Abstract
Background:
Parkinson’s disease (PD) is a chronic neurodegenerative disorder. There is limited knowledge about the function of the hypothalamic-pituitary-adrenal axis in PD. The primary aim of this prospective study was to analyze diurnal salivary cortisol concentrations in patients with PD and correlate these with age, gender, body mass index (BMI), duration of PD, and pain. The secondary aim was to compare the results with a healthy reference group.
Methods:
Fifty-nine PD patients, 35 women and 24 men, aged 50–79 years, were recruited. The reference group comprised healthy individuals matched for age, gender, BMI, and time point for sampling. Salivary cortisol was collected at 8 am, 1 pm, and 8 pm, and 8 am the next day using cotton-based Salivette® tubes and analyzed using Spectria® Cortisol I125. A visual analog scale was used for estimation of pain.
Results:
The median cortisol concentration was 16.0 (5.8–30.2) nmol/L at 8 am, 5.8 (3.0–16.4) at 1 pm, 2.8 (1.6–8.0) at 8 pm, and 14.0 (7.5–28.7) at 8 am the next day. Total secretion and rate of cortisol secretion during the day (8 am–8 pm) and the concentration of cortisol on the next morning were lower (12.5 nmol/L) in the reference group. No significant correlations with age, gender, BMI, duration of PD, Hoehn and Yahr score, Unified Parkinson’s Disease Rating Scale III score, gait, pain, or cortisol concentrations were found.
Conclusion:
The neurodegenerative changes in PD does not seem to interfere with the hypothalamic-pituitary-adrenal axis. Salivary cortisol concentrations in PD patients were increased in the morning compared with the reference group, and were not influenced by motor dysfunction, duration of disease, or coexistence of chronic or acute pain.
Keywords: cortisol, hypothalamic-pituitary-adrenal axis, Parkinson’s disease
Introduction
Parkinson’s disease (PD) is a chronic progressive neurodegenerative disorder accompanied by autonomic dysfunction and alterations in a number of regulatory mechanisms, including loss of circadian rhythms in dopaminergic systems and fluctuations in the kinetics of drugs used in treatment of the disease.1
Pain in PD is common. Our own investigations2 reveal an incidence of pain of about 60%. Other studies in this area reveal incidence rates of 40%–80%.3–7 The pathogenesis of pain in PD is probably complex. Degeneration of descending dopaminergic pain-inhibiting fibers from the midbrain is probably one of the central pathways. Dystonia, a motor symptom of PD, is a common explanation for pain. Direct effects of levodopa on pain sensation support the hypothesis of an influence of the regulating mechanisms of autonomic and inhibitory modulation of pain input in dopamine-dependent centers.8
Typically, signs of PD are hypokinesia, rigidity, and tremor, also referred to as the motor symptoms of the disease. Nonmotor signs, such as mood changes and pain, are frequent.9 The pathogenesis of the nonmotor symptoms is not fully understood, and concomitant endocrine dysfunctions have been suggested. There have been few studies in PD on endocrinopathy, such as hypothyreosis and cortisol deficiency. Munhoz et al showed that the secretion of thyroid and cortisol hormones is changed in PD, possibly caused by disturbances in the hypothalamic-pituitary-adrenal axis.10 A recent study by Aziz et al analyzed thyroid-stimulating hormone, free thyroxine, prolactin, and growth hormone, but not cortisol, in PD patients.11
Influences of aging and stress on the glucocorticoid system may result in reduction of hormone production capacity, impaired neuronal adaptive responses to environmental challenges, and increased vulnerability to stress-induced loss of hippocampal neurons.12 Aging is hypothesized to alter the function of the hypothalamic-pituitary-adrenal axis in both men and women. Increasing cortisol concentrations, especially nocturnal concentrations,13,14 have been described. Some studies have indicated that there are gender differences.13–16 One study showed significantly higher evening cortisol concentrations with increasing age, regardless of gender, while in the mornings this pattern was seen only in men. Diurnal cortisol variations were lower in older women but not in men.17
Studies of plasma cortisol in PD have shown variable results. Higher cortisol concentrations have been reported in untreated PD patients without dementia compared with healthy controls,18,19 and also compared with age-matched and gender-matched patients with Alzheimer’s disease. However, another study found decreased plasma cortisol concentrations in untreated PD patients compared with healthy controls, suggesting that this may be a consequence of hypothalamic/hypophyseal disturbance. Further, a previous study showed higher plasma cortisol concentrations in the evening and during the night in PD patients.18 One study reported higher concentrations of adrenocorticotrophic hormone in a subgroup of PD patients (both demented and nondemented) found to be dexamethasone nonsuppressors, suggesting higher concentrations of corticotrophin-releasing hormone.20 This surprisingly high incidence of dexamethasone non-suppression in patients with PD could indicate a possible central pathologic disturbance of neurotransmitter function. However, levodopa medication and dopamine alone exert no influence on corticotrophin-releasing hormone, and the effects of other PD medications (such as dopamine agonists) on cortisol concentrations have not been studied.
In one study, acute levodopa intake has been shown to induce lower plasma cortisol levels in patients on long-term treatment for PD who were depleted of antiparkinsonian medication for 12 hours.21 We believe that description of the diurnal salivary cortisol concentration curve in patients with chronic neurodegenerative diseases, such as PD, could be of great interest for future studies of pharmacological and nonpharmacological interventions, with the aim of reducing stress-related symptoms and lifelong suffering.
The primary aim of this study was to measure salivary cortisol concentrations in a well-defined group of PD patients, with and without chronic PD-related pain, with regard to age, duration of disease, body mass index (BMI), motor function (Unified Parkinson’s Disease Rating Scale [UPDRS] III, gait) and influence of concomitant pain. The secondary aim was to compare the salivary cortisol concentrations in these PD patients with those in a healthy reference group, matched by age, gender, and BMI.
Methods and materials
Patients
Patients with stable and well-defined PD22 for more than two years, who were aged 40–80 years, with chronic pain (PD-P) or without chronic pain (PD no-P), were recruited from the outpatient departments of three medium-sized city hospitals in southern Sweden. The study was approved by the ethics committees at the University of Gothenburg and the University of Linkoping.
A period of two years since receiving the diagnosis of PD was chosen to decrease the risk of recruiting patients with an incorrect diagnosis, given that a number of other disorders can mimic PD. The individual course of PD is variable, and in our study the range of disease duration was 2–27 years (median 5–6 years). Stable PD was defined as lack of severe fluctuations of the disease (on-off symptomatology) in terms of need for frequent extra doses of antiparkinsonian medication and absence of dementia. Exclusion criteria were severe fluctuations in PD, concurrent epilepsy, active malignancy, polyneuropathy, or other serious disease of somatic or psychiatric origin that could interfere with the study. Patients with severe abnormalities of blood parameters, electrolytes, liver or renal parameters, including bilirubin >20 mmol/L, serum creatinine >130 mmol/L, SR >30 mm, fasting plasma glucose >6.7 mmol/L, were excluded. Patients on corticosteroids (oral, nasal, or inhalation), insulin, antiepileptic drugs, or medication for dementia, and those participating in other therapeutic or pharmacological studies were also excluded.
Chronic pain was defined as the occurrence of PD-related pain on at least three days per week during the three months prior to recruitment. A reference population consisting of healthy individuals, matched by gender, age, and BMI, were recruited from another project,17 and consisted of 1700 healthy men and women aged 30–80 (mean 48) years. These individuals were recruited from the same catchment area as our patients, and their cortisol levels were analyzed using the same method and in the same laboratory. Demographic and clinical characteristics of the population with PD and the reference group are presented in Table 1.
Table 1.
Characteristics of the PD population and the healthy reference group
| Group | Sex | Number | Ageb | Weighta | BMIa | UPDRS IIIa,b |
|---|---|---|---|---|---|---|
| PD | Male | 24 | 50–78 | 84.1 | 26.8 | 20.1 (8–37) |
| Female | 35 | 60–79 | 68.4 | 25.5 | 22.0 (3–57) | |
| Referencea | Male | 303 | 50–74 | – | 26.9 | – |
| Female | 305 | 50–74 | – | 26.8 | – |
Note: Values are given as meana and rangeb.
Abbreviations: PD, Parkinson’s disease; UPDRS, Unified Parkinson’s Disease Rating Scale.
Methods
Motor function was assessed by the UPDRS.23 Duration and severity of pain was measured using a visual analog scale (VAS)24 for five consecutive days before sampling. Maximal pain during each of these five days was registered in our protocol.
Collection of salivary cortisol samples for both groups was done in the community using a technique which has been well described elsewhere.25–29 To summarize, patients were instructed to have no intake of food within 30 minutes of sampling. Samples were taken at four time points, ie, at 8 am, 1 pm, and 8 pm, and then at 8 am the next morning. Cotton-based neutral Salivette® tubes (Landskrona, Sweden) were used. A swab was chewed for two minutes and then placed in a sterile plastic tube. This was then put in the patient’s refrigerator at home. The tubes for each patient were collected and sent by post to the laboratory within three days. The Salivette tubes were then centrifuged at 1711 G for 15 minutes at 20°C, and then frozen at −80°C until assayed. A commercial radioimmunoassay-based technique for measurement of salivary cortisol was used (Spectria™ Cortisol I125, Landskrona, Sweden). Total cortisol secretion during the day (8 am–8 pm) and during the night (8 pm–8 am) was calculated using the formula for area under the curve from the zero level (AUC0–AUCG), and the increase in cortisol secretion from the baseline level during the same time interval (AUCi) was calculated according to the method reported by Pruessner et al30 and Fekedulegn et al.31 The latter author has shown significant associations (r > 0.7; P = 0.001) between AUCG and cortisol concentrations. All analyses of saliva from the same person were performed at the same time to minimize interassay variance.
Statistical analysis
STATISTICA version 8.0 (Statsoft Inc, Tulsa, OK) and SPSS version 18.0 (SPSS Inc, Chicago, IL) were used for the statistical evaluations. Nonparametric, Mann–Whitney U, and Wilcoxon paired signed-rank tests were used. The Spearman’s rank correlation test was also used. The Wilcoxon signed-rank test for one sample was used when comparing median salivary cortisol levels in PD patients with the median in the reference population.
Results
Fifty-nine patients, consisting 24 men and 35 women aged 50–79 years of age (median 66.5/67.5 years for men/women) were recruited for this study. The PD-P group comprised 43 patients (16 men and 27 women aged 50–77 years [median 63/66 years for men/women]), and the PD no-P group comprised eight men and eight women (median 70/75 years for men/women). Age at onset of PD was 40–74 years (median 60.0) and duration of PD was 2–27 years, with a median of 5.0/6.0 years for men/women, respectively. Most patients (96%) were over 55 years of age at the start of the study. No patient was younger than 64 years in the PD no-P group compared with 18 of 43 (42%) patients in the PD-P group.
Time of awakening in the PD-P and PD no-P groups did not differ significantly, and varied from 4.35 am to 8.00 am on the two days when sampling took place. Time points for sampling varied in relation to specified time points, ie, 8 am (±30 minutes), 1 pm (−60/+30 minutes) and 8 pm (−95/+75 minutes). Time intervals between awakening and sampling in the morning were 0–220 minutes and 5–187 minutes in the PD-P group and PD no-P group, respectively, and in 10 patients was less than 45 minutes. A cortisol arousal reaction with an increase in salivary cortisol of 2.5 nmol/L was noted in only one patient.
Maximal pain in the PD patients during the five days prior to inclusion were calculated on the VAS scale as the median (10/90 percentiles), with a value of 6.2 (2.8/9.1) and minimal pain of 3.0 (0.0/6.5). Motor function as estimated by UPDRS III scores was 3–57, corresponding to mild to severe PD (see Table 1).
Basal salivary cortisol
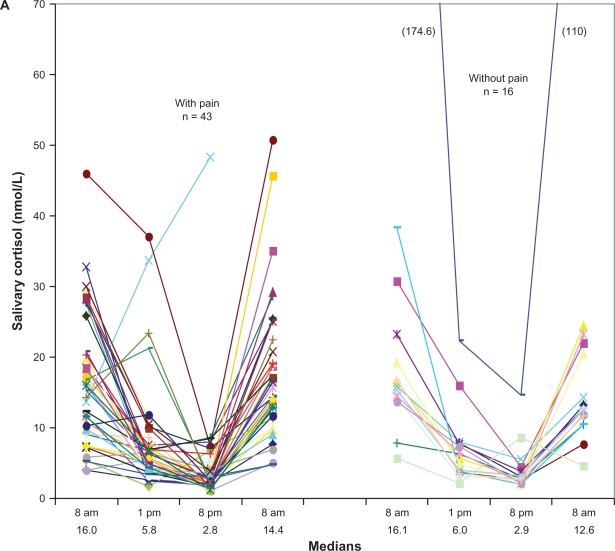
Salivary cortisol concentrations varied over a 24-hour period, as shown in Figures 1A and 1B. Individual salivary cortisol values in the PD-P and PD no-P patients are shown in Figure 1A. There were no statistically significant differences in salivary cortisol concentrations between the two groups. One patient in the PD no-P group had extremely high values (174.6, 22.3, 14.6, and 110 nmol/L).
Figure 1A.
Individual diurnal salivary cortisol concentrations (nmol/L) in Parkinson’s disease with and without chronic pain.
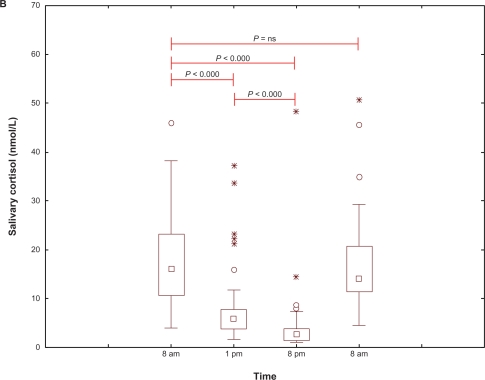
Figure 1B.
Diurnal salivary cortisol concentrations (nmol/L) in all 59 patients with Parkinson’s disease. Statistical analysis, between paired time points.
Notes: Correlations – Spearman two-tailed test: 8 am–8 am, r = 0.44: P < 0.01; 1 pm–8 am, r = 0.39: P < 0.01.
Abbreviation: ns, not significant.
Salivary cortisol concentrations at 8 am, 1 pm, 8 pm, and 8 am, along with delta values, are shown in Tables 2A and 2B. Morning cortisol concentrations were higher in the PD group compared with the reference group, and the concentration was not dependent on time interval between awakening and time point of salivary sampling. There was also no difference in cortisol concentration between participants taking their levodopa medication within one hour either side of salivary sampling. The linear equation for the cortisol trend curve calculated to estimate AUC was y = 23.56–1.02x versus y = 17.84–0.69x for the PD and reference groups, respectively.
Table 2A.
Comparisons of salivary cortisol concentrations (nmol/L) in PD patients with (PD-P) and without chronic PD-related pain (PD no-P) and the reference group
| Group | Sex (n) |
Day 1 |
Day 2 |
||||
|---|---|---|---|---|---|---|---|
|
8 am |
1 pm |
8 pm |
8 am |
||||
| Geom mean median with (10th and 90th perc) | P-valueb | Geom mean median with (10th and 90th perc) | Geom mean median with (10th and 90th perc) | P-valueb | Geom mean median with (10th and 90th perc) | ||
| PD-P | Male (16) | 12.5 | 5.6 | 2.3 | 15.1 | ||
| 14.8 (5.2–20.3) | 0.215 | 5.6 (3.2–11.8) | 2.6 (1.1–5.1) | 0.016d | 14.2 (5.1–35) | ||
| Female (27) | 15.6 | 6.4 | 3.4 | 15.1 | |||
| 17.9 (5.8–30) | 0.021d | 6.2 (2.6–21.2) | 2.9 (1.6–8.5) | 0.614 | 15.4 (7.6–28.6) | ||
| PD no-P | Male (8) | 20.5 | 6.4 | 4.2 | 16.9 | ||
| 15.4 (5.7–174.6) | 0.128 | 6.5 (2.1–22.3) | 3.1 (2.2–14.6) | 0.779 | 12.9 (4.6–110) | ||
| Female (8) | 17.5 | 5.3 | 2.8 | 13.0 | |||
| 16.8 (7.8–38.2) | 0.091 | 5.6 (3.5–8.0) | 2.6 (2–5.5) | 0.035d | 12.1 (7.6–23.2) | ||
| Reference | Male (303) | 12.1a | – | – | 3.9c | – | – |
| Female (305) | 12.5a | – | – | 4.1c | – | – | |
Notes:
Values are given as geometric mean;
testing median of the corresponding reference population;
values were estimated according to equations of lines between 8 am and 10 pm;
statistically significant at 5% level.
Abbreviations: Geom, geometric; perc, percentiles; PD, Parkinson’s disease; PD no-P, PD without pain; PD-P, PD with pain.
Table 2B.
Differences in salivary cortisol concentrations between paired time points, delta cortisol (nmol/L)
| Group | Sex (n) |
Day 1 |
Day 2 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 8 am | 1 pm | 8 pm | 8 am | Delta 8 am–1 pm | Delta 1 pm–8 pm | Delta 8 am–8 pm | |||||
| Geom mean median with (10th and 90th perc) | P-valueb | Geom mean median with (10th and 90th perc) | Geom mean median with (10th and 90th perc) | P-valueb | Geom mean median with (10th and 90th perc) | Geom mean median | Geom mean median | Geom mean median | P-valueb | ||
| PD-P | Male (16) | 12.5 | 5.6 | 2.3 | 15.1 | 6.9 | 3.3 | 10.2 | |||
| 14.8 (5.2–20.3) | 0.215 | 5.6 (3.2–11.8) | 2.6 (1.1–5.1) | 0.016c | 14.2 (5.1–35) | 9.2 | 3.0 | 12.2 | 0.049c | ||
| Female (27) | 15.6 | 6.4 | 3.4 | 15.1 | 9.2 | 3.0 | 12.2 | ||||
| 17.9 (5.8–30) | 0.021c | 6.2 (2.6–21.2) | 2.9 (1.6–8.5) | 0.614 | 15.4 (7.6–28.6) | 11.7 | 3.3 | 15.0 | 0.052 | ||
| PD no-P | Male (8) | 20.5 | 6.4 | 4.2 | 16.9 | 14.1 | 2.2 | 16.3 | |||
| 15.4 (5.7–174.6) | 0.128 | 6.5 (2.1–22.3) | 3.1 (2.2–14.6) | 0.779 | 12.9 (4.6–110) | 8.9 | 3.4 | 12.3 | 0.128 | ||
| Female (8) | 17.5 | 5.3 | 2.8 | 13.0 | 12.2 | 2.5 | 14.7 | ||||
| 16.8 (7.8–38.2) | 0.091 | 5.6 (3.5–8.0) | 2.6 (2–5.5) | 0.035c | 12.1 (7.6–23.2) | 11.2 | 3 | 14.2 | 0.043c | ||
| Reference | Male (303) | 12.1a | – | – | 3.9b | – | – | – | – | 8.2a | – |
| Female (305) | 12.5a | – | – | 4.1b | – | – | – | – | 8.4a | – | |
Notes:
Values are given as geometric mean;
testing median of the corresponding reference population;
statiscally singinificant at 5% level.
Abbreviations: Geom, geometric; perc, percentiles; PD, Parkinson’s disease; PD no-P, PD without pain; PD-P, PD with pain.
Total cortisol secretion and secretion rate
Total cortisol secretion during the day (8 am–8 pm, AUC0–AUCG) was significantly increased in PD patients, at 112.8 nmolh versus 81.1 nmolh in the reference group (P < 0.001). The corresponding value for 8 pm–8 am in PD patients was 109.8 nmolh. The decrease in the salivary cortisol secretion rate during the day (8 am–8 pm, negative AUCi) in the PD and reference groups was −73.7 nmolh versus −49.9 nmolh. This difference was statistically significant (P = 0.001). The increase in salivary cortisol secretion rate during the night (8 pm–8 am, AUCi) was 72.6 nmolh, and similar to the day time value.
Somatic status and symptom correlations with cortisol
There was a highly significant correlation (r = 0.44; P < 0.01) between values at 8 am on day 1 and 8 am on day 2. There were also significant correlations between cortisol concentrations at 1 pm and for all other time points (r values 0.28–0.42; P 0.001–0.034). No significant correlations between BMI, motor dysfunction, measured as UPDRS III ≤ 20 compared with >20, gait (UPDRS III, item 30), acute pain (maximum VAS at screening), chronic pain, and cortisol concentrations were identified.
Discussion
In this study, we compared salivary cortisol concentrations in a group of patients with a diagnosis of PD for more than two years with those in a reference group of gender-, BMI-, and age-matched healthy individuals.17 There were two groups of PD patients, ie, those with and those without PD-related pain.
The cortisol concentrations in this study were unrelated to age. This is in disagreement with the hypothesis that aging alters the function of the hypothalamic-pituitary-adrenal axis in both men and women. Increasing cortisol concentrations, especially at night, have been described previously.13,16 Even in our reference group, significantly higher evening cortisol concentrations were found with increasing age, regardless of gender, while in the mornings this pattern was seen only in men.17
We found no gender differences in cortisol rhythm and/or amplitude in our PD patients. This is in contrast with findings in our reference group, where differences were found for cortisol concentrations in the morning, and the diurnal variations in cortisol were lower in older women but not in men. Other studies have also indicated gender differences.13–16
For estimation of total secretion and the secretion rate of cortisol, we analyzed AUC0–AUCG for cortisol during the daytime (8 am–8 pm) according to the recommendations of Fekedulegn et al.31 The results were significantly higher in the PD group than in the reference group. The corresponding value for nocturnal AUCG (8 pm–8 am) was similar. The decreasing secretion rate (negative AUCi) was significantly higher in the PD group. Our results showing a significant increase in secretion rate and total cortisol secretion are potential evidence for a well functioning adrenal and hypothalamic-pituitary-adrenal axis, as reported by Fekedulegn et al.31
The excellent correlation between salivary cortisol levels and plasma total and free biologically active cortisol levels in healthy men and women was reported as early as 1983 by Vining et al,32 and this was confirmed in a subsequent study.33 This method has been the “gold standard” for estimating stress in psycho-biologic-endocrine research for a number of years.34 A recent report by Törnhage described the usefulness of salivary cortisol for assessing the hypothalamic-pituitary-adrenal axis.27 These observations make it appropriate and convenient to use salivary cortisol sampling at home as a pain-free, simple, repeatable, and useful method for assessment of the hypothalamic-pituitary-adrenal axis.
Cortisol as a reflector of chronic stress in chronic disease has not undergone adequate investigation, although some studies have been performed. PD has several potentially stressful nonmotor symptoms, such as pain, mood change, and autonomic dysfunction, all of which could result in changes in cortisol secretion.
The time point for sampling in the evening differed between the PD and reference groups. Sampling occurred about two hours later in the reference group. We believe that the consequences of this are trivial, because we know that the negative slope is minimal between 8 pm and 10 pm.35 We also estimated the linear equation for salivary cortisol in both groups. When we adjusted for the time difference, the salivary cortisol concentration at 8 pm in the reference group was 4.0 nmol/L compared with 3.2 nmol/L in the PD group, and this difference was not statistically significant.
The fact that the time point for awakening corresponds to sleep duration is important. A previous study found a positive correlation between sleep duration and cortisol concentration.35 The time interval from awakening in the morning to the exact time point of sampling is also important because of the cortisol arousal reaction. In our study, we registered the exact time for sampling in all patients in order to control for both the cortisol arousal reaction and food intake. For most patients in our study, the exact time points for sampling were in accordance with those stipulated and stated for the reference group (±30 minutes). In 11 patients, the time interval was less than 60 minutes. In seven of these 11 patients, the interval was 30–45 minutes, with a high risk for an arousal effect. There was a cortisol arousal reaction in only one of 59 participants.
We found that patients in both PD groups generally showed a similar 24-hour rhythm of cortisol secretion. However, morning cortisol concentrations were higher in the PD group compared with those in the reference group. This is in disagreement with the findings of Hartmann et al, who reported normal morning plasma cortisol but increased concentrations in the evening and at night.18
Our hypothesis that chronic neurodegenerative disease, using PD as an example, could change hypothalamic-pituitary-adrenal axis function was not confirmed. However, we found no correlation between duration of disease and cortisol concentrations. Some patients in our study showed very high morning salivary cortisol concentrations on both days. Function of the hypothalamic-pituitary-adrenal axis seems to be optimal, even at this age and after many years of disease. This, in turn, could indicate a normal-functioning hypothalamic-pituitary-adrenal axis in individuals with PD, thereby not supporting the hypothesis of earlier studies by Rabey et al20 and Bellomo et al36 concerning pathophysiological changes at the hypothalamic-hypophyseal-adrenal level.
There were marked differences in motor function of the patients according to UPDRS III scores. We predicted that motor dysfunction would be a severe stress factor resulting in increased cortisol concentration, but this was not confirmed. We found no correlation between gait problems, defined by UPDRS III item 30, and salivary cortisol concentration. This is in disagreement with Charlett et al who found a positive correlation between gait problems and plasma cortisol concentrations.19 The reason for this difference is not obvious.
In this study, there was no correlation between BMI and cortisol concentrations in either the PD group or the reference group. In contrast, a study by Travison et al found a negative correlation between BMI and morning cortisol.37
The hypothalamic-pituitary-adrenal axis seems to be preserved in patients with PD. Effects of acute or chronic pain were not seen in our study, in contrast with the findings by Heim et al.38 The “glucocorticoid cascade hypothesis,” as described by McEwen,12 ie, an acquired or primary decrease in hippocampal glucocorticoid receptor numbers leads to a reduction in central feedback sensitivity that results in basal glucocorticoid hypersecretion, is partially confirmed in our study. Possibly, the night-time lack of antiparkinsonian dopaminergic substitution contributes to the elevated cortisol concentration in the morning. The limitation of our study is the relatively small numbers of PD patients (n = 59), although this number compares well with those used in earlier studies in this field.19,20
Conclusion
PD patients with mild to severe PD have a normal diurnal cortisol rhythm, and higher morning cortisol concentrations and increased cortisol secretions during the day (8 am–8 pm) compared with healthy age-matched and gender-matched individuals. PD patients seem to have a normal cortisol arousal reaction and hypothalamic-pituitary-adrenal axis function, and their cortisol concentration is unrelated to age, duration of disease, gender, severity of motor dysfunction, and BMI, supporting the hypothesis that this neurodegenerative disorder itself does not interfere with hypothalamic-pituitary-adrenal axis function.
Acknowledgments
Financial support for this study was provided by the Research Fund at Skaraborg Hospital, the Research and Development Council of County Skaraborg, the Palle Ferb Foundation, the Academy for Healthcare, Jonkoping County Hospital, the Medical Research Council of Southeast Sweden, the Else Torgard Memorial Foundation, and the Skaraborg Institute of Research and Development. We thank Professor Bo Eriksson and Salmir Nasic for statistical support, and Astrid Borg for excellent secretarial and financial assistance and, last but not least, the study participants.
Footnotes
Disclosure
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported in this paper.
References
- 1.Bruguerolle B, Simon N. Biologic rhythms and Parkinson’s disease: A chronopharmacologic approach to considering fluctuations in function. Clin Neuropharmacol. 2002;25(4):194–201. doi: 10.1097/00002826-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Borg A, Törnhage C-J. “Parkitouch”-studien, Parkinsons sjukdom och effekten av beröringsmassage. [the study of “Parkitouch”, Parkinson’s disease and the effects of tactile touch] Parkinson Journalen. 2009;1:22–24. [Google Scholar]
- 3.Beiske AG, Loge JH, Ronningen A, Svensson E. Pain in Parkinson’s disease: Prevalence and characteristics. Pain. 2009;141(1–2):173–177. doi: 10.1016/j.pain.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 4.Negre-Pages L, Regragui W, Rascol O, DoPaMi PSG. Chronic pain in Parkinson’s disease: The cross-sectional French DoPaMiP survey. Mov Disord. 2008;23(10):1361–1369. doi: 10.1002/mds.22142. [DOI] [PubMed] [Google Scholar]
- 5.Ford B. Pain in Parkinson’s disease. Clin Neurosci. 1998;5(2):63–72. [PubMed] [Google Scholar]
- 6.Buzas B, Max MB. Pain in Parkinson disease. Neurology. 2004;62(12):2156–2157. doi: 10.1212/01.wnl.0000130384.56476.75. [DOI] [PubMed] [Google Scholar]
- 7.Borgman. Parkinsonenkät-98. Parkinsonjournalen. 2002 [Google Scholar]
- 8.Schestatsky P, Kumru H, Valls-Sole J, et al. Neurophysiologic study of central pain in patients with Parkinson disease. Neurology. 2007;69(23):2162–2169. doi: 10.1212/01.wnl.0000295669.12443.d3. [DOI] [PubMed] [Google Scholar]
- 9.Simuni T, Sethi K. Nonmotor manifestations of Parkinson’s disease. Ann Neurol. 2008;64(Suppl 2):S65–S80. doi: 10.1002/ana.21472. [DOI] [PubMed] [Google Scholar]
- 10.Munhoz RP, Teive HA, Troiano AR, et al. Parkinson’s disease and thyroid dysfunction. Parkinsonism Relat Disord. 2004;10(6):381–383. doi: 10.1016/j.parkreldis.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 11.Aziz NA, Pijl H, Frolich M, Roelfsema F, Roos RA. Diurnal secretion profiles of growth hormone, thyrotropin and prolactin in Parkinson’s disease. J Neuroendocrinol. 2011;23(6):519–524. doi: 10.1111/j.1365-2826.2011.02134.x. [DOI] [PubMed] [Google Scholar]
- 12.McEwen BS. Re-examination of the glucocorticoid hypothesis of stress and aging. Prog Brain Res. 1992;93:365–381. doi: 10.1016/s0079-6123(08)64585-9. [DOI] [PubMed] [Google Scholar]
- 13.Van Cauter E, Leproult R, Kupfer DJ. Effects of gender and age on the levels and circadian rhythmicity of plasma cortisol. J Clin Endocrinol Metab. 1996;81(7):2468–2473. doi: 10.1210/jcem.81.7.8675562. [DOI] [PubMed] [Google Scholar]
- 14.Seeman TE, Singer B, McEwen B. Gender differences in age-related changes in HPA axis reactivity. Psychoneuroendocrinology. 2001;26(3):225–240. doi: 10.1016/s0306-4530(00)00043-3. [DOI] [PubMed] [Google Scholar]
- 15.Laughlin GA, Barrett-Connor E. Sexual dimorphism in the influence of advanced aging on adrenal hormone levels: The Rancho Bernardo Study. J Clin Endocrinol Metab. 2000;85(10):3561–3568. doi: 10.1210/jcem.85.10.6861. [DOI] [PubMed] [Google Scholar]
- 16.Kudielka BM, Buske-Kirschbaum A, Kirschbaum C, et al. HPA axis responses to laboratory psychosocial stress in healthy elderly adults, younger adults, and children: Impact of age and gender. Psychoneuroendocrinology. 2004;29(1):83–98. doi: 10.1016/s0306-4530(02)00146-4. [DOI] [PubMed] [Google Scholar]
- 17.Larsson CA, Gullberg B, Rastam L, Lindblad U. Salivary cortisol differs with age and sex and shows inverse associations with WHR in Swedish women: A cross-sectional study. BMC Endocr Disord. 2009;9:16. doi: 10.1186/1472-6823-9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hartmann A, Veldhuis JD, Deuschle M, Standhardt H, Heuser I. Twenty-four hour cortisol release profiles in patients with Alzheimer’s and Parkinson’s disease compared to normal controls: Ultradian secretory pulsatility and diurnal variation. Neurobiol Aging. 1997;18(3):285–289. doi: 10.1016/s0197-4580(97)80309-0. [DOI] [PubMed] [Google Scholar]
- 19.Charlett A, Dobbs RJ, Purkiss AG, et al. Cortisol is higher in parkinsonism and associated with gait deficit. Acta Neurol Scand. 1998;97(2):77–85. doi: 10.1111/j.1600-0404.1998.tb00614.x. [DOI] [PubMed] [Google Scholar]
- 20.Rabey JM, Scharf M, Oberman Z, Zohar M, Graff E. Cortisol, ACTH, and beta-endorphin after dexamethasone administration in Parkinson’s dementia. Biol Psychiatry. 1990;27(6):581–591. doi: 10.1016/0006-3223(90)90525-7. [DOI] [PubMed] [Google Scholar]
- 21.Muller T, Welnic J, Muhlack S. Acute levodopa administration reduces cortisol release in patients with Parkinson’s disease. J Neural Transm. 2007;114(3):347–350. doi: 10.1007/s00702-006-0552-0. [DOI] [PubMed] [Google Scholar]
- 22.Calne DB, Snow BJ, Lee C. Criteria for diagnosing Parkinson’s disease. Ann Neurol. 1992;32(Suppl):S125–S127. doi: 10.1002/ana.410320721. [DOI] [PubMed] [Google Scholar]
- 23.Ramaker C, Marinus J, Stiggelbout AM, Van Hilten BJ. Systematic evaluation of rating scales for impairment and disability in Parkinson’s disease. Mov Disord. 2002;17(5):867–876. doi: 10.1002/mds.10248. [DOI] [PubMed] [Google Scholar]
- 24.Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976;2(2):175–184. [PubMed] [Google Scholar]
- 25.Jones MT, Gillham B, Campbell EA, Al-Taher AR, Chuang TT, Di Sciullo A. Pharmacology of neural pathways affecting CRH secretion. Ann N Y Acad Sci. 1987;512:162–175. doi: 10.1111/j.1749-6632.1987.tb24958.x. [DOI] [PubMed] [Google Scholar]
- 26.Tornhage CJ, Alfven G. Diurnal salivary cortisol concentration in school-aged children: Increased morning cortisol concentration and total cortisol concentration negatively correlated to body mass index in children with recurrent abdominal pain of psychosomatic origin. J Pediatr Endocrinol Metab. 2006;19(6):843–854. doi: 10.1515/jpem.2006.19.6.843. [DOI] [PubMed] [Google Scholar]
- 27.Tornhage CJ. Salivary cortisol for assessment of hypothalamic-pituitary-adrenal axis function. Neuroimmunomodulation. 2009;16(5):284–289. doi: 10.1159/000216186. [DOI] [PubMed] [Google Scholar]
- 28.Clements AD, Parker CR. The relationship between salivary cortisol concentrations in frozen versus mailed samples. Psychoneuroendocrinology. 1998;23(6):613–616. doi: 10.1016/s0306-4530(98)00031-6. [DOI] [PubMed] [Google Scholar]
- 29.Tornhage CJ. Reference values for morning salivary cortisol concentrations in healthy school-aged children. J Pediatr Endocrinol Metab. 2002;15(2):197–204. doi: 10.1515/jpem.2002.15.2.197. [DOI] [PubMed] [Google Scholar]
- 30.Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28(7):916–931. doi: 10.1016/s0306-4530(02)00108-7. [DOI] [PubMed] [Google Scholar]
- 31.Fekedulegn DB, Andrew ME, Burchfiel CM, et al. Area under the curve and other summary indicators of repeated waking cortisol measurements. Psychosom Med. 2007;69(7):651–659. doi: 10.1097/PSY.0b013e31814c405c. [DOI] [PubMed] [Google Scholar]
- 32.Vining RF, McGinley RA, Maksvytis JJ, Ho KY. Salivary cortisol: A better measure of adrenal cortical function than serum cortisol. Ann Clin Biochem. 1983;20(Pt 6):329–335. doi: 10.1177/000456328302000601. [DOI] [PubMed] [Google Scholar]
- 33.Aardal E, Holm AC. Cortisol in saliva – reference ranges and relation to cortisol in serum. Eur J Clin Chem Clin Biochem. 1995;33(12):927–932. doi: 10.1515/cclm.1995.33.12.927. [DOI] [PubMed] [Google Scholar]
- 34.Weibel L. Methodological guidelines for the use of salivary cortisol as biological marker of stress. Presse Med. 2003;32(18):845–851. French. [PubMed] [Google Scholar]
- 35.Leproult R, Van Cauter E. Role of sleep and sleep loss in hormonal release and metabolism. Endocr Dev. 2010;17:11–21. doi: 10.1159/000262524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bellomo G, Santambrogio L, Fiacconi M, Scarponi AM, Ciuffetti G. Plasma profiles of adrenocorticotropic hormone, cortisol, growth hormone and prolactin in patients with untreated Parkinson’s disease. J Neurol. 1991;238(1):19–22. doi: 10.1007/BF00319704. [DOI] [PubMed] [Google Scholar]
- 37.Travison TG, O’Donnell AB, Araujo AB, Matsumoto AM, McKinlay JB. Cortisol levels and measures of body composition in middle-aged and older men. Clin Endocrinol (Oxf) 2007;67(1):71–77. doi: 10.1111/j.1365-2265.2007.02837.x. [DOI] [PubMed] [Google Scholar]
- 38.Heim C, Ehlert U, Hellhammer DH. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology. 2000;25(1):1–35. doi: 10.1016/s0306-4530(99)00035-9. [DOI] [PubMed] [Google Scholar]