Abstract
Objectives
Assess the recovery of ankle function and general health status at multiple time points during the first 24 months after an isolated tibial plafond fracture treated with joint spanning external fixation. Furthermore, determine factors that affect a rapid vs. a slow recovery, and factors that influence patient outcome at a minimum of two years after injury.
Design
Prospective observational study.
Setting
Two level one trauma centers.
Patients
43 patients (mean age, 42 years; range, 20 - 60 years) with unilateral fractures of the tibial plafond were prospectively assessed. These 43 patients had a 24 month follow-up and were seen for at least three additional scheduled visits prior to the 24 month follow up.
Intervention
Spanning articulated external fixator and follow ups at defined time intervals after injury to track the progress of the outcome measures over time.
Main Outcome Measures
The Short Form Health Survey (SF-36) Medical Outcomes Study (MOS) version 2 Physical Component Summary Score (PCS) and Mental Component Summary Score (MCS) and the Ankle Osteoarthritis (AOS) Pain and Disability Scales.
Results
Early after injury, the MCS was not as negatively affected as the PCS. By six months after injury, the MCS had improved to be equivalent to age matched norms and remained there at two years after injury. The PCS was more severely compromised and did not level off until the 12 month clinic visit. At two years the PCS remained on average one standard deviation below age matched normal.
Although not statistically significant, both the average pain and disability AOS scales deteriorated between 6 and 12 months, suggesting some patients actually perceived their ankle as being worse as they begin walking on their injured ankle. Between 12 and 24 months they trended towards improvement in both the pain and function scales. However their ankle continued to have dramatically increased pain and decreased function compared to population based norms.
Conclusions
In patients recovering from a tibial plafond fracture that was treated with joint spanning external fixation, the MCS improves quickly and completely, while the PCS often takes one full year or longer to reach maximal improvement and does not completely recover, since it remains on average one standard deviation below normal at two years after injury. Changes in the AOS pain and disability scales between 6 and 12 months after injury were not significantly different but at all time points the patient’s ankle pain and function remains dramatically different than the normal population. These results can be used in future studies for comparison with patients treated with alternate treatment techniques and to assess the effect of important treatment variables such as stabilization techniques and quality of reduction.
Keywords: Plafond, pilon, ankle fracture, outcome, SF-36, AOS
Introduction
Outcomes after tibial plafond fractures are variable but typically they are not excellent.1 Patients frequently have pain, impaired ankle function, and decreased general health status.1-5 Most studies that report outcomes after these fractures have assessed patients at a single point in time and report an average length of follow up.1-6 Although these studies are important they do not provide information about what patients can expect at defined times after injury and they do not assess the time course and sequence of recovery after these devastating ankle injuries.
Information on sequential recovery after injury has been reported for some fracture problems such as malleolar fractures7-9 and calcaneus fractures10 as well as for reconstructions after tibial nonunions.11 This information is important for patient counseling and decisions on reconstructive management. After a tibial plafond fracture the function, pain and recovery of general health that a patient can expect at six months, one year or two years after injury is largely unknown, since the sequential recovery has not been systematically analyzed.
The purpose of this prospective observational study is to assess the recovery of ankle function and general health status at multiple time points during the first 24 months after an isolated tibial plafond fracture treated with a specific technique of joint spanning external fixation. Factors that determine a rapid vs. a slow recovery (age, gender, fracture classification, articular comminution, quality of reduction, associated fibula fracture, and education) and the factors that influence patient outcome at a minimum of two years after injury (age, gender, fracture classification, quality of reduction, articular comminution, education, income, associated injuries, other medical problems, employment status, plans to return to work, involvement in legal action due to injury, and compensation status) were also assessed.
Materials and Methods
This study was performed with the approval of the Human Subjects Review Boards at the two institutions. Between January 2000 and August 2005, eighty-one patients with unilateral tibial plafond fractures (AO/OTA type B-2, B-3, C-1, C-2, or C-3) were treated and entered into a database. Patients with bilateral fractures, ipsilateral calcaneus or talus fractures, those with type III open wounds, and those patients with an Injury Severity Score of 18 or greater were not included. Patients with head injuries, severe osteopenia, or patients who had previous attempts to surgically reduce the articular surface were also excluded. Pregnancy, previous ankle fractures, contralateral ankle abnormalities, and intervening ankle trauma between the index injury and the two-year follow-ups were additional exclusion criteria.
The protocol was for patient clinic visits to obtain outcome measures at specific time points after injury - 1, 2, 3, 6, 12, and 24 months. Since this study was designed to describe a specific time-course to recovery, only patients with reasonably complete data were included. To be included, patients had to have a 24 month follow-up and not miss more than two of the previous follow-up appointments. These inclusion criteria were chosen to balance keeping sufficient patient numbers in the study against the importance of having complete follow up at all time points. Of the 81 patients entered into the database, 43 patients (mean age, 41.8 years; range, 20 - 60 years) met these criteria and were included in this study. These 43 patients had a 24 month follow-up and were seen for at least three additional visits prior to 24 months. Two study patients passed away during follow-up, one patient moved, and thirty-five patients were not included due to lack of adequate follow-up. To assess the effect of the high number of excluded patients the forty three included patients were compared to the thirty-eight excluded patients for factors such as age, gender, fracture classification, articular comminution, education, associated fibula fracture, income, associated injuries, other medical problems, employment status, plans to return to work, involvement in legal action due to injury, and compensation status. The only significant difference between the two groups was in education level with a larger proportion of patients that completed college in the group that were included in the study (p-value of 0.05).
There were 28 males (65.2%) and 15 females (34.8%). The AO/OTA classification of the fractures was 31 types C (4 C1, 9 C2, and 18 C3) and 12 type B (5 B2, 7 B3).12 The mechanisms of injury were falls from a height (range, 4 - 25 feet) in 60%, motor vehicle accidents in 20%, and the other 20% were caused by other mechanisms including crush, bicycle accidents, and motorcycle accidents. Each fracture was treated with a spanning articulated external fixator and limited internal fixation of the articular surface. The approach to reducing and internally fixing the articular surface was variable based on the case and the treating surgeon and ranged from percutaneous techniques only to fairly extensive open reductions. This technique has been previously published.12
At each clinic visit patients were assessed with a general health status measure, Short-Form 36 (SF-36), and a joint specific outcome measure, Ankle Osteoarthritis Scale (AOS). The SF-36 was recorded at all time points. The AOS was recorded at 6, 12, and 24 months after injury.
The SF-36 MOS version 2.0 is a thirty-six question general health survey designed to assess physical and emotional health and health-related quality of life.13 It produces an eight-scale profile of scores as well as physical (PCS) and mental (MCS) component summary scores based on twenty-one and fifteen questions, respectively.13 These scores were scaled and normalized to 1998 population norms. For both the PCS and the MCS a score of 50 is equivalent to age matched norms with one and two standard deviations above and below the normal scores being plus and minus 10 and 20 points, respectively.
The AOS was used to measure pain and disability related to the injured ankle. Both the pain and disability scores are nine question visual analogue scales measured from 0 - 100, with higher scores indicating greater pain and disability. The AOS has previously been found to be a reliable and valid assessment instrument. Normal subjects report little ankle pain or disability and have been found to have scores close to one. 14, 15
For each clinic visit, the scores for the MCS, PCS, AOS pain and AOS disability for all patients were averaged and the averages were compared to the averages at the previous and subsequent clinic visits. The time-course to recovery was assessed by comparing averages of the scores for the four outcome measures across adjacent time points.
To assess whether there were factors that affected the speed of recovery, the patients’ PCS at 12 and 24 months were compared. Patients were divided into three categories; those that showed no significant change between the 12 and 24 month time points, those that deteriorated (< 1 STD, PCS − 10), and those that showed continued improvement between the 12 and 24 month visits (≥ 1 STD, PCS + 10). Factors such as age, gender, fracture classification, articular comminution, associated fibula fracture, and education were analyzed for significant differences between these three groups of patients. Articular comminution was assessed on plain x-ray and classified by the investigators using the AO/OTA classification of fractures of the distal tibia. Fractures classified as C3 and B3 were scored as articularly comminuted and those classified as B1, B2, C1, and C2 were scored as not comminuted. Levels of education were classified according to four categories; did not complete high school, completed high school, some college or vocational school, completed college. Articular comminution and level of education were classified as dichotomous variables.
In addition to the speed of recovery, the effect of a broader set of factors on the outcome at 24 months after injury was assessed. The risk factors assessed were age, gender, fracture classification, articular comminution, education, income, associated injuries, other medical problems, employment status, plans to return to work, involvement in a legal action due to injury, and compensation status. The outcomes assessed were the AOS and SF-36 scores at the 24 month follow-up.
A mixed model with statistical contrasts was used to compare outcomes at adjacent time-points because the data included repeated measures and contained correlation within each group with some empty cells. Several tests with different correlation (covariance) structures were performed, and based on the model fitting criteria, the SP(POW) covariance structure was chosen. Predictive factors in the speed of recovery were modeled using logistic regression with a forward variable selection strategy. A univariate model was also used due to the limited power for this analysis. At two years after injury, a general linear model was used to assess the relationships between response variables PCS/MCS and several demographic variables.
Results
At two years after injury, on average the result for the physical - PCS vs. the mental - MCS component of the SF-36 was very different. On the MCS the patients’ scores were similar to age matched norms (50.8 ± 11.5), but on the PCS they remained one standard deviation below age matched norms (39.4 ± 9.9). Not surprisingly their ankle as assessed on the AOS had dramatically increased pain and decreased function compared to population-based norms. The average pain score was 34.2 ± 23.7 (population norm 1.0), and the average disability score was 38.4 ± 27.1 (population norm 1.2). The two year PCS, MCS, AOS pain or AOS disability were not significantly affected by age, gender, fracture classification, articular comminution, education, income, associated injuries, other medical problems, employment status, plans to return to work, involvement in a legal action due to injury, and workers compensation due to the injury.
Although follow up appointments were scheduled at specific time points after injury (1, 2, 3, 6, 12, and 24 months) there was some variation in when patients were actually seen. The average difference for all patients between the scheduled time and the time they were actually seen as well as the largest deviations positive and negative at each time point were: 1 month - avg. 2.7 days (−16 to +14) , 2 month - avg. 6.2 days (−17 to +24), 3 month - avg. 15.4 days (−34 to +38), 6 month - avg. 15.1 days (−54 to +45), one year - avg. 3.6 days (−72 to +75) and two years - avg. 104.5 days (−142 to +270).
Table 1 and Figure 1 illustrate the time dependent average scores for the SF-36 PCS and MCS. The data demonstrates that there were important differences between these two scores. Early after injury the MCS was not as negatively affected as the PCS, with the one month averages being 44.3 ± 11.9 for the MCS and 31.4 ± 7.7 for the PCS. By six months after injury the MCS had improved to be equivalent to age matched norms (51.9 ± 10.6). The improvement between 3 and 6 months (47.6 ± 13.5 and 51.9 ± 10.6, respectively) was statistically significant. The PCS was more severely compromised after injury and did not plateau until the 12 month clinic visit (39.9 ± 8.8). The PCS improved significantly between 3 and 6 months (32.4 ± 5.8 and 35.9 ± 8.2, respectively) and also between 6 and 12 months (35.9 ± 8.2 and 39.9 ± 8.8, respectively). These data show that the physical component of general health status was more negatively affected by a tibial plafond fracture, and recovered more slowly and less completely, compared to the mental component of the SF-36.
Table 1.
Sequential SF-36 MCS and PCS average scores (* denotes statistically significant values, p< 0.05 as compared to the previous time-point)
| SF-36 MCS | SF-36 PCS | Sample Size |
|||
|---|---|---|---|---|---|
| 1 month: | 44.3 ± 11.9 | 31.4 ± 7.7 | (33/43) | ||
| 2 months: | 47.8 ± 10.1 | p = 0.07 | 31.3 ± 6.1 | p = 0.93 | (39/43) |
| 3 months: | 47.6 ± 13.5 | p = 0.70 | 32.4 ± 5.8 | p = 0.58 | (40/43) |
| 6 months: | *51.9 ± 10.6 | p = 0.02 | *35.9 ± 8.2 | p = 0.00 | (40/43) |
| 12 months: | 51.4 ± 10.5 | p = 0.85 | *39.9 ± 8.8 | p = 0.01 | (36/43) |
| 24 months: | 50.8 ± 11.5 | p = 0.74 | 39.4 ± 9.9 | p = 0.65 | (43/43) |
Figure 1.
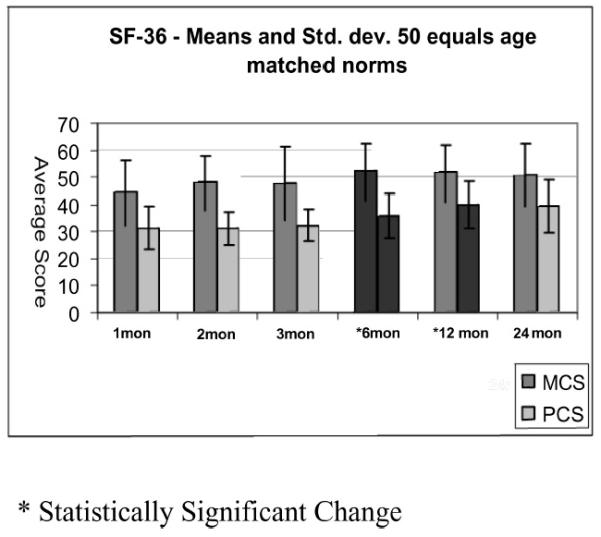
SF-36
Table 2 and Figure 2 show that the AOS (both pain and disability) had a different time-course than either of the SF-36 summary scores. Both the pain and disability AOS averages were higher at 12 months after injury than at 6 months (higher scores mean greater pain and disability). Between 12 and 24 months, the AOS trended towards improvement in both the pain and function scales and returned to a level very similar to the six month scores. The changes in these scores over the first two years suggest that some patient’s perceive that their ankle pain and function is worse when they begin to increase their activities 6 months after injury and slowly improves thereafter. However the spread in the data for the AOS scores is much greater than for the PCS or the MCS components of the SF-36 and the differences in the average scores were not significant.
Table 2.
Sequential Ankle Osteoarthritis Scale pain and disability average scores
| AOS pain | Sample Size | AOS disability | Sample Size | |
|---|---|---|---|---|
| 6 months: | 34.0 ± 18.539.4 ± 24.9 | (34/43) | 36.8 ± 19.343.6 ± 25.3 | (34/43) |
| 12 months: 24 months: |
p = 0.16 34.2 ± 23.7 p = 0.24 |
(31/43) (37/43) |
p = 0.09 38.4 ± 27.1 p = 0.26 |
(32/43) (38/43) |
Figure 2.
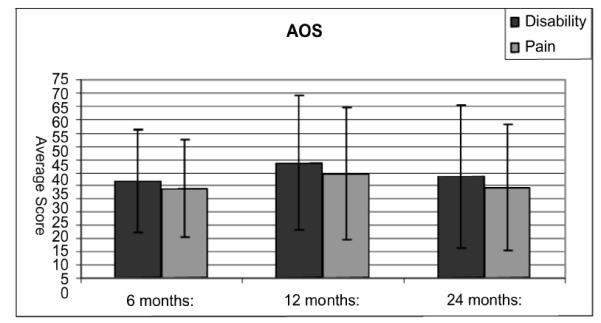
AOS - means and std. dev.
Higher number = more pain and disability
Ten patients continued to improve on their PCS (by one standard deviation or more) after 12 months (slower recovery), 18 had no change, and 8 deteriorated. Seven patients were excluded from this analysis because they did not have one year follow up. The speed of recovery as defined by these three groups was not significantly affected by any of the following factors; age, gender, fracture classification, presence of a fibula fracture, and education. Univariate analysis showed that comminution was the only significant variable predicting the speed of recovery for PCS outcomes; a comminuted fracture predicted a slower recovery (p=0.04).
Female patients and patients with low educational level, and/or low income, tended to have lower PCS scores; and female patients and those with low income tended to have lower MCS scores. These differences did not reach statistical significance.
Discussion
This study demonstrates the negative impact of fractures of the tibial plafond on ankle pain and function and on general health status in patients treated with a specific technique of joint spanning external fixation. At two years after injury, patients are substantially impaired on the SF-36 PCS, scoring one standard deviation below age matched norms. On the AOS ankle score they were found to have significant ankle pain and decreased function. These results are similar to those previously reported in the literature. As long as five to eleven years after injury, Marsh et al. showed that the negative effect of tibial plafond fractures on physical function and on ankle pain and function was still evident.3 Decreased general health status after these injuries also occurs in patients treated with other techniques since it has been reported in cases series of patients treated with external fixators3, plates5, and series in which both of these devices were used.2, 4
Using well accepted outcome tools allows the effect of a tibial plafond fracture on general health status and on ankle pain and function to be compared with the effect of other disease processes that have been studied with similar outcome tools. For instance, Saltzman et al. found that patients with established ankle arthritis presenting to a specialty clinic for treatment of their ankle had more ankle pain and decreased function than our patients had at two years after a tibial plafond fracture.15 Ankle arthritis patients were found to score on average 32 on the PCS compared to our patients average of 39 and on the AOS function scale (higher scores equals worse function) they were on average 61 compared to 34 for our patients. These differences are not unexpected. Although our patients had imperfect ankles, most of them were not actively seeking treatment. These results could be interpreted to indicate that if post traumatic osteoarthritis does not develop after these fractures, the patient will have less pain and function will be better than in patients that have established ankle osteoarthritis. Similar to our study the MCS for the ankle arthritis patients was minimally affected, indicating the major affect of ankle problems is on a patient’s perception of their physical health. A similar greater effect on physical health than mental health has been identified for patients with other chronic medical conditions such as cervical spine pain and radiculopathay, chronic heart conditions and patients with kidney failure on hemodialysis.16-18
The course to recovery of health status measures over time has been studied after rotational ankle fractures. Obremskey et al. assessed patients with low energy rotational ankle fractures at 4 and 20 months after injury with the SF-36.9 They found significant improvement between these two time points.9 Belcher et al. found that functional outcome measured by ankle scores and pedometers were not better between groups of patients seen between 8-10 months after injury compared with those seen between 11-24 months, implying that functional outcome had been restored relatively quickly in these patients.19 Egol et al found significant functional improvement between 6 and 12 months after injury.8 Bhandari et al found that all domains of the SF-36 improved over 24 months of follow up except the general health domain, which was normal at baseline.7 Similar to our study they identified that the MCS component of the SF-36 improved rapidly in the first 3-6 months after injury and that PCS improved more slowly and remained below age matched norms at two years after injury. Their study emphasized the importance of associated factors by finding that some scores were significantly affected by patient demographic data (age and education level) and co-morbid conditions (smoking and alcohol use). The information in these studies on rotational ankle fractures suggests that patients exhibit the greatest improvement between three and twelve months after injury, with further improvements in the second year being small and mostly on the physical rather than mental side of health recovery.
Relatively little information has been available on the time course to recovery after tibial plafond fractures. In one study Marsh et al. assessed nine patients with sequential ankle scores and found that they all improved between two and six years after injury.3 Patients perceived that they improved for on average 2.4 years. Ruedi et al found 74% good and excellent results at an average 4 years postoperatively. In a second follow-up 9 years postoperatively a number of the same patients had a further improved functional result. The authors concluded that in patients with anatomic reduction and fixation that function maybe preserved for a long period of time after injury. On the other hand malreductions lead to post traumatic OA and poor results. Unlike the current study, the study by Ruedi et al did not assess patients general health status.20
The current study provides new information about recovery after these most severe ankle injuries treated with joint spanning external fixation. The MCS scores improved quickly and by 6 months reached and then remained similar to age matched norms. These data suggest that most patients learn to accept and accommodate to their residual disability relatively soon after their injury. This is similar to what Bhandari et al. found for rotational ankle fractures, but it is in contrast to the LEAP study where 42% of patients with a severe lower extremity injury screened positive for a psychological disorder at 24 months after injury.21 The difference may be explained by the fact that our patients, in comparison to the LEAP patients, had mostly isolated intra-articular fractures. In addition, the MCS component of the SF-36 is a less sensitive screening tool for psychological disorders than that utilized in the LEAP study.
General physical function returned more slowly and less completely than mental health and took 12 months to plateau for most patients in this study. At two years after injury the PCS remained one standard deviation from age matched norms. In assessing ankle pain and function this study suggests that some patients perceive their ankle pain and function as worse in the second six months after injury. One explanation is that as some patients increase their activities they appreciate more ankle pain and more clearly recognize their functional impairment. At two years after injury the average scores returned to the six month level.
The strengths of this sequential observational study are that it provides information about patient recovery from a tibial plafond fracture treated with a specific technique of joint spanning external fixation that was not previously available. It is patient centered based on patients perceptions quantified hrough validated health status measures. These data indicate that on average a patient with a tibial plafond fracture will have a PCS score that is one standard deviation below age matched norms. This information of health status after a tibial plafond fracture can now be compared to other disease states and to patients with plafond fractures treated with different techniques. The time course information can be used to counsel patients about the expected recovery from this injury.
There are weaknesses to this study that potentially could affect the observed outcomes. Despite the prospective nature of the study design and data collection many of the patients did not complete the follow ups and were excluded. Among the study group, up to two follow-up visits may have been missed. In addition although follow ups were at prescribed intervals and the data reported are based on these intervals, there was variability in the times when the patients were actually seen. These issues mean the data points are not as sharply defined as ideal, potentially affecting the clarity of the results. Although we found that most of the demographic and co-morbid conditions we assessed had no effect on either the time to recovery or the eventual degree of recovery at two years, the study is underpowered to detect potentially meaningful differences and there were potentially important factors that were not studied such as quality of reduction. The only exception was that patients with more comminuted fractures tended to have slower recovery of their PCS scores. This could be an effect of either the more severe injury or less satisfactory reduction in these comminuted cases. For the AOS scores the data spread was very wide decreasing the impact of the averaged data on individual patients. Finally the results cannot be generalized to all tibial plafond fractures since the fractures in this study were all treated with a specific technique of spanning external fixation and screw fixation of the articular surface. These results do provide a benchmark to compare similar outcome measures obtained from other patients treated with alternate techniques.
In summary, observing general health and ankle specific outcome measures at multiple time points after a tibial plafond fracture treated with a specific technique of joint spanning external fixation has demonstrated important insights into the process of recovery. For most patients mental health measured by the MCS improves quickly and completely while general physical health measured by the PCS often takes one full year or longer to reach maximal improvement and does not completely recover remaining on average one standard deviation below normal at two years after injury. This typical pattern should be considered when counseling patients about their ankle pain and function in the second six months after their injury.
Acknowledgment
The authors would like to thank Yubo Gao, PhD for his help as a statistical consult during the statistical analysis part of this project.
Footnotes
Financial Disclosure: Sources of support for this project include: OREF, NIAMS AR 48939, OTA, and the Arthritis Foundation. They helped to aide in the financial backing of this study.
This study was presented in part at the Annual Meeting of the Orthopaedic Trauma Association, Boston, MA, 2007.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Andrew Pick, 2415 38th St. Des Moines, IA 50310.
Geoffrey Haft, Department of Orthopaedics 1210 W. 18th St. Ste. G01, Sanford Clinic Orthopaedics and Sports Medicine Sioux Falls, SD 57104.
References
- 1.Williams TM, Nepola JV, DeCoster TA, Hurwitz SR, Dirschl DR, Marsh JL. Factors affecting outcome in tibial plafond fractures. Clin Orthop Relat Res. 2004 Jun;(423):93–98. doi: 10.1097/01.blo.0000127922.90382.f4. [DOI] [PubMed] [Google Scholar]
- 2.Harris AM, Patterson BM, Sontich JK, Vallier HA. Results and outcomes after operative treatment of high-energy tibial plafond fractures. Foot Ankle Int. 2006 Apr;27(4):256–265. doi: 10.1177/107110070602700406. [DOI] [PubMed] [Google Scholar]
- 3.Marsh JL, Weigel DP, Dirschl DR. Tibial plafond fractures. How do these ankles function over time? J Bone Joint Surg Am. 2003 Feb;85-A(2):287–295. [PubMed] [Google Scholar]
- 4.Pollak AN, McCarthy ML, Bess RS, Agel J, Swiontkowski MF. Outcomes after treatment of high-energy tibial plafond fractures. J Bone Joint Surg Am. 2003 Oct;85-A(10):1893–1900. doi: 10.2106/00004623-200310000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Sands A, Grujic L, Byck DC, Agel J, Benirschke S, Swiontkowski MF. Clinical and functional outcomes of internal fixation of displaced pilon fractures. Clin Orthop Relat Res. 1998 Feb;(347):131–137. [PubMed] [Google Scholar]
- 6.Etter C, Ganz R. Long-term results of tibial plafond fractures treated with open reduction and internal fixation. Arch Orthop Trauma Surg. 1991;110(6):277–283. doi: 10.1007/BF00443458. [DOI] [PubMed] [Google Scholar]
- 7.Bhandari M, Sprague S, Hanson B, et al. Health-related quality of life following operative treatment of unstable ankle fractures: a prospective observational study. J Orthop Trauma. 2004 Jul;18(6):338–345. doi: 10.1097/00005131-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Egol KA, Tejwani NC, Walsh MG, Capla EL, Koval KJ. Predictors of short-term functional outcome following ankle fracture surgery. J Bone Joint Surg Am. 2006 May;88(5):974–979. doi: 10.2106/JBJS.E.00343. [DOI] [PubMed] [Google Scholar]
- 9.Obremskey WT, Dirschl DR, Crowther JD, Craig WL, 3rd, Driver RE, LeCroy CM. Change over time of SF-36 functional outcomes for operatively treated unstable ankle fractures. J Orthop Trauma. 2002 Jan;16(1):30–33. doi: 10.1097/00005131-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Allmacher DH, Galles KS, Marsh JL. Intra-articular calcaneal fractures treated nonoperatively and followed sequentially for 2 decades. J Orthop Trauma. 2006 Jul;20(7):464–469. doi: 10.1097/00005131-200608000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Zlowodzki M, Obremskey WT, Thomison JB, Kregor PJ. Functional outcome after treatment of lower-extremity nonunions. J Trauma. 2005 Feb;58(2):312–317. doi: 10.1097/01.ta.0000154302.23143.63. [DOI] [PubMed] [Google Scholar]
- 12.Marsh JL, Bonar S, Nepola JV, Decoster TA, Hurwitz SR. Use of an articulated external fixator for fractures of the tibial plafond. J Bone Joint Surg Am. 1995 Oct;77(10):1498–1509. doi: 10.2106/00004623-199510000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Ware JE., Jr. SF-36 health survey update. Spine. 2000 Dec 15;25(24):3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 14.Domsic RT, Saltzman CL. Ankle osteoarthritis scale. Foot Ankle Int. 1998 Jul;19(7):466–471. doi: 10.1177/107110079801900708. [DOI] [PubMed] [Google Scholar]
- 15.Saltzman CL, Zimmerman MB, O’Rourke M, Brown TD, Buckwalter JA, Johnston R. Impact of comorbidities on the measurement of health in patients with ankle osteoarthritis. J Bone Joint Surg Am. 2006 Nov;88(11):2366–2372. doi: 10.2106/JBJS.F.00295. [DOI] [PubMed] [Google Scholar]
- 16.Daffner SD, Hilibrand AS, Hanscom BS, Brislin BT, Vaccaro AR, Albert TJ. Impact of neck and arm pain on overall health status. Spine. 2003 Sep 1;28(17):2030–2035. doi: 10.1097/01.BRS.0000083325.27357.39. [DOI] [PubMed] [Google Scholar]
- 17.Knight EL, Ofsthun N, Teng M, Lazarus JM, Curhan GC. The association between mental health, physical function, and hemodialysis mortality. Kidney Int. 2003 May;63(5):1843–1851. doi: 10.1046/j.1523-1755.2003.00931.x. [DOI] [PubMed] [Google Scholar]
- 18.Sneed NV, Paul S, Michel Y, Vanbakel A, Hendrix G. Evaluation of 3 quality of life measurement tools in patients with chronic heart failure. Heart Lung. 2001 Sep-Oct;30(5):332–340. doi: 10.1067/mhl.2001.118303. [DOI] [PubMed] [Google Scholar]
- 19.Belcher GL, Radomisli TE, Abate JA, Stabile LA, Trafton PG. Functional outcome analysis of operatively treated malleolar fractures. J Orthop Trauma. 1997;11(2):106–109. doi: 10.1097/00005131-199702000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Ruedi TP, Allgower M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res. 1979 Jan-Feb;(138):105–110. [PubMed] [Google Scholar]
- 21.McCarthy ML, MacKenzie EJ, Edwin D, Bosse MJ, Castillo RC, Starr A. Psychological distress associated with severe lower-limb injury. J Bone Joint Surg Am. 2003 Sep;85-A(9):1689–1697. doi: 10.2106/00004623-200309000-00006. [DOI] [PubMed] [Google Scholar]


