Abstract
End-stage kidney disease (ESKD) patients on maintenance hemodialysis (MHD) have a lot of anxiety. Anxiety and coping are associated with the locus of control; the present investigation aimed to study the state and trait anxiety, locus of control, and active and passive coping among patients on MHD. Thirty MHD patients and 30 controls were administered State–Trait Anxiety Inventory, Rotter's Locus of Control Scale, and Coping Responses Inventory. There were significantly higher scores on state and trait anxiety, respectively (67.53 ± 10.89 vs. 59.40 ± 6.97, P < 0.01, and 62.97 ± 8.45 vs. 58.07 ± 7.06, P < 0.05), and locus of control (11.27 ± 3.55 vs. 9.04 ± 1.86, P < 0.01) in patients as compared to controls. On coping responses, patients and controls differed on positive reappraisal (54.33 ± 4.67 vs. 51.17 ± 3.12, P < 0.01), seeking guidance and support (58.07 ± 5.51 vs. 53.27 ± 4.22, P < 0.01), problem solving (51.03 ± 4.70 vs. 47.57 ± 4.73, P < 0.01), cognitive avoidance (60.27 ± 6.76 vs. 56.80 ± 4.08, P < 0.05), acceptance or resignation (61.67 ± 6.30 vs. 58.83 ± 4.23, P < 0.01), emotional discharge (68.07 ± 6.78 vs. 64.30 ± 4.50, P < 0.05), approach coping (205.57 ± 10.55 vs. 189.70 ± 11.37, P < 0.01), and avoidance coping (255.30 ± 16.45 vs. 241.10 ± 10.50, P < 0.01). A higher prevalence of anxiety trait could be the cause of anxiety in MHD patients besides the medical problems. The locus of control among patients though a mixed one was significantly more toward externalism. Thus, there is a need to identify this group well in advance and prepared not only medically but also psychologically for MHD.
Keywords: Coping responses, end-stage kidney disease, hemodialysis, locus of control, psyhchonephrology, state anxiety, trait anxiety
Introduction
Psychonephrology refers to the psychological problems and their management related with kidney disorders such as depression, anxiety, sexual problems, psychosis, problems in rehabilitation, maladjustment due to dependency, etc.[1] Recently, work on patients with renal diseases has advanced the understanding of the effect of the interaction of psychosocial and biological factors on the outcome.[1,2]
End-stage kidney disease (ESKD) is associated with depression and anxiety disorders.[3,4] Causes and effects of depression in ESKD patients with or without dialytic support have been addressed[5–7] but anxiety somehow has not received that much attention. Anxiety is a physiological and psychological state characterized by cognitive, somatic, emotional, and behavioral components. These components combine together to create the painful feeling that is typically recognized as uneasiness, apprehension, or worry. Anxiety is a normal reaction to stress but extreme anxiety is a problem in itself as it leads to mental health problems and reduced quality of life and subjective wellbeing.
Among ESKD patients undergoing hemodialysis, besides the disease itself, accompanying modifications in the occupational, marital, familial, societal, and personal life provide a sufficient base to give rise to anxiety. The effects of illness, dietary constraints, time restrictions, financial burdens, feeling of handicap, psychological strain of awareness of impending death, and many such factors impede the normal life and normal ways of coping. Therefore, it is highly relevant to study the patterns of these patients. No doubt the disease and associated problems lead to anxiety but it is quite possible that individuals with inherent trait anxiety are more vulnerable to this problem. If so this group needs to be identified well in advance and prepared not only medically but also psychologically for maintenance hemodialysis (MHD). This aspect of the anxiety trait has not been addressed so far.
Anxiety certainly is controlled by the locus of control. The locus of control refers to a center of perceived responsibility for one's behavior. Individuals with an internal locus of control believe that they can control events related to their life, whereas those with an external locus of control tend to believe that real power resides in forces outside themselves that determine their life. Generally, the internals show lesser anxiety.[8,9] Appropriate coping strategies are required to overcome the anxiety. Coping strategy is a behavior that helps one to function better in a given situation. Coping is the process of managing taxing circumstances, expanding efforts to solve personal and interpersonal problems, and seeking to master, minimize, reduce, or tolerate stress or conflict. Poorer the coping responses, more is the chance of having a higher level of anxiety. Coping is especially important in MHD patients as it is extremely difficult for patients to get used to dialysis machines and the associated therapy.[10] It is important to have positive cognitions and adopt deliberate behavioral efforts so as to enable a good quality of life for ESKD patients.
Keeping all the above-mentioned factors in mind, it seems highly relevant to study the accompanying anxiety, locus of control as well as the ways of coping in ESKD patients on MHD. This will help devising new ways of management of these patients thus adding to the applied side of psychonephrology. Therefore, the present study was undertaken to compare the state-trait anxiety, locus of control, and coping ways of ESKD patients on MHD and healthy controls.
Patients and Methods
Sample
A sample of 60 subjects which was divided into two groups was used for the study. The first group consisted of 30 patients of ESKD on MHD. The mean age of the subjects was 42.4 ± 9.86 (range 27–58 years) years. The mean duration of MHD was 6.2 ± 3.1 (range 3–11 months) months. Patients were on MHD in different dialysis centers (outpatient) on a twice weekly basis. The patients were being followed up regularly at Post Graduate Institute of Medical Sciences, Rohtak, India, a tertiary care center in North India. Only stable patients with no acute illness were recruited for the study. The following questionnaires were administered to patients on a nondialysis day. The second group comprised 30 healthy controls. The subjects in both the groups were matched on sociodemographic variables and cohort life events or stressors.
The following tools (questionnaires) were used in the study:
State–Trait Anxiety Inventory – Form Y[11]
Rotter's Locus of Control Scale[12]
Coping Responses Inventory by Moos.[13]
All the above questionnaires have been used and validated in Indian patients.
This scale is a self-evaluation questionnaire developed by Spielberger et al.[11] This inventory has been used extensively in research and clinical practice. The inventory is split into two scales: The State Anxiety scale and the Trait Anxiety scale each having 20 items. The State Anxiety scale (Form Y-1) evaluates “how respondents feel right now at this moment.” Each statement has four alternative responses, i.e., not at all, somewhat, moderately so, and very much so. The Trait Anxiety scale (Form Y-2) assesses “how people generally feel.” The responses are recorded on four-point scales, i.e., almost never, sometimes, often, and almost always. The score of state anxiety and trait anxiety was obtained with the help of a scoring procedure given in the manual. The level of anxiety is directly proportional to the score on both subscales of the inventory, i.e. higher the score, greater the anxiety. The subjects above the 75th percentile were considered to be very high on anxiety to calculate the prevalence.
Rotter's locus of control scale
The Hindi version of Rotter's locus of control scale was used.[12] The scale is a forced choice instrument which consists of 29 pairs of statements, 23 of which are scored and 6 filler items (not to be scored) from different life situations, where locus of control attitudes might be relevant to behavior. Each alternative is keyed as to a belief in either internal or external control of reinforcing event. The score is obtained with the help of the scoring key. A high score indicates a belief in an external locus of control on the internal–external dimension of score.
Coping Responses Inventory (adult form)
Coping Responses Inventory (CRI) has been prepared by Rudolf H. Moos. The Coping Responses Inventory – Adult form (CRI-Adults) measures eight different types of coping responses to stressful life circumstances. These responses are measured by eight scales – logical analysis (LA), positive reappraisal (PR), seeking guidance and support (SG), problem solving (PS), cognitive avoidance (CA), acceptance or resignation (AR), seeking alternative rewards (SR), and emotion discharge (ED). The inventory consists of two parts. Part 1 has 10 items related to the selection and description of a recent (focal) stressor. This part provides the information on how the individual appraises the focal stressor and its outcome. Part 2 consists of 48 items related with the behaviors of a person often engaged to deal with problems or stressful life circumstances. The responses are obtained on a four-point scale varying from “not at all” to “fairly often.” The first set of four scales, i.e., LA, PR, SG, and PS measures approach coping responses. The second set of scales namely CA, AR, SR, and ED measures avoidance coping responses. The first two scales in each set measure cognitive coping strategies, the third and fourth scales in each set measure behavior coping. In general, approach coping is problem focused; it reflects cognitive and behavioral efforts to resolve life stressors. In contrast, avoidance coping tends to be emotion focused; it reflects cognitive and behavioral attempts to avoid thinking about a stressor and its implication or to manage the effect associated with it. The score for each coping strategy is obtained with the help of a scoring procedure mentioned in the manual. Higher scores of each coping scale indicate the greater use of the coping strategy.
Analysis of data was carried out by employing the statistical method of chi-square and t-test.
Results
The prevalence of state and trait anxiety was higher among the patients as compared to the healthy controls. State anxiety was seen in 26 patients (87%) and in 19 (63%) healthy controls (χ2 = 1.09, P > 0.05) while trait anxiety was significantly higher in 22 patients (73%) as compared to 10 (33%) healthy controls (χ2 = 4.50, P < 0.05). Further, the scores of both the state and the trait anxiety were significantly higher among the patients in comparison to the healthy controls when tested by employing t for uncorrelated means [Table 1].
Table 1.
Scores of the state and trait anxiety and locus of control in MHD patients and healthy controls
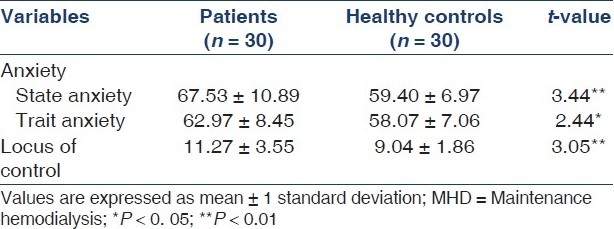
The score of locus of control of patients was significantly higher than the healthy controls [Table 1]. Comparison with the means in the norm table shows that this was an average score. So both types of subjects had a mixed locus of control. However, a higher score of the patients shows that they were more toward externalism, in their mixed locus of control.
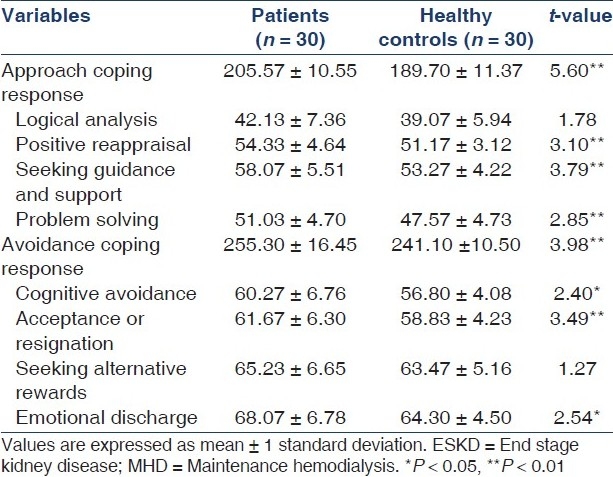
The scores of coping responses on various types of coping have been indicated in Table 2. Both the approach and the avoidance coping significantly increased in the patient group. Except for logical analysis which is a cognitive approach coping response and seeking alternatives rewards which is a behavioral response on avoidance coping, all other types of coping responses were significantly higher among the patients as compared to the healthy controls.
Table 2.
Scores of coping responses inventory of ESKD in MHD patients and healthy controls
Discussion
The level of anxiety in MHD patients has been observed to be as high as 69.3% by Squalli et al.[14] and 85.1% by Dumitrescu et al.[15] The disease, particularly a chronic one has been associated with add-on stress. The associated psychological and sociological factors add to the stress in addition to the underlying chronic disease. A number of psychosocial problems like loss of freedom due to dependency on machine,[16] marital and social adjustment problems, deterioration in psychomotor performances, mental functions and perceptual performances add on to lead to an anxiety state.[5–7,17]
In the present study, the anxiety state was seen in 87% of patients but an important observation was that there was a significantly higher trait anxiety among the patients. This indicates that the basic nature of having anxiety as a trait could be a major underlying factor for this suffering among the patients. Tanaka et al.[18] found that the state and trait anxieties were more closely related to somatic factors than to social factors. On the other hand, Novakovic[19] observed that anxiety may be independent, somatized as a part of another mental disorder, or reinforced by a cognitive damage. The results of the present study point out that anxiety may not be entirely due to the underlying disease but it could be the result of the anxiety trait which these patients had. So the implication of these results from the view point of psychonephrology lies in identifying this subgroup and preparing training them well in advance before the initiation of MHD to minimize anxiety. Such patients need to be taught to perform relaxation exercises both as preventive and therapeutic measures. Cognitive behavior therapeutic techniques can also be used.[17]
Regarding the locus of control in this study, it was observed that the patients were significantly more toward externalism in comparison to the healthy controls. The patients had to undergo hemodialysis for their treatment in order to manage the disability caused by ESKD. The treatment including hemodialysis is a successful scientific management which is full of decision taking and adoption of other health care behavior on the part of patients, which should lead these subjects to develop faith in their own efforts. But this does not seem to be so. The subjects turned toward externalism, i.e., a dependence-type locus of control. Two reasons seem to be valid for this. First, as they are totally dependent upon others like family, doctors, medicines, dialysis staff, and machine, so a feeling of “loss of freedom” emerges.[20] Second, the religious and spiritual coping is the most common way of coping in all kinds of problems whether disease related or others. Burns[21] found that turning toward God was the most frequently identified strategy for physical and psychosocial adaptation among hemodialysis patients. That is how the locus of control of the patients might have turned to be external from the mixed locus of control. The anxiety is more among those with an external locus of control. Patients on hemodialysis with an internal locus of control (independent) adjust and adapt better than those with an external locus of control.[22] Their compliance with diet, acceptance for limitations, and vocational adjustments as well as coping in terms of seeking information and adopting an active, problem-solving attitude has been found to be better.[22] Cvengros et al.[6] also suggested that the internal health locus of control over time may be a particularly important determinant of adjustment for individuals with chronic illnesses.
In chronic diseases, the patients generally show lesser approach coping and more avoidance coping. In patients of rheumatoid arthritis, as the anxiety level increased with more functional disability, there was more avoidance coping.[23] In this study, the patients on MHD had both approach and the avoidance coping responses. Among the approach coping responses, positive reappraisal was significantly higher among the patients. It meant that the patients made more cognitive attempts to look at the problem in a positive way and could reframe their problem for better adjustment. Greater use of reappraisal was found to be significantly associated with lower levels of anxiety.[24] Similarly, seeking guidance and support and problem solving were higher in patients, implying that patients made more behavioral attempts to seek information, guidance, or support as well as could take prompt actions, to deal directly with the problem. Yeh and Chu[25] also found more social support seeking among such patients. Although the patients had predominantly an external locus of control (dependency on others) but still the approach coping responses were good.
Among the avoidance coping responses, cognitive avoidance as well as acceptance or resignation were significantly higher in the patient groups. The cognitive avoidance or the deliberate attempts to avoid thinking realistically about the problem is also thought to be a good attempt on the part of the patients. Investigators find it similar to the “minimization” of problem which certainly is a positive and helping coping response. Denial is an effective coping style against negative emotions, but the drawback is that it can diminish compliance.[26]
In chronic illnesses, it is important to develop behavioral attempts to involve patients in substitute activities by seeking alternative rewards. This would help them in getting new sources of satisfaction, and enhance the effectiveness of dealing with various problems in personal, familial, societal, and occupational disturbances. However, such tendencies are less in those with an external locus of control which was there in patients in the present study.
This study has a drawback of a small sample size, and secondly, patients were on twice a week MHD, thus bringing in manifestations of inadequate dialysis which has an influence on psychological aspects. Despite these drawbacks, the study points toward the fact that MHD patients have to be managed not only medically but also psychologically. Some of the behaviors have to be changed and the patients have to play an active role in their management. Intervention to enhance logical analysis, i.e., the cognitive attempts to understand and prepare mentally for a stressor and its consequences, needs to be put in practice much before the initiation of MHD.
Conclusion
To conclude, a higher prevalence of the anxiety trait could be the cause of anxiety in MHD patients besides the medical problems. The locus of control among patients though a mixed one was significantly more toward externalism. Thus there is a need to identify this group well in advance and prepare the patients not only medically but also psychologically for MHD. It is recommended that there is a need to design intervention for dealing with state anxiety as a help after the disease and trait anxiety even before the disease. Similarly, strategies need to be designed for improving coping strategies like logical analysis capacity and seeking alternative rewards at the cognitive and behavioral level, respectively, in order to enhance the psychological and social rehabilitation, among ESKD patients on MHD.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Levy NB. What is psychonephrology? J Nephrol. 2008;21:S51–3. [PubMed] [Google Scholar]
- 2.Kimmel PL. Depression in patients with chronic renal disease: What we know and what we need to know. J Psychosom Res. 2002;53:951–6. doi: 10.1016/s0022-3999(02)00310-0. [DOI] [PubMed] [Google Scholar]
- 3.Cukor D, Peterson RA, Cohen SD, Kimmel PL. Depression in end-stage renal disease hemodialysis patients. Nat Clin Pract Nephrol. 2006;2:678–87. doi: 10.1038/ncpneph0359. [DOI] [PubMed] [Google Scholar]
- 4.Cukor D, Cohen SD, Peterson RA, Kimmel PL. Psychosocial aspects of chronic disease: ESRD as a paradigmatic illness. J Am Soc Nephrol. 2007;18:3042–55. doi: 10.1681/ASN.2007030345. [DOI] [PubMed] [Google Scholar]
- 5.Kimmel PL, Peterson RA. Depression in patients with end-stage renal disease treated with dialysis: Has the time to treat arrived? Clin J Am Soc Nephrol. 2006;1:349–52. doi: 10.2215/CJN.00890306. [DOI] [PubMed] [Google Scholar]
- 6.Cvengros JA, Christensen AJ, Lawton WJ. Health locus of control and depression in chronic kidney disease: A dynamic perspective. J Health Psychol. 2005;10:677–86. doi: 10.1177/1359105305055320. [DOI] [PubMed] [Google Scholar]
- 7.Sousa AD. Psychiatric issues in renal failure and dialysis. Ind J Nephrol. 2008;18:47–50. doi: 10.4103/0971-4065.42337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meijer SA, Sinnema G, Bijstra JO, Mellenbergh GJ, Wolters WHG. Coping styles and locus of control as predictors for psychological adjustment of adolescents with a chronic illness. Soc Sci Med. 2002;54:1453–1461. doi: 10.1016/s0277-9536(01)00127-7. [DOI] [PubMed] [Google Scholar]
- 9.Dunn K, Elsom S, Cross W. Self efficacy and locus of control affect management of aggression by mental health nurses. Issues in Ment Health Nurs. 2007;28:201–17. doi: 10.1080/01612840601096321. [DOI] [PubMed] [Google Scholar]
- 10.Logan SM, Pelletier HM, Hodgins M. Stressors and coping of in-hospital haemodialysis patients aged 65 years over. J Adv Nurs. 2006;54:382–91. doi: 10.1111/j.1365-2648.2006.04015.x. [DOI] [PubMed] [Google Scholar]
- 11.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory (Form Y) Palo Alto, CA: Consulting Psychologist Press; 1983. [Google Scholar]
- 12.Kumar A, Srivastava SN. Manual for Hindi Version of Rotter's Locus of Control Scale. Varanasi: Kumar Publications; 1985. [Google Scholar]
- 13.Moos RH. Coping Responses Inventory (Adult Form) Professional Manual. Odessa: Florida Psychological Assessment Resources, Inc; 1993. [Google Scholar]
- 14.Sqalli-Houssaini T, Ramouz I, Fahi Z, Tahiri A, Sekkat FZ, Ouzeddoun N, et al. Effects of anxiety and depression on haemodialysis adequacy. Nephrol Ther. 2005;1:31–7. doi: 10.1016/j.nephro.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 15.Dumitrescu AL, Gârneaţă L, Guzun O. Anxiety, stress, depression, oral health status and behaviours in Romanian hemodialysis patients. Rom J Intern Med. 2009;47:161–8. [PubMed] [Google Scholar]
- 16.Kohli S, Aggarwal HK. Psychological aspects of end-stage renal disease patients on maintenance hemodialysis. Ind J Nephrol. 2007;16:15–8. doi: 10.4103/0971-4065.83729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cukor D, Coplan J, Brown C, Friedman S, Cromwell-Smith A, Peterson RA, et al. Depression and anxiety in urban hemodialysis patients. Clin J Am Soc Nephrol. 2007;2:484–90. doi: 10.2215/CJN.00040107. [DOI] [PubMed] [Google Scholar]
- 18.Tanaka K, Morimoto N, Tashiro N, Hori K, Katafuchi R, Fujimi S. The features of psychological problems and their significance in patients on hemodialysis- with reference to social and somatic factors. Clin Nephrol. 1999;51:161–76. [PubMed] [Google Scholar]
- 19.Novakovik M. Anxiety disorders in dialysis patients. Med Pregl. 2007;60:484–8. doi: 10.2298/mpns0710484n. [DOI] [PubMed] [Google Scholar]
- 20.Hagren B, Petterson IM, Severinsson F, Lutzen K, Clyne N. The haemodialysis machine is a lifeline: Experiences of suffering from end-stage renal disease. J Adv Nurs. 2001;34:196–202. doi: 10.1046/j.1365-2648.2001.01745.x. [DOI] [PubMed] [Google Scholar]
- 21.Burns B. Physical and psychological adaption of blacks on hemodialysis. App Nurse Res. 2004;17:116–24. doi: 10.1016/j.apnr.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 22.Poll IB, De Nour AK. Locus of control adjustment to chornic haemodialysis. Psychol Med. 1980;10:153–7. doi: 10.1017/s0033291700039696. [DOI] [PubMed] [Google Scholar]
- 23.Scharloo M, Kapatein AA, Weinman JA, Haze JM, Breedveld FC, Rooijman HG. Predicting functional status in patient with rheumatoid arthritis. J Rheumatol. 1999;26:1686–93. [PubMed] [Google Scholar]
- 24.Gillanders S, Wild M, Deighan C, Gillanders D. Emotion regulation, affect, psychosocial functioning and well being in hemodialysis patient. Am J Kid Dis. 2008;51:651–62. doi: 10.1053/j.ajkd.2007.12.023. [DOI] [PubMed] [Google Scholar]
- 25.Yeh SC, Chou HC. Coping strategies and stressors in patients with hemodialysis. Psychosom Med. 2007;69:182–90. doi: 10.1097/PSY.0b013e318031cdcc. [DOI] [PubMed] [Google Scholar]
- 26.Jadoulle V, Havois P, Jadoul M. Anxity and depression in chronic hemodialysis: Some somotopsychic determinants. Clin Nephrol. 2005;63:113–8. doi: 10.5414/cnp63113. [DOI] [PubMed] [Google Scholar]


