Abstract
The measurement of functional capacity in mental illness is an important recent development. Determination of functional capacity may serve as a surrogate marker for real-world functioning, thereby aiding clinicians in making important treatment determinations. This manuscript provides an overview of a model of functioning, discusses the various areas of functioning relevant to real-world functioning in persons with mental illness, and reviews existing measures that assess functional capacity. Limitations of existing methods of assessing functional capacity are discussed and future areas of research are suggested.
Functional capacity refers to an individual’s capability, under controlled conditions, to perform tasks and activities that are necessary or desirable in their lives. In this paper we emphasize capacity, that is, how well someone can perform a task under ideal or nearly ideal conditions. In the perfect world a person’s functional capacity performance would relate perfectly to their performance in the real world, and could therefore serve as a proxy for their ability to perform that behavior in the real world. Unfortunately, as discussed below, this is not the case. However, given difficulties with measurement of behavior in the real world, measurement of functional capacity provides us with information that allows us to examine the effects of disease on performance of an individual, to compare how specific diseases impact ability to perform specific tasks, and how specific treatments (e.g., medications, psychosocial interventions) improve performance on skills critical to their lives. Clearly the measurement of functional capacity is specific to different roles or tasks, and to specific disorders. In this discussion we focus on functional capacity as it relates to the skills needed by patients with schizophrenia to function independently. We begin our discussion with an overview of models of functioning. We move on to discuss approaches to measuring functional capacity, which areas should be considered in these measures, and describe available measures of capacity.
Models of Disablement and Functional Capacity
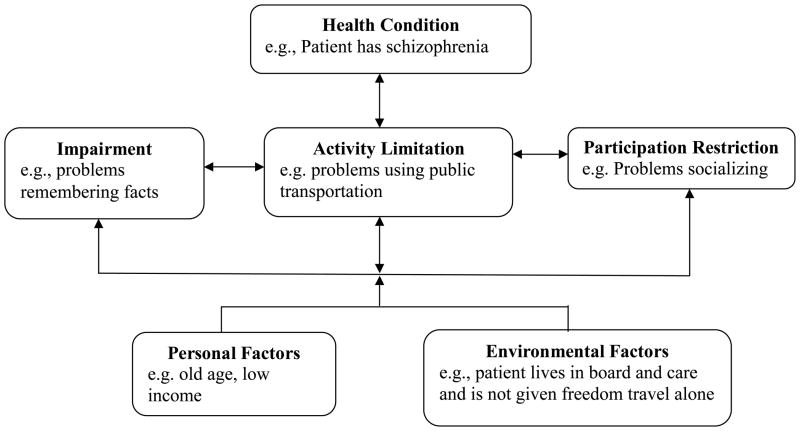
As has been described previously (McKibbin et al 2004), placing functioning into context requires consideration of models of disablement or disability (or conversely, functioning). Such models are useful in conceptualizing and testing the efficacy and effectiveness of psychosocial and pharmacologic interventions designed to improve functioning. The past three decades has seen a number of proposed disablement models, each of which has conceptual limitations (National Advisory Board on Medical Rehabilitation Research 1992). Most recently, the World Health Organization developed what they termed a revised working disability model (see Fig. 1). This model provided conceptual clarity to constructs and operationalized functioning across three levels (Nagi 1976; Pope & Tarlov 1991; Vebrungge & Jette 1994; Whiteneck et al 1997): a) the body; b) the person as a whole; and c) the person in social contexts. For example, in schizophrenia, disability involves dysfunction at one or more of these levels. At the body level, impairments in body function or structure may be reflected by micro- and macro-deviations in brain structure (e.g., frontal lobe) as well as cognitive (e.g., memory, attention) and psychiatric deficits (e.g., hallucinations, delusions). In the person as a whole, Activity Limitations may be reflected as difficulties in executing activities, such as difficulty with mental calculations (e.g., counting change) or producing logical, fluent, and goal-directed speech. Finally, Participation Restrictions (i.e., person in social contexts), problems experienced in real life situations, refer to the total life context of the individual, and may occur when a person cannot maintain a bank account, participate in meaningful work activities, or join community activities (McKibbin et al 2004).
Figure 1.
World Health Organization (WHO) Model of disablement
Recent literature has expanded our understanding of the specifics of the WHO disablement model described above. For example, there is growing evidence for the central role that cognitive deficits play in determining functional capacity in individuals with psychiatric disorders. The centrality of cognition grows as people age. This is due in part to declines in the severity of symptoms of psychopathology, and also because cognitive impairments may cross thresholds to create impairment. Beyond the influence of cognitive impairments on functional capacity, specific psychiatric symptoms may influence functioning more than others. For example, the functioning of patients with schizophrenia appears to be influenced more by negative symptoms than positive symptoms (Cardenas et al 2008). Other work suggests that among older adults with severe mental illnesses, earlier age of onset of illness is associated with greater functional impairments compared to those with later onset. Earlier onset may be a proxy for a more severe form of the illness, because patients have a longer time to accrue deficits, or because the period during which these individuals have to establish social roles free of illness is shortened. Other work suggests that co-morbidities such as substance abuse contribute to functional capacity. Clearly, the environment in which the individual functions influences their actual performance of a behavior, and through that practice their capacity to perform the behavior in other environments. In fact some interventions designed to improve functioning in patients with schizophrenia specifically emphasize environmental supports which enable patients to compensate for their cognitive deficits (Velligan et al 2000).
Within the WHO model there are likely to be additional paths which are present. For example, if an individual has Schizophrenia, a Psychiatric Health Condition, it is likely to relate to their psychological status, and perhaps has a direct relationship to their functional capacity. It is also possible that this relationship is mediated by other internal factors which enable or moderate it. For example, Bowie et al. (2006) suggested that the relationship between adaptive life skills in real-world settings and performance on neuropsychological tests may be complicated by other factors that interfere with use of such skills in everyday life. They used functional capacity data collected using the UCSD Performance-Based Skills Assessment (UPSA) (Patterson et al 2001a), and real-world functioning (using case manager rating of interpersonal skills, work skills, and community activities), neuropsychological performance, and symptoms in a group of patients with Schizophrenia to examine the relationships between these variables. More specifically, they used confirmatory path analyses to evaluate the effects of neuropsychological performance, functional capacity, and symptoms on the various domains of real-world functioning. Their findings suggested that neuropsychological performance predicted functional capacity, which predicted all three domains of real-world functioning. Psychiatric symptoms, specifically depression, predicted interpersonal and work skills, while negative symptoms affected interpersonal skills independently of other predictors. However, while real-world adaptive life skills were predicted by neuropsychological performance, symptoms, and functional capacity, neuropsychological performance contributed little to the prediction of real-world performance after accounting for functional capacity. Other symptoms, such as negative symptoms, like amotivation, may also impact outcomes as well (Harvey & Bellack 2009). Indeed, depressive symptoms which is frequently associated with schizophrenia (Siris 2000) has also been independently associated with deficits in vocational functioning (Bowie et al).
It is clear that functional deficits are the result of a complex set of determinants. While cognitive impairments are often associated with disability across a range of neuropsychiatric conditions (Heaton & Pendleton 1981), neuropsychiatric deficits account for only a moderate amount of variance in everyday functional impairments, with correlations are in the range of r=.3 to r=.5 (Albert et al 1995; Green 1996). There are several factors that could potentially impact real-world functional deficits beyond an individual’s ability to perform the skills needed to engage in those activities. For example, normal-range cognitive functioning was recently found to be a strong predictor of residential functioning in people with schizophrenia (Leung et al 2008), but was not related to social (e.g., marriage) or vocational (e.g., full-time employment) attainment. Similarly, Rosenheck et al (2006) reported that while cognitive performance was correlated with occupational status in people with schizophrenia, racial status, and disability status and compensation had a much larger influence on employment status. Furthermore, in a recent cross-national study (Harvey et al 2009), people with schizophrenia in the US and Sweden performed identically on measures of everyday living skills, while they differed minimally on performance on a clinical NP assessment, and were rated as equally impaired in their ability to live independently by their case managers. Remarkably, individuals from Sweden were more than twice as likely to be living independently as their American counterparts. This was likely due to generous disability compensation and housing supports that Swedish individuals received from the health authority.
What functional skills should be assessed?
In their most basic form, skills needed to function independently have been termed “activities of daily living” (ADLs), which reflect a person’s ability to perform the most basic of self-care functions, and “instrumental activities of daily living” (IADLs), which consist of functions that may be needed for independence depending on allocation of tasks in a family, or demands made by a person’s life. Historically, the most widely used measure of ADLs was developed by Katz and colleagues (1963) which classified people as independent or dependent on each of six ADL functions (i.e. bathing, dressing, using the toilet, transferring in and out of beds or chairs, eating, and continence which is usually removed because it is more indicative of a physiological state than a function). Other ADL measures focus on particular functions in more detail (Loewenstein et al 1989), while others add tasks (e.g., walking a specified distance), (Reuben & Sui 1990). At the grossest level, individuals are considered to be independent within a particular function if they can perform the function without help, even if they require some type of equipment or aid to perform the function, and dependent if they require help from someone to perform the behavior. Instrumental Activities of Daily Living (IADLs) (Lawton & Brody 1969) are functions that may be needed for independence in a particular setting in which demands are made by a person’s environment. Examples of IADLs include cooking, cleaning, laundry, shopping, making and receiving telephone calls, driving or using public transportation, and taking medicines.
Regardless of the specific domain under consideration, deficits in functional capacity can be the result of physical problems, cognitive impairments, lack of social skills, or lack of motivation, or a combination of these factors. Thus, interventions seeking to improve an individual’s functional ability (e.g., ability to manage their own finances) can target anyone or a combination of these problems. For example, if memory loss is the reason for functional impairment, some people might be able to perform the function with cueing and reminders. It is beyond the scope of this discussion to review interventions to improve functional independence.
Evaluation of functional capacity is based on the measurement of the functional consequences of impairment related to the specific condition under consideration. Further, individuals assume several roles in society (e.g., worker, patient), and impairment should occur in tasks that are pertinent to the particular role under consideration. For example, if the goal of an assessment is to determine if the level of disability affects capacity to perform work skills, it will be necessary to measure functional capacity relevant to the work skills rather than functional capacities related to being a patient (e.g., medication management). As discussed below, a major issue for such assessments is the approach used to assess functioning. The emphasis in the present discussion is on the measurement of capacity to function in the real world. However, we will focus our discussion on assessments conducted under controlled conditions. By focusing on real-world assessment in controlled conditions (i.e., functional capacity), we establish an individual’s maximum level of functioning on skills deemed necessary to function independently.
Approaches to measuring functioning
There are many methods for evaluating outcomes (e.g., functional capacity), each of which has its own advantages and disadvantages. The advantages and disadvantages of each of these methods are discussed below. However, before we begin that discussion, it is useful to think about the measurement of quality of life. Interestingly, while the literature is replete with discussion on the measurement of quality of life, there has been little discussion on the association between functional capacity and quality of life, which we feel will further enrich the present discussion.
Assessment of quality of life has focused on two major approaches: 1) psychometric evaluation, and 2) decision theory. The psychometric approach is used to offer a profile summarizing different dimensions of quality of life. The best known example of the psychometric tradition is the Medical Outcomes Study 36-Item Short Form (SF-36) (Ware & Gandek 1998). In contrast, the decision theory approach attempts to weight the different dimensions of health in order to provide a single expression of health status. Supporters of the latter approach argue that psychometric methods fail to consider that different health problems may be listed as a symptom (e.g., both a minor itch and coughing up blood are symptoms), the importance of these symptoms are not equivalent. Thus simple symptom counts may miss the severity or impact of more serious complaints. A parallel problem exists with functional measures. A measure which only considers how many roles an individual engages in is likely to miss the fact that their participation in a particular role may be impaired. In addition, it is possible that some aspects of functioning may improve over time, while others get worse. For example, patients with schizophrenia may have fewer positive symptoms as they get older, but their memory may become more impaired. The sum of these symptoms may result in poor ability to manage their finances in both young and old patients, but the components contribute differently at different ages. When components of outcome change in different directions, an overall subjective evaluation, or some objective measure of ability to perform the function, may be needed to integrate the components and offer a summary of whether the patient is better or worse off.
In addition to the distinction between psychometric and decision theory approaches, measures can be classified as either generic or targeted to a specific disease. Generic measures can be used with any population, while disease targeted measures are used for patients with a particular diagnosis. Furthermore, measures can be divided by their uses. Most measures can be used to characterize populations and to study clinical changes. However, only generic, decision theory based measures can be used to evaluate cost-effectiveness since a single composite score is needed for such calculations.
Therefore, because functioning is ultimately tied to quality of life, when considering methods of assessing functioning, one should also consider how these methods ultimately impact the individual’s quality of life. As mentioned above, an individual’s everyday functioning may be measured by several approaches, including direct observation, self-report, proxy report, and performance-based measures of functional capacity. Each approach has advantages and disadvantages which we discuss below.
Direct Observation
Logically, direct observation of a person’s activities in natural settings would provide the most reliable information about their actual functioning. However, the length of time and resources required to collect reliable data on a person’s complete behavioral repertoire would be far in excess of what is practical for research or clinical practice.
Self-report
Self-report interviews ask a person to judge and report their own level of functioning. Self-reports have the virtue of simplicity, being economic both in terms of time to gather information and actual costs, and they incorporate a persons’ own perception of how well they are functioning. However, a person’s ability to accurately report their own behavior can be effected by a number of factors. For example, the reliability of patients with schizophrenia may be affected by poor insight or other psychopathological symptoms. For example, Atkinson, Zibin, and Chuang (1997) administered two quality of life measures to patients with schizophrenia, one based on self-report, and another based on objective indicators. They found that the patients’ judgment of their own personal situations had little relationship to their actual life conditions. Rather, the patients’ judgment was more likely to be a reflection of their pathology, cognitive abilities, or recent events. Normal individuals may over report or underreport their ability to function depending on the consequences of their reports (cite). Thus, self-reports may produce suspect information which may be neither a valid nor reliable measure of a patient’s actual level of functioning.
Caregiver/Proxy Report
Another frequently used method is to gather proxy data from a significant other or caregiver. However, proxy reports may be problematic since individuals may not be able to identify a suitable proxy. For example, Patterson and colleagues (1996) found that as many as two-thirds of older patients with schizophrenia were not able to name a caregiver who could provide a report on how they were functioning. Even when an appropriate proxy is identified, there may be significant discrepancies between patients’ and the proxies’ reports of functioning (Sainfort et al 1996). In some cases discrepancies may be due to poor insight by the individual. In other cases the proxy may not have observed the person’s full spectrum of behavior, and may under- or over-report the subject’s ability to perform the behavior in question. This may be particularly problematic for individuals who reside in board-and-care or assisted living facilities, where the proxy may only be exposed to a limited repertoire of the subjects’ behavior, and it is neither practical nor appropriate for the assessor to decide whether the patient or proxy report is more accurate.
Performance-based Measures
The limitations present in other methods led to the development of performance-based measures of functional capacity. Performance-based measures assess the capacity of an individual to perform specific skills required for independent living (e.g., financial, household management, communication, and social skills) in a controlled situation. This is in contrast to real world assessments which occur in situations which may be effected by external distractions such as background noise. Performance-based measures are conducted in controlled environments using props and role-plays where appropriate. Because the patient is demonstrating behaviors in an “ideal” environment, one limitation of performance-based assessments is their validity to transfer to real-world functioning. However, as noted by Green and colleagues (2008), capacity measures remove mediating variables such as motivation and opportunity that are difficult to measure. Further, improvements in capacity are more likely to be temporally linked with improvements in cognitive ability, which increases the measure’s sensitivity to change. Since performance-based measures of capacity are administered in a controlled environment that may mitigate these confounds, we argue they are the optimal form of functional measurement.
Measures of Functional Capacity
In the section below we provide a summary of measures that have appeared in the literature between 1990 and 2009, when this review was conducted. In order to limit our discussion, measures are limited to those which focus the measurement of functioning, either functional capacity, functional recovery, or functional outcome, and were developed for use with individuals with schizophrenia or schizoaffective disorder. In addition to a brief description of the measures we focus our discussion on the measure’s validity, reliability, and relationship to real world outcomes such as independence, communication, or community functioning.
We should also point out our distinction between functional capacity and functional attainment. What we describe below are assessments of functional capacity, or one’s ability to perform tasks similar to those found in the real-world. Indeed, these tasks are typically assessed in a controlled environment using structured role-plays with props often found in the real-world. The construct of capacity differs from functional attainment, which we would define as a sustained level of functioning necessary to function independently in the “real-world.” Therefore, one would need to establish higher levels of functional capacity prior to demonstrating functional attainment. In the sections below, we demonstrate how tests of functional capacity link to at least immediate assessments of functional attainment.
University of California, San Diego (UCSD) Performance-Based Skills Assessment (UPSA)
The UPSA was developed as a means of assessing basic everyday living skills in older people with schizophrenia. It was designed to assess the capacity of individuals to perform skills in five areas that are critical to independent living. The 5 subtests focus on Planning/Organization (e.g., planning a trip to the beach/zoo), Managing Finances (e.g., counting change; writing a check), Communication skills (e.g., calling information to request a phone number; calling the doctor to reschedule an appointment), using Transportation (e.g., reading a bus route map), and Household management (e.g., completing a shopping list; reading a recipe). Each subtest yields a score ranging from 0 to 20 which summed to create a total score (range = 0–100). The UPSA requires approximately 30 minutes to administer, requires no specialized qualifications for administration, and can be administered by a trained paraprofessional. The reliability of the UPSA appears to be excellent. Harvey et al (2007) report excellent reliability statistics for the UPSA, with both schizophrenia/schizoaffective disorder patients and normal comparison participants. Specifically, the interrater reliability coefficient was .91; and 2-week test-retest reliability was .93. In another study of 176 participants with schizophrenia, the 4-week test-retest reliability was .70 (Green et al 2008). Using data from the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) trial, Green and colleagues (Green et al 2008) suggest that the UPSA practice effects were small, with a Cohen’s d effect size of 0.23.
A number of studies suggest that the USPA demonstrates strong convergent validity. For example, schizophrenia patients perform worse on all subscales and the total scores compared to normal controls (Patterson et al 2001a). In other work, UPSA scores were significantly correlated with overall cognitive performance, which was significantly higher than the correlations between cognitive performance and two interview-based measures (i.e., the Schizophrenia Cognition Rating Scale; the Clinical Global Impression of Cognition in Schizophrenia—Neurocognitive State Composite score) (Green et al 2008). In addition, the correlations between the UPSA and cognitive performance measures were also significantly higher than that between cognitive performance and the Maryland Assessment of Social Competence Effectiveness score.
The UPSA has also been shown to have good criterion validity with a number of real-world outcome measures. For example, Twamley and colleagues (2002) found that among a sample of schizophrenia patients, level of residential independence was significantly related to their total UPSA scores. Mausbach et al (2008a) used the UPSA to predict the current residential status of 434 middle-aged and older adults with schizophrenia or schizoaffective disorder. Participants were classified as either independent (residing alone in a house or apartment) or non-independent (residing in a care facility such as board and care, skilled nursing facility, etc.). The UPSA predicted current living status with 68% accuracy when a cutoff of 75 was used. The UPSA also appears to be useful in predicting engagement in community responsibility. Cardenas and colleagues (2008) assessed the ability of a group of middle-aged and older Latinos with schizophrenia to engage in various activities including working for pay, doing volunteer work, and going to school. Results from this study suggest that individuals who were able to engage in more activities had higher UPSA scores. More specifically there was a linear relationship between UPSA scores and number of responsibilities: UPSA was 44.9 for those who engaged in 0 activities; 58.1 for those who engaged in 2 activities, and 67.4 for those who engaged in more than two activities. Using a modified version of the UPSA, Bowie et al (2006) examined the relationship between the UPSA and an observer-rated measure of real-world functioning, the Specific Level of Functioning (SLOF) Scale. Case managers used the SLOF to rate the personal care skills, interpersonal skills, community activities, and work skills of participants with schizophrenia or schizoaffective disorder and found that patients who performed better on the USPA had significantly better functioning in their interpersonal skills, community activities, and work skills. In other work with 222 participants with schizophrenia or schizoaffective disorder, higher scores on the UPSA were related to better ratings of patient performance in Community Activities and Work Skills (Bowie et al 2008b). Finally, the UPSA has been shown to be sensitive to change in at least three clinical trials designed to improve functioning. The first was in a sample of older patients with schizophrenia (Patterson et al 2006a). The second was with Hispanic/Latino patients with schizophrenia (Patterson et al 2005). The third trial was a Cognitive Behavioral Social Skills Training program for older patients with schizophrenia (Granholm et al 2005).
Because the full version of the UPSA may present as a burden to both clinicians and patients, recent modifications have been made to the UPSA to make it briefer and more convenient to administer (Mausbach et al 2007). This abbreviated version of the UPSA, known as the UPSA-Brief (Mausbach et al 2007) requires an average of 10–15 minutes to administer, and consists of 2 of the original 5 subscales from the full UPSA (i.e., Finance and Communications subscales). The UPSA-Brief requires no specialized qualifications for administration and, in addition to saving administration time, it requires fewer props. However, the reliability of this scale has yet to be established. The validity or relationship to real-world outcomes of this measure appears to be good. Because the UPSA-B was derived from the UPSA it is not surprising that they are highly correlated (Pearson r = .91). Data suggest that the UPSA-Brief is correlated with measures of overall cognitive functioning and educational attainment but less correlated with symptoms of psychosis (Mausbach et al 2007). Similar to results for the full version of the UPSA, UPSA-Brief scores are significantly associated with concurrent residential status (i.e., independent vs nonindependent) (Mausbach et al 2007), with scores of 60 or greater most discriminating of individuals who were and were not residing independently in the community. In addition, UPSA-Brief scores appear to adequately predict concurrent level of community responsibility (Mausbach et al 2008b; Mausbach et al 2007)
Since the UPSA-Brief was only recently introduced, little data on its utility in clinical trials are available. Mausbach and colleagues (2007) demonstrated that change on the UPSA-Brief improved significantly for participants who had received a behavioral skills training intervention. The authors also reported that 35% of participants in the skills-training condition, compared to 18% in the control condition, moved from below the cutoff score of 60 to above.
Social Skills Performance Assessment
The Social Skills Performance Assessment (SSPA) (Patterson et al 2001b) uses role plays to assess an individual’s capacity to engage in everyday social interactions. For three minutes participants play the role of a tenant meeting a new neighbor (played by the interviewer). A second three minute role play involves a tenant, played by the participant, contacting his/her landlord, played by the tester, discuss a leak that has yet to be repaired after a previous complaint. For both role-plays, participants are scored on a) their willingness to engage in the interaction, b) overall flow of conversation, c) ability and willingness to express themselves clearly and directly, d) ability to concentrate on and track the role-play, e) tone of voice, f) body posture, g) physical appearance, h) social appropriateness, and i) overall conversation. For the second role play, additional scoring includes the individual’s: a) ability to generate solutions and make compromises, b) ability and willingness to stick firmly to the goal of reaching a solution, c) overall argument, and d) social appropriateness. Patterson and colleagues (2001b) reported excellent interrater reliability (intraclass correlation = .91) and 1-week test-retest reliability (.92) for the SSPA total score. The validity and relationship to real-world outcomes of the SSPA was suggested by schizophrenia group scoring significantly lower than normal controls, scores on the SSPA being positively correlated with the quality of well-being (QWB), and it being inversely correlated with negative symptoms of psychosis and worse cognitive functioning (Patterson et al 2001b). Other work by Pratt and colleagues (2007) found very high interrater reliability (item characteristic curve = .99), and scores on the SSPA were positively and significantly correlated with cognitive functioning (ie, DRS scores) in a sample of patients with severe psychiatric disorders including schizophrenia. Other work also suggests significant positive relationships between SSPA scores and overall cognitive ability (Patterson et al 2001b). Less work has been conducted demonstrating the relationship between the SSPA to real-world outcomes. The SPAA was positively associated with interpersonal behavior, work skills, and community activity participation in a sample of 222 outpatients with schizophrenia (Bowie et al 2008b). Finally the SSPAs sensitivity to change has been demonstrated in two clinical trials (Patterson et al 2005; Patterson et al 2006a).
Medication Management Ability Assessment
The Medication Management Ability Assessment (MMAA) (Patterson et al 2002) is a brief role-play test designed to assess prescription medication management ability in older adults with schizophrenia. Participants are presented with 4 prescribed mock medications, and the interviewer describes the medication regimen to the participants and after a one hour delay, they are asked to walk the interviewer through their day, giving the interviewer pills as they would take them throughout the day. Participants are scored on taking their meds at the correct time, and taking them with or without food. The test-retest reliability for the MMAA ranges from .48 to .96 (Green et al 2008; Patterson et al 2002). The lower reliability may be due to ceiling effects seen in the Green et al. study. The MMAA has good ecological validity, patients with schizophrenia or schizoaffective disorder score worse compared to normal age matched controls. Also, construct validity is adequate, whereby the MMAA is significantly correlated with negative symptoms, the QWB, and the Mini Mental State Examination (MMSE) (Patterson et al 2002). Other researchers have examined the relationship of the MMAA cognitive performance and found it was more highly correlated than the Maryland Assessment of Social Competence, Schizophrenia Cognition Rating Scale, Clinical Global Impression of Cognition in Schizophrenia, and the Global Assessment of Functioning (GAF) (Green et al 2008). However they also reported that the MMAA was only modestly related to self-reported measures of global (r = .18) and work functioning (r = .26), and it was unrelated to self-reported social and independent living. Finally, two studies have examined change on the MMAA as a function of treatment (Patterson et al 2005; Patterson et al 2006b), with both showing little impact of the active treatments on MMAA scores, which may be a function of the MMAA’s relatively low test-retest reliability.
Test of Adaptive Behavior in Schizophrenia (TABS)
The TABS (Velligan et al 2007) is a functional capacity role play test which taps five domains: (a) Medication Management Skills, (b) identify what items are needed in an empty bathroom so they could use it every day, (c) using a map to get to a store, shop for items by viewing pictures of supermarket aisles, and identify when they have not received correct change, (d) selecting appropriate clothes for various circumstances, (e) correctly collate flyers, and (f) a rating of the patients social skills during the test. The examiner also rates two additional constructs deemed important to functioning among schizophrenia: (a) initiation of tasks, and (b) identifying problems that occur during the course of functional activities. Reliability was strong (Velligan et al 2007), Cronbach’s alpha for all items reported as .84, and test-retest reliability over a 3-month period was also good, with the Pearson correlation coefficient and intraclass coefficient both being .80. Significant correlations between the TABS and the Multnomah Community Ability Scale (.49), the Social and Occupational Functioning Scale (.43), and the Independent Living Scales (ILS; .58) suggest the validity of the scale is good (Velligan et al 2007). TABS scores were significantly related to negative symptoms (r=.56) but not to positive symptoms (r=.12), and scores were significantly worse for persons with schizophrenia compared to normal controls. No reports of the association of the TABS with real-world (e.g., employment), or its sensitivity to change in response to interventions were found at the time of this review.
Independent Living Skills Survey (Self-Report Version)
There are two versions of the Independent Living Skills Survey (ILSS) (Wallace et al 2000). The first relies on an informants report (ILSS-I), while the second is a self-report form (ILSS-SR). Here we focus on the self-report version which consists of 70 items taping into 10 domains of functioning: (a) Personal Hygiene, (b) Appearance and Care of Clothing, (c) Care of Personal Possessions and Living Space, (d) Food Preparation, (e) Care of Personal Health and Safety, (f) Money Management, (g) Transportation, (h) Leisure and Recreational Activities, (i) Job Seeking, and (j) Job Maintenance. Internal reliability for a large sample (Wallace et al 2000) of individuals with “Severe and Persistent Mental Illness” for the 10 subscales was mixed, ranging from .435 for the Transportation subscale to .90 for the Job Seeking subscale. Six subscales had coefficients below .70. Similar internal consistency values were reported with in a sample of middle-aged and older adults with psychosis, and six-month test-retest coefficients ranged from .418 for the Leisure and Recreational Activities subscale to .904 for the Job Maintenance subscale (Perivoliotis et al 2004). Validity for the ILSS-SR is suggested by its significant correlations with scores on the Brief Psychiatric Rating Scale (BPRS), the Profile of Adaptation to Life—Change version, and the Global Assessment Scale (GAS) (Perivoliotis et al 2004). In addition, older patients with psychosis score significantly worse on the ILSS-SR compared to nonpsychiatric participants of a similar age, and patients with more symptoms scored worse than those with fewer symptoms (Perivoliotis et al 2004). Wallace and colleagues (2000) examined the relationship between ILSS-SR score and 2 measures of employment (i.e. whether or not the participant worked at least 1 month and earned a minimum of $300 during the month of work; and, whether or not the participant “worked at that income level for either 6 continuous months or the last 3 months of the follow-up period” and the ILSS-SR was the best predictor of employability and second best predictor of sustained employability. Finally ILSS-SR scores have been shown to be sensitive to a skills-training intervention compared to an occupational therapy intervention (Liberman et al 1998) and to a CBSST intervention compared to a treatment as usual condition (Granholm et al 2005).
Global Assessment of Functioning (GAF)
The GAF scale is a clinician-rated measure of an individual’s overall functioning (American Psychiatric Association 2000). Clinicians rate an individual’s functioning on a scale from 1 to 100 with 100 indicating superior functioning. Interrater reliability for the GAF are range from .89 to .95 with a group of schizophrenia patients (Startup et al 2002), .61 to .91 for the GAS, a precursor to the GAF with a general mental health population (Endicott et al 1976), .56 to .76 among hospital patients (Jones et al 1995) and .86 to .92 among an outpatient sample (Hilsenroth et al 2000). A GAF review article reported the interrater reliability of the ranging from .62 to .96. (Burlingame et al 2005). In regards to validity, Startup and colleagues (2002) found that GAF ratings were generally unrelated to concurrent measures of clinical symptoms or social behavior prior to receiving treatment, but were highly negatively correlated with clinical symptoms and social functioning following treatment. An additional study (Roy-Byrne et al 1996) used a revised version of the GAF which considered only social and occupational functioning (i.e., excluding psychological symptoms) to rate overall functioning, and found that board certified psychiatrists ratings did not differ significantly for individuals who were homeless vs. those with homes. Other work demonstrated that GAF ratings did not differ significantly between psychiatrists between patients who required maximum supervision, moderate supervision, or minimum supervision (Revheim & Medalia 2004a). Finally, a review of 10 treatment studies suggested that the GAF is highly sensitive to change (Burlingame et al 2005).
The ILS (Loeb 1996)
The ILS is a self-report measure of an individual’s competency to perform daily functioning activities and to for care for themselves. The scale consists of 5 subscales: (a) Memory/Orientation, (b) Money Management, (c) Management of Home and Transportation, (d) Health and Safety, and (e) Social Adjustment which are added together to create an overall score ranging from 0 to 140, with higher scores indicating better performance. Alternatively two subscales can be created: (a) Performance/Information and (b) Problem Solving, the latter of which is commonly used as a measure of problem solving required of individuals independently residing in the community (Revheim & Medalia 2004a; b). Standard cut points have been provided to aid in making decisions regarding the level of supervision an individual requires in the community (Loeb 1996). The coefficient alpha for the entire ILS is .86, test-retest reliability is .90, and interrater reliability is .98 (Revheim & Medalia 2004a). Discriminate validity has been shown: clinical samples score significantly lower than nonclinical samples (Revheim & Medalia 2004a; b). In addition, ILS scores are strongly correlated with Wechsler adult intelligence Scale-revised comprehension scores (r = .65) (Revheim & Medalia 2004a), and is related to several neurocognitive tests (Revheim et al 2006). Finally, the ILS has been associated with several real world outcomes including sensitivity to residential status (Revheim & Medalia 2004b; Revheim et al 2006), and living situation (Medalia et al 2001). The ILS has also been shown to be sensitive to change associated with a cognitive remediation intervention (Medalia et al 2001).
Final Thoughts and future directions
We have argued that assessment of functional capacity is a valid and useful approach to characterize how well an individual is able to function in the real world. While there are a variety of measures available to assess functional capacity, the approaches to how such data are gathered vary. Because each approach has its own set of pros and cons, and because little work has been conducted comparing the various scales for assessing functional capacity, clinicians are left to weigh the costs and benefits of each assessment tool to help them determine a patient’s functional capacity or ability to function in their personal environments.
A recent review of the existing methods for assessing functional capacity has led to the conclusion that performance-based measures may exceed other approaches in terms of reliability and validity (Mausbach et al 2009). However, a clear limitation of performance-based measures is that performance is measured under controlled conditions which may not reflect an individual’s true performance in the “noisy” real world. In addition, existing literature appears focused on general, global outcomes such as independent-living vs. non-independent, and working vs. not working. However, little is known about the ability of existing measures to predict more specific areas of functioning such as quality of work and varying intermediate levels of independence. Validating measures against these outcomes would be helpful for clinicians, who often are faced with making more precise decisions about their patients’ level of independent functioning.
Further, little research examines a modular approach to examining functioning in multiple domains. For example, research on the UPSA has focused on the “summary score” and its ability to predict functional outcomes. Little is known if specific subtests may be enough to predict specific areas of functioning. For example, it is unclear if the UPSA subscales (e.g., finance skills; communication skills) assess one’s ability to actually perform skills in these specific domains, or if these subscales are simply different ways of measuring global functioning. Existing data suggests the latter, and little has been done to test the specificity of the UPSA subscales. A related issue is whether adding scales such as the SSPA and MMAA, which measure social and medication management skills, respectively, provide incremental validity to other scales (e.g., the UPSA) for predicting overall functional ability. That is, if the UPSA (and its respective subscales) assesses global functioning, including medication management and social skills, do domain specific scales such as the SSPA and MMAA provide better prediction of these specific domains?
As reviewed, researchers and clinicians have a variety of measures available to choose from. While the measurement of functional capacity is a relatively new field, there is a growing list of measures that are specific to particular populations, and more general measures. Clinicians and policy makers will demand meaningful cut points to guide their decision making. Few papers are available for any of the measures reviewed in this paper and this area clearly is in need of more research. In this review we provide a model of functional capacity which we hope will stimulate research to explore relationships between variables which will result in refinements to this model.
Functional capability is most appropriately examined with reference to particular life-cycle tasks that an individual may need to perform. However, little research has examined whether or not there is a need to separate measures for children, adults, and geriatric populations. For children, functional requirements may include learning at school, participating in play, and involvement in family life. For adults, functional abilities in the labor force are important, as well as (in many cases) activities related to rearing and inter-acting with their children. Some assessment tools examine the ability to perform such age-related tasks in some detail. Other assessment tools, especially those used in large-scale research, attempt to use questions that work for all age groups. An example of a general question about functional capacity would be: “How often are you unable to perform your usual activities because of illness or disability?” This approach would be less than optimal for persons of retirement age, who may not have a wide range of “usual activities.” A narrower, more general approach is to ask how many days an individual has been in bed because of illness or disability in a particular time period. The most common approach is to consider ability to perform each in a list of specific tasks or activities.
It is important to consider the sensitivity of measures over time. An evaluation of functional capacity represents a snapshot in time. Psychiatric conditions are not static. While impairments associated with such conditions may be chronic and/or progressive, improvement in function or adaptation to functional loss over time frequently occurs. In order to determine if functional capacity has improved enough to warrant a change in disability coverage, or living situation, it is important for measures to be sensitive to improvements due to development, medication, or some psychosocial intervention.
In sum, we suggest that assessment of functional capacity, or functioning in controlled settings, is a valid and important task to help researchers, clinicians, and patients determine what resources are available to them (e.g., clinical treatments to address existing deficits; assisted living facilities; work training; etc). In this review and elsewhere (my prior review paper?), we find that performance-based measures outperform other methods of assessing functional capacity. These measures include the UPSA, UPSA-Brief, and the TABS, which appear best-suited to validly predict global “real-world” outcomes such as ability to work or live independently. However, more research is needed on these measures to determine more specific outcomes, such as work quality or semi-independent living. We further recommend that future research determine the validity of these measures for predicting outcomes for a wider variety of mental illnesses, such as major depression, dementias, etc, to determine their sensitity to specific life-cycles, and the sensitivity of these measures over time (e.g., response to treatment). Despite these current limitations, the promise of functional capacity measures to aid in determining functional outcomes is bright, and we remain hopeful that new research will continue to shed light on how to best help those who need functional aid.
Acknowledgments
Funding
National Institute of Mental Health (MH078775 to T.L.P.).
Footnotes
Conflict of Interest
Dr Patterson developed 4 tests reviewed in this article (ie, the UPSA, UPSA-Brief, SSPA, and MMAA) and Dr Mausbach has published several articles assessing these tests. Neither Dr Patterson nor Dr Mausbach has received financial compensation for the development or administration of these tests.
References
- Albert SM, Marder K, Dooneief G, Bell K, Sano M, et al. Neuropsychologic impairment in early HIV infection. A risk factor for work disability. Arch Neurol. 1995;52:525–30. doi: 10.1001/archneur.1995.00540290115027. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Atkinson M, Zibin S, Chuang H. Characterizing quality of life among patients with chronic mental illness: a critical examination of the self-report methodology. Am J Psychiatry. 1997;154:99–105. doi: 10.1176/ajp.154.1.99. [DOI] [PubMed] [Google Scholar]
- Bowie CR, Leung WW, Reichenberg A, McClure MM, Patterson TL, et al. Predicting schizophrenia patients’ real-world behavior with specific neuropsychological and functional capacity measures. Biol Psychiatry. 2008a;63:505–11. doi: 10.1016/j.biopsych.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie CR, Leung WW, Reichenberg A, McClure MM, Patterson TL, et al. Predicting schizophrenia patients’ real-world behavior with specific neuropsychological and functional capacity measures. Biological Psychiatry. 2008b;63:505–11. doi: 10.1016/j.biopsych.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real-world functioning performance in Schizophrenia: Correlations with cognition, functional capacity, and symptoms. American Journal of Psychiatry. 2006;163:418–25. doi: 10.1176/appi.ajp.163.3.418. [DOI] [PubMed] [Google Scholar]
- Burlingame GM, Dunn TW, Chen S, Lehman A, Axman R, et al. Selection of outcome assessment instruments for inpatients with severe and persistent mental illness. Psychiatric Services. 2005;56:444–51. doi: 10.1176/appi.ps.56.4.444. [DOI] [PubMed] [Google Scholar]
- Cardenas V, Mausbach BT, Barrio C, Bucardo J, Jeste D, Patterson T. The relationship between functional capacity and community responsibilities in middle-aged and older Latinos of Mexican origin with chronic psychosis. Schizophrenia Research. 2008;98:209–16. doi: 10.1016/j.schres.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33:766–71. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- Granholm E, McQuaid JR, McClure FS, Auslander LA, Perivoliotis D, et al. A randomized, controlled trial of cognitive behavioral social skills training for middle-aged and older outpatients with chronic schizophrenia. Am J Psychiatry. 2005;162:520–9. doi: 10.1176/appi.ajp.162.3.520. [DOI] [PubMed] [Google Scholar]
- Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–30. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- Green MF, Nuechterlein KH, Kern RS, Baade LE, Fenton WS, et al. Functional co-primary measures for clinical trials in schizophrenia: results from the MATRICS Psychometric and Standardization Study. Am J Psychiatry. 2008;165:221–8. doi: 10.1176/appi.ajp.2007.07010089. [DOI] [PubMed] [Google Scholar]
- Harvey PD, Bellack AS. Toward a terminology for functional recovery in schizophrenia: is functional remission a viable concept? Schizophr Bull. 2009;35:300–6. doi: 10.1093/schbul/sbn171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey PD, Helldin L, Bowie CR, Heaton RK, Olsson AK, et al. Performance-Based Measurement of Functional Disability in Schizophrenia: A Cross-National Study in the United States and Sweden. Am J Psychiatry. 2009 doi: 10.1176/appi.ajp.2009.09010106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey PD, Velligan DI, Bellack AS. Performance-based measures of functional skills: usefulness in clinical treatment studies. Schizophr Bull. 2007;33:1138–48. doi: 10.1093/schbul/sbm040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaton RK, Pendleton MG. Use of neuropsychological tests to predict adult patients’ everyday functioning. J Consult Clin Psychol. 1981;49:807–21. doi: 10.1037//0022-006x.49.6.807. [DOI] [PubMed] [Google Scholar]
- Hilsenroth MJ, Ackerman SJ, Blagys MD, Baumann BD, Baity MR, et al. Reliability and validity of DSM-IV Axis V. American Journal of Psychiatry. 2000;157:1858–63. doi: 10.1176/appi.ajp.157.11.1858. [DOI] [PubMed] [Google Scholar]
- Jones SH, Thornicroft G, Coffey M, Dunn G. A brief mental health outcome scale: Reliability and validity of the Global Assessment of Functioning (GAF) British Journal of Psychiatry. 1995;166:654–9. doi: 10.1192/bjp.166.5.654. [DOI] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moscowitz RW, Jackson BA, Jaffee MW. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. Journal of the American Medical Association. 1963;185:914–19. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- Leung WW, Bowie CR, Harvey PD. Functional implications of neuropsychological normality and symptom remission in older outpatients diagnosed with schizophrenia: A cross-sectional study. J Int Neuropsychol Soc. 2008;14:479–88. doi: 10.1017/S1355617708080600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberman RP, Wallace CJ, Blackwell G, Kopelowicz A, Vaccaro JV, Mintz J. Skills training versus psychosocial occupational therapy for persons with persistent schizophrenia. American Journal of Psychiatry. 1998;155:1087–91. doi: 10.1176/ajp.155.8.1087. [DOI] [PubMed] [Google Scholar]
- Loeb PA. Independent Living Scales (ILS) Manual. San Antonio: The Psychological Corporation; 1996. [Google Scholar]
- Loewenstein DA, Amigo E, Duara R, Guterman A, Hurwitz D, et al. A new scale for the assessment of functional status in Alzheimer’s disease and related disorders. J Gerontol. 1989;44:114–21. doi: 10.1093/geronj/44.4.p114. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Bowie CR, Harvey PD, Twamley EW, Goldman SR, et al. Usefulness of the UCSD Performance-Based Skills Assessment (UPSA) for predicting residential independence in patients with chronic schizophrenia. Journal of Psychiatric Research. 2008a;42:320–7. doi: 10.1016/j.jpsychires.2006.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach BT, Depp CA, Cardenas V, Jeste DV, Patterson TL. Relationship between functional capacity and community responsibility in patients with schizophrenia: Differences between independent and assisted living settings. Commun Ment Health J. 2008b;44:385–91. doi: 10.1007/s10597-008-9141-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach BT, Harvey PD, Goldman SR, Jeste DV, Patterson TL. Development of a brief scale of everyday functioning in persons with serious mental illness. Schizophrenia Bulletin. 2007;33:1364–72. doi: 10.1093/schbul/sbm014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach BT, Moore R, Bowie C, Cardenas V, Patterson TL. A review of instruments for measuring functional recovery in those diagnosed with psychosis. Schizophrenia Bulletin. 2009;35:307–18. doi: 10.1093/schbul/sbn152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKibbin CL, Brekke JS, Sires D, Jeste DV, Patterson TL. Direct assessment of functional abilities: relevance to persons with schizophrenia. Schizophr Res. 2004;72:53–67. doi: 10.1016/j.schres.2004.09.011. [DOI] [PubMed] [Google Scholar]
- Medalia A, Revheim N, Casey M. The remediation of problem-solving skills in schizophrenia. Schizophrenia Bulletin. 2001;27:259–67. doi: 10.1093/oxfordjournals.schbul.a006872. [DOI] [PubMed] [Google Scholar]
- Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Mem Fund Q Health Soc. 1976;54:439–67. [PubMed] [Google Scholar]
- National Advisory Board on Medical Rehabilitation Research. National Center of Medical Rehabilitation Research, National Institutes of Health. Bethesda, MD: 1992. [Google Scholar]
- Patterson TL, Bucardo J, McKibbin CL, Mausbach BT, Moore D, et al. Development and pilot testing of a new psychosocial intervention for older Latinos with chronic psychosis. Schizophrenia Bulletin. 2005;31:922–30. doi: 10.1093/schbul/sbi036. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV. UCSD Performance-based Skills Assessment: Development of a new measure of everyday functioning for severely mentally ill adults. Schizophrenia bulletin. 2001a;27:235–45. doi: 10.1093/oxfordjournals.schbul.a006870. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Lacro J, McKibbin CL, Moscona S, Hughs T, Jeste DV. Medication Management Ability Assessment: Results from a performance-based measure in older outpatients with schizophrenia. Journal of Clinical Psychopharmacology. 2002;22:11–9. doi: 10.1097/00004714-200202000-00003. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Mausbach BT, McKibbin C, Goldman S, Bucardo J, Jeste DV. Functional Adaptation Skills Training (FAST): A randomized trial of a psychosocial intervention for middle-aged and older patients with chronic psychotic disorders. Schizophrenia Research. 2006a;86:291–9. doi: 10.1016/j.schres.2006.05.017. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Mausbach BT, McKibbin C, Goldman S, Bucardo J, Jeste DV. Functional adaptation skills training (FAST): a randomized trial of a psychosocial intervention for middle-aged and older patients with chronic psychotic disorders. Schizophr Res. 2006b;86:291–9. doi: 10.1016/j.schres.2006.05.017. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Moscona S, McKibbin CL, Davidson K, Jeste DV. Social skills performance assessment among older patients with schizophrenia. Schizophrenia Research. 2001b;48:351–60. doi: 10.1016/s0920-9964(00)00109-2. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Semple SJ, Shaw WS, Grant I, et al. Researching the caregiver: Family members who care for older psychotic patients. Psychiatric Annals. 1996;26:772–84. [Google Scholar]
- Perivoliotis D, Granholm E, Patterson TL. Psychosocial functioning on the Independent Living Skills Survey in older outpatients with schizophrenia. Schizophrenia Research. 2004;69:307–16. doi: 10.1016/j.schres.2003.09.012. [DOI] [PubMed] [Google Scholar]
- Pope AM, Tarlov AR. Disability in America: Toward a National Agenda for Prevention. Washington, DC: National Academy Press; 1991. [Google Scholar]
- Pratt SI, Kelly SM, Mueser KT, Patterson TL, Goldman S, Bishop-Horton S. Reliability and validity of a performance-based measure of skills for communicating with doctors for older people with serious mental illness. Journal of Mental Health. 2007;16:569–79. [Google Scholar]
- Reuben DB, Sui AL. An objective measure of physical function of elderly outpatients: The physical performance test. Journal of the American Geriatric Society. 1990;38:1113–9. doi: 10.1111/j.1532-5415.1990.tb01373.x. [DOI] [PubMed] [Google Scholar]
- Revheim N, Medalia A. The independent living scales as a measure of functional outcome for schizophrenia. Psychiatric Services. 2004a;55:1052–4. doi: 10.1176/appi.ps.55.9.1052. [DOI] [PubMed] [Google Scholar]
- Revheim N, Medalia A. Verbal memory, problem-solving skills and community status in schizophrenia. Schizophrenia Research. 2004b;68:149–58. doi: 10.1016/j.schres.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Revheim N, Schechter I, Kim D, Silipo G, Allingham B, et al. Neurocognitive and symptom correlates of daily problem-solving skills in schizophrenia. Schizophrenia Research. 2006;83:237–45. doi: 10.1016/j.schres.2005.12.849. [DOI] [PubMed] [Google Scholar]
- Rosenheck R, Leslie D, Keefe R, McEvoy J, Swartz M, et al. Barriers to Employment for People With Schizophrenia. Am J Psychiatry. 2006;163:411–7. doi: 10.1176/appi.ajp.163.3.411. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne P, Dagadakis C, Unutzer J, Ries R. Evidence for limited validity of the revised global assessment of functioning scale. Psychiatric Services. 1996;47:864–6. doi: 10.1176/ps.47.8.864. [DOI] [PubMed] [Google Scholar]
- Sainfort F, Becker M, Diamond R. Judgments of quality of life of individuals with severe mental disorders: Patient self-report versus provider perspectives. Am J Psychiatry. 1996;153:497–502. doi: 10.1176/ajp.153.4.497. [DOI] [PubMed] [Google Scholar]
- Siris SG. Depression in schizophrenia: perspective in the era of “Atypical” antipsychotic agents. Am J Psychiatry. 2000;157:1379–89. doi: 10.1176/appi.ajp.157.9.1379. [DOI] [PubMed] [Google Scholar]
- Startup M, Jackson MC, Bendix S. The concurrent validity of the Global Assessment of Functioning (GAF) Br J Clin Psychol. 2002;41:417–22. doi: 10.1348/014466502760387533. [DOI] [PubMed] [Google Scholar]
- Twamley EW, Doshi RR, Nayak GV, Palmer BW, Golshan S, et al. Generalized cognitive impairments, ability to perform everyday tasks, and level of independence in community living situations of older patients with psychosis. Am J Psychiatry. 2002;159:2013–20. doi: 10.1176/appi.ajp.159.12.2013. [DOI] [PubMed] [Google Scholar]
- Vebrungge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Velligan DI, Bow-Thomas CC, Huntzinger C, Ritch J, Ledbetter N, et al. Randomized controlled trial of the use of compensatory strategies to enhance adaptive functioning in outpatients with schizophrenia. Am J Psychiatry. 2000;157:1317–23. doi: 10.1176/appi.ajp.157.8.1317. [DOI] [PubMed] [Google Scholar]
- Velligan DI, Diamond P, Glahn DC, Ritch J, Maples N, et al. The reliability and validity of the Test of Adaptive Behavior in Schizophrenia (TABS) Psychiatry Res. 2007;151:55–66. doi: 10.1016/j.psychres.2006.10.007. [DOI] [PubMed] [Google Scholar]
- Wallace CJ, Liberman RP, Tauber R, Wallace J. The independent living skills survey: a comprehensive measure of the community functioning of severely and persistently mentally ill individuals. Schizophrenia bulletin. 2000;26:631–58. doi: 10.1093/oxfordjournals.schbul.a033483. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol. 1998;51:903–12. doi: 10.1016/s0895-4356(98)00081-x. [DOI] [PubMed] [Google Scholar]
- Whiteneck GG, Fougeyrollas P, Gerhart KA. Elaborating the model of disablement. In: Fuhrer MJ, Brookes PH, editors. Assessing Medical Rehabilitation Practices: The Promise of Outcomes Research. Baltimore, MD: Brookes Pub Co; 1997. pp. 91–102. [Google Scholar]