Abstract
OBJECTIVE
To determine the prevalence of impaired fasting glucose (IFG) and undiagnosed and diagnosed diabetes in Thai adults in 2009 and examine the extent of changes in proportions of diagnosis, treatment, and control for blood glucose, high blood pressure, and high total cholesterol between 2004 and 2009.
RESEARCH DESIGN AND METHODS
Data from the multistage cross-sectional National Health Examination Survey (NHES) IV of 18,629 Thai adults aged ≥20 years conducted in 2009 were used to analyze and compare with the data from NHES III in 2004.
RESULTS
The prevalence of IFG and diabetes was 10.6 and 7.5%, respectively. Of all diabetes diagnoses, 35.4% were not previously diagnosed, and the proportion was higher in men than in women (47.3 vs. 23.4%, P < 0.05). Compared with those in year 2004, the proportions of individuals with diabetes and concomitant hypertension did not significantly decrease in 2009 in both sexes, but the proportions of women with diabetes who were abdominally obese or had high total cholesterol (≥5.2 mmol/L) significantly increased in 2009 by 18.0 and 23.5%, respectively (all P < 0.01). The rates of treatment and control of blood glucose, high blood pressure, and high total cholesterol were favorably improved in 2009. However, in substantial proportions of individuals with diabetes these concomitants were still controlled suboptimally.
CONCLUSIONS
The prevalence of diabetes and IFG remained high in Thai adults. Improvement in detection and control of diabetes and associated metabolic risk factors, particularly obesity and high serum cholesterol, are necessary.
Diabetes has become a major global public health burden. It has been estimated that the number of people with diabetes worldwide was 285 million in 2010 and will increase to 439 million in 2030, with the majority of increase (69%) occurring in developing countries (1). The estimated number of individuals with diabetes in Asia was 113 million in 2010 and will increase to 180 million in 2030 (2). The increase has been the result of the rise in obesity as a consequence of changes in lifestyle toward urbanization, with high energy intake and low physical activity following the rapid economic growth and urbanization in this region (2).
In Thailand, a low-middle income country, diabetes has been a major cause of morbidity and mortality in the past decade (3). Diabetes alone is responsible for 3.3 and 8.3% of total deaths in Thai men and women, respectively (3). A high prevalence rate of diabetes in Thailand makes it among the top ten in Asia (2). In 2004, the National Health Examination Survey (NHES) III reported a prevalence of 6.7% in adults aged ≥15 years, of whom 53.3% went undiagnosed. The prevalence of impaired fasting glucose (IFG) is 12.5% (4). Undiagnosed diabetes increases the risk of complications as a result of being untreated, and about 40% of those treated have their fasting plasma glucose (FPG) under control (<7.8 mmol/L) (4).
To monitor the diabetes situation, the fourth NHES was conducted in 2009. This study aimed to determine the prevalence of IFG, diabetes, and associated metabolic risk factors in Thai adults aged ≥20 years and older in 2009. Among individuals with diabetes, we also examined the extent of changes in proportions of metabolic risk factors and lack of diagnosis, treatment, and control for high blood glucose, high blood pressure, and high total cholesterol between the years 2004 and 2009.
RESEARCH DESIGN AND METHODS
The fourth Thai NHES (NHES IV) 2009 was a nationally representative cross-sectional survey using a multistage, stratified sampling of the Thai population. The survey was approved by the Ethical Review Committee for Research in Human Subjects, Ministry of Public Health. The multistage sampling frame was based on the population registers. For all regions, with the exception of Bangkok, the first stage was a random sample of five provinces in each of the four regions. At the second stage, three to five districts were selected, proportional to size (PPS), from each province. For the third step, in each province, 13–14 electoral units (EU) and villages were selected by the PPS method from urban and rural areas, respectively, which amounted to a total of 68 EU and 68 villages in each region. At the final stage, for each electoral unit per village, 8–10 men and women were selected by systematic random sampling from population registers from each of four broad age and sex groups (men and women aged 15–59 or ≥60 years). In Bangkok, 12 districts were randomly selected by PPS, and 5 to 6 EU were selected by PPS from each district. A total of 68 EU in Bangkok were selected. The method in the final stage was similar to those used in other regions. The final sample size was targeted at 21,960 individuals, and the final sample collected was 20,450 individuals (93.1%). In the current study, we excluded those aged <20 years from the analysis, leaving a total of 18,629 individuals aged ≥20 years in the study. The response rates for men and women aged ≥20 years were 85.5 and 95.4%, respectively, and 87.8% for urban and 93.7% for rural areas. NHES III, with a similar sampling approach to that of NHES IV, has been described in detail elsewhere (4). Initially, a total of 36 provinces were randomly selected. Then, 9 EU or villages were randomly selected by PPS. Finally, 15 people were selected from each of the four broad groups of male or female sex and 15–59 or ≥60 years of age. The current study included a total of 35,846 individuals aged ≥20 years in the analysis, with a response rate of 92.9% for this age-group.
Data collection and measurement
Questions on previously diagnosed diabetes, hypertension and high total cholesterol, and medication were asked. Weight, height, and waist circumference were measured by a standardized procedure (5). Participants were asked to fast 12 h overnight before the venous blood was obtained the next morning. Plasma glucose was measured at the provincial laboratory using a hexokinase enzyme method with standardized technique. All the provincial laboratories were standardized by a central laboratory of the Ministry of Public Health. Serum samples were frozen and transferred to a central laboratory in Ramathibodi Hospital, Mahidol University. Total serum cholesterol, HDL cholesterol, and triglyceride were measured using enzymatic colorimetric methods. LDL cholesterol was calculated based on the Friedewald formula for those with triglyceride <4.5 mmol/L and was directly measured by enzymatic method for those with triglyceride ≥4.5 mmol/L. Of note, in the 2004 survey only total cholesterol was measured. Blood pressure measurement was made by using standardized automatic blood pressure monitor model A100 (6). Each participant was seated for at least 5 min before the first reading of three serial measurements of blood pressure in a sitting position at 1 min apart (7).
Definition
Diagnosed diabetes was defined as a previous diagnosis of diabetes by a physician and intake of hypoglycemic drugs during the past 2 weeks. Undiagnosed diabetes was defined as FPG ≥7.0 mmol/L but a lack of previous diagnosis. IFG was defined as a FPG of 5.6 to <7.0 mmol/L (8). Hypertension was defined as systolic blood pressure (SBP) ≥140 mmHg, diastolic blood pressure (DBP) ≥90 mmHg, or use of blood pressure–lowering medication. High total cholesterol was defined as total serum cholesterol ≥5.2 mmol/L or use of cholesterol-lowering medication in the past 2 weeks. Individuals with diabetes were also categorized into four groups as follows: “undiagnosed,” “diagnosed but not treated,” “treated but not controlled,” and “treated and controlled.” Diabetes that was considered “treated and controlled” referred to treatment with glucose-lowering medication and FPG <7.2 mmol/L. Controlled high blood pressure referred to SBP/DBP <130/80 mmHg, and controlled total cholesterol referred to total cholesterol <5.2 mmol/L.
Statistical methods
Analysis was restricted to participants who had fasted >12 h before blood collection (90.1% of participants). All analyses were weighted to take into account the probability of sampling of the 2008 Thai population aged ≥20 years. Prevalence of diabetes was estimated for the whole population together with subgroups according to age-group, sex, and urban/rural location. Data from the 2004 NHES were obtained from the National Health Examination Office, Thailand. All comparisons by sex and year of surveys (2004 and 2009) were age and sex standardized to the national population in 2004. Among individuals with diabetes and concomitant hypertension or high total cholesterol, the proportions of undiagnosed, untreated, “treated but not controlled,” and “treated and controlled” for each concomitant were calculated. Adjusted Wald tests were used to examine the difference, with P < 0.05 considered statistically significant. Robust methods of variance estimation were used to take into account the complex survey design using STATA 10.1.
RESULTS
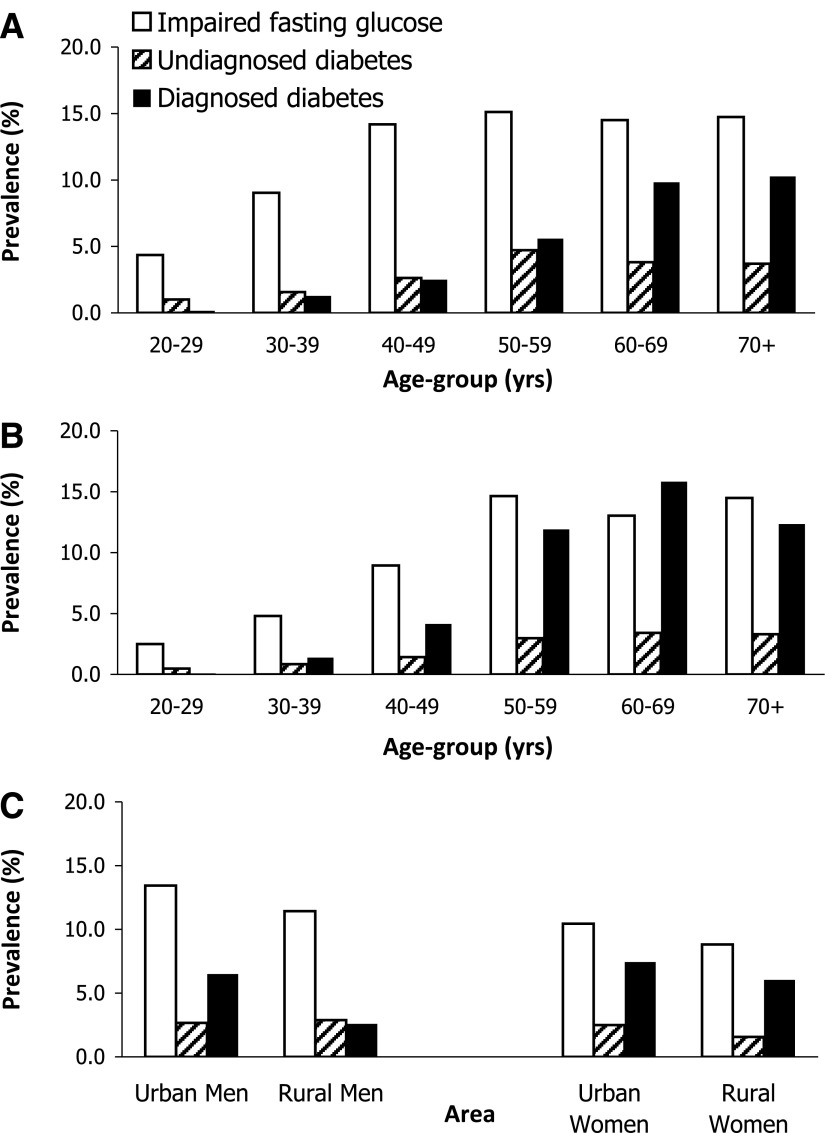
Age-adjusted prevalence of IFG, undiagnosed diabetes, and diagnosed diabetes in individuals aged ≥20 years was 10.6, 2.3, and 5.2%, respectively. The prevalence of IFG and undiagnosed diabetes increased with age and peaked at age ≥75 years and 55–64 years, respectively (Fig. 1A and B). The age-adjusted prevalence of IFG was significantly higher in men compared with women (12.0 vs. 9.5%, respectively; P < 0.01). The age-adjusted prevalence of all diabetes was 7.5% and was significantly higher in women than in men (8.3 vs. 6.6%; P < 0.01). A proportion of diabetes that was undiagnosed was significantly higher in men than in women (47.3 vs. 23.4%, respectively; P < 0.001). Total prevalence of diabetes was higher in urban residents than their counterpart in rural area for both sexes (P < 0.001 for both men and women). There were differences in the proportion of diabetes undiagnosed by area of residence (urban/rural) in men and women. For men, the proportion of diabetes that was undiagnosed was higher in rural than in urban areas (52.8 vs. 29.1%, respectively; P < 0.05). However, for women the proportions were in the opposite direction but not significantly different (20.6 vs. 25.2%, respectively; P = 0.11) (Fig. 1C).
Figure 1.
Age-specific prevalence of IFG, undiagnosed diabetes, and diagnosed diabetes in Thai adults aged ≥20 years. A: Men. B: Women. C: Age-adjusted prevalence of the hyperglycemic conditions by urban/rural area, NHES IV 2009.
Cardiovascular risk factors in those with IFG and diabetes
Table 1 shows characteristics and metabolic risk factors of men and women by diabetes status. Mean age was highest in the diagnosed diabetes group in both sexes, whereas mean FPG was highest in the undiagnosed group in women. In men, the mean BMI, waist circumference, and SBP were significantly highest and HDL cholesterol was lowest in the diagnosed diabetes group, whereas triglyceride and prevalence of smoking were highest in the undiagnosed diabetes group. In women, BMI, waist circumference, SBP, and triglyceride in undiagnosed diabetes were as high as in the diagnosed group, with the highest level of total cholesterol in the undiagnosed group. There were differences in educational levels; proportions of individuals with secondary school attainment or higher were highest in the normal FPG and lowest in the undiagnosed group in men and in the diagnosed group in women.
Table 1.
Age-standardized means and percentages (SE) of cardiovascular risk factors in Thai adults aged ≥20 years: NHES IV 2009
| Normal fasting glucose level | IFG | Undiagnosed diabetes | Diagnosed diabetes | P | |
|---|---|---|---|---|---|
| Men (n = 8,803) | |||||
| n | 6,658 | 1,250 | 305 | 590 | |
| Age (years) | 44.3 (0.3) | 49.5 (0.3) | 50.9 (0.7) | 57.3 (0.7) | <0.001 |
| FPG (mmol/L) | 4.6 (0.1) | 6.0 (0.1) | 8.9 (0.2) | 9.0 (0.4) | <0.001 |
| BMI (kg/m2) | 23.1 (0.1) | 24.6 (0.2) | 24.2 (0.2) | 26.8 (0.3) | <0.001 |
| Waist circumference (cm) | 79.4 (0.3) | 84.8 (0.5) | 84.7 (0.6) | 91.8 (0.8) | <0.001 |
| SBP (mmHg) | 122.8 (0.4) | 131.6 (0.7) | 132.3 (1.6) | 133.3 (1.6) | <0.001 |
| DBP (mmHg) | 76.5 (0.3) | 81.8 (0.5) | 82.6 (0.9) | 81.3 (0.8) | <0.001 |
| Total cholesterol (mmol/L) | 5.2 (0.1) | 5.6 (0.1) | 5.6 (0.1) | 5.3 (0.1) | 0.001 |
| HDL cholesterol (mmol/L) | 1.2 (0.01) | 1.2 (0.01) | 1.1 (0.02) | 1.0 (0.01) | <0.001 |
| LDL cholesterol (mmol/L) | 3.2 (0.03) | 3.4 (0.04) | 3.1(0.1) | 3.1 (0.1) | <0.001 |
| Triglyceride (mmol/L) | 1.9 (0.04) | 2.2 (0.1) | 3.4 (0.4) | 2.6 (0.1) | <0.001 |
| Current smoking (%) | 49.2 (1.1) | 40.6 (2.0) | 61.0 (3.5) | 38.9 (3.5) | 0.001 |
| Secondary school education or higher (%) | 38.7 (1.5) | 34.0 (2.1) | 27.4 (3.5) | 35.0 (2.8) | 0.001 |
| Family history of diabetes (%) | 24.0 (1.0) | 32.1 (2.0) | 33.1 (3.9) | 59.3 (3.3) | <0.001 |
| Women (n = 9,826) | |||||
| n | 7,532 | 1,117 | 263 | 914 | |
| Age (years) | 44.7 (0.2) | 52.8 (0.4) | 53.9 (1.0) | 57.1 (0.4) | <0.001 |
| FPG (mmol/L) | 4.6 (0.03) | 6.0 (0.1) | 9.3 (0.2) | 8.5 (0.2) | <0.001 |
| BMI (kg/m2) | 24.3 (0.1) | 26.6 (0.2) | 27.1 (0.7) | 26.9 (0.3) | <0.001 |
| Waist circumference (cm) | 78.3 (0.3) | 84.6 (0.6) | 87.6 (1.6) | 87.6 (0.6) | <0.001 |
| SBP (mmHg) | 119.2 (0.3) | 128.0 (0.8) | 132.4 (1.7) | 131.1 (1.3) | <0.001 |
| DBP (mmHg) | 73.7 (0.1) | 78.6 (0.5) | 80.1 (0.8) | 78.4 (0.6) | <0.001 |
| Total cholesterol (mmol/L) | 5.4 (0.1) | 5.8 (0.1) | 6.0 (0.17) | 5.6 (0.1) | <0.001 |
| HDL cholesterol (mmol/L) | 1.3 (0.01) | 1.2 (0.02) | 1.2 (0.03) | 1.2 (0.01) | <0.001 |
| LDL cholesterol (mmol/L) | 3.4 (0.03) | 3.6 (0.05) | 3.8 (0.1) | 3.4 (0.04) | <0.001 |
| Triglyceride (mmol/L) | 1.5 (0.03) | 1.9 (0.05) | 2.2 (0.1) | 2.2 (0.1) | <0.001 |
| Current smoking (%) | 2.8 (0.2) | 6.0 (1.4) | 2.4 (0.7) | 2.3 (0.6) | 0.001 |
| Secondary school education or higher (%) | 32.2 (1.2) | 19.8 (1.6) | 20.5 (3.8) | 13.6 (1.6) | 0.001 |
| Family history of diabetes (%) | 24.1 (1.0) | 35.6 (2.0) | 47.2 (5.3) | 65.4 (2.4) | <0.001 |
Changes in cardiovascular risk factors between 2004 and 2009
Age-standardized prevalence of diabetes slightly increased from year 2004 to 2009. The proportions of all diabetes cases with concomitant hypertension did not significantly decrease in 2009 in both sexes. However, the proportions of diabetic patients with abdominal obesity (waist circumference ≥90 cm for men and ≥ 80 cm for women) and high total cholesterol (at two cut points: ≥6.2 or ≥5.2 mmol/L) significantly increased in 2009, particularly for women (all P < 0.05) (Table2).
Table 2.
Age-adjusted prevalence (95% CI) and changes of cardiovascular risk factors among Thai adults aged ≥20 years with diabetes by sex between 2004 and 2009
| Men |
Women |
|||||
|---|---|---|---|---|---|---|
| 2004 | 2009 | % Change from 2004 | 2004 | 2009 | % Change from 2004 | |
| n | 1,824 | 895 | 2,439 | 1,177 | ||
| Diabetes | 6.3 (5.2–7.2) | 6.4 (5.5–7.3) | 2.1 | 7.6 (6.8–8.4) | 8.1 (7.4–8.8) | 5.5 |
| Hypertension | 46.3 (40.6–51.9) | 41.5 (37.1–46.0) | −10.2 | 47.6 (43.2–52.0) | 47.1 (42.1–52.1) | −1.0 |
| High total cholesterol (≥6.2 mmol/L or treated) | 30.6 (25.0–36.2) | 36.4 (31.0–41.9) | 18.8 | 34.4 (28.5–40.3) | 48.6 (43.6–53.6) | 41.3* |
| High total cholesterol (≥5.2 mmol/L or treated) | 57.2 (47.5–66.9) | 57.3 (51.6–63.0) | 0.2 | 60.1 (52.8–67.3) | 74.2 (69.1–79.2) | 23.5* |
| High LDL cholesterol (≥2.6 mmol/L or treated) | NA | 76.1 (70.6–81.6) | NA | NA | 86.4 (83.3–89.6) | NA |
| BMI 23 to <25 kg/m2 | 19.0 (15.7–22.8) | 20.3 (15.2–26.4) | 6.6 | 19.1 (16.2–22.4) | 18.3 (14.5–22.9) | −3.9 |
| BMI ≥25 kg/m2 | 45.1 (37.6–52.6) | 49.7 (44.0–55.5) | 10.1 | 56.3 (50.6–61.9) | 63.8 (58.4–69.2) | 13.2 |
| Abdominal obesity | 38.9 (32.5–45.3) | 40.3 (35.7–45.0) | 3.6 | 66.7 (60.8–72.5) | 78.6 (74.7–82.6) | 18.0* |
| Current regular smoker | 41.6 (36.5–46.6) | 45.1 (38.6–51.6) | 8.6 | 2.6 (1.4–3.8) | 1.9 (0.8–3.0) | −26.2 |
Abdominal obesity: waist circumference ≥90 cm for men and ≥80 cm for women. NA, not applicable.
*P < 0.05.
Diagnosis of diabetes and treatment and control of blood glucose, blood pressure, and cholesterol in individuals with diabetes
Table 3 shows percentages of individuals with diabetes and concomitant hypertension or hypercholesterolemia that was diagnosed, treated, and controlled. There were favorable changes in the proportions of undiagnosed, treated, and controlled blood glucose, blood pressure, and serum cholesterol from 2004 to 2009 (all P < 0.05 for both sexes). However, all of the proportions of diagnosed, treated, and controlled metabolic traits remained low, especially among men. For example, two-thirds of men and more than one-half of women with diabetes and hypercholesterolemia were still undiagnosed for high blood cholesterol. Additional analysis for individuals with diabetes in 2009 found that 81.4% of all diabetic patients had LDL cholesterol ≥2.6 mmol/L or took cholesterol-lowering agents. Among those with diabetes and high LDL cholesterol, 66.7% were unaware that they had high LDL cholesterol (72.1% in men and 61.5% in women; P < 0.05), 7.0% were not treated (6.1% in men and 7.8% in women), and 17.2% were treated but did not have LDL cholesterol controlled to <2.6 mmol/L (14.4% in men and 19.9% in women), which left only 9.2% of all diabetic subjects with high LDL cholesterol controlled to <2.6 mmol/L (7.4% in men and 10.8% in women).
Table 3.
Percentages (SE) of undiagnosed diabetes, diagnosed but untreated diabetes, and controlled diabetes among Thai adults aged ≥20 years with diabetes and concomitants hypertension and hypercholesterolemia in 2004 and 2009
| Diabetes |
Hypertension |
High total cholesterol |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men |
Women |
Men |
Women |
Men |
Women |
|||||||
| 2004 | 2009 | 2004 | 2009 | 2004 | 2009 | 2004 | 2009 | 2004 | 2009 | 2004 | 2009 | |
| n | 1,824 | 895 | 2,439 | 1,177 | 1,100 | 562 | 1,447 | 709 | 1,095 | 555 | 1,744 | 925 |
| Undiagnosed | 66.5 (1.3) | 47.3 (1.8) | 51.4 (1.0) | 23.4 (1.2) | 65.6 (1.9) | 43.6 (2.2) | 55.2 (1.8) | 28.7 (1.8) | 85.0 (0.9) | 65.3 (2.1) | 86.6 (0.9) | 55.7 (1.2) |
| Diagnosed but not treated | 2.6 (0.5) | 5.6 (0.8) | 1.7 (0.2) | 1.9 (0.2) | 5.6 (0.7) | 7.9 (1.2) | 7.1 (0.8) | 2.6 (0.3) | 3.4 (0.4) | 5.8 (0.8) | 2.7 (0.4) | 8.5 (0.9) |
| Treated but not controlled | 23.2 (1.1) | 29.7 (1.4) | 31.2 (1.2) | 40.8 (1.0) | 25.4 (1.5) | 36.3 (1.5) | 31.3 (1.8) | 54.9 (1.7) | 7.6 (0.7) | 12.6 (1.1) | 7.0 (0.5) | 18.5 (0.7) |
| Treated and controlled | 7.7 (0.5) | 17.5 (1.1) | 15.8 (0.9) | 33.9 (0.9) | 3.4 (0.5) | 12.2 (1.6) | 6.4 (0.7) | 13.8 (1.0) | 4.0 (0.5) | 16.3 (1.3) | 3.8 (0.5) | 17.3 (1.0) |
Control target of diabetes is FPG < 7.2 mmol/L. Control target of high blood pressure is SBP/DBP <130/80 mmHg. Hypercholesterolemia: total cholesterol ≥5.2 mmol/L. Control target of high total cholesterol is <5.2 mmol/L.
CONCLUSIONS
Based on this study, 7.5% of Thai adults aged ≥20 years, an estimated 3.2 million people, had diabetes, of whom one-third was undiagnosed. Higher prevalence of diabetes was found in women, older individuals, and urban areas; however, undiagnosed diabetes as a proportion of all diabetes was higher in men and in those with less than a secondary school education. Compared with that in the previous study in 2004, the prevalence of total diabetes in 2009 increased slightly and diabetic subjects were more likely to be abdominally obese and have higher total cholesterol, particularly women. The proportion of individuals with diabetes that was diagnosed, treated, and controlled for blood glucose, blood pressure, and serum cholesterol improved in 2009; however, the proportion remained substantially low.
IFG and diabetes prevalence in this study are likely to remain underestimated, given that the diagnosis relied only on a single instance of FPG, history of physician diagnosis, and information on medication (9,10). A study of diabetes prevalence in the U.S. revealed that a 2-h glucose tolerance test could identify approximately twice the amount of undiagnosed diabetes prevalence than that detected by the FPG test (9). The prevalence found in this study was relatively comparable with that in other countries such as Sri Lanka, Malaysia, Hong Kong, Korea, China, and Japan (1,2,11) but lower than that in the U.S. (9). However, these comparisons should be interpreted with caution because of the variation among studies with regard to age ranges of study population, method of glucose measurements, year of study, and other environmental factors (1,2).
The improvement in rates of detection and control of diabetes and high blood pressure observed in the year 2009 might be due in part to the national screening campaign targeted at diabetes and hypertension by the Ministry of Public Health since 2006 (12). Another explanation could be the effect of improvement in health care accessibility since the implementation of universal health care coverage in 2002 to cover all Thai individuals who were not covered by the civil servant medical benefits and social security scheme (13,14). Despite the improvement, the high proportion of undiagnosed diabetes is of concern because these subjects were likely to have as poor or worse metabolic risk factors (dyslipidemia and obesity) as those diagnosed. The proportion of undiagnosed diabetes in this population was comparable with what was found in other studies (9,10), but proportions of diagnosis, treatment, and control of high blood pressure and hypercholesterolemia remained much lower than those of other countries (15). There were higher undiagnosed rates of hypercholesterolemia compared with high blood pressure and diabetes, perhaps because of the low availability of laboratory tests for serum cholesterol in primary care facilities. In Thailand, a substantial proportion of patients with diabetes was followed up at the primary care units and community hospitals, which had limited resources. For example, a lipid-lowering medicine was not generally available at the primary care settings. The finding of low treated and controlled rates may suggest that more efforts are needed to manage the conditions from the health care system, care providers, and patients in terms of adherence to treatment and behavior.
Men continued to suffer from higher rates of lack of diagnosis and lower rates of treatment and control of the conditions compared with women, and this suggests lower accessibility to early detection and management in men, particularly in rural areas. The disparity between the sexes has been consistently supported by a periodic national health and welfare survey conducted by the Thai National Health Statistics, reporting a lower rate of health care utilization in men than in women (16). This might be due to the fact that men had fewer health concerns compared with women or to other factors needing further investigation.
There are some limitations of the current study. First, we did not use the 2-h glucose tolerance test because the test was not feasible in the survey; hence, we might have underestimated diabetes prevalence. However, FPG is a reproducible, convenient, and inexpensive test, and it is still a practical choice in prevalence surveys in developing countries. Second, other lipid profiles such as HDL and LDL cholesterol and triglyceride were not available in the 2004 survey. Finally, long-term glycemic control measured by HbA1c was not measured. Despite the limitations, this study has strength as a nationally representative study with a large sample size and could provide a relatively good approximation of the country prevalence and trends. Future surveys should incorporate the glucose tolerance test in addition to FPG.
These findings serve as an example for other countries with similar rapid economic growth in establishing and sustaining a surveillance system for diabetes. The high prevalence of diabetes with higher proportions of obesity and dyslipidemia as well as suboptimal control of blood glucose, high blood pressure, and serum cholesterol signifies the burden imposed on the health system. Perhaps the increases in access to care and the population screening campaign could partly contribute to the improvement in detection and treatment of diabetes and its concomitants but only to a certain degree. Other determining factors concerning quality of care that require further investigation include the following: tracking systems, resource allocation, and the incentive and capacity of health care providers and patients. Allocation of screening tools and medication for diabetes and its concomitants, especially for hypercholesterolemia, should be implemented. Innovation to promote individuals with IFG and diabetes to maintain a healthy diet, physical exercise, and weight control is required.
Acknowledgments
NHES IV was conducted by the NHES Office, Health Systems Research Institute, Thailand. NHES IV was supported by the Health System Research Institute; the Bureau of Policy and Strategy, Ministry of Public Health; the Thai Health Promotion Foundation; and the National Health Security Office, Thailand.
No potential conflicts of interest relevant to this article were reported.
W.A. designed and managed the project and wrote the manuscript. S.C. collected data and reviewed and edited the manuscript. P.K. collected data and reviewed and edited the manuscript. R.S. collected data and reviewed and edited the manuscript. R.I. analyzed data. P.P. collected data and reviewed and edited the manuscript. S.T. collected data and reviewed and edited the manuscript. All of the authors participated in approving the final manuscript.
The authors thank Dr. Amnuay Thithapandha and Mr. John Wilson, Faculty of Medicine, Mahidol University, for their help in editing the manuscript.
APPENDIX
NHES IV Study Group includes the National Health Examination Survey Office: W.A., R.I., Jiraluck Nonthaluck, Supornsak Tipsukum, and Yawarat Porrapakkham.
Northern region: S.C., Kanittha Thaikla (Chiang Mai University), Wongsa Laohasiriwong, Wanlop Jaidee, Sutthinan Srathonghon, Ratana Phanphanit, Jiraporn Suwanteerangkul, and Kriangkai Srithanaviboonchai.
Northeastern region: P.K., Somdej Pinitsoontorn, Piyathida Kuhirunyaratn, Sauwanan Bumrerraj, Amornrat Rattanasiri, Suchada Paileeklee, Bangornsri Jindawong, Napaporn Krusun, and Weerapong Seeupalat (Khon Kaen University).
Southern region: Virasakdi Chongsuvivatwong, R.S., and Mafausis Dueravee (Prince of Songkla University).
Central region: S.T., Somrat Lertmaharit, Vilai Chinveschakitvanich, Onuma Zongram, Nuchanad Hounnaklang, and Sukarin Wimuktayon (Chulalongkorn University).
Bangkok region: P.P., Chalermsri Nuntawan, and Karn Chaladthanyagid (Mahidol University).
Footnotes
*A full list of members of the Thai National Health Examination Survey IV Study Group is available in the appendix.
References
- 1.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010;87:4–14 [DOI] [PubMed] [Google Scholar]
- 2.Chan JC, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 2009;301:2129–2140 [DOI] [PubMed] [Google Scholar]
- 3.Porapakkham Y, Rao C, Pattaraarchachai J, et al. Estimated causes of death in Thailand, 2005: implications for health policy. Popul Health Metr 2010;8:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aekplakorn W, Abbott-Klafter J, Premgamone A, et al. Prevalence and management of diabetes and associated risk factors by regions of Thailand: Third National Health Examination Survey 2004. Diabetes Care 2007;30:2007–2012 [DOI] [PubMed] [Google Scholar]
- 5.WHO Expert Committee on Physical Status. The Use and Interpretation of Anthropometry. Geneva, World Health Org., 1995 [PubMed] [Google Scholar]
- 6.Bonso E, Dorigatti F, Palatini P. Accuracy of the BP A100 blood pressure measuring device coupled with a single cuff with standard-size bladder over a wide range of arm circumferences. Blood Press Monit 2009;14:216–219 [DOI] [PubMed] [Google Scholar]
- 7.Pickering TG, Hall JE, Appel LJ, et al. ; Council on High Blood Pressure Research Professional and Public Education Subcommittee, American Heart Association. Recommendations for blood pressure measurement in humans: an AHA scientific statement from the Council on High Blood Pressure Research Professional and Public Education Subcommittee. J Clin Hypertens (Greenwich) 2005;7:102–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010;33(Suppl. 1):S62–S69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cowie CC, Rust KF, Ford ES, et al. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988-1994 and 2005-2006. Diabetes Care 2009;32:287–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang W, Lu J, Weng J, et al. ; China National Diabetes and Metabolic Disorders Study Group. Prevalence of diabetes among men and women in China. N Engl J Med 2010;362:1090–1101 [DOI] [PubMed] [Google Scholar]
- 11.Kim SM, Lee JS, Lee J, et al. Prevalence of diabetes and impaired fasting glucose in Korea: Korean National Health and Nutrition Survey 2001. Diabetes Care 2006;29:226–231 [DOI] [PubMed] [Google Scholar]
- 12.Clinical Practice Guidelines for Management of Diabetes 2008. Bangkok, Thailand, Diabetes Association of Thailand, Endocrine Society of Thailand and National Health Security Office, 2008
- 13.Prakongsai P, Limwattananon S, Tangcharoensathien V. The equity impact of the universal coverage policy: lessons from Thailand. Adv Health Econ Health Serv Res 2009;21:57–81 [PubMed] [Google Scholar]
- 14.Tangcharoensathien VS, Jongudomsuk P, Srithamrongswat S, Patcharanarumol W, Prakongsai P, Thammathataree J. Universal Coverage Scheme in Thailand: Equity Outcomes and Future Agendas to Meet Challenges, Health System Financing. World Health Report 2010, Background Paper 43. Geneva, World Health Org., 2010 [Google Scholar]
- 15.Gakidou E, Mallinger L, Abbott-Klafter J, et al. Management of diabetes and associated cardiovascular risk factors in seven countries: a comparison of data from national health examination surveys. Bull World Health Organ 2011;89:172–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.2004 Health and Welfare Survey Report. Bangkok, National Statistical Office, Ministry of Information and Communication Technology, 2004