Abstract
Background
The adverse respiratory effects of ground-level ozone are well-established. Ozone is the air pollutant most consistently projected to increase under future climate change.
Purpose
To project future pediatric asthma emergency department visits associated with ground-level ozone changes, comparing 1990s to 2020s.
Methods
This study assessed future numbers of asthma emergency department visits for children aged 0–17 years using (1) baseline New York City metropolitan area emergency department rates, (2) a dose–response relationship between ozone levels and pediatric asthma emergency department visits, and (3) projected daily 8-hour maximum ozone concentrations for the 2020s as simulated by a global-to-regional climate change and atmospheric chemistry model. Sensitivity analyses included population projections and ozone precursor changes. This analysis occurred in 2010.
Results
In this model, climate change could cause an increase in regional summer ozone-related asthma emergency department visits for children aged 0–17 years of 7.3% across the New York City metropolitan region by the 2020s. This effect diminished with inclusion of ozone precursor changes. When population growth is included, the projections of morbidity related to ozone are even larger.
Conclusions
The results of this analysis demonstrate that the use of regional climate and atmospheric chemistry models make possible the projection of local climate change health effects for specific age groups and specific disease outcomes – such as emergency department visits for asthma. Efforts should be made to improve on this type of modeling to inform local and wider-scale climate change mitigation and adaptation policy.
Introduction
Asthma, the most common chronic disease in seen in pediatrics, is a genetic and environmental disorder.1, 2 The lungs are exposed to air pollution more than other organ systems particularly for children because of their increased minute ventilation compared to adults. As such, asthma exacerbations may be viewed as the “canary in the coal mine” for children's environmental health. In recent years, public health literature has highlighted respiratory illness as a potential future health impact related to climate change.3–7 However, projections of such health impacts remain uncommon for regional morbidity projections, such as asthma outcomes.8 While some studies have modeled regional climate change–related mortality9, 10 and global morbidity,11, 12 no models to date have produced regional projections of future pediatric asthma related to climate-driven changes in the U.S.
Climate change through both temperature and wind-pattern changes is projected to affect multiple air-pollutant levels and specifically ground-level ozone (O3).13 Ozone is a secondary pollutant formed through photochemical reactions involving other pollutants such as nitrogen oxides (NOx) and volatile organic chemicals (VOC).14 Acute ground-level O3 exposure is linked to childhood respiratory illness,15 exacerbations of asthma16 and, more specifically, increased emergency department visits for asthma.17–21 For example, during the Atlanta Olympics in 1996 when peak daily O3 dropped 28%, there was an 11% reduction in pediatric emergency department visits for asthma and an over-40% reduction in acute care asthma events not seen with non-asthma acute care events.17 Asthma emergency department visits are one manifestation of uncontrolled asthma which is associated with both direct (services and medication) and indirect (such as missed work by parents) costs.22, 23 The objective of this study was to demonstrate one method of projecting climate-driven, ozone-related pediatric asthma effects for the 2020s in an urban area of the U.S.
Methods
Climate change and O3 modeling
Projections of ground-level O3 were developed on a 36×36 km grid over the New York City metropolitan area by linking models for global climate, regional climate, and regional air quality.24–27 Such linkages are necessary to be able to project local future conditions and have been used previously for future health projections.9, 10 Briefly, global climate was modeled using the Goddard Institute for Space Studies general circulation model. The regional climate model used the Penn State/National Center for Atmospheric Research Mesoscale Model 5. The atmospheric chemistry and O3 simulations came from the Community Multiscale Air Quality model. The specific greenhouse gas emissions projection came from the A2 scenario of the Intergovernmental Panel on Climate Change (IPCC) Special Report on Emissions Scenarios (SRES). The IPCC SRES involve future assumptions about energy use; population growth; and political, environmental, and social development and have been used to help standardize climate modeling. The A2 scenario assumes relatively rapid growth in greenhouse gas emissions and population.28 Knowlton et al (2004)10 and Hogrefe et al (2004)24 previously published a description of these models, the greenhouse gas emission scenarios, the O3 simulations, the model evaluation compared to historic values, and uncertainties within models.
The present study focused on the 14 New York State counties that are considered part of the New York City (NYC) metropolitan area (Appendix A, available online at www.ajpmonline.org). The regional model simulated O3 for the summer season (June–August) for five consecutive mid-decadal years (e.g., 1993–1997) in the 1990s and 2020s.24 While the entire period of May – September can have high O3 levels, this study was restricted, due to computational constraints, to model outputs for June–August. The health effect model used daily 8-hour maximum O3 concentrations, the same metric specified in the National Ambient Air Quality Standards 2008 revision.29
Morbidity analysis
This study used a health-impact assessment framework to assess changes in O3-related asthma emergency department visits in the population aged 0–17 years in the 2020s compared with the 1990s.
For a typical summer of each decade, county-level impacts were computed as
where M is the mean number of daily asthma emergency department visits among children aged 0–17 years attributable to daily 8-hour maximum O3 concentrations; P is the county population in that age group during time period of interest; B is the baseline county-level daily asthma emergency department visit rate among children aged 0–17 years in June–August (per 10,000 population); ERC is the exposure–risk coefficient of asthma morbidity for a given change in the mean O3 metric, as follows:
where b is the parameter estimate that reflects a 4% change in asthma emergency department visits per 20 parts per billion (ppb) change in ground-level O3 (daily 8-hour maximum) derived from Tolbert et al.(2000),21 and ΔO3 is the average daily 8-hour maximum O3 concentration for the time period of interest.
Tolbert et al. (2000)21 examined associations between air pollutants and emergency department visits for children aged 0–16 years in Atlanta. Ideally, the ERC comes from pooled results that are geographically, diagnostically, and age matched to the study population. However, no such pooled study exists; thus, after considering the relevant epidemiologic literature, this study's ERC was derived from a single study.
The Tolbert et al.21 study of respiratory emergency department visits and air pollutant associations included multiple ICD-9 diagnostic codes30 to capture asthma events (asthma (ICD-9 code 493), wheezing (ICD-9 code 786.09) and reactive airway disease (ICD-9 code 519.1, relevant in only 1993 prevalence data) for pediatric emergency department visits among children aged 0–16 years. That study calculated the association of ozone and asthma events with 1-day lag. This study used their relative risk estimate for asthma of 1.04 per 20 ppb increase in daily maximum 8-hour ozone (95% CI, 1.008– 1.073) to calculate the ERC.
Once the mean daily O3-related morbidity was derived, the summer morbidity was calculated by multiplying by 92 for the number of days in June–August. County populations in the mid-1990s were obtained from 2000 U.S. Census data.31 Population was held constant in the 2020s for base-case calculations with the intent of isolating the climate influence and reserving exploration of this expected underestimation for the sensitivity analysis described below.
Baseline morbidity rate estimation
This study used publicly available New York State Department of Health asthma emergency department visit data which define an asthma emergency department visit as a primary emergency department diagnosis or an admitting diagnosis from the emergency department of ICD-9 code 493 for any age.32 Use of this diagnosis in children aged <3 years is problematic due to the difficulty of asthma diagnosis in this age group but more refined population-level data were not available.33, 34
Despite these limitations of the state data set, these data were the most appropriate for this model. Average daily summer pediatric asthma emergency department visits for each of the 14 counties were calculated by adjusting the annual age-specific rates with a summer scaling factor. The scaling factor of 0.137 was derived from the proportion of annual asthma emergency department visits that occurred in June–August in New York State.32 The summer seasonal rate was then converted to a daily rate. For comparison, the average summer scaling value for asthma hospitalizations for children aged 0–4 years in New York State from 1990 to 2004 was calculated to be 0.138.35 The comparable summer asthma hospitalizations for all ages—including adults— from 2000 to 2005 in New York State was 0.173; these comparisons suggest that the scaling factor used was reasonable.
These scaling calculations were made because the historical daily pediatric emergency department data for these counties (i.e., at a comparable temporal and geographic scale) were not available to these researchers. Baseline morbidity rates were held constant in all analyses. Although morbidity rates will undoubtedly change in the future in response to changes in disease management, access to preventive and chronic disease care and changing demographics (age, race/ethnicity, SES), projection of these shifts was beyond the scope of this study.
Impact assessments
One primary health outcome assessment and two sensitivity analyses were performed. The health outcomes assessment (HOA) used models of future O3 concentrations to project asthma emergency department visits resulting only from climate change with altered greenhouse gas emissions under the A2 SRES scenario. Sensitivity analyses examined alterations in two of the assumptions underlying the primary assessment.
HOA: 2020s climate change only
The objective here was to assess how climate change alone might contribute to changes in summer O3 concentrations and associated pediatric asthma emergency department visits in the New York region over the next 10–15 years. County population totals were held constant at Census 2000 levels.31 Similarly, anthropogenic O3 precursor emissions were held constant consistent with the 1996 county-level U.S. Environmental Protection Agency (EPA) National Emissions Trends inventory. Thus, no projected changes in anthropogenic precursor emissions were applied in the Community Multiscale Air Quality model projections of 2020s summer O3. The base case did allow for temperature-dependent changes in biogenic and mobile source emissions. No threshold for O3 impacts was assumed.36
Sensitivity analyses
Two sensitivity analyses were conducted to better understand the effects on projections of changing individual modeling assumptions. The first analysis, S1, included the same assumptions of the HOA model but added population growth projections. For S1 in which population was allowed to grow, 2020s populations used the county and age-specific population projections from Cornell University Program on Applied Demographics.37 This method projected a regional population increase in 2025 compared to 2000 of 3.9% among those aged 0–17 years with a range of negative 14.2% in suburban counties to positive 20% among the urban core counties.
The second analysis, S2, explored the effects of increasing anthropogenic O3-precursor emissions in addition to climate change. The first step used projections from a separate run of the climate model that included climate change and emissions changes that would be consistent with the A2 SRES story line (increases of 29.5% for all anthropogenic NOx emission sources and 9% for all anthropogenic VOC emissions). Of note, NOx and VOC have documented respiratory health effects but this model captures only O3-related impacts.38, 39 With this second set of O3 projections, isolation of the emissions effect was then possible by adding the difference of the two projections from the 2020s to the estimates of O3 from the 1990s and using those projections to model the health projections. These analyses occurred in 2010.
Results
Health outcomes assessment
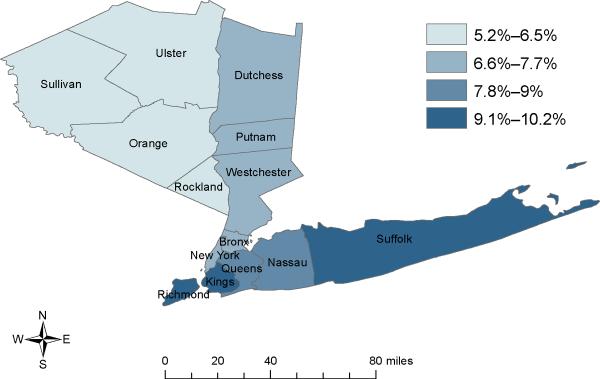
County-specific O3 concentrations and the associated pediatric morbidity projections for emergency department visits for the primary morbidity assessment (HOA) appear in Table 1. Percentage changes in emergency department visits between the 1990s and 2020s for the HOA model appear in Figure 1. The calculations of projections for O3-related asthma morbidity include the 95% CI from the epidemiologic study of Tolbert et al.21. The O3 projections for average summer daily 8-hour maximum concentrations under the HOA model – which included only climate change - increased their median by 2.7–5.3 ppb across the 14 counties. The distribution of the O3 changes shows greater increases in those counties outside the urban core toward the coast and along the predominant air mass trajectory from the southwest. As a direct result, the distribution of percentage changes for emergency department visits follows a similar pattern (Figure 1). The underlying population of each county strongly influences the absolute numbers. Median regional O3-attributable asthma pediatric emergency department visits increased 7.3% in the 2020s compared to the 1990s. This analysis suggests that projected increases in emergency department visits occur both in the surrounding metropolitan counties as well as the urban core.
Table 1.
O3-related asthma emergency department visit change for children aged 0–17 years in New York City area.
| 2020s under A2 IPCC SRES climate change scenario |
||||||
|---|---|---|---|---|---|---|
| 1990 |
(HOA) |
|||||
| County | O3 (ppb)a | O3 asthma emergency department visits | O3 (ppb) | Δ O3 | O3 asthma emergency department visits | % Δ |
| Bronx | 43.8 | 188 (111–267) | 47.0 | 3.1 | 202 (119–288) | 7.5 |
| Dutchess | 56.1 | 7 (4–10) | 59.9 | 3.8 | 8 (5–11) | 7.3 |
| Kings | 38.5 | 131 (78–187) | 41.9 | 3.3 | 143 (85–204) | 9.0 |
| Nassau | 50.9 | 32 (19–46) | 54.9 | 4.0 | 35 (20–50) | 8.2 |
| New York | 38.5 | 83 (49–118) | 41.2 | 2.7 | 89 (53–127) | 7.3 |
| Orange | 56.3 | 12 (7–18) | 59.6 | 3.4 | 13 (8–19) | 6.3 |
| Putnam | 56.3 | 1 (1–2) | 59.9 | 3.6 | 1 (1–2) | 6.8 |
| Queens | 42.1 | 93 (55–133) | 45.2 | 3.2 | 101 (60–143) | 7.9 |
| Richmond | 37.9 | 13 (8–18) | 41.5 | 3.6 | 14 (8–20) | 9.8 |
| Rockland | 54.2 | 5 (3–8) | 57.4 | 3.2 | 6 (3–8) | 6.3 |
| Suffolk | 54.7 | 46 (27–66) | 60.0 | 5.3 | 51 (30–72) | 10.2 |
| Sullivan | 54.9 | 2 (1–4) | 57.7 | 2.7 | 3 (2–4) | 5.2 |
| Ulster | 54.6 | 5 (3–7) | 57.9 | 3.3 | 5 (3–7) | 6.4 |
| Westchester | 54.1 | 30 (18–43) | 57.8 | 3.7 | 33 (19–47) | 7.2 |
|
| ||||||
| Total | 648 | 704 | Median 7.3% increase | |||
Mean summer daily 8-hour maximum O3 concentration in ppb.
HOA, Health Outcome Assessment; ppb, part per billion; IPCC SRES, Intergovernmental Pane] on Climate Change Special Report on Emissions Scenarios; O3, ozone.
Figure 1.
Percentage change in emergency department visits (2020s A2 vs 1990s baseline) within each of 14 New York state counties of metropolitan NYC modeled under the HOA with A2 SRES.
Note: HOA, health outcomes assessment; IPCC SRES, Intergovernmental Panel on Climate Change Special Report on Emissions Scenarios.
Sensitivity analyses
The results of the HOA model and the sensitivity analysis outcomes appear in Appendix B (available online at www.ajpmonline.org) which plots the median and 95th percentiles of the percentage change for emergency department visits. Sensitivity analysis S1 shows that population change accounts for the largest contribution to changes in the O3-attributable emergency department visits. This change is bidirectional as the population of those aged 0–17 years is projected to increase in urban counties – where asthma morbidity is already greatest – but decrease in some suburban counties. Including population growth projections (S1) resulted in a median of 10.6% increase in morbidity.
The second sensitivity analysis S2 isolated the effect of increased anthropogenic O3-precursor emissions. In the first step of this sensitivity analysis, the O3 projections from the model run that included both climate change and increased emissions showed a greater range by county but the median increase in asthma emergency department visits was only 6.5%. The isolated emissions effect when climate change effect was removed also showed decreased emergency department visit projections compared to the HOA projections. This result occurred because of decreases in projected O3 concentrations for most of the urban metropolitan counties in this model, a result of air pollutant interactions that can cause O3 to decrease in areas where there are higher concentrations of other pollutants such as NOx.10 The median O3-related asthma emergency department visits in the S2 analysis was decreased by 0.4%.
Discussion
The results of this assessment suggest that, compared to the 1990s, by the 2020s climate change could cause a median increase of 7.3% in regional summer O3-related asthma emergency department visits for children aged 0–17 years across the New York City metropolitan region. However, when examining individual counties, O3-related emergency department increases ranged from 5.2% to 10.2%. Actual O3 precursor emissions have been decreasing as opposed to increasing – as detailed by U.S. EPA40 - and updated precursor emissions assumptions would be useful in future analyses. A sensitivity analysis demonstrated the sometimes counterintuitive effects of air pollution dynamics. As with previous health-impact assessments using these climate models, these O3 simulations did not account for O3 precursor emission effects from outside of the modeled region (Eastern U.S.) on future air quality dynamics within the study area.10, 41
The assumption of uniform exposure to ozone within each county and the application of a single ERC to children of all ages are two other significant limitations of this study. Other U.S. studies have shown variable associations of O3 and asthma emergency department visits18, 42, 43 with a range of RR from 0.98 to 1.06 per 20 ppb increase in daily maximum 8-hour O3. These studies included a mixture of pediatric and adult patients and used lags ranging from 0 to 3 days. The study by Peel et al.42 included the same data as Tolbert et al. but included all ages and the association was not significant. Confounding by other air pollutants and choice of lag days are discussed more fully within the original article and subsequent articles published by those same researchers.21, 42, 44
In addition, the ERC came from a study in Atlanta, not New York, because of its availability as an age-matched study for asthma emergency department visits. To the extent that air conditioning is more prevalent in Atlanta than in New York (98% versus 85% according to 2003 and 2004 American Housing Survey data),45 effects of O3 would likely be lower in Atlanta, since O3 penetrates indoors only partially in the presence of air conditioning.46 In this regard, the health-impacts modeling presented here is conservative. However, populations can adapt to climate through behavior changes such as increased time indoors or purchase of air conditioning units. Thus, levels of New York air conditioning use could match those of Atlanta in the future as the climate warms in which case such an ERC is arguably appropriate for projection of future health effects.
In a sensitivity analysis, an examination was made of the additional impact on future morbidity resulting from plausible increases in the exposed population. However, no examination was made of any scenarios of changing baseline morbidity rates, due to the high level of uncertainty regarding such estimates. It should be noted that projected cases scale directly to the baseline rate; thus a reduction by 50% in the baseline for asthma emergency department use would result in a 50% reduction in projected O3-related cases.
Prior modeling exercises similar to this one have mainly used mortality as an outcome; few have addressed morbidity or the unique vulnerabilities of children.8, 47, 48 Another strength of this particular assessment is the use of county-specific inputs. Other pediatric respiratory effects have been well documented to be associated with O3 changes such as increased asthma hospitalization,16 asthma medication use,49 increased symptoms,50, 51 and increased missed school days.52 These additional documented health effects from O3 as well as a narrow definition for the baseline rates (i.e., excluding diagnoses of wheezing in young children) make these projections inherently conservative regarding the overall burden of disease from O3. Because the development of the chronic asthma phenotype is a function of both genotype and environmental insults,2, 53 the future incidence of asthma exacerbations and likely also emergency department visits will change as a function of the changing prevalence of chronic asthma (due in part to increased O3) as well as the increased rate of O3-induced exacerbations.
Clearly, this model simplifies complex relationships among change in climate, O3 precursors, population growth, asthma prevalence, healthcare utilization and the exposure-risk coefficient of O3 and this specific outcome of asthma. Ethnicity and SES are important risk factors of uncontrolled asthma such is signaled by emergency department visits and are only indirectly included as part of the baseline morbidity estimates.23 Improvements of these projections would include more geospatially refined and updated data for all of the above as well as different regional population and urbanization growth patterns, more current climate models – as will be used in the 2013 release of the IPCC's 5th Assessment Report, inclusion of bioaerosols such as pollen and other allergens, and additional scenarios beyond the single A2 SRES one used in this study.
Given that the projections of this single outcome of asthma emergency department visits are small in absolute number, the costs would not be expected to be staggering. However, given that a single asthma emergency department visits often represents far more uncontrolled asthma cases with associated increase in outpatient visits, medication use and indirect costs such as missed school days for children and work days for parents, the combined costs would be much greater.16, 22
Conclusion
These projected effects add an important contribution to current research regarding climate-related disease in children. As the first model of climate-related, regional, pediatric morbidity, this study not only demonstrates an important modeling approach but also provides some quantitative projections to which future work can add and compare. Adaptation measures to climate change that work to reduce ozone levels should be coupled with ongoing efforts for better disease management of asthma. The projections from this study can inform the discussion of local, regional and national policy.
Supplementary Material
Acknowledgements
Dr. Sheffield received support from the NIH Research Training Program in Environmental Pediatrics (NIH #5T32 HD049311). Dr. Kinney is supported by NIEHS Center grant ES09089. This work was also partially supported by EPA STAR grant R-82873301. The authors extend their gratitude to Philip J. Landrigan for his assistance in enabling this research to happen, Jessie L. Carr for her geographic technology expertise, and Christian Hogrefe of the Atmospheric Sciences Research Center at the University at Albany in New York for his guidance on interpreting the climate models.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the U.S., 1980–2007. Pediatrics. 2009;123(Suppl 3):S131–45. doi: 10.1542/peds.2008-2233C. [DOI] [PubMed] [Google Scholar]
- 2.Lemanske RF, Jr., Busse WW. Asthma: clinical expression and molecular mechanisms. J Allergy Clin Immunol. 2010;125(2 Suppl 2):S95–102. doi: 10.1016/j.jaci.2009.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Campbell-Lendrum D, Bertollini R, Neira M, Ebi K, McMichael A. Health and climate change: a roadmap for applied research. Lancet. 2009;373(9676):1663–5. doi: 10.1016/S0140-6736(09)60926-0. [DOI] [PubMed] [Google Scholar]
- 4.Frumkin H, McMichael AJ. Climate change and public health: thinking, communicating, acting. Am J Prev Med. 2008;35(5):403–10. doi: 10.1016/j.amepre.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 5.Shea KM. Global climate change and children's health. Pediatrics. 2007;120(5):1149–52. doi: 10.1542/peds.2007-2645. [DOI] [PubMed] [Google Scholar]
- 6.Epstein PR. Climate change and human health. N Engl J Med. 2005;353(14):1433–6. doi: 10.1056/NEJMp058079. [DOI] [PubMed] [Google Scholar]
- 7.Wiley LF, Gostin LO. The international response to climate change: an agenda for global health. JAMA. 2009;302(11):1218–20. doi: 10.1001/jama.2009.1381. [DOI] [PubMed] [Google Scholar]
- 8.Bell ML, Goldberg R, Hogrefe C, Kinney PL, Knowlton K, Lynn B, et al. Climate change, ambient ozone, and health in 50 U.S. cities. Climatic Change. 2007;82:61–76. [Google Scholar]
- 9.Knowlton K, Lynn B, Goldberg RA, Rosenzweig C, Hogrefe C, Rosenthal JK, et al. Projecting heat-related mortality impacts under a changing climate in the New York City region. Am J Public Health. 2007;97(11):2028–34. doi: 10.2105/AJPH.2006.102947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knowlton K, Rosenthal JE, Hogrefe C, Lynn B, Gaffin S, Goldberg R, et al. Assessing ozone-related health impacts under a changing climate. Environ Health Perspect. 2004;112(15):1557–63. doi: 10.1289/ehp.7163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McMichael A, Campbell-Lendrum DH, Kovats RS, Edwards S, Wilkinson P, Wilson T, et al. Global Climate Change. In: Ezzati M, Lopez A, Rodgers A, Murray C, editors. Comparative Quantification of Health Risks: Global and Regional Burden of Disease due to Selected Major Risk Factors. WHO; Geneva: 2004. pp. 1543–1649. [Google Scholar]
- 12.WHO Global Burden of Disease 2004 Update. 2008 [cited 2010 1 February]; Available from: http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf.
- 13.Kinney PL. Climate change, air quality, and human health. Am J Prev Med. 2008;35(5):459–67. doi: 10.1016/j.amepre.2008.08.025. [DOI] [PubMed] [Google Scholar]
- 14.Etzel RA, Balk SJ, editors. Pediatric Environmental Health. 2nd ed. American Academy of Pediatrics; Elk Grove Village, IL: 2003. [Google Scholar]
- 15.American Academy of Pediatrics Committee on Environmental Health Ambient air pollution: respiratory hazards to children. Pediatrics. 1993;91(6):1210–3. [PubMed] [Google Scholar]
- 16.Trasande L, Thurston GD. The role of air pollution in asthma and other pediatric morbidities. J Allergy Clin Immunol. 2005;115(4):689–99. doi: 10.1016/j.jaci.2005.01.056. [DOI] [PubMed] [Google Scholar]
- 17.Friedman MS, Powell KE, Hutwagner L, Graham LM, Teague WG. Impact of changes in transportation and commuting behaviors during the 1996 Summer Olympic Games in Atlanta on air quality and childhood asthma. JAMA. 2001;285(7):897–905. doi: 10.1001/jama.285.7.897. [DOI] [PubMed] [Google Scholar]
- 18.Jaffe DH, Singer ME, Rimm AA. Air pollution and emergency department visits for asthma among Ohio Medicaid recipients, 1991–1996. Environ Res. 2003;91(1):21–8. doi: 10.1016/s0013-9351(02)00004-x. [DOI] [PubMed] [Google Scholar]
- 19.Stieb DM, Burnett RT, Beveridge RC, Brook JR. Association between ozone and asthma emergency department visits in Saint John, New Brunswick, Canada. Environ Health Perspect. 1996;104(12):1354–60. doi: 10.1289/ehp.961041354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tenias JM, Ballester F, Rivera ML. Association between hospital emergency visits for asthma and air pollution in Valencia, Spain. Occup Environ Med. 1998;55(8):541–7. doi: 10.1136/oem.55.8.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tolbert PE, Mulholland JA, MacIntosh DL, Xu F, Daniels D, Devine OJ, et al. Air quality and pediatric emergency room visits for asthma in Atlanta, Georgia, USA. Am J Epidemiol. 2000;151(8):798–810. doi: 10.1093/oxfordjournals.aje.a010280. [DOI] [PubMed] [Google Scholar]
- 22.Bahadori K, Doyle-Waters MM, Marra C, Lynd L, Alasaly K, Swiston J, et al. Economic burden of asthma: a systematic review. BMC Pulm Med. 2009;9:24. doi: 10.1186/1471-2466-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sawicki GS, Vilk Y, Schatz M, Kleinman K, Abrams A, Madden J. Uncontrolled asthma in a commercially insured population from 2002 to 2007: trends, predictors, and costs. J Asthma. 2010;47(5):574–80. doi: 10.3109/02770901003792841. [DOI] [PubMed] [Google Scholar]
- 24.Hogrefe C, Biswas J, Lynn B, Civerolo K, Ku J-Y, Rosenthal J, et al. Simulating regional-scale ozone climatology over the eastern U.S.: model evaluation results. Atmos Environ. 2004;38:2627–2638. [Google Scholar]
- 25.Hogrefe C, Lynn B, Civerolo K, Ku J-Y, Rosenthal J, Rosenzweig C, et al. Simulating changes in regional air pollution over the eastern U.S. due to changes in global and regional climate and emissions. J. Geophys. Res. 2004;109:D22301. [Google Scholar]
- 26.Lynn BH, Rosenzweig C, Goldberg R, Rind D, Hogrefe C, Druyan L, et al. Testing GISSMM5 physics configurations for use in regional impacts studies. Climatic Change. 2010;99:567–587. [Google Scholar]
- 27.Kinney PL, Rosenthal J, Knowlton K, Rosenzweig C, R. G. Assessing Potential Public Health and Air Quality Impacts of Changing Climate and Land Use in Metropolitan New York. In: Rosenthal J, Kinney PL, Knowlton K, editors. New York Climate and Health Project. Columbia Earth Institute; New York: 2004. al. e. al. e. [Google Scholar]
- 28.Nakicenovic N, Swart R, editors. Special Report on Emissions Scenarios. Cambridge University Press; Cambridge, UK: 2000. [Google Scholar]
- 29.U.S. EPA (Environmental Protection Agency) Ozone Air Quality Standards. 2010 [cited 2010 February]; Available from: http://www.epa.gov/air/ozonepollution/standards.html.
- 30.DHHS . The International Classification of Diseases, 9th Revision. Washington, D.C.: 1991. [Google Scholar]
- 31.U.S. Census Bureau Profiles of General Demographic Characteristics (DP-1): 2000 Census of Population and Housing. 2001 [cited 2009 November]; Available from: http://www.census.gov/prod/cen2000/
- 32.NYS DOH (NYS Department of Health) New York State Asthma Surveillance Summary Report. 2007 [cited 2009 November]; Available from: http://www.health.state.ny.us/statistics/ny_asthma/pdf/2007_asthma_surveillance_summary_ report.pdf.
- 33.Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. Asthma and wheezing in the first six years of life. The Group Health Medical Associates. N Engl J Med. 1995;332(3):133–8. doi: 10.1056/NEJM199501193320301. [DOI] [PubMed] [Google Scholar]
- 34.Taussig LM, Wright AL, Holberg CJ, Halonen M, Morgan WJ, Martinez FD. Tucson Children's Respiratory Study: 1980 to present. J Allergy Clin Immunol. 2003;111(4):661–75. doi: 10.1067/mai.2003.162. quiz 676. [DOI] [PubMed] [Google Scholar]
- 35.Lin RY, Pitt TJ, Lou WY, Yi Q. Asthma hospitalization patterns in young children relating to admission age, infection presence, sex, and race. Ann Allergy Asthma Immunol. 2007;98(2):139–45. doi: 10.1016/S1081-1206(10)60686-2. [DOI] [PubMed] [Google Scholar]
- 36.Bell ML, Peng RD, Dominici F. The exposure-response curve for ozone and risk of mortality and the adequacy of current ozone regulations. Environ Health Perspect. 2006;114(4):532–6. doi: 10.1289/ehp.8816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.PAD (Program on Applied Demographics) PAD projections from Cornell University College of Human Ecology. 2009 [cited 2009 September]; Available from: http://www.human.cornell.edu/che/BLCC/pad/data/projections.cfm.
- 38.Delfino RJ, Gong H, Linn WS, Hu Y, Pellizzari ED. Respiratory symptoms and peak expiratory flow in children with asthma in relation to volatile organic compounds in exhaled breath and ambient air. J Expo Anal Environ Epidemiol. 2003;13(5):348–63. doi: 10.1038/sj.jea.7500287. [DOI] [PubMed] [Google Scholar]
- 39.U.S. EPA . Integrated Science Assessment for Oxides of Nitrogen - Health Criteria (Final Report) Washington, DC: 2008. [Google Scholar]
- 40.U.S. EPA . Final Ozone NAAQS Regulatory Impact Analysis. EPA-452/R-08-003. U.S. Environmental Protection Agency; Research Triangle Park, North Carolina: 2008. [Google Scholar]
- 41.Kinney PL, Knowlton K, Hogrefe C. Ozone, Kinney, et al. Respond. Environmental health perspectives. 2005;113:A87. [Google Scholar]
- 42.Peel JL, Tolbert PE, Klein M, Metzger KB, Flanders WD, Todd K, et al. Ambient air pollution and respiratory emergency department visits. Epidemiology. 2005;16(2):164–74. doi: 10.1097/01.ede.0000152905.42113.db. [DOI] [PubMed] [Google Scholar]
- 43.Wilson AM, Wake CP, Kelly T, Salloway JC. Air pollution, weather, and respiratory emergency room visits in two northern New England cities: an ecological time-series study. Environ Res. 2005;97(3):312–21. doi: 10.1016/j.envres.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 44.Tolbert PE, Klein M, Peel JL, Sarnat SE, Sarnat JA. Multipollutant modeling issues in a study of ambient air quality and emergency department visits in Atlanta. J Expo Sci Environ Epidemiol. 2007;17(Suppl 2):S29–35. doi: 10.1038/sj.jes.7500625. [DOI] [PubMed] [Google Scholar]
- 45.U.S. Census Bureau Housing and Household Economic Statistics Division American Housing Survey (AHS) 2008 [cited 2010 8 November]; Available from: http://www.census.gov/hhes/www/housing/ahs/ahs.html.
- 46.Blondeau P, Iordache V, Poupard O, Genin D, Allard F. Relationship between outdoor and indoor air quality in eight French schools. Indoor Air. 2005;15(1):2–12. doi: 10.1111/j.1600-0668.2004.00263.x. [DOI] [PubMed] [Google Scholar]
- 47.Patz JA, Campbell-Lendrum D, Holloway T, Foley JA. Impact of regional climate change on human health. Nature. 2005;438(7066):310–7. doi: 10.1038/nature04188. [DOI] [PubMed] [Google Scholar]
- 48.Sheffield PE, Landrigan PJ. Global Climate Change and Children's Health: Threats and Strategies for Prevention. Environ Health Perspect. 2010 doi: 10.1289/ehp.1002233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Millstein J, Gilliland F, Berhane K, Gauderman WJ, McConnell R, Avol E, et al. Effects of ambient air pollutants on asthma medication use and wheezing among fourth-grade school children from 12 Southern California communities enrolled in The Children's Health Study. Arch Environ Health. 2004;59(10):505–14. doi: 10.1080/00039890409605166. [DOI] [PubMed] [Google Scholar]
- 50.Gent JF, Triche EW, Holford TR, Belanger K, Bracken MB, Beckett WS, et al. Association of low-level ozone and fine particles with respiratory symptoms in children with asthma. JAMA. 2003;290(14):1859–67. doi: 10.1001/jama.290.14.1859. [DOI] [PubMed] [Google Scholar]
- 51.Triche EW, Gent JF, Holford TR, Belanger K, Bracken MB, Beckett WS, et al. Low-level ozone exposure and respiratory symptoms in infants. Environ Health Perspect. 2006;114(6):911–6. doi: 10.1289/ehp.8559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gilliland FD, Berhane K, Rappaport EB, Thomas DC, Avol E, Gauderman WJ, et al. The effects of ambient air pollution on school absenteeism due to respiratory illnesses. Epidemiology. 2001;12(1):43–54. doi: 10.1097/00001648-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 53.Martinez FD. Genes, environments, development and asthma: a reappraisal. Eur Respir J. 2007;29(1):179–84. doi: 10.1183/09031936.00087906. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.