outcomes: 1) TB or other respiratory infections; 2) household socio-economic position; and 3) factors mediating the association between low household socio-economic position and TB, including inadequate health-seeking behaviours, food insecurity and biological TB risk factors such as human immunodeficiency virus (HIV) and adult malnutrition. Interventions targeting special populations were excluded.
RESULTS
Fifteen cash transfer schemes (four unconditional and 11 conditional) and seven microfinance programmes met the eligibility criteria. No intervention addressed TB or any other respiratory infection. Of 11 cash transfer and four microfinance interventions, respectively seven and four reported a positive impact on indicators of economic well-being. A positive impact on household food security was documented in respectively eight of nine and three of five cash transfer and microfinance interventions. Improved health care access was documented respectively in 10 of 12 cash transfer and four of five microfinance interventions. The only intervention evaluating impact on HIV incidence was a microfinance project that found no effect. No cash transfer or microfinance interventions had an impact on adult malnutrition.
CONCLUSIONS
Cash transfer and microfinance interventions can positively impact TB risk factors. Evaluation studies are urgently needed to assess the impact of these social protection interventions on actual TB indicators.
Keywords: tuberculosis, cash, microcredit, impact, review
THERE IS EVIDENCE that the reduction in tuberculosis (TB) mortality observed in Europe and North America before World War II resulted from the successful combination of economic growth and specific public health policies such as patient isolation and the elimination of bovine TB.1,2 The importance of a combined approach has recently been reinforced by a number of studies suggesting that while DOTS programmes have significantly contributed to the reduction of TB prevalence and TB mortality, socio-economic development still remains the main determinant of TB incidence decline in many regions of the world.3-5 Despite this, literature on interventions addressing structural and social determinants6 of TB is currently virtually non-existent. Through the improvement of material living conditions, psychosocial circumstances and health-seeking behaviours, these interventions have the double potential to improve access to quality TB care and also reduce people’s vulnerability to TB.
A broad range of poverty alleviation strategies may achieve the above objectives; among them, cash transfer and microfinance programmes have gathered considerable visibility in the last decade, due to both the large number of individuals enrolled and the increasing number of studies formally documenting their impact.
Cash transfers are innovative forms of social protection based on the provision of money to poor or vulnerable households and individuals (such as the elderly and children) with the aim of enabling them to move out of poverty by protecting and building their financial, physical and human capital assets.7 Cash transfers can be unconditional (given without obligation) or conditional on some behavioural requirements, such as school enrolment, health services utilisation and/or the attendance of health education workshops. Microfinance programmes are considered poverty alleviation measures aimed at directly averting deprivation.8 These programmes are based on the provision to the poor of small loans to enable them to engage in productive activities that can ultimately contribute to their long-term economic growth and productivity.8
Despite the impressive scale-up of these interventions and their acknowledged potential public health relevance,9,10 their relevance for TB control largely depends on evidence of their effect on outcomes epidemiologically linked to TB and the critical assessment of the challenges limiting their implementation in the context of TB.
This review aimed to address these issues by: 1) systematically quantifying the impact of these interventions and 2) evaluating their main design and implementation features from the perspective of TB control.
METHODS
Conceptual framework
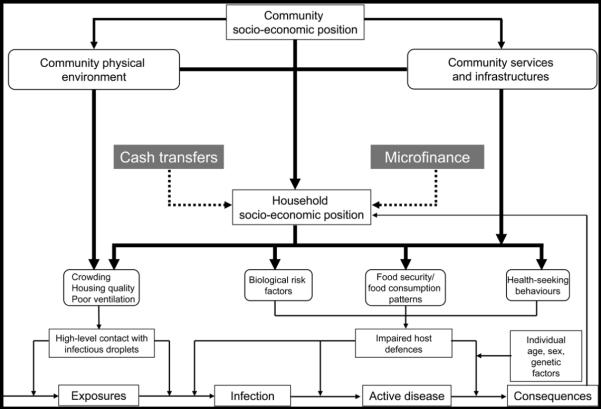
Hargreaves et al. discuss the mechanisms by which cash transfer and microfinance interventions might contribute to strengthening the international TB response, which outcome and risk factors may be potentially impacted by such interventions, and which effect should be expected depending on the stage of TB targeted (i.e., TB exposure, infection, disease and outcomes).11 Building on this conceptual framework, we designed this review to formally assess the impact of cash transfer and microfinance interventions on the hypothesised TB outcomes and risk factors. In particular, we focused on household socio-economic position and those risk factors that mediate the association between household socio-economic position and TB disease, including inappropriate health-seeking behaviours, food insecurity12 and biological risk factors impairing host immune system defences (such as human immunodeficiency virus [HIV] and adult malnutrition; Figure).
Figure.
Conceptual framework. In this review we focus on tuberculosis (TB) disease and interventions targeting socio-economic position at household level. It is hypothesised that cash transfer, either conditional or unconditional, and microfinance interventions can support TB control by improving a household’s socio-economic position and thereby reducing the exposure to biological risk factors (such as human immunodeficiency virus and malnutrition) and improving the household food security and health-seeking behaviour.
Search strategy and selection criteria
A wide range of electronic databases and websites were searched (Table 1). Eligible interventions had to: 1) address the following outcomes of interest: TB (or other respiratory infections), household socio-economic position or any of the postulated mediating risk factors (Figure); 2) explicitly document an impact evaluation (i.e., the assessment of any change in a given outcome among the intervention beneficiaries compared to the non-beneficiaries); and 3) take place in low- and middle-income countries.
Table 1.
Search strategy. As the terminology in socio-economic interventions is often imprecise, technical (non-medical) and constantly evolving, we first conducted a scoping search with a provisional set of text word terms.13 We then refined the search strategy by adding indexed terms and text words as suggested by the studies identified in the preliminary search.
| Queries launched through electronic databases | |||
|---|---|---|---|
| Electronic databases |
Biomedical EMBASE MEDLINE Global Health HMIC EPPI DoPHER TRoPHI Social sciences Social Policy & Practice |
Socio-economic interventions Social protection/ livelihood strengthening |
(Socioeconomic OR Social OR Economic OR Complex OR Structural) AND (Programme OR Program OR Project OR Intervention OR Prevention) AND (Evaluation OR Impact) (Microcredit OR Microfi nance OR Cash OR economic empowerment OR Income) AND (Poverty OR food security OR Access OR Health-seeking behaviours OR TB OR Respiratory OR HIV OR Nutrition) AND (Reduction OR Progr* OR Project OR Prevention OR Integration) AND (Evaluation OR Impact) |
| Websites |
http://scholar.google.com; http://www.omni.ac.uk; http://www.sosig.ac.uk; http://www.eelv.ac.uk; http://www.undp.org; http://www.worldbank.org; http://www.eldis.org; http://www.usaid.gov; http://www.dfid.gov.uk; http://www.ifpri.org |
||
| Grey literature and expert consultation | |||
Experimental and observational studies with a controlled or uncontrolled design providing a retrospective or a prospective evaluation of the intervention of interest were included. No time or language restriction was applied. Studies conducted in specific special settings (e.g., hospitals, prisons, workplaces, schools) or in specific population groups (e.g., homeless, professional categories, students) were excluded. Given the heterogeneity of the study design and study results, the evidence collected was summarised through a ’narrative synthesis’ approach.14,15
RESULTS
Approximately 150 documents of potential interest were appraised. Through them, we identified 15 cash transfer and 7 microfinance intervention evaluations meeting the inclusion criteria, from respectively 13 and 5 different countries (Table 2). Evidence on microfinance was integrated with data from a recent review on the impact of microfinance on poverty and household socio-economic position.16
Table 2.
Study design and main study findings: an overview
| Impact findings* |
||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention | Country† | Type of intervention |
Evaluation design |
Follow-up period | Significant positive impact |
Uncertain positive impact‡ |
No effect |
Opposite impact to that expected |
| Poverty/household socio-economic position§ | ||||||||
| RMP | Bangladesh | CCT | H-QEXP | 25 months¶ | • • | — | — | — |
| BF | Brazil | CCT | H-QEXP | 2004–2005 | — | — | • | — |
| PFA | Colombia | CCT | C-QEXP | 2002–2003 | • • | — | — | — |
| BDH | Ecuador | CCT | CRT | 2003–2005 | — | — | • | — |
| PRAF | Honduras | CCT | CRT | 2000–2002 | — | — | • | — |
| PROGRESA | Mexico | CCT | CRT | 1998–2000 | — | • | — | — |
| RPS | Nicaragua | CCT | CRT | 2000–2004 | • • • | — | — | — |
| PSNP# | Ethiopia | SCT | H-QEXP | 01/2005–06/2006 | — | — | • | • |
| MCHINJI | Malawi | SCT | H-QEXP | 2007–2008 | • • • | — | — | — |
| DECT | Malawi | SCT | CSS | 12/2006–04/2007 | — | • | — | — |
| SCT | Zambia | SCT | H-QEXP | 2004–2007 | — | • • | — | — |
| CFRP/TUP | Bangladesh | Microfinance | C-QEXP | 2002–2004 | • | — | — | — |
| RDP | Bangladesh | Microfinance | H-QEXP | 1993 and 1996 | • • | — | — | — |
| IGVGD | Bangladesh | Microfinance | CSS | 1994, 1996, and 1999 | — | • • • | — | — |
| IMAGE | South Africa | Microfinance | CRT | 2001–2005 | — | • • | — | — |
| Food security/household food consumption patterns** | ||||||||
| RMP | Bangladesh | CCT | H-QEXP | 25 months¶ | • • | — | • | — |
| BF | Brazil | CCT | H-QEXP | 2004–2005 | — | • • • | — | — |
| PFA | Colombia | CCT | C-QEXP | 2002–2003 | • • | — | — | — |
| PROGRESA | Mexico | CCT | CRT | 1998–2000 | • | • • • | — | — |
| RPS | Nicaragua | CCT | CRT | 2000–2004 | • • • | — | — | — |
| PSNP# | Ethiopia | SCT | H-QEXP | 01/2005–06/2006 | — | — | • • • | — |
| MCHINJI | Malawi | SCT | H-QEXP | 2007–2008 | • • • | — | — | — |
| DECT | Malawi | SCT | CSS | 12/2006–04/2007 | — | • • • | — | — |
| SCT | Zambia | SCT | H-QEXP | 2004–2007 | — | • • • | — | — |
| CFRP/TUP | Bangladesh | Microfinance | H-QEXP | 2002–2004 | • • • | • • | — | — |
| Grameen Bank†† | Bangladesh | Microfinance | CSS | Not reported | • | — | — | — |
| WISDOM | Ethiopia | Microfinance | CSS | 10 and 20 months¶ | — | — | • • • | — |
| IMAGE | South Africa | Microfinance | CRT | 2001–2005 | — | — | • | — |
| Kafo Jigenew†† | Mali | Microfinance | CSS | 12 and 24 months¶ | • • | — | — | — |
| Health-seeking behaviours/health care access†† | ||||||||
| BF | Brazil | CCT | C-QEXP | 2004–2005 | — | — | • • | — |
| PFA | Colombia | CCT | C-QEXP | 2002–2003 | • | — | — | — |
| PRAF | Honduras | CCT | CRT | 2000–2002 | • • | — | • | — |
| JSY | India | CCT | H-QEXP | 2002/4–2007/9 | • • • | — | — | — |
| PATH | Jamaica | CCT | H-QEXP | 2004–2005 | • | — | • | — |
| — | Malawi | CCT | RT | Not applicable§§ | • • • | — | — | — |
| PROGRESA | Mexico | CCT | CRT | 1998–2000 | • • | • • • | — | — |
| SDIP | Nepal | CCT | CSS | 2005–2008 | • • • | — | — | — |
| RPS | Nicaragua | CCT | CRT | 2000–2004 | • | • | — | — |
| MCHINJI | Malawi | SCT | H-QEXP | 2007–2008 | • • | — | — | — |
| DECT | Malawi | SCT | CSS | 12/2006–04/2007 | — | • | — | — |
| SCT | Zambia | SCT | H-QEXP | 2004–2007 | — | — | • | — |
| RDP/ICCDR,P | Bangladesh | Microfinance | H-QEXP | 1992,1996, 2001 | — | — | — | • |
| CFRP/TUP | Bangladesh | Microfinance | H-QEXP | 2002–2004 | • • • | • • | • | — |
| CHC | Cambodia | Microfinance | CSS | 1999–2001 | • • | • • | — | — |
| SHG | India | Microfinance | CSS | ≤48 and >48 months¶ | • | — | • | — |
| IMAGE | South Africa | Microfinance | CRT | 2001–2005 | • | — | — | — |
| Factors impairing host defences: adult malnutrition¶¶ and HIV | ||||||||
| RMP | Bangladesh | CCT | H-QEXP | 25 months¶ | — | — | • | — |
| PROGRESA | Mexico | CCT | CRT | 1998–2000 | — | — | — | • |
| MCHINJI | Malawi | SCT | H-QEXP | 2007–2008 | — | — | • | — |
| CFRP/TUP | Bangladesh | Microfinance | H-QEXP | 2002–2004 | — | — | • | — |
| WISDOM | Ethiopia | Microfinance | CSS | Not applicable§§ | — | — | • | — |
| IMAGE | South Africa | Microfinance | CRT | 2001–2005 | — | — | • | — |
• = evidence from one indicator; •• = evidence from 2 indicators; ••• = evidence from 3 or more indicators.
Countries listed in alphabetical order and by type of intervention.
Measures of effect did not reach significance level or it was not reported in the reference.
Indicators include household consumption expenditure (monthly or annual, per capita or total), household income (monthly or annual, per capita or total), proportion of households below the poverty line or the extreme poverty line, number of assets owned and proportion of households in debt.
Length of time of beneficiaries’ participation at the time of the survey.
The impact evaluation of the PSNP was conducted using three different definitions of ‘treatment’ households. In this article we reviewed the impact data following from the first definition (i.e., households that received any cash for public works in the period from June 2005 to May 2006). This was due to the second definition adopted providing data only from a sub-region of Ethiopia, whereas the third did include households receiving PSNP completed by other food security interventions, making it difficult to understand the net impact of PSNP.
Indicators include food quantity (i.e., number of meals per day, grams of food per day) and quality (food diversity, consumption of meals containing proteins), food availability, food shortage, mean Kcalories intake per capita, food share, monthly expenditure on food.
Results from the Goldberg review16 are synthesised in the text.
Indicators include mean total number of consultations per month (overall and by specific health care provider), health care expenditure, antenatal care, infacility births, skilled birth attendance, post partum check-ups, preventive health care visits, child growth monitoring visits, HIV testing and results collection, exclusion from health care, mean case notification rates, proportion of extra-pulmonary cases detected, diagnostic delay.
In this intervention, respondents in rural Malawi were offered free door-to-door HIV testing and were randomly given US$0–US$3 redeemable upon obtaining HIV testing results after 2–4 months from sample collection.
As TB is an adult disease, we focused on adult malnutrition. Indicators include prevalence of acute malnutrition measured by body mass index (BMI) and mid-upper arm circumference (MUAC).
RMP = Rural Maintenance Programme; CCT = conditional cash transfer; H-QEXP = Household–Quasi-experimental design; BF = Bolsa Familia; PFA = Programa Familias en Acción; C-QEXP = Community-Quasi-experimental design; BDH= Bono de Desarollo Humano; CRT = Community Randomised Trial; PRAF = Programa de Asignación Familiar; PROGRESA = Programa de Educación, Salud y Alimentación; RPS = Red de Proteción Social; PSNP = Productive Safety Net Program; SCT = Social Cash Transfer; DECT = Dowa Emergency Cash Transfer Project; CSS = Cross Sectional Survey; CFRP/TUP = Challenge the Frontiers of Poverty Reduction/Targeting the Ultra Poor; RDP = Rural Development Programme; IGVGD = Income Generation for Vulnerable Group Development; IMAGE = Intervention with Microcredit for AIDS and Gender Equity; JSY = Janani Suraksha Yojana; PATH = Programme for Advancement Through Health and Education; RT = Randomised Trial; SDIP = Safe Delivery Incentive Programme; ICCDR,B = International Centre for Diarrhoeal Research, Bangladesh; CHC= Cambodia Health Committee; SHG = Self-Help Group.
With the exception of one microfinance intervention in Cambodia,17 none of the interventions we reviewed targeted individuals with any kind of health conditions. For both microfinance and cash transfer interventions, the selection of the target population was based mainly on socio-economic criteria, the specificity of which varied depending on the intervention objectives and resources available.
Four of the 15 cash transfer programmes were unconditional, and these were all reported from African countries, including Ethiopia,18,19 Zambia20 and Malawi21,22 (Table 2). The only African study of a conditional programme was from Malawi, in which conditionality was based on HIV testing and the collection of HIV results.23
Virtually all conditional cash programmes from Latin America required child school enrolment, the attendance of nutritional education sessions and health care uptake for children (<5 years of age) and pregnant/lactating women; adult health conditionalities were less common, and included generic health care,24,25 in-facility medically attended delivery,26,27 HIV testing and result recollection.28
Apart from the Dowa Emergency Cash Transfers (DECT) intervention in Malawi,21 cash transfer schemes all employed complex impact evaluation designs, including community randomised trials and quasi-experimental studies (Table 2). Cross-sectional surveys were more commonly employed in microfinance interventions. The impact data refer to a follow up period of between 1 and 3 years of observation in most interventions (Table 2). Only in the microfinance intervention in Cambodia was the impact of the intervention measured against TB indicators.17
Impact on poverty and household socio-economic position
Evidence was gathered from 11 cash transfer and four microfinance interventions (Table 2).
In Nicaragua, Red de Protección Social beneficiary households found a significant net increase in both the total and per capita annual consumption (Table 3).29 A net increase in the overall monthly household expenditure was observed among the beneficiary households of PROGRESA in Mexico24 and the Programa Familias en Acción in Colombia,32 whereas Rural Maintenance Programme (RMP) beneficiaries in Bangladesh experienced a 31% increase in their monthly per capita expenditure (Table 3).34 In Malawi, Mchinji households showed a significantly higher annual expenditure, a higher income from all sources,22 as well as a higher number of assets owned compared to the control households.22 These results were also observed in Zambia (Table 3).20,37 The proportion of households living below the poverty line significantly decreased in Nicaragua,29 Colombia32 and Bangladesh34 (Table 3). No effect was detected among cash transfer participants in Honduras,38 Ecuador,38 Brazil33 or Ethiopia18 (Table 2).
Table 3.
Positive impact findings of conditional and social cash transfer: a quantitative summary
| Programme, country, reference |
Household socio-economic position |
Food security/household food consumption patterns |
|||||
|---|---|---|---|---|---|---|---|
| Income/expenditure | Poverty level | Food security | Food expenditure | Food quantity | Food quality | Health care seeking | |
| PROGRESA, Mexico24,30 |
+ 13% median monthly total expenditure† |
+ 11% monthly median increase/person‡ |
+ 7.8% mean Kcal/day/ person*† |
+30% monthly median value of animal products consumed/ person‡ +16.3% monthly median value of vegetables & fruit consumed/person‡ |
+2 visits/day/public clinic on average*† 78 quality score of health procedures received vs. 72 among non-beneficiaries* 8% increase in prenatal visits*† |
||
| PRAF, Honduras31 |
+ 18.7% antenatal care visits*† + 20.2% child care visits*† |
||||||
| RPS, Nicaragua29 | +US$322 annual total household expenditure*† + US$77 annual total per capita expenditure*† |
22% points reduction* † |
+ US$68 annual per capita* † +4.7% food share*† |
+2.2% food share on meat*† +2.4% on fats*† (compared to baseline) |
+16% child care visits in 2001 vs. 2000* +8.4% child care visits in 2002 vs. 2000 |
||
| PFA, Colombia32 | +19.5% and +9.3% average monthly total expenditure in rural and urban beneficiaries*† |
6% points reduction in both the rural and urban areas |
+US$27 and +US$15 monthly expenditure per rural and urban household*† |
+ 23% and +33% children (respectively 24 and 24– 48 months of age) with an up-to-date schedule of preventive health care visits* |
|||
| B F, Brazil33 | +23.2 Brazilian Real among intervention households |
||||||
| PATH, Jamaica25 | 38% increase in health care visits for children (0-6 years) |
||||||
| RMP, Bangladesh34 |
+ 31.4% average monthly per capita expenditure*† |
16% reduction*† | +113 Taka/person/ month† among benefi ciary households compared to the control group |
+ 271 Kcal/day/person*† | |||
| JSY, India§27 | +11% net increase in the frequency of women reporting three antenatal care visits*† +43.5% net increase in births in health facilities*† +36.2% net increase in skilled birth attendance*† |
||||||
| SDIP, Nepal35 | +13% increase in skilled birth attendance −5% decrease in delivery at home +24% increase in delivery in governmental institutions¶ |
||||||
| SCT, Zambia SCT‡20,36 |
+64% increase among beneficiary households compared to the control group |
13% households with 1 meal/day vs. 19% at baseline 35% households still hungry after meal vs. 56% at baseline |
Average weekly fat consumption rose from 0.7 days/week to almost 2 days/week Percentage of households consuming proteins 7 days/week increased from 23% to 35% |
||||
| MCHINGJI, Malawi#22 |
MK15 103 net annual non-food expenditure increase among intervention households compared to controls Intervention households reporting higher total annual income compared to control households (MK27 079 vs. MK3528)* |
88% of the intervention households had food store vs. 57% of control households* |
MK3125 net increase in monthly food expenditure among intervention households compared to controls* |
93% of intervention house- holds reported food consumption improved compared to 11% of control households* 37% of control households reporting hunger after meal compared to 7.5% of intervention households* Mean number of days without enough to eat in the past month: 1.2 (intervention households) vs. 5.2 (comparison households)* 44% of intervention households had three meals/day compared to 8% of control households* |
8.1 food groups on average consumed by intervention households vs. 4.9 in the control households* Intervention households reported to have meat, chicken and fish 2.1 days/week vs. 0.3/week in the control households* |
Beneficiary households more likely to get health care when members were sick compared to control households (84% vs. 10%)* 63% of control households reporting spending nothing on health care for adult illness compared to 25% of intervention households* |
|
| DECT, Malawi21 | 64% of cash transfer #x2003;spent on food |
Average number of meals rose #x2003;from 1.5 (2006) to 2.4 #x2003;(2007) and respectively #x2003;from 1.4 to 2.3 in male- #x2003;headed households and #x2003;from 1.2 to 2.5 in female- #x2003;headed households |
Number of different food #x2003;groups from 2.5 (2006) #x2003;to 4.0 and 3.6, #x2003;respectively, in male- #x2003;headed households #x2003;and female-headed #x2003;households (2007) |
||||
| Malawi23 | 27% increase in HIV testing #x2003;43% increase in VCT attendance #x2003;9.1% increase in VCT attendance #x2003;for every US$ of incentive |
||||||
Statistically significant result.
Result adjusted for confounding factors.
In Zambia, it was also documented that the average debt of beneficiary households dropped from approximately 13 000 Zambian Kwacha (USD 2.6) to 8000 (USD 1.6) and that the average number of assets per households rose from four to five.20
In the JSY programme in India the net impact has been estimated through three different methods. In the case of antenatal care visits, the net impact was equal to approximately 11% for all the three methods; in the case of in-facility birth the net impact was equal to 43.5%, 43.9% and 49.2%, depending on the method used; in the case of skilled birth attendance the net impact was equal to 36.6%, 36.2% and 39.3%, depending on the method used. For each indicator we have reported the lower estimate.27
The impact evaluation in Nepal was conducted through propensity score matching and time series analysis. Results in the table refer to the propensity score matching analysis. The time series analysis showed that the implementation of SDIP in Nepal had an immediate positive impact on the utilisation of institutional deliveries in governmental health facilities; however, the long-term effect is negative, with the SDIP effect disappearing in just 3 years from implementation. This has been attributed to the fact that in the hill district (accounting for most of the national deliveries) the implementation of SDIP was followed by a dramatic growth in the utilisation of home delivery care. Two possible explanations include the inefficient implementation in the programme in the first two years and the payment delays, which may have reduced programme’s credibility among women.35
In the Mchiji programme (Malawi) it was also documented that after one year of intervention more intervention households owned every type of asset and some households owned multiple assets per category.22
PRAF = Programa de Asignación Familiar; RPS = Red de Proteción Social; PFA= Programa Familias en Acción; BF = Bolsa Familia; PATH = Programme for Advancement Through Health and Education; RMP = Rural Maintenance Programme; JSY = Janani Suraksha Yojana; SDIP = Safe Delivery Incentive Programme; SCT= Social Cash Transfer; MK= Malawi Kwacha; DECT = Dowa Emergency Cash Transfer Project; HIV = human immunodeficiency virus; VCT= voluntary counselling and testing.
Microfinance appeared to significantly reduce extreme poverty, as demonstrated by the Challenge the Frontiers of Poverty Reduction/Targeting the Ultra Poor (CFRP/TUP) and the Rural Development Programme (RDP) interventions in Bangladesh39,40 (Tables 3 and 4). The percentage of Income Generation for Vulnerable Group Development (IGVGD) households earning more than 300 Taka rose from 7% (1994) to 64% (1996); however, it dropped to 31% 3 years after the intervention.47 Additional evidence from Goldberg’s review showed the consistently positive effect of microcredit on household poverty and socio-economic position.16 The Intervention with Microfinance for AIDS (acquired immunedeficiency syndrome) and Gender Equity (IMAGE) study in South Africa appeared to somewhat improve the economic well-being of beneficiary households (Table 4).42
Table 4.
Positive impact findings of microfinance interventions: a quantitative summary
| Programme, country, reference |
Household socio-economic position |
Food security/household food consumption patterns |
|||||
|---|---|---|---|---|---|---|---|
| Income/expenditure | Poverty level | Food security | Food expenditure | Food quantity | Food quality | Health care seeking | |
| IMAGE, South Africa 41,42 |
65% of IMAGE households able to spend >200 South African Rand on food and clothing vs. 54% of the control group† |
IMAGE clients: OR = 1.6, 95%CI 1.1–2.6 for HIV testing*† |
|||||
| CFRP/TUP, Bangladesh43-45 |
30% reduction* | 20% of households living in chronic food deficiency compared to 60% at baseline 14.9% of households couldn’t eat whole day vs. 62.1% at baseline |
+13.5 Taka/person/day vs. 8.7 at baseline* |
85 g/person/day animal food vs. 22 at baseline* 1019 g/person/day vs. 706 at baseline* 2138 Kcal/person/day vs. 1750* at baseline 3.2% of energy from animal source vs. 1.3% at baseline* |
5.6 different food items/day vs. 3.7* |
−7.2% self-care visits*† +9.2% formal care visits† |
|
| RDP, Bangladesh46 | 25% of RDP house- holds moved out of extreme poverty* 8% of RDP households moved into extreme poverty compared to 30% of the control group* |
||||||
| IGVGD, Bangladesh47 |
% of households earning >300 Taka rose from 7 (1994) to 64 (1996) Household monthly income rose from 75 Taka (1994) to 717 Taka (1996) |
||||||
| GRAMEEN BANK, Bangladesh16 |
+8% compared to non-clients in Grameen Villages +35% compared to non-clients in non Grameen Village |
||||||
| SHG, India48 | Exclusion from health care among SHG clients OR = 0.6 (0.4–0.9)*† |
||||||
| Cambodia Health Committee17 |
13% of extra-pulmonary cases detected through home-DOTS vs. 4% through hospital/health care package* 6 months diagnostic delay with home-DOTS vs. 30 months HHC* |
||||||
| KAFO JIGINEW, Mali16 |
12% of clients in food insecurity vs. 30% of incoming clients* 0.25 months in food insecurity (clients) vs. 1.2 (incoming clients) |
||||||
Statistically significant result.
Result adjusted for confounding factors.
IMAGE = Intervention with Microfinance for AIDS and Gender Equity; OR = odds ratio; CI = confidence interval; HIV = human immunodeficiency virus; CFRP/TUP = Challenge the Frontiers of Poverty Reduction/Targeting the Ultra Poor; RDP = Rural Development Programme; IGVGD= Income Generation for Vulnerable Group Development; SHG = Group.
Impact on food security and household food consumption patterns
Evidence was gathered from nine cash transfer and five microfinance interventions (Table 1), of which respectively eight and three reported a positive impact. An increase in food expenditure was documented in the conditional transfer programmes of Mexico,30 Nicaragua,49 Colombia,32 Brazil33 and Bangladesh34 and both the social cash transfer schemes in Zambia36,37 and the Mchinji in Malawi22 (Table 3). Beneficiaries of PROGRESA in Mexico and RMP in Bangladesh experienced a significant increase in the average daily energy intake.30,34 Except for Ethiopia,18 all the cash transfer schemes in Africa documented a significant increase in the daily number of meals consumed and a reduction in the number of households still hungry after a meal.20-22 Higher food quality and diversity are also an indicator of food security,50 and were both found to be improved in the cash transfer programmes of Mexico,30 Nicaragua,49 Zambia,36 and both the DECT and Mchinji cash transfer schemes in Malawi (Table 3).21,22
Among microfinance interventions, food expenditure increased significantly among CFRP-TUP44 and Grameen Bank clients (Tables 2-4),16 whereas no effect was observed among the IMAGE42 and WISDOM beneficiaries (Table 4).51 CFRP-TUP in Bangladesh39 and the Kafo Jijinew in Mali16 resulted in a significant reduction of the food insecurity experienced by clients in terms of acute food shortage,16,39 chronic food deficit39 and duration of food insecurity (Table 4).16 No effect on food security was observed among the IMAGE42 and WISDOM clients51 (Table 3). CFRP-TUP beneficiaries consumed significantly higher food quantity and quality intake compared to the control group (Table 4).44
Impact on health-seeking behaviours and health care access
Evidence was derived from 12 cash transfer and six microfinance interventions (Table 1). In Mexico, PROGRESA resulted in an 18% increase in child and adult health care visits in the intervention areas compared to control areas.24 A significant increase in the number of child-care visits was documented from Honduras,31 Nicaragua,29 Colombia52 and Jamaica25 (Table 3). Maternal health care also appeared to be improved, in terms of the frequency of antenatal visits,24,27,31 in-facility delivery,26,27 skilled birth attendance26,27 and the quality of services requested and received by women (Table 2).53 Mchinji beneficiaries in Malawi were significantly more likely to access heath care when sick compared to control households (Table 3).22 Unlike Zambia, where no effect was detected,36 Mchinji beneficiaries showed a significant increase in the household expenditure on each adult illness (Table 2).22 In the other Malawi study, monetary incentive resulted in a significant 27% increase in HIV testing and a 43% increase in voluntary counselling and testing attendance (Table 3).
CFRP-TUP microfinance clients experienced a significant increase in the use of formal medical care and health expenditure per ill person (Table 4),54 whereas, unexpectedly, the RDP/International Centre for Diarrhoeal Research Bangladesh intervention resulted in a significant increase in the proportion of households using self-care as an elective health care strategy (Table 2).55 Self-help group clients in India were significantly less likely than the comparison group to have experienced health exclusion.48 The Cambodia Health Committee intervention was associated with significant increases in both extra-pulmonary TB detection and earlier diagnosis compared to its hospital-based counterpart (Table 4).17 Finally, at follow-up, the IMAGE study showed a significant increase in the voluntary counselling and testing uptake in the intervention group compared to controls (Table 4).41
Impact on adult malnutrition and HIV
Impact on adult nutritional status, assessed as body mass index (BMI), was documented in three cash transfer schemes in Mexico,56 Bangladesh,34 Malawi,22 and two microfinance interventions in Ethiopia51 and Bangladesh.57 However, none of them appeared to have a significant positive impact on this indicator (Table 2). In Mexico, doubling cash transfer was associated with higher BMI among both male and female PROGRESA participants, but it was also associated with a higher prevalence of excess weight and obesity (Table 2).56 No significant reduction in HIV incidence was detected in the villages covered by the IMAGE intervention (Table 2).42
DISCUSSION
This review shows a lack of studies on microfinance and cash transfer interventions that specifically address TB or other respiratory infections. While the documented effect on risk factors epidemiologically relevant for TB may be an informative way of inferring the potential impact on TB of such interventions,58 this evidence cannot replace actual studies specifically addressing TB. The evidence gathered comes from a relatively small, heterogeneous pool of studies, making the data synthesis methodologically challenging and difficult to interpret. Also, given the relatively short follow-up period in many of the studies, little can be concluded concerning the sustainability of these impact findings. As a result, conclusions on the two main questions posed by this review should be drawn with caution.
Do cash transfer and microfinance interventions have a quantifiable impact on outcomes epidemiologically linked to TB?
Both conditional and unconditional cash transfer programmes have reported influences on risk factors for TB in countries with a major TB burden. In principle, if rolled out in communities with a high TB burden, these interventions have the potential to improve people’s access to TB service access and reduce people’s vulnerability to TB, by improving households’ socio-economic position and food security (in terms of both food availability and food diversity). The importance of the latter effect is supported by at least three historical studies that, despite their ecological design, present fairly convincing evidence that a low-protein diet has a direct effect on TB incidence.59 Although less consistently, this review also suggests that microfinance could benefit TB-affected communities by turning the loans received into income-generating activities. This may result in the improvement of household material well-being and also reduce household vulnerability.60 As discussed below, there may be significant barriers to successfully designing microfinance programmes for TB-affected families.
Both cash transfer and microfinance interventions had a modest positive impact on adult malnutrition, probably because nutritional status is a function not only of food availability, but also of health status and health care services utilisation.61 It is also known that lending programmes are unlikely to significantly improve nutritional status unless they are linked to education to promote nutritionally important behavioural changes.61 This last notion makes the adverse effect observed in the PROGRESA intervention even more surprising, given that participants did receive workshops on nutrition.56,62
The only study attempting to affect HIV incidence did not show the desired impact. Such results have been attributed to the fact that the microfinance and the gender and HIV training components of the I MAGE study did not directly aim to reach young people,63 but only indirectly, through changes in the household economy and information sharing between IMAGE clients and young people.63 Although both components were important elements of the interventions, such indirect targeting, together with the short follow-up period, may have been insufficient to instigate sexual behavioural changes, and therefore HIV decline, among the highest risk group.63
What are the key design and implementation challenges to consider?
Targeting and conditionality are critical aspects in the design and implementation of cash transfer schemes and microfinance interventions. In the light of TB control they could be read as follows.
Targeting
All the interventions appraised applied some population targeting criteria. Targeting is a complex and expensive procedure, often leading to accuracy, equity, sustainability and even stigma problems; all these factors are likely to become even more relevant when adopting either microfinance or cash transfer for TB control. It is unclear, for example, whether these interventions are best targeted at TB-affected families or very poor households. While this choice largely depends on the objective we want to achieve (e.g., TB prevention among the very poor or TB care support in TB-affected families), both options can be challenging.
In the case of microfinance, some experiences with people affected by HIV/AIDS suggest that targeting vulnerable populations (such as TB-affected families) with microfinance may result in poor loan management, inadequate use of the loan for the intended purposes, and weak repayment systems.64,65 This view is somewhat contradicted by the community-based programme conducted in Cambodia, where loan repayment rates approached 100% among TB-affected families benefiting from participation in village banks.17 Targeting TB-affected families with cash transfers may be similarly challenging from an ethical perspective, as unaffected families may be equally in need of assistance.66
Targeting very poor households at high risk of TB is also controversial. Microfinance institutions are generally reluctant to enrol very poor households due to their uncertain repayment capacity.67 It should be noted that there is a strong norm within the non-governmental microfinance sector to work towards a model of financial sustainability. High levels of loan repayment are essential, and this is of course quite different from cash transfer programmes. The IGVGD and CFRP-TUP microfinance interventions demonstrated that it is possible to bring even the most destitute households to a position where they can successfully access microfinance services.40,47 Nonetheless, when programmes were appraised in more detail, the reason for programme success did not appear to be principally due to microfinance. Rather, the main incentive to participate in IGVGD appeared to be receipt of supplementary food, whereas microfinance was probably the least successful component of the intervention, with an 8% repayment default rate among the clients.46 It is also noteworthy that the most successful microfinance programmes included in this review involved the creative and flexible collaboration between microfinance and safety net programmes (e.g., all the BRAC programmes)47 or training/education components (e.g., the IMAGE intervention).42 In conclusion, the adoption of microfinance for TB control purposes is possible; however, to be effective, additional health, nutritional and educational support may be necessary.
Conditionality
The experiences from Honduras, Ecuador and Columbia demonstrated that successful conditional cash transfer programmes can be implemented in very poor settings; however, the scaling up of conditional cash transfer programmes in high TB burden countries, often characterised by weak health systems and administrative capacities, may be challenging.68,69 Conditioning the cash transfer, for example, on TB care access and treatment adherence of TB-affected families may not only be impractical, but also unethical if TB services and management capacities are inadequate. In these contexts, while waiting for health systems strengthening, it may be more appropriate to test conditionality on a small scale and only under very specific TB control-related behaviour. Alternatively, conditionality could be completely removed and cash transfer used to reduce TB vulnerability by addressing household food insecurity and material living conditions.
Whereas the evidence provided from the social cash transfer schemes implemented in Zambia and Malawi20-22 seems to demonstrate that conditionality may not be essential to achieve an impact on risk factors increasing TB vulnerability, it is unclear whether changes in TB care-seeking behaviours can be achieved without conditionality, and under which conditions conditionality should be applied to maximise impact.
CONCLUSIONS
The global TB control community is in need of innovative strategies to move towards TB elimination. The experiences reviewed here support the hypothesis that synergies between social protection interventions and TB control programmes could be effective. Nonetheless, several questions remain unanswered, most importantly: how can these partnerships be most cost-effectively implemented, and what would be their actual impact on TB outcomes? While funding to address these important research questions materialises, a preliminary and relatively inexpensive way to move forward would be to undertake proper studies specifically exploring what obstacles limit their integration with TB control programmes and, through the retrospective analysis of existing data, assess any unintentional impact these interventions may already have had on local TB trends.
Although policy recommendations are not possible at this stage, we hope that the evidence and critical considerations here reported will encourage a new generation of socio-economic interventions addressing key TB risk factors and supporting the existing biomedical strategy. Such studies can significantly advance our understanding of the social determinants of TB and inform broader and more effective TB control policies for the future.
Acknowledgements
The authors acknowledge the role of M Petticrew for his useful intellectual contribution to the review protocol during the early stage of the project. DB worked under an ad-hoc WHO contract. Other members of the research team were funded by the Medical Research Council/Economic and Social Research Council, Innovation for Health and Development, the Wellcome Trust, the Foundation for Innovative New Diagnostics and the UK Department for International Development.
Footnotes
Disclaimer: Knut Lönnroth, Ernesto Jaramillo and Mukund Uplekar are staff members of the World Health Organization (WHO). The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions, policy or views of the WHO.
References
- 1.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol. 2001;30:668–677. doi: 10.1093/ije/30.4.668. [DOI] [PubMed] [Google Scholar]
- 2.Szereter S. Economic growth, disruption, deprivation, disease and death: on the importance of the politics of public health for development. Popul Dev Rev. 1997;23:693–728. [Google Scholar]
- 3.Obermeyer Z, Abbott-Klafter J, Murray CJ. Has the DOTS strategy improved case finding or treatment success? An empirical assessment. PLoS ONE. 2008;3:e1721. doi: 10.1371/journal.pone.0001721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dye C, Lonnroth K, Jaramillo E, Williams BG, Raviglione M. Trends in tuberculosis incidence and their determinants in 134 countries. Bull World Health Organ. 2009;87:683–691. doi: 10.2471/BLT.08.058453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lonnroth K, Castro KG, Chakaya JM, et al. Tuberculosis control and elimination 2010–50: cure, care, and social development. Lancet. 2010;375:1814–1829. doi: 10.1016/S0140-6736(10)60483-7. [DOI] [PubMed] [Google Scholar]
- 6.Commission on Social Determinants of Health . A conceptual framework for action on the social determinants of health (draft) World Health Organization; Geneva, Switzerland: [Accessed February 2011]. 2007. http://www.who.int/social_determinants/resources/csdh_framework_action_05_07.pdf. [Google Scholar]
- 7.Adato M. Social protection: opportunity for Africa. IFPRI; Washington DC, USA: 2008. International Food Policy Research Institute policy brief. [Google Scholar]
- 8.Mohindra KS, Haddad S. Evaluating the unintended health consequences of poverty alleviation strategies: or what is the relevance of Mohammed Yunus to public health? Can J Public Health. 2008;99:66–68. doi: 10.1007/BF03403744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pronyk PM, Hargreaves JR, Morduch J. Microfinance programs and better health: prospects for sub-Saharan Africa. JAMA. 2007;298:1925–1927. doi: 10.1001/jama.298.16.1925. [DOI] [PubMed] [Google Scholar]
- 10.Adato M, Bassett L. Social protection in the context of HIV and AIDS: the potential of cash transfers to protect children’s education, health, and nutrition. AIDS Care. 2009;21(Suppl 1):S60–S75. doi: 10.1080/09540120903112351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hargreaves JR, Boccia D, Evans CA, Adato M, Petticrew M, Porter JD. The social determinants of tuberculosis: from evidence to action. Am J Public Health. 2011;101:654–662. doi: 10.2105/AJPH.2010.199505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Food and Agricultural Organization Rome declaration on world food security and World Food Summit plan of action; World Food Summit, 13–17 November, Rome, Italy; Rome, Italy: Food and Agricultural Organization. 1996. [Google Scholar]
- 13.Ogilvie D, Hamilton V, Egan M, Petticrew M. Systematic reviews of health effects of social interventions: 1. Finding the evidence: how far should you go? J Epidemiol Community Health. 2005;59:804–808. doi: 10.1136/jech.2005.034181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arai L, Britten N, Popay J, et al. Testing methodological developments in the conduct of narrative synthesis: a demonstration review of research on the implementation of smoke alarm interventions. Evidence and Policy. 2007;3:361–383. [Google Scholar]
- 15.Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis: final report. Economic and Social Research Council Methods Programme; Swindon, UK: 2006. [Google Scholar]
- 16.Goldberg N. Measuring the impact of microfinance: taking stock of what we know. Grameen Foundation; Washington DC, USA: 2005. [Google Scholar]
- 17.Thim S, Sath S, Sina M, et al. A community-based tuberculosis program in Cambodia. JAMA. 2004;292:566–568. doi: 10.1001/jama.292.5.566-c. [DOI] [PubMed] [Google Scholar]
- 18.Gilligan DO, Hoddinott J, Taffesse AS. An analysis of Ethiopia’s productive safety net program and its linkages. International Food Policy Research Institute; Washington DC, USA: 2008. [Google Scholar]
- 19.Devereux S, Sabates-Wheeler R, Tefera M, Taye H. Ethiopia’s Productive Safety Net Programme (PSNP). Trends in PSNP transfers within targeted households. Final report. Institute of Development Studies and Indak International; Sussex, UK: 2006. [Google Scholar]
- 20.Schüring E. Cashing in: how cash transfers shore up Zambian households affected by HIV. German Technical Cooperation (GTZ); Berlin, Germany: 2009. [Google Scholar]
- 21.Devereux S, Mthinda C, Power F, Sakala P, Suka A. An evaluation of Concern Worldwide’s Dowa Emergency Cash Transfer project (DECT) in Malawi, 2006/07. Concern Worldwide; Dublin, Ireland: 2007. [Google Scholar]
- 22.Miller C, Tsoka M, Reichert K. Impact evaluation report. External evaluation of the Mchinjii Social Cash Transfer pilot. Centre for International Health and Development; Washington DC USA: 2008. [Google Scholar]
- 23.Thornton RL. Demand for and impact of learning HIV status. American Economic Review. 2008;98:1829–1863. doi: 10.1257/aer.98.5.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gertler PJ, Boyce S. An experiment in incentive-based welfare: the impact of PROGRESA on health in Mexico. University of California, Berkeley; San Francisco, CA, USA: 2001. [Google Scholar]
- 25.Levy D, Ohls J. Evaluation of Jamaica’s PATH program: final report. Mathematica Policy Research, Inc.; Washington DC, USA: 2007. [Google Scholar]
- 26.Powell-Jackson T, Dev Neupane B, Tiwari S, Morrison J, Costello A. Evaluation of the Safe Delivery Incentive Programme. Final report of the evaluation. Support to the Safe Motherhood Programme; Katmandu, Nepal: 2008. [Google Scholar]
- 27.Lim SS, Dandona L, Hoisington JA, et al. India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. Lancet. 2010;375:2009–2023. doi: 10.1016/S0140-6736(10)60744-1. [DOI] [PubMed] [Google Scholar]
- 28.Thornton RL. The demand for and impact of learning HIV status: evidence from a field experiment. AIDSMark; Washington DC, USA: 2006. [Google Scholar]
- 29.Maluccio JA, Flores R. Impact evaluation of a conditional cash transfer program—the Nicaraguan Red de Proteccion Social. International Food Policy Research Institute; Washington DC, USA: 2005. [Google Scholar]
- 30.Hoddinott J, Skoufias E, Washburn R. The impact of PROGRESA on consumption: a final report. International Food Policy Research Institute; Washington DC, USA: 2000. [DOI] [PubMed] [Google Scholar]
- 31.Morris SS, Flores R, Olinto P, Medina JM. Monetary incentives in primary health care and effects on use and coverage of preventive health care interventions in rural Honduras: cluster randomised trial. Lancet. 2004;364:2030–2037. doi: 10.1016/S0140-6736(04)17515-6. [DOI] [PubMed] [Google Scholar]
- 32.Attanasio O, Mesnard A. The impact of conditional cash transfer programme on consumption in Colombia. Institute for Fiscal Studies, Centre for the Evaluation of Development Policies; London, UK: 2005. [Google Scholar]
- 33.Soaeres FV, Perez Ribas R, Osorio RG. Evaluating the impact of Brazil’s Bolsa Familia cash transfer programmes in comparative perspective. Evaluation notes. International Poverty Centre, United Nations Development Programme; Brasilia, Brazil: 2007. [Google Scholar]
- 34.Ahmed AU, Quisumbing R, Hoddinott JF. Relative efficacy of food and cash transfers in improving food security and liveli-hoods of the ultra-poor in Bangladesh. International Food Policy Research Institute; Washington DC, USA: 2007. [Google Scholar]
- 35.Powell-Jackson T, Morrison J, Tiwari S, Neupane BD, Costello AM. The experiences of districts in implementing a national incentive programme to promote safe delivery in Nepal. BMC Health Serv Res. 2009;9:97. doi: 10.1186/1472-6963-9-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schüring E, Boonstoppel E, Michelo S. Final evaluation report: Kalomo Social Cash Transfer Scheme. Ministry of Community Development and Social Services and the German Technical Cooperation; Lusaka, Zambia: 2007. [Google Scholar]
- 37.Tembo G, Freeland N. Impact of social cash transfers on household welfare, investment and education in Zambia. Wahenga; Johannesburg, South Africa: 2009. Wahenga brief number 17, February 2009. [Google Scholar]
- 38.Fiszbein A, Schady N. Conditional cash transfers. Reducing present and future poverty. World Bank; Washington DC, USA: 2009. [Google Scholar]
- 39.Rabbani M, Prakash VA, Sulaiman M. Impact assessment of CFPR/TUP: a descriptive analysis based on 2002–2005 panel data. BRAC, and the Aga Khan Foundation, Canada; Dhaka, Bangladesh: 2006. CFPR/TUP Working Paper series no. 12. [Google Scholar]
- 40.Halder SR. Poverty outreach and BRAC’s microfinance interventions: program impact and sustainability. BRAC; Dhaka, Bangladesh: [Accessed February 2011]. 2010. http://www.bracresearch.org/reports/poverty_outreach_of_brac_mf_interventions_pdf.pdf. [Google Scholar]
- 41.Pronyk PM, Kim JC, Abramsky T, et al. A combined microfinance and training intervention can reduce HIV risk behaviour in young female participants. AIDS. 2008;22:1659–1665. doi: 10.1097/QAD.0b013e328307a040. [DOI] [PubMed] [Google Scholar]
- 42.Pronyk PM, Hargreaves JR, Kim JC, et al. Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet. 2006;368:1973–1983. doi: 10.1016/S0140-6736(06)69744-4. [DOI] [PubMed] [Google Scholar]
- 43.Haseen F. Change in food and nutrient consumption among the ultra poor: is the CFPR/TUP programme making a difference? BRAC; Dhaka, Bangladesh: 2006. CFPR/TUP Working Paper series no. 11. [PubMed] [Google Scholar]
- 44.Haseen F. Change in food and energy consumption among the ultra poor: is the poverty reduction programme making a difference? Asia Pac J Clin Nutr. 2007;16(Suppl 1):S58–S64. [PubMed] [Google Scholar]
- 45.Ahmed SM. Combining health and social protection measures to reach the ultra-poor: experiences of BRAC. In: Matlin SA, editor. Global Forum update on research for health, Volume 4. Equitable access: research challenges for health in developing countries. Pro-Brook Publishing; London, UK: 2007. [Google Scholar]
- 46.Halder SR, Mosley P. Working with the extra-poor: learning from BRAC experiences. J Int Dev. 2004;16:387–406. [Google Scholar]
- 47.Hashemi S. Linking microfinance and safety net programs to include the poorest: the case of IGVGD in Bangladesh. Consultative Group to Assist the Poor; Washington DC, USA: 2001. Focus Note series 21. [Google Scholar]
- 48.Mohindra K, Haddad S, Narayana D. Can microcredit help improve the health of poor women? Some findings from a cross-sectional study in Kerala, India. Int J Equity Health. 2008;7:2. doi: 10.1186/1475-9276-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Maluccio JA. The impact of conditional cash transfers in Nicaragua on consumption, productive investments and labor allocation. Food and Agricultural Organization; Rome, Italy: 2007. ESA Working Paper no. 07-11. [Google Scholar]
- 50.Ruel MT. Is dietary diversity an indicator of food security or dietary quality? A review of measurement issues and research needs. International Food Policy Research Institute; Washington DC, USA: 2003. FCND Discussion Paper no. 140. [DOI] [PubMed] [Google Scholar]
- 51.Doocy S, Teferra S, Norell D, Burnham G. Credit program outcomes: coping capacity and nutritional status in the food insecure context of Ethiopia. Soc Sci Med. 2005;60:2371–2382. doi: 10.1016/j.socscimed.2004.10.025. [DOI] [PubMed] [Google Scholar]
- 52.Attanasio O, Battistin E, Fitzsimons E, Mesnard A, Vera-Hernandez M. How effective are conditional cash transfers? Evidence from Colombia. Institute for Fiscal Studies; London, UK: Briefing Note no. 54. [Google Scholar]
- 53.Barber SL, Gertler PJ. Empowering women to obtain high quality care: evidence from an evaluation of Mexico’s conditional cash transfer programme. Health Policy Plan. 2009;24:18–25. doi: 10.1093/heapol/czn039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ahmed SM, Petzold M, Kabir ZN, Tomson G. Targeted intervention for the ultra poor in rural Bangladesh: does it make any difference in their health-seeking behaviour? Soc Sci Med. 2006;63:2899–2911. doi: 10.1016/j.socscimed.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 55.Ahmed SM, Adams AM, Chowdhury M, Bhuiya A. Changing health-seeking behaviour in Matlab, Bangladesh: do development interventions matter? Health Policy Plan. 2003;18:306–315. doi: 10.1093/heapol/czg037. [DOI] [PubMed] [Google Scholar]
- 56.Fernald LC, Gertler PJ, Hou X. Cash component of conditional cash transfer program is associated with higher body mass index and blood pressure in adults. J Nutr. 2008;138:2250–2257. doi: 10.3945/jn.108.090506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ahmed SM, Rana Masud AKM. Customized development interventions for the ultra poor: preliminary changes assessment of health and health seeking behaviour (CFPR/TUP 2002 to 2004) BRAC; Dhaka, Bangladesh: 2005. CFPR/TUP Working Paper series no. 7. [Google Scholar]
- 58.Harpham T, Burton S, Blue I. Healthy city projects in developing countries: the first evaluation. Health Promot Int. 2001;16:111–125. doi: 10.1093/heapro/16.2.111. [DOI] [PubMed] [Google Scholar]
- 59.Cegielski JP, McMurray DN. The relationship between malnutrition and tuberculosis: evidence from studies in humans and experimental animals. Int J Tuberc Lung Dis. 2004;8:286–298. [PubMed] [Google Scholar]
- 60.Bond V, Chileche M, Sullivan C, Magazi B. The converging impact of tuberculosis, HIV/AIDS, and food insecurity in Zambia and South Africa. Final working report, February 2009. Regional Network on HIV/AIDS, Livelihoods, and Food Security (RENEWAL); Johannesburg, South Africa: [Accessed February 2011]. 2009. http://programs.ifpri.org/renewal/pdf/ZambiaSAFinalReport.pdf. [Google Scholar]
- 61.MkNelly B, Dunford C. Are credit and savings services effective against hunger and malnutriution? Freedom from hunger; Davis, CA, USA: 1996. Research paper no. 1. [Google Scholar]
- 62.Hoddinott J, Skoufias E. The impact of PROGRESA on food consumption. Economic Development and Cultural Change. 2004;53:37–61. [Google Scholar]
- 63.Hargreaves J, Hatcher A, Strange V, et al. Process evaluation of the Intervention with Microfinance for AIDS and Gender Equity (IMAGE) in rural South Africa. Health Educ Res. 2009;25:27–40. doi: 10.1093/her/cyp054. [DOI] [PubMed] [Google Scholar]
- 64.Datta D, Njuguna J. Microcredit for people affected by HIV and AIDS: insights from Kenya. SAHARA J. 2008;5:94–102. doi: 10.1080/17290376.2008.9724906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kim J, MacPherson E, Pronyk P, Barnett T, Watts C. Global review of good practices on the intersections between HIV/AIDS and economic empowerment. Final report (draft) Ford Foundation; New York, NY, USA: [Accessed February 2011]. 2009. http://genderviolence.lshtm.ac.uk/files/FF_Final_Report_Addressing_Intersections_Between_Economic_Empowerment_and_AIDS.pdf. [Google Scholar]
- 66.Adato M, Bassett L. What is the potential of cash transfer to strengthen families affected by HIV and AIDS? Review of the evidence on impacts and key policy debates. IFPRI policy brief. International Food Policy Research Institute; Washington DC, USA: 2008. [Google Scholar]
- 67.Consultative Group to Assist the Poor . No. 14 Donor Brief: helping to improve donor effectiveness in microfinance. CGAP; Washington DC, USA: 2003. [Google Scholar]
- 68.de Janvry A, Sadoulet E. When to use a CCT versus a CT approach?; Third International Conference on Conditional Transfers, Turkey, Istanbul; Berkley, CA, USA: University of California and The World Bank’s Development Research Group. July 26–30, 2006; 2006. Conference paper. [Google Scholar]
- 69.Schubert B, Slater R. Social cash transfers in low income African countries: conditional or unconditional? Development Policy Review. 2006;24:571–578. [Google Scholar]