Abstract
Context: In the United States, more than a third of patients are referred to a specialist each year, and specialist visits constitute more than half of outpatient visits. Despite the frequency of referrals and the importance of the specialty-referral process, the process itself has been a long-standing source of frustration among both primary care physicians (PCPs) and specialists. These frustrations, along with a desire to lower costs, have led to numerous strategies to improve the specialty-referral process, such as using gatekeepers and referral guidelines.
Methods: This article reviews the literature on the specialty-referral process in order to better understand what is known about current problems with the referral process and what solutions have been proposed. The article first provides a conceptual framework and then reviews prior literature on the referral decision, care coordination including information transfer, and access to specialty care.
Findings: PCPs vary in their threshold for referring a patient, which results in both the underuse and the overuse of specialists. Many referrals do not include a transfer of information, either to or from the specialist; and when they do, it often contains insufficient data for medical decision making. Care across the primary-specialty interface is poorly integrated; PCPs often do not know whether a patient actually went to the specialist, or what the specialist recommended. PCPs and specialists also frequently disagree on the specialist's role during the referral episode (e.g., single consultation or continuing co-management).
Conclusions: There are breakdowns and inefficiencies in all components of the specialty-referral process. Despite many promising mechanisms to improve the referral process, rigorous evaluations of these improvements are needed.
Keywords: Medical specialties, referral and consultation, review
Referrals are the link between primary and specialty care. In the nonelderly population, about one in three patients each year is referred to a specialist (Forrest, Majeed, et al. 2002), and among the elderly, on average two referrals are made per person per year (Shea et al. 1999). Visits to specialists constitute more than half of outpatient physician visits in the United States (Machlin and Carper 2007). In their area of expertise, specialists are more likely than primary care physicians (PCPs) to provide evidence-based care, and several studies have shown that specialists’ co-management of care with PCPs results in better health outcomes for patients with chronic diseases (Ayanian et al. 2002; Lafata et al. 2001; Willison et al. 1998).
Despite the frequency of referrals and the importance of the specialty-referral process, the process itself has been a long-standing source of frustration among physicians. In 1964 the specialty-referral process was described as “often incomplete and needlessly inefficient” (Kunkle 1964, 103). In 1983 it was said that the process “often falls short of its goals” (Lee, Pappius, and Goldman 1983, 111). In 2000 it was described as a system that is “not consciously designed and leaves much to be desired” (Gandhi et al. 2000, 629), and in 2008 it was cited as a prominent aspect of a patient's “perilous journey through the health care system” (Bodenheimer 2008, 1064).
These frustrations—along with a desire to decrease costs stemming from perceived inefficient use of resources by specialists—have led to numerous strategies to improve the specialty-referral process. Managed care's “gatekeeper” authorization for referrals to specialists is perhaps the best known of these strategies. But patients’ and physicians’ frustration, along with a lack of empirical support for gatekeeping (Ferris et al. 2001; Forrest et al. 2001), has led to interest in several newer approaches. In most medical home pilot programs, practices have a financial incentive to track referrals and to provide decision support for referral decisions (Bitton, Martin, and Landon 2010; CMS 2009). Referral guidelines also have been promoted as a means of improving the appropriateness of referrals (Bodenheimer 2008). Surveys of patients’ experiences, which are used for pay-for-performance incentives, now ask patients to evaluate the coordination of care between PCPs and specialists (Rodriguez et al. 2009). Among the advantages of electronic medical records and bundled (“episode-based”) payments is that they might improve communication and care coordination related to referrals (RAND 2009).
What evidence do we have that the specialty-referral process needs to be changed? Do current improvement strategies, such as the medical home and bundled payments, address the known deficiencies in the specialty-referral process? In this article, we first discuss the key components of the referral process. We then present a comprehensive literature review of the specialty-referral process in the United States, specifically addressing: (1) referral decision making; (2) care coordination, including information transfer and integration of care; and (3) entry into specialty care. The goal of our review is to summarize what is known about deficiencies in the referral process and to identify opportunities for improvement.
The Specialty-Referral Process: A Conceptual Framework
Although numerous papers have examined the specialty-referral process, they do not clearly define the specialty referral or what it constitutes. Our model is built on the work by Forrest (2009) and Haggerty and colleagues (2003). A specialty referral is the interface between the referring provider and the specialist. While the referring provider can be any type of provider, the focus in the literature has been on PCPs. For simplicity, we maintain this focus on PCPs, but the model also applies when specialists initiate the referral, which is sometimes called a cross-referral. The need for a referral assumes that the PCP and the specialist are in separate practices. As we point out, the need for a specialty referral is less clear when care is provided by a multispecialty team at a single practice (e.g., visits with both a PCP and an endocrinologist for patients with diabetes).
What information needs to be transferred across the interface depends on the goal of the referral. While there currently is no normative role for specialists, Forrest created a typology to help define responsibilities in order of specialists’ increasing responsibility: cognitive consultant (e.g., input on unclear diagnosis), procedural consultant (e.g., referral for colonoscopy), co-manager sharing the care of a specific problem (e.g., heart failure), and co-manager when a specialist becomes the principal caregiver for a specific problem or when a specialist becomes the primary caregiver (e.g., nephrologists commonly serve this role for patients with end-stage renal disease) (Forrest 2009). The distinctions among different types of specialist roles, however, are rarely addressed in the published literature on referrals.
The referral itself is the formal mechanism by which a relationship is established between two providers who care for the same patient and is intended to satisfy the specific purpose based on the typology just defined (e.g., the specialist provides cognitive input on how best to evaluate or manage a health issue or provides the principal care for a specific health issue such as heart failure). Our conceptual framework for the referral process from primary to specialty care (shown in Figure 1) divides the process into three components: referral decision making, care coordination, and access to a specialist.
Figure 1.
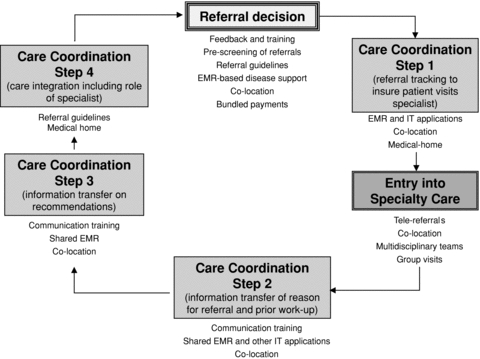
Idealized steps in specialty-referral process and potential mechanisms for improvement at each step.
Notes: EMR = electronic medical record; IT = information technology.
The referral process begins with the PCP's decision to refer a patient to a specialist: referral decision making. Ideally, the decision to refer should be appropriate (e.g., the question being addressed is outside the PCP's typical scope of care or the patient needs a procedure that PCPs do not typically perform), and the correct specialist has been identified to help evaluate or manage the condition. Once the referral has been initiated, the PCP should coordinate care by tracking the referral and ensuring that it is carried out. The patient also must be able to obtain an appointment with a specialist, or specialty access. The process then requires a transfer of relevant information, including earlier workup such as laboratory and imaging results, to the specialist. After the specialist's evaluation, along with diagnostic and therapeutic interventions (specialist care), there again is an information transfer of findings and follow-up recommendations from the specialist to the PCP and the patient. Another key step is care integration, which means that the PCP and specialist agree on the management plan and the role of the specialist. We believe that care coordination encompasses several key aspects of the specialty-referral process: information transfer, tracking of referrals, and care integration. Although we have described a clean linear process of specialty referral, we recognize that these components often take place nonlinearly.
In the ideal situation, the entire process works seamlessly for both providers and patients. Haggerty and colleagues described a typology of continuity of care relevant to the referral process (Haggerty et al. 2003). According to their model, the domains of continuity are information continuity, management continuity, and relational continuity. For a specialty referral, information continuity might be simplified as the transfer of “facts” (e.g., earlier tests, list of medications, reason for consultation). From the patient's perspective, management continuity is a coherent approach to managing a condition. With a specialty referral, we want the patient to understand that the referring physician and specialist are “on the same page.” Relational continuity describes the ongoing therapeutic relationship between the patient and the provider(s), and it is enhanced by information and management continuity, which together can establish the trust necessary in a therapeutic relationship.
The literature we describe generally focuses on information continuity, or whether there was communication about the reason for consultation and earlier workup. Management continuity improves with information continuity, but it also requires the other aspects of care coordination. In particular, a patient will perceive management continuity if there is referral tracking (the referring physician ensures that the patient visited the specialist) and care integration (both the PCP and the specialist agree on the management plan and their respective roles in it).
Methods
We chose to conduct a narrative review, as opposed to a systematic review, because of the breadth of topics and issues addressed (Collins and Fauser 2005). To inform our review we searched five databases (MEDLINE, CINAHL, LocatorPlus, NLM Gateway, and PsycINFO) for relevant articles between January 1970 and January 2009, in the English language, using the search terms referral and consultation, physician practice patterns, specialist, referral decision, referral process, variation, appropriate, inappropriate, and communication. Two of us (Mehrotra and Lin) examined all the titles and abstracts to the relevant articles. We concentrated on referrals to specialist physicians for input on diagnosis or management but chose not to address referrals for radiology/pathology services, hospice, postacute care, dental care, specific procedures (e.g., endoscopies), immunizations, disability evaluation/occupational medicine, physical and/or occupational therapy, alternative/complementary medicine, clinical trials, and anticoagulation clinics. We also excluded studies conducted in practices outside the United States, as the practice context and payment methods in other countries are different.
Results
What Is Known about Referral Decision Making (frequency, appropriateness, and timeliness of referrals)?
The three main actors in referral decision making are the referring provider, the specialist, and the patient. Much of the existing literature centers on referral decision making by PCPs, recognizing their responsibility to decide to refer and to match the appropriate type and level of specialty service to the patient's needs. Patients typically want their PCP to play this role (Grumbach et al. 1999). In contrast, both the specialist's decision to refer to another specialist and the patient's decision to seek a specialist's care without a referral are relatively understudied.
Variation in Referrals
The decision to refer varies widely, with some PCPs making more than five times as many referrals per patient or per visit as others do (Borowsky et al. 1997; Calman, Hyman, and Licht 1992; Chen, Fryer, and Norris 2005; Forrest et al. 1999; Franks et al. 1999). A physician's referral rate—that is, the “referral threshold”—tends to be stable from year to year and across diagnostic categories (Franks et al. 1999). The types of specialists to which PCPs refer patients with a given condition also varies significantly (e.g., type of surgeon or surgical versus medical specialist) (Forrest, Nutting, et al. 2002; Starfield et al. 2002).
What accounts for the variation in PCPs’ referral decisions? Much of it is associated with factors related to the patient, such as the nature of the presenting problem, the patient's expectations, and the burden of morbidity (Chen, Fryer, and Norris 2005; Forrest et al. 2006; Lin et al. 2000; Moore and Roland 1989; Shea et al. 1999). A substantial amount of the variation also is attributable to the provider's characteristics, including type of training (e.g., any specialist training) (Bachman and Freeborn 1999; Boulis and Long 2002; Chen 2001; Everett, Parsons, and Christensen 1984; Lawler 1987), number of years of experience (Bachman and Freeborn 1999; Everett, Parsons, and Christensen 1984), experience with the condition at hand (Forrest and Reid 2001), and certainty in diagnosis (Calman, Hyman, and Licht 1992). To a smaller degree, referrals also are influenced by the provider's “practice style,” as represented by the degree of risk aversion (Forrest et al. 2006), technical orientation of care (Bertakis et al. 2001), and concerns about malpractice suits (Franks et al. 2000), as well as the provider's practice environment (Chen, Fryer, and Norris 2005). The specialist's characteristics, such as his or her perceived medical skill, prior interactions, availability, and whether the specialist is known to return the patient to the referring physician also influence which specialist is chosen (Kinchen et al. 2004). The community in which the provider practices helps determine decisions to refer. For example, referrals are made more frequently by urban physicians than by rural physicians (Iverson et al. 2005) and in environments with more physicians per capita (Shea et al. 1999). Although these various factors together explain some of the variation, we believe much of the variation likely reflects physicians’ idiosyncratic practice styles.
Few studies have evaluated variations in those situations when a patient visits a specialist without a referral or one specialist refers the patient to another specialist. Up to 50 percent of new visits to a specialist represent situations in which the patient scheduled an appointment without a referral (Forrest and Reid 1997), although these rates differ significantly by type of specialist. More “self-referrals” are associated with dissatisfaction and poorer continuity of care with the PCP (Forrest et al. 2001). One study of specialists’ cross-referrals showed that they are uncommon, accounting for only about 3 percent of referrals (Forrest and Reid 1997).
Appropriateness of Referrals
While many studies focus on the variation in referral decisions, relatively few delve into the appropriateness of the referrals and whether the observed variation in referral rates is due to overreferral, underreferral, or both. A key issue is defining appropriateness. Three general methods have been used to define the appropriateness of referrals: (1) adherence to existing guidelines or predefined research criteria; (2) judgment by the provider making the referral, the specialist receiving the referral, or an external expert not involved in the patient's care; and (3) whether the referral results in a change in diagnosis or management. Some studies have used dichotomous outcomes (appropriate versus inappropriate), and others have used scales (e.g., appropriateness scored from 1 to 10). Studies use different terms to describe the same phenomenon (e.g., appropriate, indicated, nondiscretionary, mandatory, necessary, and nonelective); we use the word appropriate to encompass all these terms.
We found sixteen articles that determined the rate of PCP-appropriate referrals that use any of the three methods: nine addressed overreferrals, and seven addressed underreferrals (see Tables 1 and 2, respectively). The overreferral studies calculated the percentage of inappropriate referrals, which ranged from 0.7 percent (children with developmental disabilities inappropriately referred to developmental specialists) (Wallerstein and Seshadri 1994) to 65 percent (children with musculoskeletal disorders inappropriately referred to pediatric orthopedists) (Reeder et al. 2004). The underreferral studies determined what percentage of patients who should have been referred were not referred, which ranged from 19 percent (for patients who had stage III or IV colorectal cancer and were not referred to medical oncologists for adjuvant therapy) (Oliveria et al. 2004) to 87 percent (for patients with diabetes or hypertension who were not referred to ophthalmologists for retinopathy screening) (Ettinger, Schwartz, and Kalet 1993). We should emphasize that these two types of studies looked at different groups of patients. The overreferral studies examined a population of patients who were referred, and the underreferral studies examined a population of patients who had a particular illness.
Table 1.
Published Studies on Inappropriate Referrals (overreferrals)
| Study | Inappropriate Referrals (%) | Condition(s) | Term Used to Define Inappropriate | Definition of Inappropriate |
|---|---|---|---|---|
| Lawler et al. 1990 | 19.2 | All conditions | Elective | Judgment of external expert (scale of 1 to 4, 4 being extremely unlikely to suffer harm without referral and could be managed by PCP). |
| Donohoe et al. 1999 | 30 | All conditions | Inappropriate | Judgment of specialist physician (scale of 1 to 9 scale, 1 being “highly inappropriate”; 9 being “highly appropriate”). |
| Albertson et al. 2000 | 17.4 | All conditions | Not indicated | Judgment of referring physician (e.g., comfortable treating, patient seeking additional reassurance not indicated). |
| Harrington and Walsh 2001 | 41 | Rheumatology | Inappropriate | Judgment of specialist receiving referral (e.g., already receiving appropriate care, no autoimmune symptoms, prior complete evaluation, no prior evaluation by referring physician). |
| Wallerstein and Seshadri 1994 | 0.7 | Pediatric developmental disability | Unnecessary | Judgment of specialist receiving referral (no evidence of chronic developmental disability and no need for further testing or services). |
| Forrest et al. 2003 | 12.4 | All conditions | Discretionary | Four predefined criteria: common condition, high certainty, low urgency, cognitive assistance only. |
| Forrest et al. 2006 | 17 | All conditions | Discretionary | Four predefined criteria: common condition, high certainty, low urgency, cognitive assistance only. |
| Warren 1994 | 16 | Strabismus | Inappropriate, invalid, excessive | Change in management (excessive referrals when >30% of referrals for strabismus are not found to have strabismus). |
| Reeder et al. 2004 | 42–65 | Pediatric musculoskeletal disorders | Inappropriate | Guidelines (2002 AAP Surgical Advisory Panel guidelines for referral to surgical subspecialties). |
Note: Limited to studies published in the United States.
Table 2.
Published Studies on Patients Not Appropriately Referred (underreferrals)
| Study | Patients with Condition Not Appropriately Referred (%) | Condition(s) | Term Used to Define Appropriate | Definition of Appropriate |
|---|---|---|---|---|
| Avidor et al. 2007 | 85 | Morbid obesity | Indicated | Guidelines (2000 National Institute of Health guidelines indicate patients with BMI > = 40 or > = 35 with significant comorbidity should be referred for bariatric surgery evaluation). |
| Ettinger, Schwartz, and Kalet 1993 | 87 | Diabetes or hypertension | Appropriate | Guidelines (ophthalmology and optometry guidelines indicate that patients with hypertension and diabetes should be screened yearly). |
| Finkelstein et al. 2000 | 1–60a | Pediatric asthma | Indicated | Guidelines (1997 NAEPP guidelines indicate referral for patients with severe persistent asthma, poor response to therapy after 3 to 6 months, life-threatening asthma episode, and others). |
| Marrero et al. 1995 | 64 | Pregnant women with diabetes | Appropriate | Guidelines (ADA and AAO guidelines indicate all pregnant women with diabetes should get first-trimester screening). |
| Oliveria et al. 2004 | 13–33a | Colorectal cancer | Appropriate | Guidelines (1990 NCI guidelines: Stages III and IV should be referred to oncologist for consideration of adjuvant therapy). |
| Steckler et al. 1995 | 70 (family practice), 86 (pediatrics) | Children with undescended testis | Indicated | Guidelines (urologic specialty guidelines indicate children should be referred before 1 year of age). |
| Swarztrauber, Vickrey, and Mittman 2002 | 53–80a | TIA, dementia, Parkinson's disease | No specific term | Expert judgment (neurologists and PCPs presented with a number of case scenarios. Neurologists preferred referral at a higher rate for all case scenarios. Percentage reported is difference between the fraction of referrals reported by PCPs and neurologists). |
Note: Limited to studies published in United States.
Study looked at a number of indications for referral. Range represents fraction across these different indications.
Only one study compared physicians with high referral rates with those with low referral rates, and it found a larger percentage of inappropriate referrals among the high-referring physicians (Warren 1994).
Timeliness of Referral
Late referrals to nephrologists for patients with chronic kidney disease have been the subject of numerous studies and the topic of a previous review (Navaneethan, Aloudat, and Singh 2008). Late referrals have been associated with worse health outcomes in this patient population. The studies indicated that from 15 to 80 percent of these patients were referred late, due to a variety of patient characteristics (e.g., age, race, gender, insurance status), as well as factors related to providers, health systems, and environments (e.g., type of referring provider, type of referring center, distance to dialysis center) (Navaneethan, Aloudat, and Singh 2008).
What Is Known about Care Coordination between Primary Care and Specialist Physicians (referral tracking, information transfer, care integration)?
Referral Tracking
Referral tracking is an important task for the referring provider to ensure that the referral was completed. Studies have found that 25 to 50 percent of referring physicians did not know whether their patients had actually seen the specialist to which they were referred (Bourguet, Gilchrist, and McCord 1998; Byrd and Moskowitz 1987) and that physicians both overestimated and underestimated the number of referrals completed (Forrest et al. 2007). Poor referral tracking leads to inappropriate re-referrals, inefficient care, worse patient satisfaction, and malpractice lawsuits (Gandhi et al. 2006).
Information Transfer
Even though all physicians highly value communication between referring providers and specialists (Linzer et al. 2006), both PCPs and specialists cite the lack of effective information transfer as one of the greatest problems in the referral process (Gandhi et al. 2000). We identified six studies that assessed the adequacy of information transfer (Table 3). Typically, in more than half the referrals, the referring provider had no communication with the specialist (Bourguet, Gilchrist, and McCord 1998; Gandhi et al. 2000; Stille et al. 2006). Similarly, up to 45 percent of referrals resulted in no communication from the specialist back to the referring provider (Bourguet, Gilchrist, and McCord 1998; Byrd and Moskowitz 1987; Gandhi et al. 2000; McPhee et al. 1984; Stille et al. 2006). Problems with information transfer are borne out in patient surveys. For example, approximately one-quarter of U.S. patients reported that the results and records from one provider did not reach another provider in time for their appointment (Blendon et al. 2003; Schoen et al. 2009).
Table 3.
Fraction of Referrals with No Communication between Referring Physician and Specialist
| Study | No Communication from Referring Physician to Specialist (% of referrals) | No Communication from Specialist to Referring Physician (% of referrals) |
|---|---|---|
| Kunkle 1964 | 28 | N.A.a |
| McPhee et al. 1984 | N.A.b | 45c |
| Byrd and Moskowitz 1987 | N.A.b | 19.5 |
| Bourguet, Gilchrist, and McCord 1998 | 54 | 45 |
| Gandhi et al. 2000 | 68 | 25 |
| Stille et al. 2006 | 50 | 4 |
Notes:
Response rate not reported in results.
Referrals were identified by filled-out referral form and therefore cannot indicate when referral form was not filled out.
Communication from specialist was self-reported by referring physician. A note from the specialist was in the chart, but referring physician did not know this.
The information, if sent, is frequently sent late. In one study, 25 percent of letters from specialists were not timely enough to “affect decisions” (McPhee et al. 1984). Gandhi and colleagues noted that at an academic institution with a shared electronic medical record, specialists failed to provide letters within seven days of a referral in 36 percent of cases (Gandhi et al. 2000). They also noted that 50 percent of referring physicians were dissatisfied with the timeliness of specialists’ feedback (Gandhi et al. 2000).
In addition to timeliness, there is the issue of adequacy of communication. Specialists believed that the inadequate content of referral letters commonly caused problems in the referral process (Gandhi et al. 2000); the specialists were not always sure why a patient was referred (McPhee et al. 1984); the specialists and the referring physicians disagreed on the reason for referral in 14 percent of cases involving inpatients (Lee, Pappius, and Goldman 1983); and 70 percent of the specialists rated the background information they usually received as fair or poor (Tanielian et al. 2000). Inadequate communication from specialists also is an issue. In one study, more than half the referring physicians needed more feedback information than was provided by the specialist (Williams et al. 2005), and in another, the referring physician was dissatisfied with the feedback in 17 percent of cases (Byrd and Moskowitz 1987).
Care Integration
As we noted in our conceptual model, there often is miscommunication about the role of the specialist. Specialists may play one of five different roles, as a cognitive consultant (e.g., input on unclear diagnosis), procedural consultant (e.g., referral for colonoscopy), co-manager sharing care of a specific problem, co-manager when the specialist becomes the principal caregiver for a given problem, or co-manager when the specialist becomes the primary caregiver (Forrest 2009). Each of these roles is associated with different responsibilities and intensity of involvement. Nonetheless, PCPs and specialists rarely discuss the preferred role for a referral and who will be responsible for what aspects of care (e.g., follow-up on tests). Studies have found significant disagreement between PCPs and specialists over whether there should be co-management by the PCP and specialist, whether the specialist should become the primary provider, or whether a single consultation from the specialist is sufficient (Salerno et al. 2007; Williams et al. 2005; Williams and Peet 1994). This lack of communication likely contributes to the fact that half of visits to specialists in the United States are for follow-up care for patients already known to the specialist (Valderas et al. 2009). Moreover, referring providers frequently express frustration when a specialist makes a secondary referral to another provider without consulting with them (Williams and Peet 1994).
Management continuity is best judged by the patient. Although patients want their PCPs and specialists to understand and agree on the management plan, this frequently does not happen (Schoen et al. 2009). One survey found that 26 percent of U.S. patients reported receiving conflicting information from different providers (Blendon et al. 2003). In another survey, patients were asked whether their PCP was informed and up to date with the care that they received from a specialist, to which 46 percent said always, 31 percent said usually/almost-always, and 24 percent said never/almost-never/sometimes (O’Malley and Cunningham 2009).
What Is Known about Access to Specialty Care?
A successful referral requires that the patient have adequate access to specialists. Access may be inadequate because there is no specialist in the community or the specialist does not accept the patient's insurance. Access to timely specialist care has been cited as a growing problem, especially in underserved populations (Cook et al. 2007; Ferrer 2007; Institute for Healthcare Improvement 2008; Mayer 2007; Weissman et al. 2003). In turn, poor access has been associated with worse health outcomes (Harrold, Field, and Gurwitz 1999; Landon et al. 2005; Wu et al. 2001). Access issues are not limited to specialty care, however. The lack of timely access to primary care in the United States (Mehrotra, Keehl-Markowitz, and Ayanian 2008; Murray 2002; Murray and Berwick 2003; Strunk and Cunningham 2002) also contributes to problems with the specialty-referral process. One study found that patients’ self-referrals were driven by poor access to primary care (Forrest et al. 2001). Moreover, the burden of primary care—with visits getting shorter for patients with a complex variety of preventive and chronic care needs—makes it difficult for PCPs to provide optimal “first contact” care (Bodenheimer 2008). This burden likely limits PCPs’ ability to make appropriate referrals and, indeed, may promote overreferral.
Adverse Consequences of Deficiencies in the Specialty-Referral Process
These deficiencies in the referral process have many adverse consequences, including reduced continuity of care, delayed diagnosis or treatment, duplication of testing, polypharmacy, and increased risk of malpractice suits (Epstein 1995; Gandhi et al. 2006; Lee, Pappius, and Goldman 1983; Williams and Peet 1994). In one study, more than 50 percent of specialists reported that poor communication hampered their ability to provide adequate care (Stille et al. 2006). In another, PCPs reported that 19 percent of referrals were “repeat referrals” because the problem was not adequately addressed by the first referral (Gandhi et al. 2000). Because of deficient communication between providers, either patients or family members, by default, become information intermediaries. Thirty-eight percent of parents of pediatric patients noted that they had to act as the agent for information transfer, and the majority of them were uncomfortable in this role (Stille et al. 2007). Furthermore, referral visits often lead to a cascade of testing, follow-up testing, and hospitalizations (Glenn, Lawler, and Hoerl 1987). Because specialists tend to use more resources than PCPs do (Greenfield et al. 1992), there is concern that the overuse of referrals wastes resources and unnecessarily drives up costs. Twenty percent of malpractice claims for missed or delayed diagnoses involved communication deficits in handoffs; 17 percent involved the failure to establish clear lines of responsibility; and 5 percent involved the failure of a requested referral to be made (Gandhi et al. 2006).
Strategies for Improving the Specialty-Referral Process
Two systematic reviews have addressed the impact of specific interventions on specialty referrals (Akbari et al. 2005; Faulkner et al. 2003) and strategies to improve the specialty-referral process (Figure 1). Here, we discuss some of the proposed mechanisms to improve the referral process and our own observations on their possible impact.
Decision Making
In general, physicians are unaware of how they compare with their peers in regard to referral rates, and they receive little training or guidance on when to make a referral (Epstein 1995; McPhee et al. 1984; Saunders 1978). While providing feedback to providers, improving training, or holding regular meetings between providers might help decision making, these are unlikely to be effective in changing referral patterns (Akbari et al. 2005; Faulkner et al. 2003; Fung et al. 2008; Grimshaw et al. 2005; Vierhout et al. 1995).
We believe that referral guidelines can provide an important foundation for improving the referral process. Referral guidelines seek to formalize and clarify those aspects of the referral process on which there is disagreement (Chen and Yee 2009), including which conditions should be managed by specialists or PCPs (St Peter et al. 1999), what type of referral should be made (co-management or consultation), what type of communication is preferred by the referring and specialist physicians before and after a referral (written, verbal, or both) (Williams and Peet 1994), and what tests should be ordered before a referral (Bodenheimer 2008). Specialty societies already offer many guidelines (Avidor et al. 2007; Ettinger, Schwartz, and Kalet 1993; Finkelstein 1998; Im et al. 2005; Marrero et al. 1995; Oliveria et al. 2004; Steckler et al. 1995). The number of guidelines that need to be created might be limited, since only a few conditions account for more than three-quarters of all visits to specialists (Forrest et al. 1999).
We caution, however, that guidelines alone will have little impact (Akbari et al. 2005; Shaw et al. 2005) unless they are developed together by generalist and specialist physicians (Akbari et al. 2005; Fertig et al. 1993; Hongsermeier and Mitus 1997; Mostert, Richardus, and de Man 2004; Murray 2002; Safran et al. 1995), are linked to checklists or structured referral forms, or are made part of an electronic medical record. As in other quality improvement work, mechanisms that make it easier for (or force) providers to use the guidelines are more successful. Consistent with our emphasis on the appropriateness of referrals, embedded guidelines may reduce the overuse of some types of specialty visits (Garrido et al. 2005), although they may increase the number of referrals for conditions that are generally underreferred (Safran et al. 1995).
One intriguing possibility is to have specialists regularly prescreen referrals (e.g., using an e-referral communication system) to detect those that are unnecessary, triage referrals to a more appropriate specialist if necessary, or suggest tests before the consultation (Harrington, Dopf, and Chalgren 2001; Harrington and Walsh 2001; Kim et al. 2009; Kim-Hwang et al. 2010; Speed and Crisp 2005). In one study, just one in ten patients whose referrals were screened needed a face-to-face visit (Bergus et al. 2006). Such screening methods can help address clinical scenarios outside the guidelines and reduce unnecessary visits to specialists (Kim-Hwang et al. 2010). Current payment methods, however, do not support such e-referrals in typical fee-for-service settings.
We believe that improvements in the specialty referral process must be spurred by changes in payment systems. Currently, specialists must physically see the patient and bill for a separate visit in order to receive payment. Bundled, or “episode-based,” payments have been proposed by health policy experts as a means of reducing the number of inappropriate referrals (Hackbarth, Reischauer, and Mutti 2008; RAND 2009). Under this payment approach, payments are bundled across providers within organizations that share care for a specific “episode of care” or illness. Like capitation (Davidson et al. 1992), the premise is that such a payment method might discourage unnecessary referrals because the organization receiving the payment will bear the costs of those referrals. Also, without a financial reason for specialists to physically see the patient, novel methods of consultation (e.g., electronic referrals) might be more possible. We should note, though, that if bundled payments become more common, underreferring could become a problem.
Information Transfer
Although providers want good communication and know what information should be included with regard to referrals (Williams and Peet 1994), our review found that time and logistical barriers hinder communicating and providing sufficient data (Epstein 1995; Gandhi et al. 2000).
As we noted earlier, guidelines have been promoted as a way to clarify what information should be transferred and what role the specialist should play after the patient's visit. Information technology can ease the transfer of data (Epstein 1995; Gandhi et al. 2000). One study found an elevenfold increase in the odds of adequate communication between PCPs and specialists sharing an electronic medical record (Stille et al. 2006).
Referral Tracking and Care Integration
Technology has been used as well to improve some aspects of care coordination, including scheduling and completion. Web-based referral systems have improved scheduling for specialty consultation visits, reduced wait times, and reduced the number of unnecessary re-referrals (Weiner et al. 2009). In addition, guidelines can help with care coordination by clarifying the roles of the specialist and the referring physician when referrals are made.
But as we have discussed above, care coordination encompasses much more than tracking and facilitating a specialist referral. The movement toward the patient-centered medical home can improve access to primary care, which in turn might prevent the need for a specialty referral (CMS 2009). Also, the hope is that in using the medical home model, PCPs will spend more time on integrating care. Unfortunately, though, some early evaluations of medical home pilots have not shown significant improvement in care coordination (Jaen et al. 2010), but other demonstration projects are still being evaluated.
Eliminating the Need for a “Referral”
A specialty referral implies two separate systems of care between which a transfer is needed. Although there always is likely to be some need for referrals, changes such as co-location and group visits may eliminate that need, as in these systems the patient sees both the PCP and the specialist at the same time or at the same location.
Because patients are typically referred by PCPs to specialists at a different site, the physical separation between providers might exacerbate both access and communication problems (Epstein 1995). In a co-location model, however, providers are in the same practice location or share a formal co-management structure (Epstein 1995; Gallo et al. 2004; Smith, Allwright, and O’Dowd 2007; Williams et al. 2005).
In multidisciplinary group visits, a group of patients with the same condition sees a team of providers, including generalists and specialists, during the same visit. Group visits can improve access and efficiency of care (AAFP 2009; Huang and Carrier 2005; Trento et al. 2001). For example, one study showed high levels of both patients’ and providers’ satisfaction with group visits by patients cared for in safety-net organizations (Huang and Carrier 2005). Other studies have found greater adherence to diabetes management and preventive care guidelines in a randomized-controlled trial comparing group visits with usual care (Clancy et al. 2007; Trento et al. 2001).
Another strategy to improve access to specialists is to use “virtual” consultations. Examples are email (Bodenheimer 2008; Hilty et al. 2004), telephone (Hilty et al. 2004; Williams et al. 2005), and video-conference visits (Wakefield et al. 2004; Weiner et al. 2009). Promising innovations would allow the transfer of sophisticated biometric data and high-resolution images via new technology. In theory, in a “virtual consultation,” there is less separation between the referring physician and the specialist, and the referring provider and the patient might even be able to visit the specialist together. Even though the feasibility of virtual consultations has been established (Granlund et al. 2003; Gustke et al. 2000), there is little information about how they affect referral rates, appropriate referrals, and access to care (Kim-Hwang et al. 2010; Perednia et al. 1998).
Summary and Conclusion
The referral process can be divided into three components: referral decision making, care coordination, and access to specialty care. Our literature review provides evidence for deficiencies in each of these components. Much of the existing literature highlights the variation in referral decision making among PCPs and the reasons for this variation, but few studies explore the appropriateness of the referral decision. Those that do measure appropriateness generally find both overreferral and underreferral. Information transfer also is problematic, as frequently inadequate or no information at all is passed on. Patients often have difficulty accessing specialty care, and the referring physician and the specialist often disagree on the role of the specialist after the initial visit; PCPs frequently do not know whether a referral visit took place or what the specialist's plan is; and patients are often the only means of communication between providers.
Indeed, the term specialty-referral process might be considered a misnomer. The primary care system and the specialty care system appear to operate in parallel with little integration beyond the patient as the intermediary. This weak integration contributes to inefficient care and dissatisfaction by PCPs, specialists, and patients alike.
Our literature review emphasizes several themes and limitations of the existing literature on specialty referrals. First, many of the articles that focused on variation in referral rates assumed that there were too many referrals. Although overreferral is a substantial problem in the United States, underreferral is a problem as well, particularly for specialties with few physicians (e.g., child and adolescent psychiatry). It is notable that 26 percent of a national sample of 307 malpractice claims pertaining to a missed or delayed diagnosis involved a failure to refer (Gandhi et al. 2006). Future work should examine the appropriateness of referrals and look at both overreferral and underreferral. Second, most articles examined only one aspect of the referral process. We hope that our conceptual framework (referral decision, care coordination, access to specialty care) helps highlight the many parts of a successful referral. Third, we hope our work emphasizes that there are many components of care coordination, such as making sure that the referred patient sees the specialist, clarifying the role of the specialist, and ensuring management continuity. One of the limitations of the published literature is its focus on a single practice setting. There is a need for studies that look more broadly across settings, because there are various ways of initiating, managing, and tracking referrals. As a result, we do not know whether the findings are idiosyncratic to the specific setting of care examined in a given study. Nonetheless, because the studies often had consistent findings, we believe it is reasonable to generalize that the issues we describe are widespread throughout the U.S. health care system.
The current state of the specialty-referral process in the United States provides substantial opportunities for improvement, as there are breakdowns and inefficiencies in all its components. Given the expected increase in the elderly segment of the U.S. population, the increasing demand for specialist care, and the expected shortage of all types of physicians by 2020, improving the specialty-referral process deserves greater attention. Many of the mechanisms to improve it, including the use of information technology and payment reform, are promising. But no single change will address all the gaps in the referral process, so we need rigorous evaluations of mechanisms to improve the process across care settings.
Acknowledgments
This work was supported by a grant from the California Health Care Foundation. The funder had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript. None of the authors has a financial interest in or a financial conflict with the subject matter or the materials discussed in this article.
References
- AAFP (American Academy of Family Physicians) Group Visits (Shared Medical Appointments) 2009. Available at http://www.aafp.org/online/en/home/practicemgt/quality/qitools/pracredesign/january05.html (accessed February 4, 2011)
- Akbari A, Mayhew A, Al-Alawi M, Grimshaw JM, Winkens RA, Glidewell E, Pritchard C, Thomas R, Fraser C. Interventions to Improve Outpatient Referrals from Primary Care to Secondary Care. Cochrane Database of Systematic Reviews. 2005 doi: 10.1002/14651858.CD005471. CD005471. [DOI] [PubMed] [Google Scholar]
- Albertson GA, Lin CT, Kutner J, Schilling LM, Anderson SN, Anderson RJ. Recognition of Patient Referral Desires in an Academic Managed Care Plan: Frequency, Determinants, and Outcomes. Journal of General Internal Medicine. 2000;15:242–47. doi: 10.1111/j.1525-1497.2000.02208.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avidor Y, Still CD, Brunner M, Buchwald JN, Buchwald H. Primary Care and Subspecialty Management of Morbid Obesity: Referral Patterns for Bariatric Surgery. Surgery for Obesity and Related Diseases. 2007;3:392–407. doi: 10.1016/j.soard.2006.12.003. [DOI] [PubMed] [Google Scholar]
- Ayanian JZ, Landrum MB, Guadagnoli E, Gaccione P. Specialty of Ambulatory Care Physicians and Mortality among Elderly Patients after Myocardial Infarction. New England Journal of Medicine. 2002;347:1678–86. doi: 10.1056/NEJMsa020080. [DOI] [PubMed] [Google Scholar]
- Bachman KH, Freeborn DK. HMO Physicians’ Use of Referrals. Social Science & Medicine. 1999;48:547–57. doi: 10.1016/s0277-9536(98)00380-3. [DOI] [PubMed] [Google Scholar]
- Bergus GR, Emerson M, Reed DA, Attaluri A. Email Teleconsultations: Well Formulated Clinical Referrals Reduce the Need for Clinic Consultation. Journal of Telemedicine and Telecare. 2006;12:33–38. doi: 10.1258/135763306775321434. [DOI] [PubMed] [Google Scholar]
- Bertakis KD, Callahan EJ, Azari R, Robbins JA. Predictors of Patient Referrals by Primary Care Residents to Specialty Care Clinics. Family Medicine Journal. 2001;33:203–9. [PubMed] [Google Scholar]
- Bitton A, Martin C, Landon BE. A Nationwide Survey of Patient Centered Medical Home Demonstration Projects. Journal of General Internal Medicine. 2010;25:584–92. doi: 10.1007/s11606-010-1262-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blendon RJ, Schoen C, DesRoches C, Osborn R, Zapert K. Common Concerns amid Diverse Systems: Health Care Experiences in Five Countries. Health Affairs (Millwood) 2003;22:106–21. doi: 10.1377/hlthaff.22.3.106. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T. Coordinating Care—A Perilous Journey through the Health Care System. New England Journal of Medicine. 2008;358:1064–71. doi: 10.1056/NEJMhpr0706165. [DOI] [PubMed] [Google Scholar]
- Borowsky SJ, Rubenstein LV, Skootsky SA, Shapiro MF. Referrals by General Internists and Internal Medicine Trainees in an Academic Medicine Practice. American Journal of Managed Care. 1997;3:1679–87. [PubMed] [Google Scholar]
- Boulis AK, Long J. Variation in the Treatment of Children by Primary Care Physician Specialty. Archives of Pediatrics & Adolescent Medicine. 2002;156:1210–15. doi: 10.1001/archpedi.156.12.1210. [DOI] [PubMed] [Google Scholar]
- Bourguet C, Gilchrist V, McCord G. The Consultation and Referral Process. A Report from NEON. Northeastern Ohio Network Research Group. Journal of Family Practice. 1998;46:47–53. [PubMed] [Google Scholar]
- Byrd JC, Moskowitz MA. Outpatient Consultation: Interaction between the General Internist and the Specialist. Journal of General Internal Medicine. 1987;2:93–98. doi: 10.1007/BF02596304. [DOI] [PubMed] [Google Scholar]
- Calman NS, Hyman RB, Licht W. Variability in Consultation Rates and Practitioner Level of Diagnostic Certainty. Journal of Family Practice. 1992;35:31–38. [PubMed] [Google Scholar]
- Chen AH, Yee HF., Jr Improving the Primary Care–Specialty Care Interface: Getting from Here to There. Archives of Internal Medicine. 2009;169:1024–26. doi: 10.1001/archinternmed.2009.140. [DOI] [PubMed] [Google Scholar]
- Chen FM. Dermatology Referrals in an Academic Family Medicine Clinic. Southern Medical Journal. 2001;94:475–77. [PubMed] [Google Scholar]
- Chen FM, Fryer GE, Jr, Norris TE. Effects of Comorbidity and Clustering upon Referrals in Primary Care. Journal of the American Board of Family Practice. 2005;18:449–52. doi: 10.3122/jabfm.18.6.449. [DOI] [PubMed] [Google Scholar]
- Clancy DE, Huang P, Okonofua E, Yeager D, Magruder KM. Group Visits: Promoting Adherence to Diabetes Guidelines. Journal of General Internal Medicine. 2007;22:620–24. doi: 10.1007/s11606-007-0150-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CMS (Centers for Medicare & Medicaid Services) Medical Home Demonstration Fact Sheet. 2009. Available at https://www.cms.gov/DemoProjectsEvalRpts/downloads/MedHome_FactSheet.pdf (accessed January 19, 2011)
- Collins JA, Fauser BC. Balancing the Strengths of Systematic and Narrative Reviews. Human Reproduction Update. 2005;11:103–4. doi: 10.1093/humupd/dmh058. [DOI] [PubMed] [Google Scholar]
- Cook NL, Nicks LS, O’Malley AJ, Keegan T, Guadagnoli E, Landon BE. Access to Specialty Care and Medical Services in Community Health Centers. Health Affairs. 2007;26:1459–68. doi: 10.1377/hlthaff.26.5.1459. [DOI] [PubMed] [Google Scholar]
- Davidson SM, Manheim LM, Werner SM, Hohlen MM, Yudkowsky BK, Fleming GV. Prepayment with Office-Based Physicians in Publicly Funded Programs: Results from the Children's Medicaid Program. Pediatrics. 1992;89:761–67. [PubMed] [Google Scholar]
- Donohoe MT, Kravitz RL, Wheeler DB, Chandra R, Chen A, Humphries N. Reasons for Outpatient Referrals from Generalists to Specialists. Journal of General Internal Medicine. 1999;14:281–86. doi: 10.1046/j.1525-1497.1999.00324.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein RM. Communication between Primary Care Physicians and Consultants. Archives of Family Medicine. 1995;4:403–9. doi: 10.1001/archfami.4.5.403. [DOI] [PubMed] [Google Scholar]
- Ettinger ER, Schwartz MD, Kalet AL. Referral Patterns of Primary Care Physicians for Eye Care. Journal of the American Optometric Association. 1993;64:468–70. [PubMed] [Google Scholar]
- Everett GD, Parsons TJ, Christensen AL. Educational Influences on Consultation Rates of House Staff Physicians in a Primary Care Clinic. Journal of Medical Education. 1984;59:479–86. doi: 10.1097/00001888-198406000-00004. [DOI] [PubMed] [Google Scholar]
- Faulkner A, Mills N, Bainton D, Baxter K, Kinnersley P, Peters TJ, Sharp D. A Systematic Review of the Effect of Primary Care–Based Service Innovations on Quality and Patterns of Referral to Specialist Secondary Care. British Journal of General Practice. 2003;53:878–84. [PMC free article] [PubMed] [Google Scholar]
- Ferrer RL. Pursuing Equity: Contact with Primary Care and Specialist Clinicians by Demographics, Insurance, and Health Status. Annals of Family Medicine. 2007;5:492–502. doi: 10.1370/afm.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferris TG, Chang Y, Blumenthal D, Pearson SD. Leaving Gatekeeping Behind—Effects of Opening Access to Specialists for Adults in a Health Maintenance Organization. New England Journal of Medicine. 2001;345:1312–17. doi: 10.1056/NEJMsa010097. [DOI] [PubMed] [Google Scholar]
- Fertig A, Roland M, King H, Moore T. Understanding Variation in Rates of Referral among General Practitioners: Are Inappropriate Referrals Important and Would Guidelines Help to Reduce Rates? BMJ. 1993;307:1467–70. doi: 10.1136/bmj.307.6917.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein JA, Lozano P, Shulruff R, Inui TS, Soumerai SB, Ng M, Weiss KB. Self-Reported Physician Practices for Children with Asthma: Are National Guidelines Followed? Pediatrics. 2000;106:886–96. [PubMed] [Google Scholar]
- Finkelstein RL. Improving Identification and Communication with Referring and Primary Care Physicians. NAHAM Management Journal. 1998;24:7–10. [PubMed] [Google Scholar]
- Forrest CB. A Typology of Specialists’ Clinical Roles. Archives of Internal Medicine. 2009;169:1062–68. doi: 10.1001/archinternmed.2009.114. [DOI] [PubMed] [Google Scholar]
- Forrest CB, Glade GB, Baker AE, Bocian AB, Kang M, Starfield B. The Pediatric Primary-Specialty Care Interface: How Pediatricians Refer Children and Adolescents to Specialty Care. Archives of Pediatrics & Adolescent Medicine. 1999;153:705–14. doi: 10.1001/archpedi.153.7.705. [DOI] [PubMed] [Google Scholar]
- Forrest CB, Majeed A, Weiner JP, Carroll K, Bindman AB. Comparison of Specialty Referral Rates in the United Kingdom and the United States: Retrospective Cohort Analysis. BMJ. 2002;325:370–71. doi: 10.1136/bmj.325.7360.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest CB, Nutting PA, Starfield B, von Schrader S. Family Physicians’ Referral Decisions: Results from the ASPN Referral Study. Journal of Family Practice. 2002;51:215–22. [PubMed] [Google Scholar]
- Forrest CB, Nutting PA, von Schrader S, Rohde C, Starfield B. Primary Care Physician Specialty Referral Decision Making: Patient, Physician, and Health Care System Determinants. Medical Decision Making. 2006;26:76–85. doi: 10.1177/0272989X05284110. [DOI] [PubMed] [Google Scholar]
- Forrest CB, Nutting PA, Werner JJ, Starfield B, von Schrader S, Rohde C. Managed Health Plan Effects on the Specialty Referral Process: Results from the Ambulatory Sentinel Practice Network Referral Study. Medical Care. 2003;41:242–53. doi: 10.1097/01.MLR.0000044903.91168.B6. [DOI] [PubMed] [Google Scholar]
- Forrest CB, Reid RJ. Passing the Baton: HMOs’ Influence on Referrals to Specialty Care. Health Affairs (Millwood) 1997;16:157–62. doi: 10.1377/hlthaff.16.6.157. [DOI] [PubMed] [Google Scholar]
- Forrest CB, Reid RJ. Prevalence of Health Problems and Primary Care Physicians’ Specialty Referral Decisions. Journal of Family Practice. 2001;50:427–32. [PubMed] [Google Scholar]
- Forrest CB, Shadmi E, Nutting PA, Starfield B. Specialty Referral Completion among Primary Care Patients: Results from the ASPN Referral Study. Annals of Family Medicine. 2007;5:361–67. doi: 10.1370/afm.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest CB, Weiner JP, Fowles J, Vogeli C, Frick KD, Lemke KW, Starfield B. Self-Referral in Point-of-Service Health Plans. JAMA. 2001;285:2223–31. doi: 10.1001/jama.285.17.2223. [DOI] [PubMed] [Google Scholar]
- Franks P, Williams GC, Zwanziger J, Mooney C, Sorbero M. Why Do Physicians Vary So Widely in Their Referral Rates? Journal of General Internal Medicine. 2000;15:163–68. doi: 10.1046/j.1525-1497.2000.04079.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franks P, Zwanziger J, Mooney C, Sorbero M. Variations in Primary Care Physician Referral Rates. Health Services Research. 1999;34:323–29. [PMC free article] [PubMed] [Google Scholar]
- Fung CH, Lim YW, Mattke S, Damberg C, Shekelle PG. Systematic Review: The Evidence That Publishing Patient Care Performance Data Improves Quality of Care. Annals of Internal Medicine. 2008;148:111–23. doi: 10.7326/0003-4819-148-2-200801150-00006. [DOI] [PubMed] [Google Scholar]
- Gallo JJ, Zubritsky C, Maxwell J, Nazar M, Bogner HR, Quijano LM, Syropoulos HJ, et al. Primary Care Clinicians Evaluate Integrated and Referral Models of Behavioral Health Care for Older Adults: Results from a Multisite Effectiveness Trial (PRISM-e) Annals of Family Medicine. 2004;2:305–9. doi: 10.1370/afm.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi TK, Kachalia A, Thomas EJ, Puopolo AL, Yoon C, Brennan TA, Studdert DM. Missed and Delayed Diagnoses in the Ambulatory Setting: A Study of Closed Malpractice Claims. Annals of Internal Medicine. 2006;145:488–96. doi: 10.7326/0003-4819-145-7-200610030-00006. [DOI] [PubMed] [Google Scholar]
- Gandhi TK, Keating NL, Ditmore M, Kiernan D, Johnson R, Burdick E, Hamann C. Improving Referral Communication Using a Referral Tool within an Electronic Medical Record. 2008. Available at http://www.ahrq.gov/downloads/pub/advances2/vol3/advances-gandhi_22.pdf (accessed January 4, 2011) [PubMed]
- Gandhi TK, Sittig DF, Franklin M, Sussman AJ, Fairchild DG, Bates DW. Communication Breakdown in the Outpatient Referral Process. Journal of General Internal Medicine. 2000;15:626–31. doi: 10.1046/j.1525-1497.2000.91119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrido T, Jamieson L, Zhou Y, Wiesenthal A, Liang L. Effect of Electronic Health Records in Ambulatory Care: Retrospective, Serial, Cross Sectional Study. BMJ. 2005;330:581. doi: 10.1136/bmj.330.7491.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn JK, Lawler FH, Hoerl MS. Physician Referrals in a Competitive Environment. An Estimate of the Economic Impact of a Referral. JAMA. 1987;258:1920–23. [PubMed] [Google Scholar]
- Granlund H, Thoden CJ, Carlson C, Harno K. Realtime Teleconsultations versus Face-to-Face Consultations in Dermatology: Immediate and Six-Month Outcome. Journal of Telemedicine and Telecare. 2003;9:204–9. doi: 10.1258/135763303322225526. [DOI] [PubMed] [Google Scholar]
- Greenfield S, Nelson EC, Zubkoff M, Manning W, Rogers W, Kravitz RL, Keller A, Tarlov AR, Ware JE., Jr Variations in Resource Utilization among Medical Specialties and Systems of Care. Results from the Medical Outcomes Study. JAMA. 1992;267:1624–30. [PubMed] [Google Scholar]
- Grimshaw JM, Winkens RA, Shirran L, Cunningham C, Mayhew A, Thomas R, Fraser C. Interventions to Improve Outpatient Referrals from Primary Care to Secondary Care. Cochrane Database of Systematic Reviews. 2005 doi: 10.1002/14651858.CD005471. CD005471. [DOI] [PubMed] [Google Scholar]
- Grumbach K, Selby JV, Damberg C, Bindman AB, Quesenberry C, Jr, Truman A, Uratsu C. Resolving the Gatekeeper Conundrum: What Patients Value in Primary Care and Referrals to Specialists. JAMA. 1999;282:261–66. doi: 10.1001/jama.282.3.261. [DOI] [PubMed] [Google Scholar]
- Gustke S, Balch DC, Rogers LO, West VL. Profile of Users of Real-Time Interactive Teleconference Clinical Consultations. Archives of Family Medicine. 2000;9:1036–40. doi: 10.1001/archfami.9.10.1036. [DOI] [PubMed] [Google Scholar]
- Hackbarth G, Reischauer R, Mutti A. Collective Accountability for Medical Care—Toward Bundled Medicare Payments. New England Journal of Medicine. 2008;359:3–5. doi: 10.1056/NEJMp0803749. [DOI] [PubMed] [Google Scholar]
- Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of Care: A Multidisciplinary Review. BMJ. 2003;327:1219–21. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington JT, Dopf CA, Chalgren CS. Implementing Guidelines for Interdisciplinary Care of Low Back Pain: A Critical Role for Pre-appointment Management of Specialty Referrals. Joint Commission Journal on Quality Improvement. 2001;27:651–63. doi: 10.1016/s1070-3241(01)27055-2. [DOI] [PubMed] [Google Scholar]
- Harrington JT, Walsh MB. Pre-appointment Management of New Patient Referrals in Rheumatology: A Key Strategy for Improving Health Care Delivery. Arthritis & Rheumatism. 2001;45:295–300. doi: 10.1002/1529-0131(200106)45:3<295::AID-ART263>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- Harrold LR, Field TS, Gurwitz JH. Knowledge, Patterns of Care, and Outcomes of Care for Generalists and Specialists. Journal of General Internal Medicine. 1999;14:499–511. doi: 10.1046/j.1525-1497.1999.08168.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilty DM, Ingraham RL, Yang SP, Anders TF. Multispecialty Telephone and E-mail Consultation for Patients with Developmental Disabilities in Rural California. Telemedicine Journal and E-Health. 2004;10:413–21. doi: 10.1089/tmj.2004.10.413. [DOI] [PubMed] [Google Scholar]
- Hongsermeier T, Mitus AJ. Managing the Interface between Primary-Care Provider and Specialist. Journal of Cardiovascular Management. 1997;8:27–29. [PubMed] [Google Scholar]
- Huang J, Carrier B. AcademyHealth. Boston: AcademyHealth; 2005. Group Visits in Safety Net Hospitals and Health Systems: A Model for Increasing Access to Care. ed. AcademyHealth, abstract 3667. [Google Scholar]
- Im SS, Gordon AN, Buttin BM, Leath CA, III, Gostout BS, Shah C, Hatch KD, Wang J, Berman ML. Validation of Referral Guidelines for Women with Pelvic Masses. Obstetrics & Gynecology. 2005;105:35–41. doi: 10.1097/01.AOG.0000149159.69560.ef. [DOI] [PubMed] [Google Scholar]
- Institute for Healthcare Improvement. Specialty Care Access. 2008. Available at http://www.ihi.org/IHI/Topics/OfficePractices/SpecialtyCareAccess (January 4, 2011)
- Iverson GD, Coleridge ST, Fulda KG, Licciardone JC. What Factors Influence a Family Physician's Decision to Refer a Patient to a Specialist? Rural Remote Health. 2005;5:413. [PubMed] [Google Scholar]
- Jaen CR, Ferrer RL, Miller WL, Palmer RF, Wood R, Davila M, Stewart EE, Crabtree BF, Nutting PA, Stange KC. Patient Outcomes at 26 Months in the Patient-Centered Medical Home National Demonstration Project. Annals of Family Medicine. 2010;8(suppl. 1):S57–67. doi: 10.1370/afm.1121. S92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y, Chen AH, Keith E, Yee HF, Jr, Kushel MB. Not Perfect, but Better: Primary Care Providers’ Experiences with Electronic Referrals in a Safety Net Health System. Journal of General Internal Medicine. 2009;24:614–19. doi: 10.1007/s11606-009-0955-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Hwang JE, Chen AH, Bell DS, Guzman D, Yee HF, Jr, Kushel MB. Evaluating Electronic Referrals for Specialty Care at a Public Hospital. Journal of General Internal Medicine. 2010;25:1123–28. doi: 10.1007/s11606-010-1402-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinchen KS, Cooper LA, Levine D, Wang NY, Powe NR. Referral of Patients to Specialists: Factors Affecting Choice of Specialist by Primary Care Physicians. Annals of Family Medicine. 2004;2:245–52. doi: 10.1370/afm.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunkle EC. Communication Breakdown in Referral of the Patient. JAMA. 1964;187:663. doi: 10.1001/jama.1964.03060220037011. [DOI] [PubMed] [Google Scholar]
- Lafata JE, Martin S, Morlock R, Divine G, Xi H. Provider Type and the Receipt of General and Diabetes-Related Preventive Health Services among Patients with Diabetes. Medical Care. 2001;39:491–99. doi: 10.1097/00005650-200105000-00009. [DOI] [PubMed] [Google Scholar]
- Landon BE, Wilson IB, McInnes K, Landrum MB, Hirschhorn LR, Marsden PV, Cleary PD. Physician Specialization and the Quality of Care for Human Immunodeficiency Virus Infection. Archives of Internal Medicine. 2005;165:1133–39. doi: 10.1001/archinte.165.10.1133. [DOI] [PubMed] [Google Scholar]
- Lawler FH. Referral Rates of Senior Family Practice Residents in an Ambulatory Care Clinic. Journal of Medical Education. 1987;62:177–82. doi: 10.1097/00001888-198703000-00005. [DOI] [PubMed] [Google Scholar]
- Lawler FH, Purvis JR, Glenn JK, Clark D, Horner RD. Physician Referrals from a Rural Family Practice Residency Clinic: A Pilot Study. Family Practice Research Journal. 1990;10:19–26. [PubMed] [Google Scholar]
- Lee T, Pappius EM, Goldman L. Impact of Inter-physician Communication on the Effectiveness of Medical Consultations. American Journal of Medicine. 1983;74:106–12. doi: 10.1016/0002-9343(83)91126-9. [DOI] [PubMed] [Google Scholar]
- Lin CT, Albertson G, Price D, Swaney R, Anderson S, Anderson RJ. Patient Desire and Reasons for Specialist Referral in a Gatekeeper-Model Managed Care Plan. American Journal of Managed Care. 2000;6:669–78. [PubMed] [Google Scholar]
- Linzer M, Myerburg RJ, Kutner JS, Wilcox CM, Oddone E, DeHoratius RJ, Naccarelli GV, Committee AW. Exploring the Generalist-Subspecialist Interface in Internal Medicine. American Journal of Medicine. 2006;119:528–37. doi: 10.1016/j.amjmed.2006.03.007. [DOI] [PubMed] [Google Scholar]
- Machlin SR, Carper K. Statistical Brief 166: Expenses for Office-Based Physician Visits by Specialty, 2004. 2007. Available at http://www.meps.ahrq.gov/mepsweb/data_files/publications/st166/stat166.pdf (accessed February 4, 2011)
- Marrero DG, Moore PS, Langefeld CD, Clark CM., Jr Patterns of Referral and Examination for Retinopathy in Pregnant Women with Diabetes by Primary Care Physicians. Ophthalmic Epidemiology. 1995;2:93–98. doi: 10.3109/09286589509057088. [DOI] [PubMed] [Google Scholar]
- Mayer ML. Disparities in Geographic Access to Pediatric Subspecialty Care. Maternal and Child Health Journal. 2007;12:624–32. doi: 10.1007/s10995-007-0275-3. [DOI] [PubMed] [Google Scholar]
- McPhee SJ, Lo B, Saika GY, Meltzer R. How Good Is Communication between Primary Care Physicians and Subspecialty Consultants? Archives of Internal Medicine. 1984;144:1265–68. [PubMed] [Google Scholar]
- Mehrotra A, Keehl-Markowitz L, Ayanian JZ. Implementing Open-Access Scheduling of Visits in Primary Care Practices: A Cautionary Tale. Annals of Internal Medicine. 2008;148:915–22. doi: 10.7326/0003-4819-148-12-200806170-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore AT, Roland MO. How Much Variation in Referral Rates among General Practitioners Is Due to Chance? BMJ. 1989;298:500–502. doi: 10.1136/bmj.298.6672.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mostert MC, Richardus JH, de Man RA. Referral of Chronic Hepatitis B Patients from Primary to Specialist Care: Making a Simple Guideline Work. Journal of Hepatology. 2004;41:1026–30. doi: 10.1016/j.jhep.2004.08.012. [DOI] [PubMed] [Google Scholar]
- Murray M. Reducing Waits and Delays in the Referral Process. Family Practice Management. 2002;9:39–42. [PubMed] [Google Scholar]
- Murray M, Berwick DM. Advanced Access: Reducing Waiting and Delays in Primary Care. JAMA. 2003;289:1035–40. doi: 10.1001/jama.289.8.1035. [DOI] [PubMed] [Google Scholar]
- Navaneethan SD, Aloudat S, Singh S. A Systematic Review of Patient and Health System Characteristics Associated with Late Referral in Chronic Kidney Disease. BMC Nephrology. 2008;9:3. doi: 10.1186/1471-2369-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveria SA, Yood MU, Campbell UB, Yood SM, Stang P. Treatment and Referral Patterns for Colorectal Cancer. Medical Care. 2004;42:901–6. doi: 10.1097/01.mlr.0000135820.44720.89. [DOI] [PubMed] [Google Scholar]
- O’Malley AS, Cunningham PJ. Patient Experiences with Coordination of Care: The Benefit of Continuity and Primary Care Physician as Referral Source. Journal of General Internal Medicine. 2009;24:170–77. doi: 10.1007/s11606-008-0885-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perednia DA, Wallace J, Morrisey M, Bartlett M, Marchionda L, Gibson A, Campbell E. The Effect of a Teledermatology Program on Rural Referral Patterns to Dermatologists and the Management of Skin Disease. Studies in Health Technology and Informatics. 1998;52(part 1):290–93. [PubMed] [Google Scholar]
- RAND. Overview of Bundled Payment Policy Options. 2009. Available at http://www.randcompare.org/options/mechanism/bundled_payment (accessed February 4, 2011)
- Reeder BM, Lyne ED, Patel DR, Cucos DR. Referral Patterns to a Pediatric Orthopedic Clinic: Implications for Education and Practice. Pediatrics. 2004;113:e163–67. doi: 10.1542/peds.113.3.e163. [DOI] [PubMed] [Google Scholar]
- Rodriguez HP, Scoggins JF, von Glahn T, Zaslavsky AM, Safran DG. Attributing Sources of Variation in Patients’ Experiences of Ambulatory Care. Medical Care. 2009;47(8):835–41. doi: 10.1097/MLR.0b013e318197b1e1. [DOI] [PubMed] [Google Scholar]
- Safran C, Rind DM, Davis RB, Ives D, Sands DZ, Currier J, Slack WV, Makadon HJ, Cotton DJ. Guidelines for Management of HIV Infection with Computer-Based Patient's Record. Lancet. 1995;346:341–46. doi: 10.1016/s0140-6736(95)92226-1. [DOI] [PubMed] [Google Scholar]
- Salerno SM, Hurst FP, Halvorson S, Mercado DL. Principles of Effective Consultation: An Update for the 21st-Century Consultant. Archives of Internal Medicine. 2007;167:271–75. doi: 10.1001/archinte.167.3.271. [DOI] [PubMed] [Google Scholar]
- Saunders TC. Consultation-Referral among Physicians: Practice and Process. Journal of Family Practice. 1978;6:123–28. [PubMed] [Google Scholar]
- Schoen C, Osborn R, How SK, Doty MM, Peugh J. In Chronic Condition: Experiences of Patients with Complex Health Care Needs, in Eight Countries, 2008. Health Affairs (Millwood) 2009;28:w1–16. doi: 10.1377/hlthaff.28.1.w1. [DOI] [PubMed] [Google Scholar]
- Shaw I, Smith KM, Middleton H, Woodward L. A Letter of Consequence: Referral Letters from General Practitioners to Secondary Mental Health Services. Qualitative Health Research. 2005;15:116–28. doi: 10.1177/1049732304270725. [DOI] [PubMed] [Google Scholar]
- Shea D, Stuart B, Vasey J, Nag S. Medicare Physician Referral Patterns. Health Services Research. 1999;34:331–48. [PMC free article] [PubMed] [Google Scholar]
- Smith S, Allwright S, O’Dowd T. Effectiveness of Shared Care across the Interface between Primary and Specialty Care in Chronic Disease Management. Cochrane Database of Systematic Reviews. 2007 doi: 10.1002/14651858.CD004910.pub2. CD004910. [DOI] [PubMed] [Google Scholar]
- Speed CA, Crisp AJ. Referrals to Hospital-Based Rheumatology and Orthopaedic Services: Seeking Direction. Rheumatology (Oxford) 2005;44:469–71. doi: 10.1093/rheumatology/keh504. [DOI] [PubMed] [Google Scholar]
- Starfield B, Forrest CB, Nutting PA, von Schrader S. Variability in Physician Referral Decisions. Journal of the American Board of Family Practice. 2002;15:473–80. [PubMed] [Google Scholar]
- Steckler RE, Zaontz MR, Skoog SJ, Rushton HG., Jr Cryptorchidism, Pediatricians, and Family Practitioners: Patterns of Practice and Referral. Journal of Pediatrics. 1995;127:948–51. doi: 10.1016/s0022-3476(95)70034-x. [DOI] [PubMed] [Google Scholar]
- Stille CJ, McLaughlin TJ, Primack WA, Mazor KM, Wasserman RC. Determinants and Impact of Generalist-Specialist Communication about Pediatric Outpatient Referrals. Pediatrics. 2006;118:1341–49. doi: 10.1542/peds.2005-3010. [DOI] [PubMed] [Google Scholar]
- Stille CJ, Primack WA, McLaughlin TJ, Wasserman RC. Parents as Information Intermediaries between Primary Care and Specialty Physicians. Pediatrics. 2007;120:1238–46. doi: 10.1542/peds.2007-1112. [DOI] [PubMed] [Google Scholar]
- St Peter RF, Reed MC, Kemper P, Blumenthal D. Changes in the Scope of Care Provided by Primary Care Physicians. New England Journal of Medicine. 1999;341:1980–85. doi: 10.1056/NEJM199912233412606. [DOI] [PubMed] [Google Scholar]
- Strunk BC, Cunningham PJ. Treading Water: Americans’ Access to Needed Medical Care, 1997–2001. Track Rep. 2002:1–6. [PubMed] [Google Scholar]
- Swarztrauber K, Vickrey BG, Mittman BS. Physicians’ Preferences for Specialty Involvement in the Care of Patients with Neurological Conditions. Medical Care. 2002;40:1196–209. doi: 10.1097/00005650-200212000-00007. [DOI] [PubMed] [Google Scholar]
- Tanielian TL, Pincus HA, Dietrich AJ, Williams JW, Jr, Oxman TE, Nutting P, Marcus SC. Referrals to Psychiatrists. Assessing the Communication Interface between Psychiatry and Primary Care. Psychosomatics. 2000;41:245–52. doi: 10.1176/appi.psy.41.3.245. [DOI] [PubMed] [Google Scholar]
- Trento M, Passera P, Tomalino M, Bajardi M, Pomero F, Allione A, Vaccari P, Molinatti GM, Porta M. Group Visits Improve Metabolic Control in Type 2 Diabetes: A 2-Year Follow-up. Diabetes Care. 2001;24:995–1000. doi: 10.2337/diacare.24.6.995. [DOI] [PubMed] [Google Scholar]
- Valderas JM, Starfield B, Forrest CB, Sibbald B, Roland M. Ambulatory Care Provided by Office-Based Specialists in the United States. Annals of Family Medicine. 2009;7:104–11. doi: 10.1370/afm.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vierhout WP, van Knottnerus JA, van Ooij A, Crebolder HF, Pop P, Wesselingh-Megens AM, Beusmans GH. Effectiveness of Joint Consultation Sessions of General Practitioners and Orthopaedic Surgeons for Locomotor-System Disorders. Lancet. 1995;346:990–94. doi: 10.1016/s0140-6736(95)91686-5. [DOI] [PubMed] [Google Scholar]
- Wakefield BJ, Buresh KA, Flanagan JR, Kienzle MG. Interactive Video Specialty Consultations in Long-Term Care. Journal of the American Geriatrics Society. 2004;52:789–93. doi: 10.1111/j.1532-5415.2004.52220.x. [DOI] [PubMed] [Google Scholar]
- Wallerstein R, Seshadri K. Are Referrals to Developmental Pediatricians Appropriate? Our Experience over a 15-Year Period. Clinical Pediatrics (Philadelphia) 1994;33:564–68. doi: 10.1177/000992289403300910. [DOI] [PubMed] [Google Scholar]
- Warren BH. An Outcomes Analysis Approach to Utilization Management: Quality Assessment of Appropriateness of Specialty Referrals. American Journal of Medical Quality. 1994;9:34–38. doi: 10.1177/0885713X9400900107. [DOI] [PubMed] [Google Scholar]
- Weiner M, El Hoyek G, Wang L, Dexter PR, Zerr AD, Perkins AJ, James F, Juneja R. A Web-Based Generalist-Specialist System to Improve Scheduling of Outpatient Specialty Consultations in an Academic Center. Journal of General Internal Medicine. 2009;24:710–15. doi: 10.1007/s11606-009-0971-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman JS, Moy E, Campbell EG, Gokhale M, Yucel R, Causino N, Blumenthal D. Limits to the Safety Net: Teaching Hospital Faculty Report on Their Patients’ Access to Care. Health Affairs. 2003;22:156–66. doi: 10.1377/hlthaff.22.6.156. [DOI] [PubMed] [Google Scholar]
- Williams J, Palmes G, Klinepeter K, Pulley A, Foy JM. Referral by Pediatricians of Children with Behavioral Health Disorders. Clinical Pediatrics (Philadelphia) 2005;44:343–49. doi: 10.1177/000992280504400410. [DOI] [PubMed] [Google Scholar]
- Williams PT, Peet G. Differences in the Value of Clinical Information: Referring Physicians versus Consulting Specialists. Journal of the American Board of Family Practice. 1994;7:292–302. [PubMed] [Google Scholar]
- Willison DJ, Soumerai SB, McLaughlin TJ, Gurwitz JH, Gao X, Guadagnoli E, Pearson S, Hauptman P, McLaughlin B. Consultation between Cardiologists and Generalists in the Management of Acute Myocardial Infarction: Implications for Quality of Care. Archives of Internal Medicine. 1998;158:1778–83. doi: 10.1001/archinte.158.16.1778. [DOI] [PubMed] [Google Scholar]
- Wu AW, Young Y, Skinner EA, Diette GB, Huber M, Peres A, Steinwachs D. Quality of Care and Outcomes of Adults with Asthma Treated by Specialists and Generalists in Managed Care. Archives of Internal Medicine. 2001;161:2554–60. doi: 10.1001/archinte.161.21.2554. [DOI] [PubMed] [Google Scholar]


