Abstract
Cancer of the cervix is the commonest genital tract malignancy in the female, and it has been ranked second to breast cancer. It has positive association with infection of human papillomavirus. Cervical cancer incidence and mortality have declined substantially in western countries following the introduction of screening programmes. This present study investigated the knowledge, attitude and practice of nurses in Lagos University Teaching Hospital (LUTH) towards cervical cancer screening as they are important health personnel that are suppose to educate women on the need for cervical cancer screening. The study is a descriptive cross-sectional survey of the knowledge, attitude and practice of 200 nurses in LUTH towards cervical cancer screening. The results obtained showed that 99% of the respondents were aware of cervical cancer and that 92% of the respondents were also aware of the causative organism of cervical cancer (human papillomavirus). Their major sources of information were through electronic media (43.9%) and health professionals (37.4%). Furthermore, the respondents were quiet aware of Pap smear (91%) as one of the screening techniques of cervical cancer and had good attitudes (89%) towards Pap smear, but most of them had never done it before. The study further revealed that majority of the respondents did not know colposcopy as one of the screening techniques for cervical cancer. Finally, it has been made known from this study that nurses have good knowledge of cervical cancer but have limited understanding of the types of cervical cancer screening techniques and poor disposition towards undergoing cervical cancer screening. It may thus be recommended that institutions should periodically organise seminars and training for health personnel especially the nurses which form a group of professionals that should give health education to women about cervical cancer. This training may be done as part of the orientation programme to newly employed staff.
Keywords: Cervical cancer, Pap smear, Nurses, Screening techniques
Introduction
Cancer is responsible for about 51 million deaths yearly, out of which cervical cancer accounts for 8.5%, most of which occurred in the developing countries. About half a million new cases are seen worldwide each year, most occurring in developing countries [1]. Cancer of the cervix is the commonest genital tract malignancy in the female [2]. It has been ranked second to breast cancer in the reports of [3, 4]. Cervical cancer has positive association with infection of human papillomavirus (HPV), and repeated or persistent HPV infections appear to raise the chances of developing the disease [5].
The work of Muñoz et al. [6] has shown that tobacco smoking, high parity, long-term hormonal contraceptive use, co-infection with Chlamydia trachomatis, herpes simplex virus type 2, HIV, immunosuppression, certain dietary deficiencies, and genetic and immunological host factors are contributing factors to cervical cancers.
The availability of effective prophylactic HPV vaccines gives new promise for a primary prevention strategy for HPV infection and cervical cancer [7]. However, the current vaccines only protect against 70% of the disease, and are only effective for those not yet exposed to the virus.
Cervical cancer incidence and mortality have declined substantially in western countries following the introduction of screening programmes. Screening programmes in Africa are however often rudimentary or nonexistent. The screening techniques often used are Pap smear test [8], visual inspection of the acetic acid-painted cervix (VIA) [9], cryotherapy for moderate cervical dysplasia [9] and HPV DNA test [10].
The earlier reports of [11–13] have respectively shown that less than 10% of the women in Maiduguri are aware of cervical cancer and its symptoms, inadequate knowledge of aetiology and prevention of cervical cancer among nurses in Ibadan, and 52.8% awareness of cervical cancer screening methods among women in Owerri.
Lack of knowledge of cancer screening exercise may be a reflection of general poor health education in the country. Therefore, comprehensive health education programmes are more likely to be beneficial than disease-specific programmes in tackling this problem.
The present study intends to investigate the knowledge, attitude and practice of nurses in Lagos University Teaching Hospital towards cervical cancer screening as they are important health personnel that are suppose to educate women on the need for cervical cancer screening.
Methodology
Description of the Study Area
Lagos University Teaching Hospital is one of the largest teaching hospitals in Nigeria. It is located in Lagos State which is a state in southwestern Nigeria. Lagos is one of Nigeria's most populated states. It is the chief port, principal economic and cultural centre. The teaching hospital has 761 bed spaces and records over 9,000 (≈10,000) patient attendances in a month. There are about 641 nurses working in Lagos University Teaching Hospital (LUTH) in all departments.
Study Population
The study population includes all the 641 nurses working in Lagos University Teaching Hospital, Lagos.
Study Design
This study is a descriptive cross-sectional survey of cervical cancer screening amongst 200 nurses in Lagos University Teaching Hospital, Lagos, Nigeria.
Sample Size Determination
A sample size of approximately 200 was calculated using Fischer formula. The sample size was increased to 250 in order to give allowance for nonresponse. However, 200 questionnaires were retrieved after the study.
Sampling Method
A systematic random sampling technique was employed to select one out of every three nurses in the different wards, theatres and clinics.
Data Collection
Data were collected using a standard closed-ended structured questionnaire adopted from WHO with three sections on sociodemography, knowledge on cervical cancer and attitude towards cervical cancer screening. The subjects were mainly not required to write but just to tick the appropriate boxes which were provided for each option given. Names were not used for identification, but coding numbers were used instead.
Data Analysis
The 200 questionnaires obtained from the study were analysed using the EPI-INFO 2002 software programme. The data were presented in frequency distribution tables with percentages, and chi-square analysis was used to test the significance at p < 0.05.
Results
The results obtained showed nurses in LUTH to have highest (38.5%) age range between 20 and 29 years and lowest age (6%) greater or equal to 50 years. Of the respondents, 55.0% (110) were married, while 79 (39.5%) were single. The tribe with highest distribution was Yoruba (69.0%) and Igbo (25.0%), and 3.5% of the nurses were of Hausa tribe. Christianity (85%) was the major religion of the respondents (Table 1).
Table 1.
Sociodemographic variable
| Variable | Frequency (n = 200) | Percent |
|---|---|---|
| Age (year) | ||
| 20–29 | 77 | 38.5 |
| 30–39 | 72 | 36.0 |
| 40–49 | 39 | 19.5 |
| ≥50 | 12 | 6.0 |
| Total | 200 | 100 |
| Marital status | ||
| Single | 79 | 39.5 |
| Married | 110 | 55.0 |
| Divorced/separated | 6 | 3.0 |
| Widowed | 5 | 2.5 |
| Total | 200 | 100 |
| Ethnicity | ||
| Hausa | 7 | 3.5 |
| Igbo | 50 | 25.0 |
| Yoruba | 138 | 69.0 |
| Others | 5 | 2.5 |
| Total | 200 | 100 |
| Religion | ||
| Christianity | 170 | 85.0 |
| Islam | 30 | 15.0 |
| Total | 200 | 100 |
| Age at first intercourse (year) | ||
| <20 | 20 | 10.0 |
| 20–24 | 66 | 33.0 |
| 25–29 | 88 | 44.0 |
| ≥30 | 26 | 13.0 |
| Total | 200 | 100 |
| Mean age at first intercourse | 24.8 ± 4.8 | |
Table 2 revealed the sources of information about cervical cancer. The results showed that the highest proportion of the respondents got the information about cervical cancer from electronic media (43.9%). The other sources are health professionals (37.4%), school seminars (31.3%) and journals (25.8%), and the lowest proportion of the respondents got their information from church/mosque (7.6%).
Table 2.
Sources of information about cervical cancer
| Source of information | Frequency (n = 198) | Percent |
|---|---|---|
| Electronic media | 87 | 43.9 |
| Print media | 33 | 16.7 |
| Health professionals | 74 | 37.4 |
| School seminars | 62 | 31.3 |
| Friends and relatives | 33 | 16.7 |
| Church/mosque | 15 | 7.6 |
| Bills/posters | 32 | 16.2 |
| Journals | 51 | 25.8 |
Multiple responses are given
The results in Fig. 1 showed that 99% of the respondents were aware of cervical cancer, while 92% of the respondents were aware of the causative organism of cervical cancer (human papillomavirus). Figure 2 further showed that 182 (91%) of the respondents were aware of Pap smear; however, 159 (79.5%) and 175 (87.5%) of the respondents have never done Pap smear and visual inspection with acetic acid, respectively.
Fig. 1.
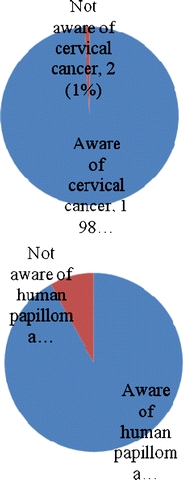
Awareness of cervical cancer and human papillomavirus among nurses (n = 200)
Fig. 2.
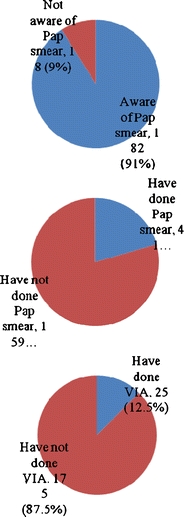
Awareness of Pap smear and uptake of Pap smear and VIA among nurses (n = 200)
Table 3 showed the respondents' comprehensive knowledge of cervical cancer. Of the respondents, 54% associated cervical cancer with having multiple sexual partners, and 47.5% linked cervical cancer with having sex at early age, while 52% of the respondents understood human papillomavirus to be a causative agent in cervical cancer. However, 18.5% and 19.5% of the respondents felt that excess alcohol and smoking could cause cervical cancer, respectively. Almost all the respondents (85.5%) were aware of the preventability and detectability (95%) of cervical cancer. The results further showed a good understanding of the signs of cervical cancer and the various screening techniques.
Table 3.
Knowledge of cervical cancer
| Frequency (n = 200) | Percent | |
|---|---|---|
| Causes of cervical cancera | ||
| Excess alcohol | 37 | 18.5 |
| Having sexual partner | 108 | 54.0 |
| Witchcraft | 8 | 4.0 |
| Having sex at early age | 95 | 47.5 |
| Use of oral contraceptive | 49 | 24.5 |
| Smoking | 39 | 19.5 |
| Human papillomavirus infection | 104 | 52.0 |
| Family history of cervical cancer | 40 | 20.0 |
| Signs of cervical cancer | ||
| Dysmenorrhoea | 25 | 12.5 |
| Menorrhagia during teenage years (DTY) | 18 | 9.0 |
| Postcoital bleeding | 32 | 16.0 |
| Postmenopausal bleeding (PMB) | 38 | 19.0 |
| Foul-smelling discharge from the vaginal (FSDPV) | 55 | 27.5 |
| Dysmenorrhoea and FSDPV | 3 | 1.5 |
| Postcoital bleeding and FSDPV | 5 | 2.5 |
| Dysmenorrhoea, postcoital bleeding and FSDPV | 5 | 2.5 |
| Menorrhagia DTY, postcoital bleeding, PMB and FSDPV | 8 | 4.0 |
| Do not know | 11 | 5.5 |
| Total | 200 | 100 |
| Screening techniques for cervical cancer | ||
| Pap smear | 103 | 51.5 |
| Testing for HPV | 21 | 10.5 |
| Visual inspection with acetic acid (VIA) | 20 | 10.0 |
| Colposcopy | 7 | 3.5 |
| Pap smear and testing for HPV | 12 | 6.0 |
| Pap smear and VIA | 11 | 5.5 |
| Pap smear, testing for HPV and VIA | 26 | 13.0 |
| Total | 200 | 100 |
| Prevention of cervical cancera | ||
| It is preventable | 171 | 85.5 |
| It is possible to detect it | 190 | 95.0 |
| Early detection can increase chance of survival | 163 | 81.5 |
aMultiple responses are given
The findings in Table 4 showed the knowledge of the uses of Pap smear and the meaning of positive Pap smear results. Of the respondents, 60% (120) understood that Pap smear could be used to detect precancerous state of cervical cancer, while 18.5% (37) respondents felt Pap smear could be used to prevent cervical cancer. Moreover, 59% (118) of the respondents knew that the positive results of Pap smear meant that cervical cancer is about to start, while 34.5% (69) of the respondents felt that the positive results of cervical cancer meant full-blown cervical cancer. The results further showed that 54% (108) of the respondents knew that Pap smear should be done once in a year, while 11.5% (23), 2.5% (5) and 13.5% (27) felt that it should be done once in 2 years, 3 years and lifetime, respectively. Of the respondents, 18.5% (37) did not know the uses of Pap smear. A poor response of 68 (34%) of the respondents felt that women above 65 years of age should have Pap smear done.
Table 4.
Knowledge of uses of Pap smear and meaning of positive Pap smear result
| Frequency (n = 200) | Percent | |
|---|---|---|
| Use of Pap smear | ||
| Detection of sexually transmitted diseases | 10 | 5.0 |
| Detection of human papillomavirus infection | 2 | 1.0 |
| Detection of precancerous state of cervical cancer | 120 | 60.0 |
| Cure of cervical cancer | 12 | 6.0 |
| Prevention of cervical cancer | 37 | 18.5 |
| Do not know | 19 | 9.5 |
| Total | 200 | 100 |
| Meaning of positive Pap smear result | ||
| Full-blown cancer of cervix | 69 | 34.5 |
| Cervical cancer that is about to start | 118 | 59.0 |
| Cancer of the breast | 5 | 2.5 |
| I do not know | 8 | 4.0 |
| Total | 200 | 100 |
| How often should Pap smear be done | ||
| At least once in a year | 108 | 54.0 |
| At least once in 2 years | 23 | 11.5 |
| At least once in 3 years | 5 | 2.5 |
| At least once in a lifetime | 27 | 13.5 |
| Do not know | 37 | 18.5 |
| Total | 200 | 100 |
| Who should have Pap smear done | ||
| Women of all age | 52 | 26.0 |
| Women that are still giving birth | 29 | 14.5 |
| Women that are 18 years and above | 44 | 22.0 |
| Women above 65 years of age | 68 | 34.0 |
| Do not know | 7 | 3.5 |
| Total | 200 | 100 |
Figure 3 results showed good attitude of nurses towards Pap smear. Of the respondents, 89% thought that it is advisable to have Pap smear done, and 34% of the respondents have recommended Pap smear to others. The results in Table 5 showed that 17% (27) of the respondents did not do Pap smear because it is costly, and 11.9% (19) claimed not to have money. The respondents did not recommend Pap smear for people because it is painful (14.4%) and risky (5.3%).
Fig. 3.
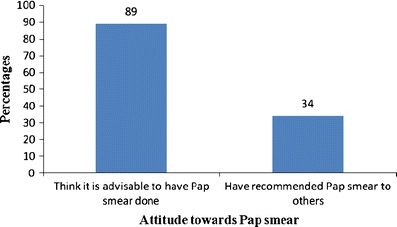
Attitude of nurses towards Pap smear (n = 200)
Table 5.
Reasons for not doing Pap smear and for not recommending it to others
| Variable | Frequency | Percent |
|---|---|---|
| Reasons for not doing Pap smear (n = 159) | ||
| No time | 15 | 9.4 |
| No money | 19 | 11.9 |
| Not thought about it | 38 | 23.9 |
| Still young for it | 13 | 8.2 |
| It is costly | 27 | 17.0 |
| Not aware of any test | 2 | 1.3 |
| Do not know where the test is done | 9 | 5.7 |
| Others | 8 | 5.0 |
| No reason | 28 | 17.6 |
| Total | 159 | 100 |
| Reasons for not recommending Pap smear to others (n = 132) | ||
| Females below 20 years are safe from cervical cancer | 13 | 9.8 |
| Pap smear is painful | 19 | 14.4 |
| Pap smear test could be dangerous and risky | 7 | 5.3 |
| Others | 32 | 24.2 |
| No reason | 61 | 46.2 |
| Total | 132 | 100 |
The results in Tables 6 and 7 showed a significant (p ≤ 0.05) association between age, marital status, and awareness of Pap smear and uptake of Pap smear, respectively.
Table 6.
Associations between sociodemographic variables and awareness of Pap smear
| Variable | Aware of Pap smear (%) | χ 2 | df | p | ||
|---|---|---|---|---|---|---|
| Yes | No | Total | ||||
| Age (year) | ||||||
| 20–29 | 60 (77.9) | 17 (22.1) | 77 | 26.22 | 3 | 0.00 |
| 30–39 | 71 (98.6) | 1 (1.4) | 72 | |||
| 40–49 | 39 (100) | 0 (0) | 39 | |||
| ≥50 | 12 (100) | 0 (0) | 12 | |||
| Marital status | ||||||
| Single | 63 (79.7) | 16 (20.3) | 79 | 20.23 | 3 | 0.0002 |
| Married | 108 (98.2) | 2 (1.8) | 110 | |||
| Divorced/separated | 6 (100) | 0 (0) | 6 | |||
| Widowed | 5 (100) | 0 (0) | 5 | |||
| Ethnicity | ||||||
| Hausa | 7 (100) | 0 (0) | 7 | 1.51 | 3 | 0.60 |
| Igbo | 45 (90.0) | 5 (10.0) | 50 | |||
| Yoruba | 126 (91.3) | 12 (8.7) | 138 | |||
| Others | 4 (80.0) | 1 (20.0) | 5 | |||
| Religion | ||||||
| Christianity | 153 (90.0) | 17 (10.0) | 170 | 1.38 | 1 | 0.21 |
| Islam | 29 (96.7) | 1 (3.3) | 30 | |||
| Age at first intercourse (year) | ||||||
| <20 | 19 (95.0) | 1 (5.0) | 20 | 4.24 | 3 | 0.34 |
| 20–24 | 62 (93.9) | 4 (6.1) | 66 | |||
| 25–29 | 76 (86.4) | 12 (13.6) | 88 | |||
| ≥30 | 25 (96.2) | 1 (3.8) | 26 | |||
Table 7.
Associations between sociodemographic variables and uptake of Pap smear
| Variable | Have done Pap smear (%) | χ 2 | df | p | ||
|---|---|---|---|---|---|---|
| Yes | No | Total | ||||
| Age (year) | ||||||
| 20–29 | 9 (11.7) | 68 (88.3) | 77 | 24.51 | 3 | 0.0001 |
| 30–39 | 11 (15.3) | 61 (84.7) | 72 | |||
| 40–49 | 13 (33.3) | 26 (66.7) | 39 | |||
| ≥50 | 8 (66.7) | 4 (33.3) | 12 | |||
| Marital status | ||||||
| Single | 6 (7.6) | 73 (92.4) | 79 | 13.83 | 3 | 0.001 |
| Married | 31 (28.2) | 79 (71.8) | 110 | |||
| Divorced/separated | 2 (33.3) | 4 (66.7) | 6 | |||
| Widowed | 2 (40.0) | 3 (60.0) | 5 | |||
| Ethnicity | ||||||
| Hausa | 3 (42.9) | 4 (57.1) | 7 | 3.65 | 3 | 0.32 |
| Igbo | 9 (18.0) | 41 (82.0) | 50 | |||
| Yoruba | 29 (21.0) | 109 (79.0) | 138 | |||
| Others | 0 (0) | 5 (100) | 5 | |||
| Religion | ||||||
| Christianity | 27 (15.9) | 143 (84.1) | 170 | 14.83 | 1 | 0.0003 |
| Islam | 14 (46.7) | 16 (53.3) | 30 | |||
| Age at first intercourse (year) | ||||||
| <20 | 5 (25.0) | 15 (75.0) | 20 | 2.87 | 3 | 0.57 |
| 20–24 | 9 (13.6) | 57 (86.4) | 66 | |||
| 25–29 | 21 (23.9) | 67 (76.1) | 88 | |||
| ≥30 | 6 (23.1) | 20 (76.9) | 26 | |||
Discussion
At every stage in life, a woman in the third world risks some serious health problems. These include HIV/AIDS, high maternal mortality rates, and cancer of the cervix later in life. Cancer of the cervix is a preventable disease, and a key aspect of its prevention is the detection of the premalignant form by cervical screening [13]
This present study has shown that nurses are aware of cervical cancer (99%) which is consistent with the earlier study of [13]. It also corroborates the reports of [14] that showed a good association between level of education and cervical cancer awareness. The major sources of information about cervical screening as revealed in this study were through electronic media and health professionals. But it is a thing of concern that information about cervical cancer is poorly disseminated in churches and mosque (7.6%). It may be important that churches and mosques begin to have a forum to discuss health issues as information obtained from these spiritual institutions are usually taken serious.
Though the respondents have good knowledge of the causes and signs of cervical cancer, a few proportions (18.5%) felt that excess intake of alcohol could cause the disease. The respondents are quiet aware of Pap smear (91%) as one of the screening techniques of cervical cancer and have good attitudes (89%) towards Pap smear, but most of them have never done it before. The extremely low percentage (12%) of the respondents above 50 years who have done Pap smear is consistent with the studies of [14, 15] that showed a good correlation between old age and low Pap smear testing. Quite sizable percentage (18.5%) of the respondent thought that Pap smear is used to prevent cervical cancer and that Pap smear should be done once in a lifetime. The study further revealed a majority of the respondents not to know colposcopy as one of the screening techniques for cervical cancer. These wrong opinions may necessitate institutional-based workshop and training on cervical cancer and other diseases so as to give people good knowledge of the disease.
The findings from this study showed that some respondents (17%) did not do Pap smear because it is costly. This observation is consistent with the work of [16] that showed that socioeconomic status played important role in the demand for cervical cancer screening. Women should be on health insurance programmes so as to encourage them to regularly undergo this examination as earlier recommended by [17]. This present study further revealed that there are significant associations (p ≤ 0.05) between age of respondents, marital status, and awareness and uptake of cervical cancer screening. This assertion may be justified by the fact that married people of reproductive age are more susceptible to cervical cancer than older married people who have passed the reproductive age.
Finally, it has been made known from this study that nurses have good knowledge of cervical cancer but have limited understanding of the types of cervical cancer screening techniques and poor disposition towards undergoing cervical cancer screening. It may thus be recommended that institutions should periodically organise seminars and training for health personnel especially the nurses which form a group of professionals that can give health education to women about cervical cancer. This training may be done as part of the orientation programme to newly employed staff. Moreover, hospital-based pro-screening campaign is highly advocated so as to enhance prevention of cervical cancer.
Acknowledgments
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Jimoh AS, Abdul IF. A review of one hundred and three (103) histologically confirmed cases of carcinoma of the cervix at the University of Ilorin Teaching Hospital Nigeria. Niger Med Pract. 2004;45:55–60. [Google Scholar]
- 2.Adefuye PO. Knowledge and practice of cervical cancer screening among female professional health workers in a sub-urban district of Nigeria. Niger Med Pract. 2006;50(1):19–22. [Google Scholar]
- 3.Adebamowo CA, Ajayi OO. Breast cancer in Nigeria. West Afr J Med. 2000;19:179–194. [PubMed] [Google Scholar]
- 4.Madong BM, Madaka AKJ, Mannaseh AN. Malignant disease in Jos: a follow up. Ann Afr Med. 2003;2:48–53. [Google Scholar]
- 5.Bosch FX, Lorincz AT, Munoz N, Meijer CJ, Shah KV. The causal relation between human papillomavirus and cervical cancer. J Clin Pathol. 2002;55:244–265. doi: 10.1136/jcp.55.4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muñoz N, Bosch FX, de Sanjosé S. The causal link between human papillomavirus and invasive cervical cancer: a population-based case-control study. Int J Cancer. 2006;119(5):1108–1124. doi: 10.1002/ijc.21953. [DOI] [PubMed] [Google Scholar]
- 7.Schiller JT, Castellsagu X, Villa LL, Hildesheim A. An update of prophylactic human papillomavirus L1 virus-like particle vaccine clinical trial results. Vaccine. 2008;26(Suppl 10):K53–K61. doi: 10.1016/j.vaccine.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Redmond O’Neal (2009) Cancer-stricken Farrah Fawcett weighs 86 pounds: Redmond O’Neal www.thaindian.com/.../cancer-stricken-farrah-fawcett-weighs-86-pounds-redmond-oneal_100181396.html USA
- 9.IARC (2003) Hand book on cancer. www.iarc.fr/en/media-centre/pr/2003/index
- 10.Dillner J, Rebolj M, Birembaut P, Petry KU, Szarewski A, Munk C, de Sanjose S, Naucler P, Lloveras B, Kjaer S, Cuzick J, van Ballegooijen M, Clavel C, Iftner T. Long term predictive values of cytology and human papillomavirus testing in cervical cancer screening: joint European cohort study. BMJ. 2008;337:a1754. doi: 10.1136/bmj.a1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Audu BM, El-Nafaty AU, Khalil M, Otubu JAM. Knowledge and attitude of cervical cancer screening among women in Maiduguri. J Obstet Gynaecol. 1999;19(3):295–297. doi: 10.1080/01443619965110. [DOI] [PubMed] [Google Scholar]
- 12.Ayinde OA, Omigodun AO. Knowledge, attitude and practices related to prevention of cancer of the cervix among female health workers in Ibadan. J Obstet Gynaecol. 2003;23(1):59–62. doi: 10.1080/0144361021000043272. [DOI] [PubMed] [Google Scholar]
- 13.Ezem BU. Awareness and uptake of cervical cancer screening in Owerri, South-Eastern Nigeria. Ann Afr Med. 2007;6(3):94–98. doi: 10.4103/1596-3519.55727. [DOI] [PubMed] [Google Scholar]
- 14.Mandelblatt JS. Is HIV infection a cofactor for cervical squamous cell neoplasia? Cancer Epidemiol Biomark Prev. 1999;8:97–106. [PubMed] [Google Scholar]
- 15.Wang PD, Lin RS. Sociodemographic factors of Pap smear screening in Taiwan. Public Health. 1996;110(2):123–127. doi: 10.1016/S0033-3506(96)80059-X. [DOI] [PubMed] [Google Scholar]
- 16.Wang PD (2005) Acceptance of Pap smear testing. In: Chapter two of theoretical framework. Nccur.lib.nccu.du.tw/bitstream
- 17.Rodriguez WR, Christodoulides N, Floriano PN, Graham S, Mohanty S. A microchip CD4 counting method for HIV monitoring in resource-poor settings. PLoS Med. 2005;2(7):e182. doi: 10.1371/journal.pmed.0020182. [DOI] [PMC free article] [PubMed] [Google Scholar]


