Abstract
OBJECTIVE:
To assess the prevalence of urinary incontinence and associated vaginal squeeze pressure in primiparous women with and without previous gestational diabetes mellitus two years post-cesarean delivery.
METHODS:
Primiparous women who delivered by cesarean two years previously were interviewed about the delivery and the occurrence of incontinence. Incontinence was reported by the women and vaginal pressure evaluated by a Perina perineometer. Sixty-three women with gestational diabetes and 98 women without the disease were screened for incontinence and vaginal pressure. Multiple logistic regression models were used to evaluate the independent effects of gestational diabetes.
RESULTS:
The prevalence of gestational incontinence was higher among women with gestational diabetes during their pregnancies (50.8% vs. 31.6%) and two years after a cesarean (44.8% vs. 18.4%). Decreased vaginal pressure was also significantly higher among women with gestational diabetes (53.9% vs. 37.8%). Maternal weight gain and newborn weight were risk factors for decreased vaginal pressure. Maternal age, gestational incontinence and decreased vaginal pressure were risk factors for incontinence two years after a cesarean. In a multivariate logistic model, gestational diabetes was an independent risk factor for gestational incontinence.
CONCLUSIONS:
The prevalence of incontinence and decreased vaginal pressure two years post-cesarean were elevated among women with gestational diabetes compared to women who were normoglycemic during pregnancy. We confirmed an association between gestational diabetes mellitus and a subsequent decrease of vaginal pressure two years post-cesarean. These results may warrant more comprehensive prospective and translational studies.
Keywords: Cesarean delivery, Gestational diabetes mellitus, Vaginal squeeze pressure, Pregnant, Urinary incontinence
INTRODUCTION
Diabetes increases the risk of urinary incontinence (UI) 2.5 fold,1-3 although the mechanisms by which type 2 Diabetes Mellitus (type 2 DM) contributes to UI development and severity are not well understood.4 Diabetes is associated with an impairment of muscle strength and physical function.5 There is a temporal relationship between the time of diabetes diagnosis and subsequent development of muscle weakness and other related complications, such as diabetic amyotrophy.6
Gestational diabetes mellitus (GDM) is a metabolic disorder that is considered to be similar to type 2 DM. In GDM, pregnancy acts as a “stress factor,” revealing an individual's tendency to become diabetic.7 GDM is associated with macrosomia, shoulder dystocia, cesarean section (CS), intrauterine fetal growth alterations and perinatal mortality.8,9 Fetal macrosomia increases the risk for the development of GDM-independent UI,10 and one of the confounding variables in the development of UI is delivery method. Chawla et al. demonstrated an association between multiparity and vaginal delivery with an increased risk for UI and decreased vaginal squeeze pressure (VSP).11
Diabetes and vaginal deliveries are the most significant risk factors implicated in the incidence of UI,3 although little is known about whether GDM and the length of time elapsed after GDM are connected to a loss of bladder control. Kim et al. demonstrated that UI is common among women with a history of GDM but does not appear to be associated with physical activity level or body mass index (BMI).12 The Kim study neither quantified pelvic floor muscle function nor controlled for the mode and number of deliveries and the time from delivery to evaluation. More detailed information would allow for quantification of UI risk of UI within the population affected by GDM, such as women who will be receiving a CS for their current pregnancy or those who have received a CS during previous pregnancies. The aim of this study was to evaluate the prevalence of UI and VSP two years post-CS in primiparous women with or without previous Gestational diabetes mellitus (pGDM) and to investigate the association between UI, VSP and pGDM.
MATERIALS AND METHODS
The Institutional Review Board of Botucatu Medical School, UNESP-Univ Estadual Paulista, São Paulo, Brazil, granted approval for this prospective study, and all subjects gave informed written consent.
This study consisted of a cross-sectional survey conducted at the Department of Gynecology and Obstetrics General Hospital, a university hospital. All women who participated in this study, when pregnant, were patients of this hospital and were routinely screened for GDM at 24-28 weeks of gestation. The cutoff values for the diagnosis of GDM were those proposed by Carpenter & Coustan,13 i.e., 95 mg/dl, 180 mg/dl, 155 mg/dl, and 140 mg/dl, at fasting, one, two and three hours after oral glucose load, respectively.
All women in this perinatal database who had delivered two years earlier (between January 1st, 2004, and September 30th, 2004), a total of 529 subjects, were eligible for inclusion in the study. They were contacted by phone and invited to participate. The women answered questions based on the Questionnaire for Urinary Incontinence Diagnosis14 and the International Consultation on Incontinence Questionnaire - Short Form (ICIQ-SF) translated into Portuguese and validated with Brazilian female patients complaining of urinary incontinence.15 The patients were questioned about the following aspects of pregnancy and childbirth: maternal weight gain, the newborn weight, if they entered partum labor, postpartum complications, involuntary urine loss (for efforts such as coughing, sneezing, laughing, catching weight, squatting, walking and/or involuntary urine lost when feeling a strong urge to urinate, contact with water, sound of running water or if exposed to low temperatures) during pregnancy and postpartum.
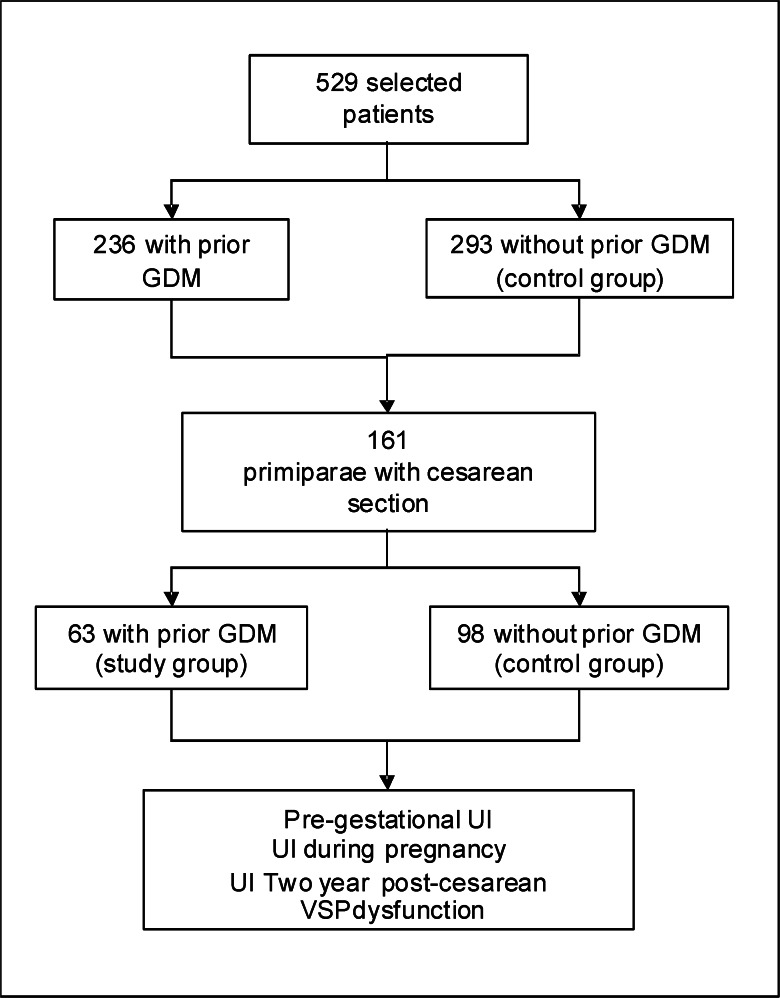
Of the 529 possible participants, 161 eligible primiparous women with singleton pregnancies delivered by CS who met the inclusion criteria were identified. An overview of the study design is outlined in Figure 1. Power analysis was performed based on a positive diagnosis of hyperglycemia during pregnancy with a type I error of 0.05 and a type II error of 0.20. The analysis indicated that the minimum number of patients enrolled in each group should be 62.
Figure 1.
Overview of the study design.
A trained physician who was blinded to the results of the oral glucose tolerance test obtained obstetric and maternal data relating to the index pregnancy from the hospital records. Demographic data collected included maternal age, gestational age at delivery, body mass index (BMI-weight in kilograms divided by height in meters squared), weight gain during pregnancy, delivery method and birth weight.
Two years postpartum, all patients were interviewed regarding their UI symptoms and the prevalence of these symptoms before, during and two years after the index pregnancy. The same author conducted all interviews. UI was as defined by Abrams et al.12 as an involuntary leakage of urine. After the interview, bidigital palpation and perineometry were performed. First, vaginal bidigital palpation was performed with the woman's knees semi-flexed. The subjects were asked to squeeze the vagina three times.16 While the subjects were in the same position, a vaginal latex sensor called a Perina perineometer was employed to measure the strength of the squeezes (Quark, São Paulo, Brazil). Based on a previous study of nulliparous women, perineometric values higher than 33.6 mmHg were considered to be normal. The perineometer used was not a validated device. It was selected based on the results of a pilot study of Barbosa.17
Statistical analyses were performed using the PASW Statistics v.17.0.2 and SAS 9.03 software programs. The statistical significance level was set at p<0.05. Categorical variables were analyzed using descriptive procedures and are expressed as percentages. The impacts of maternal age, gestational age at delivery, BMI, weight gain during pregnancy, birth weight, GDM, VSP and UI two years postpartum were evaluated in univariate analyses. Multiple logistic regression models were then used to evaluate the independent effects of GDM and maternal age on gestational UI after controlling for other significant factors.
Odds ratios were computed to express the magnitude of the association between UI, VSP and GDM with 95% confidence intervals to express statistical significance. The adjusted odds ratios (OR) and estimates of 95% confidence intervals (95% CI) were based on the Mantel-Haenszel χ2 test. The adjusted odds ratios were calculated to express the magnitude of the association between prior GDM and UI/VSP and were controlled for other confounding variables. For logistic regression analyses, UI and VSP were used as the response variables.
RESULTS
Clinical data for pGDM patients and control subjects at the time of pregnancy and two years after CS are shown in Table 1. Among the 161 patients enrolled, 63 (39.1%) had pGDM and 98 (60.9%) did not have pGDM. The length of time since the index pregnancy was similar for both groups (25.8±3.2 months for pGDM and 24.8±2.1 months for controls). The overall prevalence of gestational UI and two-year postpartum UI was significantly higher among women with pGDM (50.8% and 44.4%, respectively) than among normoglycemic pregnant women (31.6% and 18.4%, respectively, p<0.01). In addition, decreased VSP was more frequently found in women with pGDM two years after receipt of CS than in the control group (53.9% and 31.6%, respectively, p = 0.04). Subject skin color, black, was homogeneous for both groups (14.2% for pGDM and 13.3% for controls, p = 0.08).
Table 1.
Characteristics of women with and without GDM during their pregnancies and two years post- cesarean section.
| Control groupn = 98 | GDMn = 63 | ||||
| n (%) | m ± sd | n (%) | m ± sd | p-value | |
| Maternal age two years post-cesarean | — | 25.4±3.2 | — | 29.3±6.15 | 0.0001 |
| Gestational age at delivery (w) | — | 39.7±1.3 | — | 38.7±0.8 | 0.0001 |
| Weight gain during index gestation (kg) | — | 14.6±4.1 | — | 17.3±6.1 | 0.0003 |
| Newborn weight (g) | — | 3143.1±472.9 | — | 3546.2±440.6 | 0.0001 |
| Length of time since index pregnancy (y) | — | 24.8±2.1 | — | 25.0±0.8 | 0.4621 |
| BMI (kg/m2) | — | 25.5±4.3 | — | 25.8±3.2 | 0.5748 |
| Decresead of VSP | 37 (37.8) | — | 34 (53.9) | — | 0.0431 |
| Pre-gestational UI | 7 (7.1) | — | 10 (15.9) | — | 0.0785 |
| Gestational UI | 31 (31.6) | — | 32 (50.8) | — | 0.0151 |
| UI two years postpartum | 18 (18.4) | — | 28 (44.4) | — | 0.0004 |
| Black skin color | 13 (13,3) | — | 9 (14,2) | — | 0.0823 |
Women with pGDM were older (29.3±6.1 years vs. 25.4±3.2 years) and experienced greater weight gain during pregnancy (17.3±6.1 vs. 14.6±4.1) compared to controls. Women with pGDM were more likely to have a lower gestational age at delivery (38.7±0.8 weeks vs. 39.7±1.3 weeks) and a higher newborn weight (3546.2±440.6 grams vs. 3143.1±472.9 grams, Table 1).
In the multivariate logistic model, newborn weight (OR 1.002; 95% CI: 1.001-1.002) and maternal weight gain (OR 1.295; 95% CI: 1.176-1.425) was associated with a decrease in VSP in cases of pGDM (Table 2). We constructed a separate model for two-year post-CS UI in women with pGDM and found that maternal age (OR 1.181; 95% CI: 1.022-1.365), gestational UI (OR 4.992; 95% CI: 1.383-18.023) and a decrease in VSP incidence (OR 20.416; 95% CI: 3.548-117.479) were associated factors (Table 3). In the multivariate logistic models, pGDM was an independent risk factor (OR 2.26; 95% CI: 1.116-4.579) for gestational UI (Table 4).
Table 2.
Estimated ß parameter, odds ratio (OR), 95% confidence interval (95% CI) and p-value obtained by adjusting the multivariate logistic model for investigating decresead of VSP two years after GDM.
| VSP – Perineometer | |||
| Variables | OR | 95% CI | p-value |
| Maternal age two years post- cesarean | 0.994 | 0.910 - 1.087 | 0.8425 |
| Gestational age (w) | 0.759 | 0.533 - 1.081 | 0.1265 |
| Newborn weight (g) | 1.002 | 1.001 - 1.002 | 0.0006 |
| Weight gain during gestation (kg) | 1.295 | 1.176 - 1.425 | <0.0001 |
| Two groups (GDM) | 0.516 | 0.191 - 1.394 | 0.1917 |
Table 3.
Estimated ß parameter, odds ratio (OR), 95% confidence interval (95% CI) and p-value obtained by adjusting the multivariate logistic model for investigating UI two years after GDM.
| UI two-year postpartum | |||
| Variable | OR | 95% CI | p-value |
| Maternal age two years post- cesarean | 1.181 | 1.022 - 1.365 | 0.024 |
| Pre-gestational UI | 4.498 | 0.437 - 46.313 | 0.206 |
| Gestational UI | 4.992 | 1.383 - 18.023 | 0.014 |
| Abnormal VSP | 20.416 | 3.548 - 117.479 | 0.001 |
Table 4.
Estimated ß parameter, odds ratio (OR), 95% confidence interval (95% CI) and p-value obtained by adjusting the multivariate logistic model for investigating gestational UI.
| Gestational UI | |||
| Variable | OR | 95% CI | p-value |
| Maternal age at time pregnancy | 0.997 | 0.930-1.068 | 0.9250 |
| GDM | 2.260 | 1.116-4.579 | 0.0236 |
DISCUSSION
GDM is considered to be an early stage in the natural history of type 2 DM. Women with prior GDM are at a higher risk of developing type 2 DM or some degree of glucose intolerance two to twelve years after the index pregnancy.18 In the present study, the presence of pGDM increased the incidence rate of UI not only during pregnancy but also after a CS. Approximately half of the women with pGDM reported having UI during their pregnancy (50.8%) and two years post-CS (44.4%). These results confirm an association between pGDM, UI and decreased VSP.
It is interesting to note that blood glucose levels do not become sufficiently elevated to cause osmotic diuresis or increase involuntary urinary loss during pregnancy.9 A history of at least one vaginal delivery, family history of prolapsed and a macrosomatic fetus have been shown to be independent risk factors for urinary incontinence and prolapse.10 The greater weight gain for fetuses in women with GDM, resulting in increased intra-abdominal pressure, could also contribute to UI. It is important to take into consideration that delivery at an earlier gestational age could decrease the rate of UI perinatal complications because of the smaller expected size of prematurely delivered newborns.19
An increased prevalence of UI among women with diabetes has been reported in cross-sectional analyses.20 In the NHANES 2001-2002 study, one in three women with impaired fasting glucose or diabetes reported weekly or more frequent UI.21 However, no previous studies have examined whether women with pGDM also have an increased prevalence of UI two years after a CS. The results presented here suggest that the cesarean delivery route does not protect against UI two years after delivery in women with pGDM. Instead, our results suggest that the complications of pGDM, including possible microvascular disease, seem to be a more relevant factor than the mode of delivery.
The potential mechanisms by which diabetes causes incontinence include microvascular damage to the innervation of the bladder and urethral sphincter, detrusor muscle dysfunction, sphincter dysfunction, overactive bladder, urinary retention and elevated post-void residual urine volume, which contributes to overflow incontinence, chronic bacterial colonization, urinary tract infections and hyperglycemia.22 Moreover, the microvascular complications associated with type 2 DM may damage the innervation of the bladder and/or alter detrusor muscle function.23
The present study has also demonstrated that patients with pGDM have a larger VSP decrease (50.8%) two years post-CS than the controls (37.8%). The results of a study by Casey et al. indicated that the increased prevalence of decreased VSP could be related to high rates of obesity and macrosomia pregnancies. Our results partially confirm these results, as there remains an association between newborn weight and VSP (OR 1.295 CI95% 1.176-1.425). Diabetes is associated with impaired muscle strength and physical function and may provide a link between the metabolic and mechanical functions of muscles.5 Motor dysfunction is considered an end-stage manifestation of severe polyneuropathy with an annual decline in muscle strength of approximately 3%, although motor function in type 2 DM is still unknown.24 Muscle weakness is considered a progressive late complication in diabetic distal symmetric polyneuropathy and has been associated with atrophy of striated muscle, probably because of insufficient re-innervation.24 Almost all muscle weakness in diabetes relates to distal weakness and the atrophy of the muscles of the lower leg and foot.24,25
In a multivariate logistic model, maternal weight gain during pregnancy and newborn weight were associated with decreased VSP, and GDM itself was not a significant risk factor (Table 2). This finding suggests that decreased VSP two years post-CS may be a consequence of either maternal or perinatal adverse effects related to GDM, maternal weight gain during pregnancy and newborn weight. GDM has previously been associated with both an increased risk of fetal and neonatal macrosomia26 and high maternal BMI.27
A higher BMI could theoretically enhance abdominal pressure, thereby increasing bladder pressure and urethral mobility, which could lead to the association seen between BMI and UI.22 Excessive body weight could also affect bladder pressure and could also be a factor in the development of UI.27 Therefore, decreased VSP two years post-CS in women with pGDM may be a consequence of the interaction between pregnancy and GDM. Our findings that advanced maternal age, UI during pregnancy and decreased VSP are risk factors for UI suggest that UI may also be an indirect consequence of GDM.
We are aware that our study sample and findings may be biased by the facts that the incontinence outcomes were self-reported and that patients were from a prenatal care service with routine screening for GDM. Patients who are symptomatic may be more willing to undergo an evaluation and receive treatment. However, our findings are in agreement with a previous study.12 Our data confirm the interaction between pGDM, UI and decreased VSP. Our data also extend this association to women who delivered by CS. These observations strongly suggest that further more comprehensive, prospective controlled and translational studies are warranted.
CONCLUSIONS
The prevalence of UI and decreased VSP two years post-CS were elevated among women with pGDM compared to normoglycemic controls during pregnancy. We confirmed an association between pGDM and a subsequent VSP decrease two years post-CS. These results may warrant the beginning of more comprehensive prospective and translational studies.
ACKNOWLEDGMENTS
This research was supported in part by the Research Support Foundation of the State of São Paulo and Coordination for the Improvement of Higher Education Personnel. The authors are grateful to Tatiana Casagrande and Carlos Negrato and to the Research Support Center of Botucatu Medical School, UNESP - Univ Estadual Paulista for their valuable contributions to the study design and statistical analysis.
REFERENCES
- 1.Sarma AV, Kanaya AM, Nyberg LM, Kusek JW, Vittinghoff E, Rutledge B, et al. Urinary incontinence among women with type 1 diabetes-how common is it. J Urol. 2009;181:1224–30. doi: 10.1016/j.juro.2008.11.024. 10.1016/j.juro.2008.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Izci Y, Topsever P, Filiz TM, Cinar ND, Uludag C, Lagro-Janssen T. The association between diabetes mellitus and urinary incontinence in adult women. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:947–52. doi: 10.1007/s00192-009-0888-8. 10.1007/s00192-009-0888-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alvaro R, Araco F, Gravante G, Sorge R, Overton J, Vellone E, et al. Epidemiological aspects of urinary incontinence in a female population of an Italian region. Int Urogynecol J Pelvic Floor Dysfunct. 2010;21:873–83. doi: 10.1007/s00192-010-1112-6. 10.1007/s00192-010-1112-6 [DOI] [PubMed] [Google Scholar]
- 4.Brown JS, Wing R, Barrett-Connor E, Nyberg LM, Kusek JW, Orchard TJ, et al. Lifestyle intervention is associated with lower prevalence of urinary incontinence: the Diabetes Prevention Program. Diabetes Care. 2006;29:385–90. doi: 10.2337/diacare.29.02.06.dc05-1781. 10.2337/diacare.29.02.06.dc05-1781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sayer AA, Dennison EM, Syddall HE, Gilboy HJ, Phillips DIW, Cooper C. Type 2 Diabetes, Muscle Strength, and Impaired Physical Function. Diabetes Care. 2005;28:2541–2. doi: 10.2337/diacare.28.10.2541. 10.2337/diacare.28.10.2541 [DOI] [PubMed] [Google Scholar]
- 6.Helander I, Westerblad H, Katz A. Effects of glucose on contractile function, Ca2+, and glycogen in isolated mouse skeletal muscle. AmJ Physiol Cell Physiol. 2002;282:1306–12. doi: 10.1152/ajpcell.00490.2001. [DOI] [PubMed] [Google Scholar]
- 7.Buchanan TA, Xiang AH. Gestational diabetes mellitus. J Clin Invest. 2005;115:485–91. doi: 10.1172/JCI24531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lucas M J. Diabetes complicating pregnancy. Obstet Gynecol Clin North Am. 2001;28:513–36. doi: 10.1016/s0889-8545(05)70215-1. 10.1016/S0889-8545(05)70215-1 [DOI] [PubMed] [Google Scholar]
- 9.Rudge MVC, Calderon IMP, Ramos MD, Abbade JF, Rugolo LM. Perinatal outcome of pregnancies complicated by diabetes and by maternal daily hyperglycemia not related to diabetes. A retrospective 10-year analysis. Gynecol Obstet Invest. 2000;50:108–12. doi: 10.1159/000010293. 10.1159/000010293 [DOI] [PubMed] [Google Scholar]
- 10.Rodrigues AM, Girão MJB, Sartori C, Ferreira MG, Martins KF, Castro RA. COL1A1 Sp1-binding site polymorphism as a risk factor for genital prolapse. Int Urogynecol J. 2008;19:1471–5. doi: 10.1007/s00192-008-0662-3. 10.1007/s00192-008-0662-3 [DOI] [PubMed] [Google Scholar]
- 11.Chawla A, Reddy S, Thomas J. Risk factors for persistent stress urinary incontinence after mid-urethral procedures. Indian J Urol. 2008;24:130–1. 10.4103/0970-1591.44272 [PMC free article] [PubMed] [Google Scholar]
- 12.Kim C, McEwen LN, Sarma AV, Piette JD, Herman WH. Stress urinary incontinence in women with a history of gestational diabetes mellitus. J Womens Health (Larchmt) 2008;17:783–92. doi: 10.1089/jwh.2007.0616. 10.1089/jwh.2007.0616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carpenter MW, Coustan DR. Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol. 1982;144:768–73. doi: 10.1016/0002-9378(82)90349-0. [DOI] [PubMed] [Google Scholar]
- 14.Bradley CS, Rovner ES, Morgan MA, Berlin M, Novi JM, Shea JA, et al. A new questionnaire for urinary incontinence diagnosis in women: development and testing. Am J Obstet Gynecol. 2005;192:66–73. doi: 10.1016/j.ajog.2004.07.037. 10.1016/j.ajog.2004.07.037 [DOI] [PubMed] [Google Scholar]
- 15.Tamanini JT, Dambros M, D'Ancona CA, Palma PC, Rodrigues Netto N., Jr [Validation of the “International Consultation on Incontinence Questionnaire - Short Form”. (ICIQ-SF) for Portuguese]. Rev Saude Publica. 2004;38:438–44. doi: 10.1590/s0034-89102004000300015. 10.1590/S0034-89102004000300015 [DOI] [PubMed] [Google Scholar]
- 16.Barbosa PB, Franco MM, Souza Fde O, Antonio FI, Montezuma T, Ferreira CH. Comparison between measurements obtained with three different perineometers. Clinics. 2009;64:527–33. doi: 10.1590/S1807-59322009000600007. 10.1590/S1807-59322009000600007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barbosa AMP, Carvalho LR, Martins AMVC, Calderon IMP, Rudge MVC. Efeito da via de parto sobre a força muscular do assoalho pélvico. Rev Bras Ginecol Obstet. 2005;27:677–82. 10.1590/S0100-72032005001100008 [Google Scholar]
- 18.Seely EW. Does treatment of gestational diabetes mellitus affect pregnancy outcome. Nat Clin Pract Endocrinol Metab. 2006;2:72–3. doi: 10.1038/ncpendmet0081. 10.1038/ncpendmet0081 [DOI] [PubMed] [Google Scholar]
- 19.Pimenta WP, Calderon IMP, Cruz NS, Santos ML, Aragon FF, Padovani CR. Subclinical anormalities o glucose metabolism in Brazilian women with a history of gestational diabetes mellitus. Acta Obstet Gynecol Scand. 2004;83:1152–8. doi: 10.1111/j.0001-6349.2004.00444.x. [DOI] [PubMed] [Google Scholar]
- 20.Jackson SL, Scholes D, Boyko EJ, Abraham L, Fihn SD. Urinary incontinence and diabetes in postmenopausal women. Diabetes Care. 2005;28:1730–8. doi: 10.2337/diacare.28.7.1730. 10.2337/diacare.28.7.1730 [DOI] [PubMed] [Google Scholar]
- 21.Brown JS, Vittinghoff E, Lin F, Nyberg LM, Kusek JW, Kanaya AM. Prevalence and risk factors for urinary incontinence in women with type 2 diabetes and impaired fasting glucose: findings from the National Health and Nutrition Examination Survey (NHANES) 2001-2002. Diabetes Care. 2006;29:1307–12. doi: 10.2337/dc05-2463. 10.2337/dc05-2463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jackson RA, Vittinghoff E, Kanaya AM, Miles TP, Resnick HE, Kritchevsky SB, et al. Urinary incontinence in elderly women: findings from the Health, Aging, and Body Composition Study. Obstet Gynecol. 2004;104:301–7. doi: 10.1097/01.AOG.0000133482.20685.d1. 10.1097/01.AOG.0000133482.20685.d1 [DOI] [PubMed] [Google Scholar]
- 23.Ellenberg M. Development of urinary bladder dysfunction in diabetes mellitus. Am Intern Med. 1980;92:321–3. doi: 10.7326/0003-4819-92-2-321. [DOI] [PubMed] [Google Scholar]
- 24.Andreassen CS, Jakobsen J, Andersen H. Muscle weakness. Diabetes. 2006;55:806–12. doi: 10.2337/diabetes.55.03.06.db05-1237. 10.2337/diabetes.55.03.06.db05-1237 [DOI] [PubMed] [Google Scholar]
- 25.Andersen H, Nielsen S, Mogensen CE, Jakobsen J. Muscle strength in type 2 diabetes. Diabetes. 2004;53:1543–8. doi: 10.2337/diabetes.53.6.1543. 10.2337/diabetes.53.6.1543 [DOI] [PubMed] [Google Scholar]
- 26. Oh W.Neonatal outcome and care (2004) In Diabetes in women. Adolescence, Pregnancy and Menopause. 3rd ed Reece E A, Coustan D R, Gabbe S G, Eds. Lippincott, Williams & Wilkins, pp. 451–9. [Google Scholar]
- 27. Mestman JH.Interaction between pregnancy, gestational diabetes, and long-term maternal outcome (2004). Diabetes in women. Adolescence, Pregnancy and Menopause. 3rd ed Reece E A, Coustan D R, Gabbe S G, Eds. Lippincott, Williams & Wilkins, pp. 233–41. [Google Scholar]