Abstract
Peritoneal dialysis (PD) related peritonitis caused by fungi is a potentially life-threatening complication. It diminishes prospects of continuing PD. We report a patient with Aspergillus terreus peritonitis treated successfully with catheter removal and antifungal therapy and subsequently had a live-related renal transplantation. There was no recurrence of the infection in 3 years of follow-up.
Keywords: Aspergillus terreus, peritonitis, transplantation
Introduction
Peritonitis is the most important and common of complications of peritoneal dialysis (PD).[1] While the episodes of PD peritonitis are predominantly due to bacteria, fungi may be the causative organisms in up to 15% of cases.[2] PD fungal peritonitis is associated with an increased mortality[3,4] with reports of up to 53%[5] in some centers making early diagnosis and treatment a necessity. We report a patient with PD peritonitis due to Aspergillus terreus which was treated successfully with antifungal therapy and catheter removal and subsequently underwent a renal transplantation. This is the first case of a successful renal transplantation after treatment of A. terreus peritonitis.
Case Report
A 61-year-old man, presented to the nephrology services at Christian Medical College Vellore, with chronic kidney disease stage 5 (CKD 5) and hypertension diagnosed 4 months ago. He had been on continuous ambulatory peritoneal dialysis (CAPD) since then. Immediately prior to his presentation, he had abdominal pain with a cloudy effluent and was diagnosed elsewhere to be having peritonitis. He was treated with intraperitoneal (IP) cefotaxime 250 mg in each of three exchanges for 7 days. As there was no resolution of the peritoneal fluid leucocytosis, IP vancomycin 2 gm followed by daily IP cefazolin 1 gm and ceftazidime 1 gram were instilled intraperitoneally to treat as for a culture-negative peritonitis.
Upon evaluation he was found to have a cloudy PD effluent. The PD fluid cell count was 1540/mm3 with 80% polymorphs and 20% lymphocytes on smear. The PD cultures were negative on two occasions. The antibiotics were upgraded to IP vancomycin (1000 mg loading dose and 25 mg per liter) and ceftazidime (500 mg loading dose and 125mg per liter) in each of his four exchanges. There was an initial decrease in the leukocytosis to 60/mm3 within 7 days. The cultures of the effluent, however, grew A. terreus and the PD fluid leucocyte count increased subsequently to 260/mm3 with 82% polymorphs, 15% lymphocytes and 3% eosinophils.
He was treated with intravenous amphotericin for 2 weeks (cumulative dose of 700 mg) followed by 2 weeks of oral fluconazole 200 mg twice daily. Oral flucytosine 500 mg was given concomitantly for 4 weeks. The PD catheter was removed and the patient was started on hemodialysis (HD). He improved with no recurrence of abdominal pain or ascites.
The patient was on thrice-weekly hemodialysis for 3 months, and had no recurrence of abdominal pain or fever. A repeat ultrasonography did not show any ascites, and the C-reactive protein (CRP) was negative. At this time, he underwent a living donor renal transplantation from his son. There were no obvious adhesions. He was maintained on prednisolone, cyclosporine and azathioprine after transplantation. This regimen was changed with substitution of everolimus for cyclosporine after 6 months when he was diagnosed to be having Kaposi's sarcoma of the hard palate with which the Kaposi's sarcoma resolved. Over a subsequent 3 years follow-up, there had been no recurrence of peritonitis or any other fungal infection. This is the first reported case of successful renal transplantation soon after treatment of Aspergillus PD peritonitis.
Discussion
As a modality of renal replacement therapy, the use of PD has been varied depending on the population. Peritonitis is perhaps the most common complication of PD and definitely the most important.[1] Fungal PD peritonitis having an increased mortality and poor technique survival (up to 40%)[2,5] mandates early diagnosis and therapy. Early initiation of therapy is imperative and it aims at eradicating the infection as well as preserving the peritoneum with a view of returning to this modality of renal replacement therapy. The treatment of fungal PD peritonitis involves removal of PD catheter[2,6,7] and treatment with antifungal agents for 4-6 weeks[8] and the catheter may be reimplanted after 4-6 weeks of removal[5,9] as the catheter may be colonized with fungi even without clinical peritonitis.[5] Immediate PD catheter insertion prior to adequate antifungal therapy may result in recolonization of the new PD catheter.[10] The 2000 International Society of Peritoneal Dialysis guidelines on management of PD peritonitis, discussed the option of treatment of fungal infection without catheter removal[8]. The view has been since revised (2005) to recommend mandatory catheter removal.[7] Other antifungal agents like the newer azoles and echinocandins have also being used successfully.[11–13] Where the infection seems resistant to the antifungal agent used, an addition of a second antifungal like Caspofungin may be prudent as was described by Fourtounas et al.[14] Three factors appeared to predict mortality: the presence of non-Candida species, the catheter being left in situ and a serum albumin level < 3 g/dl with multivariate analysis showing the latter two as predictors of mortality.[15] This paper reports one patient (4%) having had a successful renal transplantation after treatment of fungal PD peritonitis.
A. terreus is a ubiquitous fungus. Found widely in the environment, it is a rare human pathogen.[5,16] On culturing the fluid in sabouraud dextrose agar, A. terreus is a rapid grower; the obverse is flat, granular and cinnamon brown and the reverse is brown [Figures 1 and 2]. On microscopy with lactophenol cotton blue preparation, septate hyphae, dome-shaped vesicles with long cylindrical metulae and phialides on upper two-thirds are seen [Figure 3].
Figure 1.

Aspergillus terreus – obverse
Figure 2.

Aspergillus terreus – reverse
Figure 3.
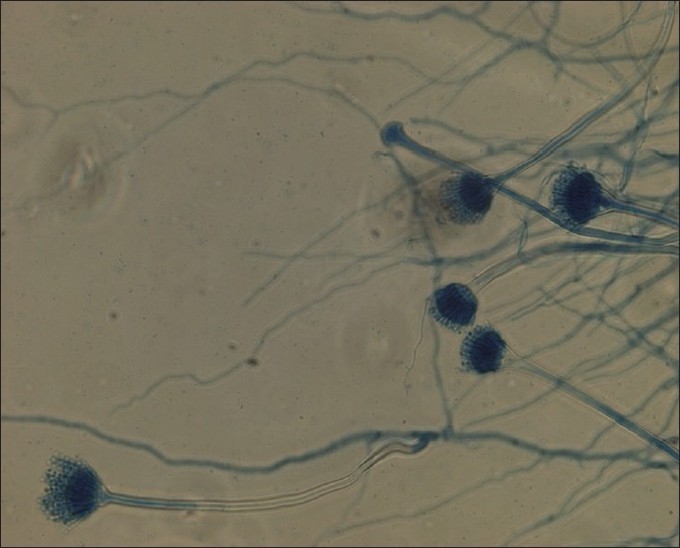
Aspergillus terreus – microscopy
There have been reports of development of resistance of A. terreus to amphotericin.[17,18] The antifungal therapy must be modified according to the sensitivity pattern and the initial drug of choice should be amphotericin unless there is known increased resistance to the drug prevalent in the area. In fact, the current Infectious Diseases Society of America (IDSA) recommends that an antifungal triazole be used instead of amphotericin as the primary agent of choice.[19] A. terreus has been reported thrice before to have caused PD peritonitis.[17,20,21] In all these cases, the patients succumbed to their infection despite removal of the catheter and antifungal therapy.
Renal transplantation is a state of heightened immunosuppression more than CKD. The usual policy for considering renal transplantation in a patient after PD peritonitis is to observe him for 2 weeks following the discontinuation of antibiotics. If no relapse occurs, he may be planned for transplantation.[22] We considered the patient to have cleared the infection after treatment and observation. Normal CRP indicated absence of inflammation and the patient was clinically well to receive a transplant roughly at a time when CAPD would have normally resumed with catheter reinsertion. The CRP usually rises about 48 hours after the onset of peritonitis and returns to normal within 4 weeks of initiating therapy.[23] In a third of patients in whom the CRP does not decline, there is a risk of recurrent peritonitis. The timing of the transplantation surgery was again extrapolated from the period of returning to PD for continued renal replacement therapy in other patients with Aspergillus peritonitis. However, most patients who had PD peritonitis due to Aspergillus who survived the infection had maintained on HD.[24] This patient has had no recurrence of his peritonitis in the 3 years of post-transplant follow-up.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Holley HL, Piraino BM. Complications of peritoneal dialysis: Diagnosis and management. Semin Dial. 1990;3:245–8. [Google Scholar]
- 2.Prasad KN, Prasad N, Gupta A, Sharma RK, Verma AK, Ayyagari A. Fungal peritonitis in patients on continuous ambulatory peritoneal dialysis: a single centre Indian experience. J Infect. 2004;48:96–101. doi: 10.1016/s0163-4453(03)00119-1. [DOI] [PubMed] [Google Scholar]
- 3.Eisenberg ES, Leviton I, Soeiro R. Fungal peritonitis in patients receiving peritoneal dialysis: experience with 11patients and review of the literature. Rev Infect Dis. 1986;8:309–21. doi: 10.1093/clinids/8.3.309. [DOI] [PubMed] [Google Scholar]
- 4.Michel C, Courdavault L, al Khayat R, Viron B, Roux P, Mignon F. Fungal peritonitis in patients on peritoneal dialysis. Am J Nephrol. 1994;14:113–20. doi: 10.1159/000168699. [DOI] [PubMed] [Google Scholar]
- 5.Prasad N, Gupta A. Fungal peritonitis in peritoneal dialysis patients. Perit Dial Int. 2005;25:207–22. [PubMed] [Google Scholar]
- 6.Wang AY, Yu AW, Li PK, Lam PK, Leung CB, Lai KN, et al. Factors predicting outcome of fungal peritonitis in peritoneal dialysis: analysis of a 9-year experience of fungal peritonitis in a single center. Am J Kidney Dis. 2000;36:1183–92. doi: 10.1053/ajkd.2000.19833. [DOI] [PubMed] [Google Scholar]
- 7.Piraino B, Bailie RG, Bernardini J, Boeschoten E, Gupta A, Holmes C, et al. Peritoneal dialysis-related infections recommendations: 2005 update. Perit Dial Int. 2005;25:107–31. [PubMed] [Google Scholar]
- 8.Keane WF, Bailie RG, Boeschoten E, Gokal R, Golper TA, Holmes CJ, et al. Adult peritoneal dialysis-related peritonitis treatment recommendations: 2000 update. Perit Dial Int. 2000;20:396–411. [PubMed] [Google Scholar]
- 9.Sugar AM. Antifungal therapy in CAPD peritonitis-do we have a choice? Semin Dial. 1991;4:145–6. [Google Scholar]
- 10.Kerr CM, Perfect JR, Craven PC, Jorgensen JH, Drutz DJ, Shelburne JD, et al. Fungal peritonitis in patients on continuous ambulatory peritoneal dialysis. Ann Intern Med. 1983;99:334–6. doi: 10.7326/0003-4819-99-3-334. [DOI] [PubMed] [Google Scholar]
- 11.Pimentel JD, Dreyer G, Lum GD. Peritonitis due to Cunninghamella bertholletiae in a patient undergoing continuous ambulatory peritoneal dialysis. J Med Microbiol. 2006;55:115–8. doi: 10.1099/jmm.0.46202-0. [DOI] [PubMed] [Google Scholar]
- 12.Sedlacek M, Cotter JG, Suriawinata AA, Kaneko TM, Zuckerman RA, Parsonnet J, et al. Mucormycosis peritonitis: more than 2 years of disease-free follow-up after posaconazole salvage therapy after failure of liposomal amphotericin B. Am J Kidney Dis. 2008;51:302–6. doi: 10.1053/j.ajkd.2007.09.026. [DOI] [PubMed] [Google Scholar]
- 13.Hashimoto H, Moriya R, Kamata K, Higashihara M, Yoshida K, Kume H. Successful treatment with micafungin (MCFG) of severe peritonitis due to Candida parapsilosis with chronic renal failure patient on hemodialysis [Japanese] Kansenshogaku Zasshi. 2005;79:195–200. doi: 10.11150/kansenshogakuzasshi1970.79.195. [DOI] [PubMed] [Google Scholar]
- 14.Fourtounas C, Marangos M, Kalliakmani P, Savidaki E, Goumenos DS, Vlachojannis JG. Treatment of peritoneal dialysis related fungal peritonitis with caspofungin plus amphotericin B combination therapy. Nephrol Dial Transplant. 2006;21:236–7. doi: 10.1093/ndt/gfi162. [DOI] [PubMed] [Google Scholar]
- 15.Ram R, Swarnalatha G, Neela P, Murty KV. Fungal peritonitis in patients on continuous ambulatory peritoneal dialysis: A single-centre experience in India. Nephron Clin Pract. 2008;110:207–12. doi: 10.1159/000167867. [DOI] [PubMed] [Google Scholar]
- 16.Kalishian Y, Miller EB, Kagan A, Landau Z. Aspergillus terreus peritonitis in a CAPD patient: report of a case. Perit Dial Int. 2004;24:93. [PubMed] [Google Scholar]
- 17.Sutton DA, Sanche SE, Revankar SG, Fothergill AW, Rinaldi MG. In vitro amphotericin B resistance in clinical isolates of Aspergillus terreus, with a head-to-head comparison to voriconazole. J Clin Microbiol. 1999;37:2343–5. doi: 10.1128/jcm.37.7.2343-2345.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hachem RY, Kontoyiannis DP, Boktour MR, Afif C, Cooksley C, Bodey GP, et al. Aspergillus terreus: an emerging amphotericin B-resistant opportunistic mold in patients with hematologic malignancies. Cancer. 2004;101:1594–600. doi: 10.1002/cncr.20554. [DOI] [PubMed] [Google Scholar]
- 19.Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, et al. Treatment of aspergillosis: Clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008;46:327–60. doi: 10.1086/525258. [DOI] [PubMed] [Google Scholar]
- 20.Nannini EC, Paphitou NI, Ostrosky-Zeichner L. Peritonitis due to Aspergillus and zygomycetes in patients undergoing peritoneal dialysis: report of 2 cases and review of the literature. Diagn Microbiol Infect Dis. 2003;46:49–54. doi: 10.1016/s0732-8893(02)00554-0. [DOI] [PubMed] [Google Scholar]
- 21.Verghese S, Palani R, Thirunavakarasu N, Chellamma T, Pathipata P. Peritonitis due to Aspergillus terreus in a patient undergoing continuous ambulatory peritoneal dialysis. Mycoses. 2008;51:174–6. doi: 10.1111/j.1439-0507.2007.01465.x. [DOI] [PubMed] [Google Scholar]
- 22.Teitelbaum I, Mehrotra R, Golper TA, Burkart JM. In: Diseases of the kidney and the urinary tract. 8th ed. Schrier RW, editor. London, United Kingdom: Lippincott Williams and Wilkins; p. 2637. [Google Scholar]
- 23.Troidle L, Gorban-Brennan N, Kliger A, Finkelstein FO. Continuous peritoneal dialysis-associated peritonitis: a review and current concepts. Semin Dial. 2003;16:428–37. doi: 10.1046/j.1525-139x.2003.16095.x. [DOI] [PubMed] [Google Scholar]
- 24.Nannini EC, Paphitou NI, Ostrosky-Zeichner L. Peritonitis due to Aspergillus and zygomycetes in patients undergoing peritoneal dialysis: report of 2 cases and review of the literature. Diagn Microbiol Infect Dis. 2003;46:49–54. doi: 10.1016/s0732-8893(02)00554-0. [DOI] [PubMed] [Google Scholar]


