Abstract
Purpose
To examine the associations between adverse interpersonal relationship histories experienced during adolescence and health in young adulthood in a large, nationally representative sample.
Methods
Using data from Waves I, II and III of the National Longitudinal Study of Adolescent Health, multiple adverse relationship experiences are examined, including high loneliness, low perceived parental support, frequent transitions in romantic relationships (relationship instability), exposure to intimate partner violence, and loss by death of important relationship figures. These histories are assessed, both individually and in a relationship risk index, as predictors of self-reported general health and depressive symptoms at Wave III (ages 18 to 27), controlling for baseline (Wave I) health and for demographic and health behavior covariates.
Results
Net of baseline health and covariates, each type of relationship risk (experienced between Wave I and Wave III) was related to either depression or general health at Wave III, with the strongest effects seen for exposure to intimate partner violence. In addition, a cumulative relationship risk index examining the extent to which youth experienced high levels of multiple relationship risk factors revealed that each additional adverse relationship experience increased the odds of reporting poor mental and general health at Wave III, with increases occurring in an additive manner.
Conclusions
Multiple types of adverse relationship experiences predicted increases in poor general health and depressive symptoms from adolescence to early adulthood. Consistent with a cumulative risk hypothesis, the more types of adverse relationship experiences a youth experienced, the worse their young adult health outcomes.
Introduction
Humans are social beings; social relationships play a central role in our lives. From infancy onward, we depend on others to help meet basic needs of sustenance, shelter and protection, to provide instrumental and emotional support, to serve as sources of companionship, comfort and pleasure, and as partners in childbearing and childrearing. Developing and maintaining positive social relationships are among the most important developmental tasks of infancy, childhood and adolescence [1]. Not surprisingly, variations in social relationship experiences have been related to individual differences in emotional and physical health [2–4]. Social relationships are thought to affect health via multiple pathways, including: direct impacts on negative and positive affect; changes in perceptions of and responses to stressors; impacts on stress-sensitive biological systems; and changes in health behaviors [5, 6].
Much of the prior research on social relationships and health has focused on the positive side of social relationships – the stress-buffering and health-promoting role of strong social supports and integration within large social networks [3, 5]. Yet, theoretical models have also proposed direct negative effects of adverse social experiences on health [5–7]. Taking a “cumulative relationship risk” approach, we argue that cumulative exposure to multiple adverse relationship experiences may be particularly deleterious for health. We also argue that certain types of adverse relationship experiences are most likely to be related to poor health -- those that are directly threatening to the social or physical self [8]. Here, we focus on high perceived loneliness, low parental support, instability in romantic relationships, violence in intimate relationships, and loss by death of important relationship figures. Before elaborating our hypotheses, we briefly discuss existing research on each of these relationship risks and emotional and physical health.
Loneliness
Loneliness, or the perceived absence of supportive social relationships, has recently emerged as a key variable predicting health [9]. Loneliness has been linked to depression, nausea, headaches, and eating disturbances [9, 10], sleep disturbances [11], and poorer immune and cardiovascular functioning [9, 12]. In addition, loneliness has been found to activate biological stress processes [13] and contribute to poorer health practices [14], providing several mechanisms by which loneliness may influence emotional and physical health outcomes.
Low Parental Support
In addition to providing for basic material and physical needs, parents play a central role in regulating the affect, behavior and physiology of their children [4]. The presence of a sensitive caregiver can buffer physiological responses to stressful events [4, 15], while the absence of warm and sensitive parenting, and exposure to parental anger or conflict are associated with physiological dysregulation [16, 17]. In theoretical models of the family environment and health, such as the “Risky Families Model” [7], low levels of parental support are hypothesized to be a major causal contributor to emotional and physical health problems in adulthood.
Romantic Relationship Instability
Recent theory and research has pointed to relationship instability as a contributor to negative outcomes in adolescents. For example, frequent changes in parent figures have been related to emotional, behavioral and physical health problems [18, 19]. There has been less research on the effects of instability in adolescent romantic relationships on health, although studies have linked adolescent romantic break ups to increased depressive symptoms [20]. Whether romantic relationship instability predicts physical health outcomes has not to our knowledge been examined.
Intimate Partner Violence (IPV)
IPV is defined as physical, sexual, and perceived emotional abuse within a romantic relationship [21]. IPV has been associated with depression and post-traumatic stress disorder [22, 23], and a wide range of physical health conditions including: chronic pain, arthritis, severe headaches; gastrointestinal disorders; and cardiovascular problems [24–26]. Some of these effects are mediated by the chronic stress and fear associated with IPV. Given that IPV threatens both the physical and the social self, we expect it to be a strong predictor of ill health.
Loss/Bereavement
A large body of evidence has linked the experience of loss or bereavement with emotional, behavioral, and physical health problems [27–29]. Increased rates of major depression have been found among adolescents who were exposed to a friend's suicide [27] or the death of a parent [28]. Bereaved children also experience greater somatic symptoms such as gastrointestinal problems, stomachaches, and headaches [30]. Bereavement has been linked to short-term dysregulation of neuroendocrine and immune systems, but limited evidence exists on the long-term physical health consequences of childhood or adolescent bereavement [31–33].
Cumulative Relationship Risk
While each of the relationship risks described above have been individually related to health in separate studies, we hypothesize that an accumulation of these risks will be particularly deleterious for mental and physical health. Rather than being singly determined, adverse outcomes are thought to be best predicted by the number of risk factors present [34, 35]. We will examine whether youth exposed to multiple relationship risks are at higher risk for negative emotional and health outcomes in young adulthood, controlling for baseline health and demographic and health behavior covariates.
Methods
Procedures and Participants
Our data come from the first three waves of the National Longitudinal Study of Adolescent Health (Add Health), which measures adolescents' social, economic, psychological and physical well-being and contextual data on family, neighborhood, community, school, friendships and romantic relationships. Add Health is a nationally representative, probability-based longitudinal survey of adolescents in grades 7–12 in the United States in 1995 [36]. It used a multistage, stratified, school-based clustered sampling design with 80 schools selected with probability proportional to size [37].
Wave I (1994–1995) included 20,745 adolescents (aged 11–20) and their parents. All adolescents in grade 7 through 11 in Wave I (but not those in grade 12) were targeted about one year later for the Wave II interview (n=14,738). Wave III took place from 2000–2001 (ages 18–27, n=15,197), targeting all respondents from Wave I. Our final analytical sample (n=10,149) included respondents who participated in all three waves, were in grades 7–11 at Wave I, and had valid sampling weights. Approval was obtained from the Northwestern University Institutional Review Board to conduct secondary analyses of the Add Health data.
Measures
Health Outcomes
Our dependent variables were measures of self-reported general health and mental health (depressive symptoms) at Wave III. General health was assessed from the question, “In general, how is your health?” (response choices included excellent=1; very good=2; good=3; fair=4; poor=5). A depressive symptoms scale was created by taking the mean of the following items from the Center for Epidemiological Studies Depression Scale [38]: felt blue; bothered by things that don't usually bother you; frequent crying; felt depressed, had trouble keeping mind on things; did not enjoy life; did not feel just as good as other people; felt disliked by people; felt sad; and felt too tired to do things (never/rarely; sometimes; a lot of the time; most/all of the time; α=0.79).
Adverse Interpersonal Relationship Experiences
Adverse relationship experiences were measured at Waves I and II, and in the case of the romantic relationship history and loss variables, retrospectively at Wave III.
Loneliness/Perceived Social Acceptance
Loneliness was measured on a 4 point scale reflecting how often respondents reported feeling lonely (never or rarely; sometimes; a lot of the time; most or all of the time), averaged across Waves I and II. Perceived social acceptance was measured by averaging responses, on a 5-point scale from strongly disagree to strongly agree, across Waves I and II to: “Do you feel socially accepted?” and “Do you feel loved and wanted?” Loneliness and acceptance measures were examined separately because they were only moderately correlated (r = −0.37).
Parental Support
A parental support scale was created by averaging responses (on a 5 point scale, with 5 indicating high support) to the following questions in Wave I and II: “how close do you feel with your mom/dad; how much does your mom/dad care about you; is your mom/dad warm and loving towards you; when you do something wrong, does your mom/dad talk with you to understand; are you satisfied with your communication with mom/dad; are you satisfied with your relationship with mom/dad”. Scales were created separately for mothers and fathers in each wave (mother: WI α=0.84, WII α=0.83; father: WI α=0.88, WII α=0.87) and then averaged across waves.
Romantic Relationship Instability
In Wave III, participants were asked to provide a list of romantic relationships experienced since 1995. Detailed relationship questions, including onset and offset dates, were asked for relationships that were sexual, rated by Add Health as important, or part of the Add Health couples sample. We calculated the number of romantic relationships transitions after the age of 16 that each respondent reported between Waves I and III. A dummy variable indicated those with “0” transitions because they had not yet initiated romantic relationships.
Intimate Partner Violence (IPV)
IVP is a binary measure of ever having experienced violent actions from an important romantic partner as reported in the Wave III detailed relationships section. Four questions on frequency of violent acts were asked of participants' two most important1 romantic relationships: (1) partner threatened, pushed or shoved, or thrown something at you; (2) partner slapped, hit, or kicked you; (3) partner insisted on or made you have sexual relations with him/her; and (4) had an injury, such as sprain, bruise, or cut, because of a fight with partner.
Loss
This binary variable indicates whether the participant experienced the loss of one or more of significant relationship figures between Waves I and III. This measure focused on the death of people who are most important in the life of the respondent: biological parents, residential parents, friends, and partners/spouses.
Cumulative Relationship Risk Index (CRRI)
We created a count variable that indicated how many relationship risks the participant had experienced. Being in the highest quartile of loneliness and/or the lowest quartile of accepted/loved added one to the count, as did being in the lowest quartile on the perceived parental support measure, the highest quartile for romantic relationship instability, ever having experienced IPV, or ever having experienced the loss of one or more close loved ones. Scores ranged from 0 to 5. From these, we created dummy variables reflecting having experienced 0, 1, 2, 3 and 4 or more relationship risks.
Demographic and Health Covariates
Basic demographic data were measured, including age, gender, race-ethnicity, parental marital status and education, participants' marital/relationship status, and race/ethnicity (Table 1). Parental education served as a proxy for socioeconomic status, due to high levels of missing data on income, and was created using the higher level of mother's or father's education. Pre-existing physical and mental conditions were measured at Wave I, including self-reported general health, asthma, heart problems, physical limitations, body mass index, depressive symptoms, low birth weight, and an index of nonspecific somatic symptoms (e.g. headaches, aches, pains, soreness). Health behaviors at Wave II, including frequency of physical exercise in the past week, whether the youth smoked cigarettes in the past month, frequency of fast food consumption in the past week, and whether the youth binge drank (had five drinks or more in row) in the past year, were included as covariates/potential mediators.
Table 1.
Weighted Descriptive Statistics for Poor Health, Depressive Symptoms, Relationship Risk Variables and Covariates.
| Full Sample (N=10,828) | Male (N=4,791) | Female (N=5,358) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Mean or % | SD | High Riskab | Mean or % | SD | High Risk | Mean or % | SD | High Risk |
| Relationship Risk | |||||||||
| Perceived loneliness | .425 | .554 | 22.8% | .350 | .484 | 18.5% | .500 | .612 | 27.3% |
| Perceived social acceptance | 4.227 | .549 | 19.6% | 4.273 | .516 | 17.3% | 4.180 | .580 | 22.0% |
| Perceived parental support | 4.322 | .559 | 24.1% | 4.388 | .484 | 19.4% | 4.256 | .625 | 29.0% |
| Romantic relationship instability (#transitions/year) | .358 | .429 | 29.5% | .362 | .429 | 30.0% | .354 | .429 | 29.1% |
| Ever experienced intimate partner violence | .317 | .463 | 31.7% | .283 | .432 | 28.3% | .350 | .489 | 35.0% |
| Ever experienced loss of a loved one | .083 | .275 | 8.3% | .075 | .254 | 7.5% | .091 | .296 | 9.1% |
| Outcome Variables WIII | |||||||||
| General health (higher score reflects worse health) | 2.011 | .886 | 1.928 | .817 | 2.096 | .907 | |||
| Average depressive symptoms | .507 | .449 | .457 | .396 | .557 | .497 | |||
| Wave I Health and Demographic Controls | |||||||||
| Baseline general health | 2.133 | .889 | 2.036 | .858 | 2.191 | .934 | |||
| Baseline average depressive symptoms | .568 | .390 | .519 | .338 | .617 | .436 | |||
| Baseline Body Mass Index | 22.228 | 4.497 | 22.407 | 4.368 | 22.042 | 4.625 | |||
| Baseline age | 14.93 | 1.542 | 15.02 | 1.526 | 14.85 | 1.550 | |||
| Baseline symptom count | 7.310 | 6.478 | 6.656 | 5.428 | 7.972 | 7.418 | |||
| Baseline physical limitations | 2.3% | .148 | 2.1% | .138 | 2.5% | .159 | |||
| Baseline asthma | 2.3% | .148 | .2% | .047 | .5% | .072 | |||
| Baseline cardiac abnormality | .1% | .034 | .1% | .029 | .1% | .039 | |||
| Race/Ethnicity | |||||||||
| Non-Hispanic Black | 15.1% | .357 | 14.7% | .341 | 15.6% | .373 | |||
| Hispanic | 11.9% | .323 | 12.2% | .316 | 11.6% | .329 | |||
| Non-Hispanic Native American | .8% | .089 | .9% | .093 | .6% | .079 | |||
| Non-Hispanic Asian/Pacific Islander | 3.7% | .187 | 4.1% | .191 | 3.2% | .182 | |||
| Non-Hispanic White | 67.7% | .466 | 67.2% | .453 | 68.2% | .478 | |||
| Non-Hispanic other race | .8% | .089 | .9% | .091 | .7% | .086 | |||
| Baseline family structure | |||||||||
| Two biological parents | 57.2% | .493 | 57.4% | .477 | 57.0% | .509 | |||
| Two parents (1 biological) | 16.5% | .370 | 16.5% | .359 | 16.4% | .380 | |||
| Single mother | 19.5% | .395 | 18.7% | .376 | 20.4% | .414 | |||
| Single father | 2.9% | .168 | 3.5% | .178 | 2.3% | .156 | |||
| Other family structure | 3.9% | .192 | 3.8% | .186 | 3.9% | .199 | |||
| Baseline parent education | |||||||||
| Less than high school | 13.7% | .343 | 13.5% | .330 | 14.0% | .356 | |||
| High School or GED | 30.0% | .457 | 29.6% | .441 | 30.4% | .472 | |||
| Some College | 20.40% | .401 | 19.50% | .382 | 21.30% | .420 | |||
| College | 22.9% | .419 | 24.2% | .414 | 21.6% | .423 | |||
| More than college | 11.0% | .312 | 10.9% | .301 | 11.2% | .323 | |||
| Marital status | |||||||||
| Married | 13.6% | .341 | 9.8% | .287 | 17.4% | .390 | |||
| Remarried | .3% | .051 | .1% | .036 | .4% | .064 | |||
| Divorced | 1.6% | .123 | 1.3% | .107 | 1.9% | .139 | |||
| Cohabitating | 15.4% | .360 | 14.0% | .335 | 16.8% | .384 | |||
| Widowed | .02% | .014 | 0% | .000 | .04% | .020 | |||
| Single | 69.5% | .495 | 75.0% | .418 | 63.8% | .493 | |||
| Wave II Health Behavior Controls | |||||||||
| Frequency of physical exercise in last week | 4.949 | 2.537 | 5.402 | 2.443 | 4.490 | 2.546 | |||
| Days ate at fast food restaurant in past week | 2.145 | 1.759 | 2.239 | 1.728 | 2.049 | 1.781 | |||
| Smoked cigarettes in the past 30 days | 32.5% | .467 | 31.6% | .449 | 33.3% | .484 | |||
| Binge drank in the past year (5 or more drinks in a row) | 27.9% | .447 | 30.1% | .443 | 25.7% | .449 | |||
High risk cut points were: >=.5 for loneliness, <4 for social acceptance, <=4 for perceived parental support, and 1 (ever having experienced) for loneliness and loss.
High risk cut points do not result in exact quartiles for the continuous variables due to large numbers of participants falling at the quartile-dividing scores.
Analytic Plan
All continuous predictors were standardized prior to analyses. We first examined bivariate associations between health outcomes and relationship risk variables. We then used ordinary least squares (OLS) regression for the continuous depressive symptoms outcome, and ordered logistic regression for the five-level general health outcome, to examine whether each of the individual relationship risk variables contributed to health outcomes at Wave III, controlling for baseline health and demographic covariates. Next, we tested whether cumulative relationship risk was more predictive than the individual risk variables by adding the cumulative relationship risk dummy variables. For all models, we tested interactions between the relationship risk variables and gender, to examine whether effects were similar for males and females, and tested whether the relationship risk effects remained after including Wave II health behaviors. Item-level missing data were replaced with the mean of other items in a scale/measure. Missing scale-level continuous data were handled by replacement with the population mean and inclusion of missing data dummy variables [39]. For Wave I categorical health controls, missing values were assigned the modal value. Listwise deletion was used for missing data on outcome variables and for age, race, and other demographic variables. Analyses were weighted using Add Health longitudinal sampling weights, which adjust for complex sample design, selection, and non-response [40].
Results
Descriptive statistics
On average, participants rated their health to be very good and had relatively low levels of depressive symptoms (Table 1). Despite experiencing relatively low levels of risk on each variable (see means/proportions in Table 1), less than a third of respondents (29%) scored zero on our risk index. A slightly larger proportion, (34%) experienced one relationship risk, 24% encountered two risks, 10% encountered three risks, and only 3% were in the four or more risk category. As illustrated in Table 1, females were exposed, on average, to a slightly larger number of relationship risks than males (1.34 vs. 1.10 risks, respectively, t= −9.13, p <.001). Chi-squared tests of independence showed that females were significantly more likely to fall in the high risk category for all the relationship risk variables except romantic relationship instability.
Correlations among relationship risk variables and health outcomes
Poor health and depressive symptoms were significantly positively correlated (Table 2). In addition, poor health was significantly positively correlated with loneliness, intimate partner violence, and loss and negatively correlated with feeling accepted or loved and perceived parental support. Depressive symptoms were significantly positively correlated with loneliness, romantic relationship violence and loss, and negatively correlated with feeling accepted or loved, and perceived parental support.
Table 2.
Intercorrelation Table of Poor Health, Depressive Symptoms and Relationship Risk Main Independent Variables (N=10010).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. General healtha | 1 | |||||||
| 2. Depressive symptoms | .260*** | 1 | ||||||
| 3. Loneliness | .139*** | .265*** | 1 | |||||
| 4. Social acceptance | −.181*** | −.210*** | −.361*** | 1 | ||||
| 5. Parental support | −.144*** | −.182*** | −.293*** | .491*** | 1 | |||
| 6. Romantic relationship instability | .017 | −.029 | −.032* | .016 | −.007 | 1 | ||
| 7. Ever experienced relationship violence | .106*** | .160*** | .068*** | −.073*** | −.120*** | .135*** | 1 | |
| 8. Ever experienced loss | .033* | .037** | .038** | −.026 | −.031* | −.015 | .012 | 1 |
Notes:
p<.05
p<.01
p<.001.
Intercorrelations used Bonferonni adjusted significance levels.
Higher scores indicate worse health
Multivariate associations between relationship risks and health outcomes
Table 3 shows results from multivariate models examining the effect of each relationship risk variable on general health and depressive symptoms while controlling for the other relationship risk variables, baseline health and demographic covariates. Each of the relationship risk predictors made a unique contribution to predicting at least one of the two health outcomes (all p <.05, except loss, p<.10).
Table 3.
Ordered Logit predicting poor health and OLS Regressions predicting depressive symptoms at Wave III from cumulative relationship risk independent variables and controls.
| General Healtha (N=9850) | Depressive Symptoms (N=9798) | |||||
|---|---|---|---|---|---|---|
| Odds Ratio | t | p | β | t | p | |
| Relationship Risk | ||||||
| Loneliness | 1.046 | 1.25 | .215 | .062 | 3.46 | .001 |
| Social acceptance | .883 | −3.94 | .000 | −.058 | −4.04 | .000 |
| Parental support | .913 | −2.94 | .004 | −.052 | −3.80 | .000 |
| Romantic relationship instability | 1.062 | 2.21 | .029 | −.007 | −.55 | .585 |
| Ever experienced relationship violence | 1.382 | 6.09 | .000 | .261 | 9.27 | .000 |
| Ever experienced loss | 1.194 | 1.71 | .089 | .069 | 1.52 | .131 |
| Wave I Health and Demographic Controls | ||||||
| Self-rated health (very good) | ||||||
| Excellent | .481 | −11.31 | .000 | −.036 | −1.18 | .240 |
| Good | 1.683 | 8.13 | .000 | .018 | .55 | .586 |
| Fair | 3.159 | 10.34 | .000 | .059 | .97 | .332 |
| Poor | 8.589 | 3.53 | .001 | −.059 | −.33 | .745 |
| Depressive symptoms | 1.044 | 1.26 | .210 | .190 | 9.25 | .000 |
| Physical limitation | 1.105 | .64 | .526 | −.086 | −1.00 | .317 |
| Symptom count | 1.010 | 2.04 | .044 | .010 | 3.91 | .000 |
| Baseline cardiac abnormality | 1.900 | .91 | .362 | .176 | .48 | .629 |
| Baseline asthma | 4.780 | 3.10 | .002 | .154 | .82 | .451 |
| Body mass indexb (2nd quartile) | ||||||
| BMI 1st quartile | 1.118 | 1.74 | .084 | .068 | 1.99 | .049 |
| BMI 3rd quartile | 1.145 | 1.83 | .070 | .069 | 2.02 | .045 |
| BMI 4th quartile | 1.691 | 6.72 | .000 | .068 | 1.92 | .058 |
| Gender (male = 1) | .837 | −3.02 | .003 | −.194 | −7.84 | .000 |
| Parental educationb (high school) | ||||||
| Less than high school | 1.013 | .12 | .901 | .062 | 1.69 | .094 |
| Some college | .995 | −.07 | .946 | .030 | .84 | .403 |
| College | .917 | −1.08 | .281 | .027 | .78 | .437 |
| More than college | .765 | −2.77 | .007 | −.061 | −1.56 | .121 |
| Race/ethnicity (White) | ||||||
| Black | .932 | −.91 | .364 | .064 | 1.43 | .155 |
| Native American | .737 | −1.50 | .135 | −.107 | −.79 | .433 |
| Asian | 1.378 | 2.39 | .018 | .131 | 2.01 | .047 |
| Hispanic | .962 | −.54 | .591 | .104 | 2.36 | .020 |
| Other | .985 | −.05 | .958 | .096 | .94 | .348 |
| Wave II Health Behavior Controls | ||||||
| Physical exercise | .986 | −1.2 | .231 | .009 | 1.87 | .064 |
| Current smoking | 1.182 | 2.77 | .006 | .031 | 1.08 | .281 |
| Fast food consumption | .997 | −.18 | .856 | −.011 | −1.61 | .110 |
| Binge drinking | 1.031 | .53 | .600 | −.006 | −.20 | .842 |
| Constantc | -- | -- | -- | −.173 | −1.16 | .250 |
| Cut 1d | −.819 | −2.86 | .005 | -- | -- | -- |
| Cut 2 | 1.222 | 4.32 | .000 | -- | -- | -- |
| Cut 3 | 3.432 | 12.12 | .000 | -- | -- | -- |
| Cut 4 | 6.056 | 16.62 | .000 | -- | -- | -- |
Note: Also controlling for age, WI family structure (two parents, both biological; two parents, one biological; single mother, single father, other); WIII marital status (married, remaried, divorced, widowed, cohabitating); WIII single parenthood, and WIII number of births.
Higher scores indicate worse health
Missing data were coded as a separate category
Intercept for OLS regression predicting depressive symptoms
Estimated cut points for ordered regression model for general health
General Health
Loneliness was not significantly associated with self-reported general health, but a one standard deviation (SD) increase in feeling accepted/loved was associated with a 12% reduction in the odds of reporting worse health. A one SD increase in perceived parental support was associated with a 9% reduction in the odds of reporting poorer health. For each additional romantic relationship transition after age 16, there was a 6% increase in odds of reporting poorer health. Experiencing intimate partner violence was associated with a 38% increase in odds of reporting poorer health. Having lost a loved one was associated with 19% greater odds of reporting poorer health, but was only marginally significant (p < .09).
Depressive Symptoms
A one SD increase in loneliness was associated with a 0.062 SD increase, and a one SD increase in feeling accepted/loved was associated with a 0.058 SD decrease in depressive symptoms. A one SD increase in perceived parental support was associated with .05 SD lower depressive symptoms. Ever having experienced intimate partner violence was associated with a 0.26 SD increase in depressive symptoms.
Cumulative relationship risk index
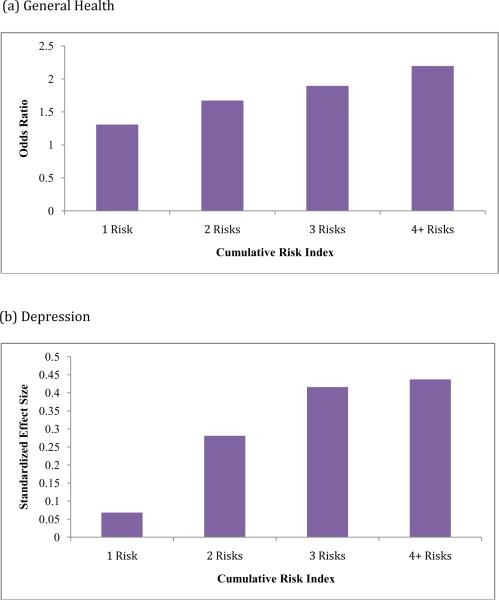
In the final two models we examined the potential cumulative effects of experiencing multiple relationship risks on general health and depressive symptoms (Table 4). Compared to no relationship risks, the odds ratios predicting poorer health increased linearly for each added relationship risk: one relationship risk, OR = 1.31; two relationship risks, OR = 1.67; three relationship risks, OR = 1.90; four or more relationship risks, OR = 2.20 (all p < .001). Participants in the highest group had more than twice the odds of reporting poorer health than those in the no risk group (p <.001; Figure 1). We also observed an increasing linear trend in effect sizes across the cumulative relationship risk groups when predicting depressive symptoms (Figure 1). Compared to youth with no relationships risks, youth with one relationship risk had a .07 SD increase in depressive symptoms, and youth with two, three and four or more relationship risks had depressive symptom increases of .28 SD, .42 SD and .44 SD, respectively (all p < .001).
Table 4.
Ordered Logit predicting poor health and OLS Regressions predicting depressive symptoms at Wave III from cumulative relationship risk index variables and controls.
| General Healtha (N=9850) | Depressive Symptoms (N=9798) | |||||
|---|---|---|---|---|---|---|
| Odds Ratio | t | p | β | t | p | |
| Relationship Risk (no relationship risk) | ||||||
| One relationship risk | 1.309 | 4.07 | .000 | .068 | 2.17 | .032 |
| Two relationship risks | 1.673 | 6.78 | .000 | .281 | 7.79 | .000 |
| Three relationship risks | 1.895 | 6.76 | .000 | .416 | 8.34 | .000 |
| Four or more relationship risks | 2.197 | 4.83 | .000 | .437 | 4.47 | .000 |
| Wave I Health and Demographic Controls | ||||||
| Self-rated health (very good) | ||||||
| Excellent | .469 | −11.77 | .000 | −.049 | −1.60 | .112 |
| Good | .170 | 8.11 | .000 | .023 | .70 | .485 |
| Fair | 3.192 | 10.63 | .000 | .069 | 1.17 | .244 |
| Poor | 9.578 | 3.65 | .001 | .009 | .05 | .963 |
| Depressive symptoms | 1.080 | 2.66 | .009 | .221 | 11.86 | .000 |
| Physical limitation | 1.079 | .50 | .621 | −.095 | −1.08 | .282 |
| Symptom count | 1.009 | 1.96 | .052 | .010 | 3.88 | .000 |
| Baseline cardiac abnormality | 2.096 | 1.04 | .299 | .188 | .50 | .165 |
| Baseline asthma | 4.998 | 3.23 | .002 | .187 | .98 | .328 |
| Body mass indexb (2nd quartile) | ||||||
| BMI 1st quartile | 1.112 | 1.68 | .095 | .062 | 1.79 | .076 |
| BMI 3rd quartile | 1.127 | 1.73 | .085 | .059 | 1.76 | .080 |
| BMI 4th quartile | 1.673 | 6.63 | .000 | .066 | 1.87 | .063 |
| Gender (male = 1) | .833 | −3.06 | .003 | −198 | −7.99 | .000 |
| Parental educationb (high school) | ||||||
| Less than high school | 1.022 | .22 | .828 | .069 | 1.92 | .057 |
| Some college | .998 | −.03 | .975 | .028 | .80 | .423 |
| College | .927 | −.93 | .352 | .029 | .83 | .410 |
| More than college | .764 | −2.76 | .007 | −.070 | −1.79 | .076 |
| Race/ethnicity (White) | ||||||
| Black | .908 | −1.24 | .217 | .070 | 1.59 | .114 |
| Native American | .747 | −1.47 | .144 | −.092 | −.68 | .498 |
| Asian | 1.406 | 2.49 | .014 | .141 | 2.15 | .034 |
| Hispanic | .961 | −.55 | .581 | .113 | 2.57 | .011 |
| Other | .985 | −.05 | .959 | .112 | 1.09 | .277 |
| Wave II Health Behavior Controls | ||||||
| Physical exercise | .982 | −1.51 | .132 | .007 | 1.52 | .130 |
| Current smoking | 1.194 | 2.93 | .004 | .039 | 1.40 | .164 |
| Fast food consumption | .997 | −.24 | .813 | −.011 | −1.53 | .129 |
| Binge drinking | 1.032 | .55 | .584 | −.009 | −.32 | .749 |
| Constantc | -- | -- | -- | −.204 | −1.33 | .187 |
| Cut 1d | −.666 | −2.29 | .024 | -- | -- | -- |
| Cut 2 | 1.369 | 4.76 | .000 | -- | -- | -- |
| Cut 3 | 3.573 | 12.46 | .000 | -- | -- | -- |
| Cut 4 | 6.194 | 16.79 | .000 | -- | -- | -- |
Note: Also controlling for age, WI family structure (two parents, both biological; two parents, one biological; single mother, single father, other); WIII marital status (married, remaried, divorced, widowed, cohabitating); WIII single parenthood, and WIII number of births.
Higher scores indicate worse health
Missing data were coded as a separate category
Intercept for OLS regression predicting depressive symptoms
Estimated cut points for ordered regression model for general health
Figure 1.
Associations between level of cumulative relationship risk exposure and (a) self-reported general health and (b) self-reported depressive symptoms in young adulthood, controlling for baseline health and demographic and health behavior covariates.
In addition to baseline health and demographic covariates, all the models included Wave II health behavior measures (exercise, smoking, diet, and binge drinking). Although smoking was a significant predictor of general health, the relationship risk coefficients were not substantially reduced by the addition of the health behavior variables, suggesting that the impact of relationship risks on changes in health from Wave I to Wave III are not accounted for by variations in these particular health behaviors.
In a final set of models (not shown), we added interactions between the relationship risk variables and gender. Although there were significant main effects of gender, with males reporting better general health and lower depressive symptoms (Tables 3 and 4), there were only two significant interactions between gender and relationship risk exposure in predicting these outcomes. Parental support had a lower impact on the general health of males, while loneliness had a significantly stronger impact on males' depressive symptoms. Thus, although males were exposed to fewer relationship risks than females, the risks they did encounter generally related to health in similar ways.
Discussion
This study provides evidence that multiple types of adverse relationship experiences, encountered during the adolescent years, are associated with worse self-reported mental and general health in adulthood, controlling for baseline health status, demographic covariates, and health behaviors. Results varied by outcome of interest: whereas relationship transitions and loss were related to general health but not depressive symptoms, loneliness predicted depression but not general health. The remaining variables (low acceptance, low perceived parental support, and IPV) significantly predicted both outcomes. The effect sizes for most of the relationship risk variables were small, except for IPV, which had the largest effect sizes for both outcomes. It is perhaps not surprising that IPV, which carries the dual threat of social and physical harm, would show the largest effects [24]. Although there were main effects of gender on our health outcomes, there was little evidence that associations between relationship risks and health outcomes were moderated by gender.
Our cumulative risk results underscore the more substantial health impacts of experiencing multiple adverse relationship experiences. A relatively linear increase in poor health was observed, with each additional risk predicting an incremental worsening of outcomes for both general health and depression. While statistically significant, the average effect size for the impact of just one relationship risk on health was small, particularly for depression. By two, three and four relationship risks, however, effect sizes reached a clinically relevant level. At four risks, the odds of moving to one step worse health status (e.g. from very good to good, or from good to fair) between Wave I and Wave III more than doubled, and the increase in depressive symptoms approached half a standard deviation (e.g. the equivalent of moving from experiencing 2–3 symptoms sometimes to experiencing at least six symptoms sometimes).
Although we favor the interpretation that relationship risks contribute causally to later poor health, an alternative explanation could be that individuals with poor health are more likely to encounter relationship risks, or that a third variable contributes to relationship risks and poor health. However, by using prospective longitudinal data, controlling for confounds, and using a change model controlling for baseline levels of our health outcomes, we strongly reduce the likelihood that stable individual differences, genetic factors, or preexisting health conditions account for our results.
In terms of potential mechanisms, the health behaviors that we examined (exercise, smoking, diet, binge drinking) did not play a large role in explaining the impact of relationship risks of our health outcomes. Another hypothesis to be tested in future research is the possibility that adverse relationship experiences result in activation of biological stress systems, which in turn have negative health implications [7]. Our “relationship risks” include the presence of actively adverse relationship experiences (e.g. exposure to violence), as well as the perceived absence of necessary positive relationship experiences (e.g. loneliness, low parental support); both types of experience have been linked to stress physiology in past research [7,13].
Conclusion
This study has some limitations, the largest of which is reliance on self-report data for measuring both relationship risks and health outcomes. Nonetheless, it is the first study to examine multiple adverse relationship experiences simultaneously, allowing a test of their cumulative/joint impact on health. Most large scale studies of social relationships and health have focused on positive features of social relationships, such as social support and social network size, and the stress buffering properties of social relationships, despite considerable research and theory [5][6] suggesting that negative social experiences may play an equally important role. Future analyses and theoretical models need to consider how multiple positive and negative features of our social relationships jointly determine health trajectories. Next steps should also include direct measurements, in longitudinal studies, of the biological stress pathways by which adverse social experiences may affect health.
Acknowledgements
This research was supported by R01-HD053731 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and by Faculty Fellow awards from the Institute for Policy Research, Northwestern University, to Emma K. Adam and Thomas W. McDade. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Child Health and Human Development. This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The criteria used by Add Health to determine the two most important relationships included marriage and cohabitation status, relationship length, presence of children or pregnancy, and whether the relationship was current (see Add Health documentation).
References
- 1.Shonkoff JP, Phillips D, editors. Committee on Integrating the Science of Early Childhood Development, Board on Children, Youth, and Families, Commission on Behavioral and Social Sciences and Education, National Resesarch Council and Institute of Medicine. National Academy Press; Washington, DC: 2000. From Neurons to Neighborhoods: The Science of Early Childhood Development. [PubMed] [Google Scholar]
- 2.Cacioppo J, Bernston G, Sheridan J, et al. Multilevel integrative analyses of human behavior: Social neuroscience and the complementing nature of social and biological approaches. Psychological Bulletin. 2000;126:829–843. doi: 10.1037/0033-2909.126.6.829. [DOI] [PubMed] [Google Scholar]
- 3.Uchino B, Cacioppo J, Kiecolt-Glaser J. The relationship between social support and physiological processes: A review with emphasis on underlying mechanisms and implications for health. Psychological Bulletin. 1996;119:488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
- 4.Adam EK, Klimes-Dougan B, Gunnar MR. Social regulation of the adrenocortical response to stress in infants, children and adolescents: Implications for psychopathology and education. In: Coch D, Dawson G, Fischer K, editors. Human Behavior, Learning, and the Developing Brain: Atypical Development. Guilford Press; 2007. pp. 264–304. [Google Scholar]
- 5.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 6.Cohen S. Social relationships and health. American Psychologist. 2004;59:676. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- 7.Repetti R, Taylor SE, Seeman T. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330. [PubMed] [Google Scholar]
- 8.Dickerson SS, Gruenewald TL, Kemeny ME. When the social self is threatened: shame physiology and health. J Personal. 2004;72:1191. doi: 10.1111/j.1467-6494.2004.00295.x. [DOI] [PubMed] [Google Scholar]
- 9.Cacioppo JT, Hawkley LC, Crawford LE, Ernst JM, Burleson MH, Kowalewski RB, Malarkey WB, VanCauter E, Berntson GG. Loneliness and health: Potential mechanisms. Psychosomatic Medicine. 2002;64:407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Pritchard ME, Yalch KL. Relationships among loneliness, interpersonal dependency, and disordered eating in young adults. Personality and Individual Differences. 2009;46(3):341–346. [Google Scholar]
- 11.Cacioppo JT, Hawkley LC, Berntson GG, et al. Do lonely days Invade the nights? Potential social modulation of sleep efficiency. Psychological Science. 2002;13(4):384–387. doi: 10.1111/1467-9280.00469. [DOI] [PubMed] [Google Scholar]
- 12.Kiecolt-Glaser JK. Urinary cortisol levels, cellular immunocompetency, and loneliness in psychiatric inpatients. Am Psychosomatic Soc. 1984:15–23. doi: 10.1097/00006842-198401000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Doane LD, Adam EK. Loneliness and cortisol: Momentary, day-to-day, and trait associations. Psychoneuroendocrinology. 2009;35(3):430–441. doi: 10.1016/j.psyneuen.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yarcheski A, Mahon NE, Yarcheski TJ, et al. A Meta-Analysis of Predictors of Positive Health Practices. Journal of Nursing Scholarship. 2004;36(2):102–108. doi: 10.1111/j.1547-5069.2004.04021.x. [DOI] [PubMed] [Google Scholar]
- 15.Nachmias M, Gunnar MR, Mangelsdorf S, et al. Behavioral inhibition and stress reactivity: The moderating role of attachment security. Child Development. 1996;67:508–522. [PubMed] [Google Scholar]
- 16.Flinn MV, England BG. Childhood stress and family environment. Current Anthropology. 1995;36:854–866. [Google Scholar]
- 17.Pendry P, Adam EK. Associations between parents' marital functioning, maternal parenting quality, maternal emotion and child cortisol levels. International Journal of Behavioral Development. 2007;31(3):218–231. [Google Scholar]
- 18.Adam EK. Beyond quality: Parental and residential stability and children's adjustment. Current Directions in Psychological Science. 2004;13(5):210–213. [Google Scholar]
- 19.Cherlin A. The marriage-go-round: The state of marriage and the family in America today. Knopf; New York: 2009. [Google Scholar]
- 20.Collins WA. More Than Myth: The Developmental Significance of Romantic Relationships During Adolescence. Journal of Research on Adolescence. 2003;13(1):1–24. [Google Scholar]
- 21.Coker AL, Oldendick R, Derrick C, et al. Intimate partner violence among men and women--South Carolina, 1998. MMWR Morbidity and Mortality Weekly Report. 2000;49(30):691–694. [PubMed] [Google Scholar]
- 22.McCauley J, Kern DE, Kolodner K, et al. The “Battering Syndrome”: Prevalence and Clinical Characteristics of Domestic Violence in Primary Care Internal Medicine Practices. Annals of Internal Medicine. 1995;123(10):737. doi: 10.7326/0003-4819-123-10-199511150-00001. [DOI] [PubMed] [Google Scholar]
- 23.Golding JM. Intimate Partner Violence as a Risk Factor for Mental Disorders: A Meta-Analysis. Journal of Family Violence. 1999;14(2):99–132. [Google Scholar]
- 24.Coker AL, Smith PH, Bethea L, et al. Physical Health Consequences of Physical and Psychological Intimate Partner Violence. Archives of Family Medicine. 2000;9(5):451. doi: 10.1001/archfami.9.5.451. [DOI] [PubMed] [Google Scholar]
- 25.Leserman J, Li Z, Drossman DA, et al. Selected symptoms associated with sexual and physical abuse history among female patients with gastrointestinal disorders: the impact on subsequent health care visits. Psychological Medicine. 1998;28(2):417. doi: 10.1017/s0033291797006508. [DOI] [PubMed] [Google Scholar]
- 26.Koss MP, Heslet L. Somatic consequences of violence against women. Archives of Family Medicine. 1992;1(1):53. doi: 10.1001/archfami.1.1.53. [DOI] [PubMed] [Google Scholar]
- 27.Brent DA, Perper J, Moritz G, et al. Psychiatric Effects of Exposure to Suicide among the Friends and Acquaintances of Adolescent Suicide Victims. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31(4):629. doi: 10.1097/00004583-199207000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Brown GW, Harris TO, Bifulco A. Long-term effects of early loss of parent. Depression in young people: Developmental and clinical perspectives. 1986:251–296. [Google Scholar]
- 29.Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. The Lancet. 2007;370(9603):1960–1973. doi: 10.1016/S0140-6736(07)61816-9. [DOI] [PubMed] [Google Scholar]
- 30.Sood B, Weller EB, Weller RA, et al. Somatic complaints in grieving children. Comprehensive Mental Health Care. 1992;2(1):17–25. [Google Scholar]
- 31.Calabrese JR, Kling MA, Gold PW. Alterations in immunocompetence during stress, bereavement, and depression: focus on neuroendocrine regulation. American Journal of Psychiatry. 1987;144(9):1123. doi: 10.1176/ajp.144.9.1123. [DOI] [PubMed] [Google Scholar]
- 32.Nicolson N. Childhood parental loss and cortisol levels in adult men. Psychoneuroendocrinology. 2004;29:1012–1018. doi: 10.1016/j.psyneuen.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 33.Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychological Bulletin. 2004;130(4):601–630. doi: 10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rutter M, Clarke S. A. The promotion of resilience in the face of adversity. Families count: Effects on Child and Adolescent Development. 2006:26–52. [Google Scholar]
- 35.Friedman RJ, Chase-Lansdale PL. Chronic adversities. Child and Adolescent Psychiatry. 2002:261–276. [Google Scholar]
- 36.Bearman PS, Jones J, Udry JR. The National Longitudinal Study of Adolescent Health: Research Design. 20:2003. Retrieved January 1997. [Google Scholar]
- 37.Harris KM, Florey F, Tabor J, et al. The National Longitudinal Study of Adolescent Health: Research Design 2003. [Online].[cited April 1, 2010]; Available from: http://www.cpc.unc.edu/projects/addhealth/design.
- 38.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 39.Allison PD. Missing data. Sage; Thousand Oaks, CA: 2001. [Google Scholar]
- 40.Tourangeau R, Shin H. National Longitudinal Study of Adolescent Health: Grand Sample Weight. Carolina Population Center, University of North Carolina at Chapel Hill. 1998 [Google Scholar]