Abstract
Pregabalin is a gamma-amino-butyric acid analog shown to be effective in several models of neuropathic pain, incisional injury, and inflammatory injury. In this review, the role of pregabalin in acute postoperative pain and in chronic pain syndromes has been discussed. Multimodal perioperative analgesia with the use of gabapentinoids has become common. Based on available evidence from randomized controlled trials and meta-analysis, the perioperative administration of pregabalin reduces opioid consumption and opioid-related adverse effects in the first 24 h following surgery. Postoperative pain intensity is however not consistently reduced by pregabalin. Adverse effects like visual disturbance, sedation, dizziness, and headache are associated with higher doses. The advantage of the perioperative use of pregabalin is so far limited to laparoscopic, gynecological, and daycare surgeries which are not very painful. The role of the perioperative administration of pregabalin in preventing chronic pain following surgery, its efficacy in more painful surgeries and surgeries done under regional anesthesia, and the optimal dosage and duration of perioperative pregabalin need to be studied. The efficacy of pregabalin in chronic pain conditions like painful diabetic neuropathy, postherpetic neuralgia, central neuropathic pain, and fibromyalgia has been demonstrated.
Keywords: Acute perioperative pain, chronic pain syndromes, pregabalin
Introduction
Pregabalin is a lipophilic gamma-amino-butyric acid (GABA) analog with anticonvulsant, anxiolytic and sleep-modulating properties. As a successor of gabapentin, pregabalin was shown to be effective in several models of neuropathic pain,[1–3] incisional injury,[4] and inflammatory injury.[5,6] Gabapentin has been found to reduce pain intensity, opioid consumption, and opioid-related adverse effects after surgery.[7,8] However, compared to gabapentin, pregabalin is more rapidly absorbed (1 h vs. 3–4 h) and has higher bioavailability (90% vs. 33–66%).[9–11] The absorption of gabapentin is saturable, whereas the absorption of pregabalin increases with the increasing dose resulting in linear kinetics. Pregabalin requires less frequent daily dosing and has been shown to provide equivalent efficacy to gabapentin at much lower doses, thereby promising less dose-related adverse effects.[12–14] Pregabalin is a 3–10 times more potent antiepileptic and 2–4 times more potent analgesic than gabapentin.[15,16]
Mechanism of action
The mechanism of action of pregabalin is similar to gabapentin. It binds to the α2-δ subunit of presynaptic, voltage-dependent calcium channels that are widely distributed throughout the central and peripheral nervous system.[17–20] Pregabalin binds to the α2-δ subunit six times more potently than gabapentin[21] and thereby reduces the release of several neurotransmitters like glutamate, norepinephrine, serotonin, dopamine, and substance P.[22–27] As with gabapentin, pregabalin is inactive at GABAA and GABAB receptors, is not metabolically converted into GABA, and does not alter the GABA uptake or degradation.[28–30]
Pharmacology
Pregabalin is available as 50, 75, 100, 150, 200, 225, and 300 mg tablets. Average daily dosing ranges from 50 to 600 mg/day. The elimination half-life is 5.5–6.7 h independent of dose and repeated administration. It does not undergo hepatic metabolism and is not bound to plasma proteins. Nearly 98% of the absorbed dose is excreted unchanged in urine. Pregabalin elimination is nearly proportional to creatinine clearance (CLcr) and 50% reduction in the daily dose is recommended for patients with CLcr < 60 ml/min.[31]
Side effects
Pregabalin is generally well tolerated[32] and associated with transient mild to moderate adverse effects which are dose dependent. Dizziness and somnolence are most frequently reported (22–29%). Other less common adverse effects are dry mouth, peripheral edema, blurred vision, weight gain, and inability to concentrate.
Pregabalin in acute postoperative pain
The multimodal analgesic technique is commonly used for acute postperative pain and it is based on judicious use of opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), paracetamol, small dose ketamine, and regional blocks with local anesthetics. Opioid use is associated with nausea, vomiting, pruritus, urinary retention, and rarely respiratory depression.[33] Regional analgesia techniques require additional intervention and have the potential risk of complications. NSAIDs can lead to gastrointestinal bleeding, renal toxicity, thromboembolic complications while ketamine is psychotogenic. The quest for an ideal drug is ongoing and a drug which has opioid-sparing analgesic effect, an anxiolytic property without the adverse effects of traditional analgesics mentioned, can be an attractive adjuvant for acute perioperative analgesia.[8]
The sensitization of dorsal horn neurons has been demonstrated in acute pain models[34,35] and possibly plays a role in the development of chronic pain after surgery.[36,37] By reducing the hyperexcitability of dorsal horn neurons induced by tissue damage, pregabalin may have a role in postoperative pain management.[38–40] The anxiolytic effect of pregabalin and its ability to prevent opioid tolerance may be beneficial.[41,42]
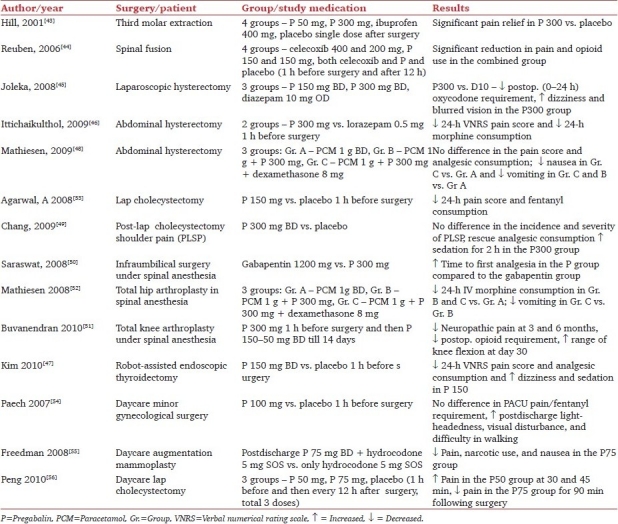
A total of 14 randomized controlled trials (RCTs), which included the use of pregabalin in the setting of a heterogenous group of surgeries performed under general anesthesia, spinal anesthesia, or daycare surgery were evaluated. The doses of pregabalin used ranged from 50 to 600 mg/day. Salient features of studies involving pregabalin in acute pain are tabulated as Table 1. Studies reviewed have been grouped as those using pregabalin ≥300 mg/day and those using <300 mg/day, for ease of discussion.
Table 1.
Studies involving pregabalin in acute pain
Studies using pregabalin ≥300 mg/day
In a double-blind RCT, pregabalin 50 and 300 mg were compared with placebo and 400 mg of ibuprofen. Study drugs were administered postoperatively to patients after the removal of impacted mandibular molar teeth. Statistically significant differences were observed in pain relief, pain intensity difference, and pain relief intensity difference between the 300-mg pregabalin group and placebo. In the 300-mg pregabalin group, the duration of analgesia was longer than the ibuprofen group and the patients had the highest score on the patient global impression of study medication. However, adverse effects, most commonly dizziness, somnolence, and vomiting, were reported in 48% patients in the pregabalin 300-mg group.[43]
In a RCT, 80 patients undergoing elective spinal fusion surgery received placebo, celecoxib 400 mg, pregabalin 150 mg, or a combination of celecoxib 400 mg and pregabalin 150 mg orally 1 h before the induction of general anesthesia. Postoperatively, patients received patient-controlled analgesia (PCA) using morphine. Twelve hours after initial study drug administration, patients were given placebo, celecoxib 200 mg, pregabalin 150 mg, or a combination of celecoxib 200 mg and pregabalin 150 mg orally. The combination of pregabalin and celecoxib significantly reduced pain and opioid use compared with the use of either analgesic alone.[44]
In another RCT, control of pain after the perioperative administration of pregabalin 300 or 600 mg was compared with diazepam 10 mg in 91 women scheduled for laparoscopic hysterectomy. The patients were randomized to receive either diazepam 10mg (D10), or pregabalin 150mg (P300) or 300mg (P300) or 300 mg (P600) as premedication, and the dose was repeated after 12 h, except for the D10 group, in which the patients received placebo. Analgesia was provided by oxycodone using patient-controlled analgesia till the first postoperative morning. The doses of oxycodone during 0–12 h after surgery were similar in the three groups, whereas the dose of oxycodone during 12–24 h after surgery was smaller in the P600 group than in the P300 group (0.09 vs. 0.16 mg/kg; P=0.025). The total dose of oxycodone (0–24 h after surgery) was smaller in the P600 group than in the D10 group (0.34 vs. 0.45 mg/kg; P=0.046). However, the incidence of dizziness (70% vs. 35%; P=0.012), blurred vision (63% vs. 14%; P=0.002), and headache (31% vs. 7%; P=0.041) was higher in the P600 group than in the D10 group.[45]
Another double-blind RCT compared the effect of premedication with pregabalin 300 mg or lorazepam 0.5 mg on postoperative morphine consumption in 80 women, aged 18–65 years, and undergoing elective abdominal hysterectomy with/without salphingo-oophorectomy. Intraoperatively, patients received intravenous (IV) morphine 100–200 μg/kg and postoperative analgesia was provided with an IV morphine-based PCA regimen: bolus 1 mg, lockout interval 5 min, 4-h limit 40 mg. Compared to the lorazepam group, patients in the pregabalin group had lower pain scores on the verbal numerical rating scale (P<0.01) and lower morphine consumption (7.115.57 mg vs. 21.187.12 mg, P<0.01) in the first 24 h. The incidence of somnolence, dizziness, nausea, and vomiting were equal among both the groups but the satisfaction score was higher in the pregabalin group.[46]
The perioperative administration of pregabalin 150 mg 1 h before surgery and repeated after 12 h was effective in reducing early postoperative pain (48 h) but not chronic pain and chest hypoesthesia in a placebo-controlled RCT done in 90 patients undergoing robot-assisted endoscopic thyroidectomy. However, the incidence of sedation and dizziness was significant.[47]
In a double-blind RCT, combinations of paracetamol and pregabalin, or paracetamol, pregabalin, and dexamethasone did not reduce the pain score and morphine consumption compared with paracetamol alone for patients undergoing abdominal hysterectomy. A total of 116 patients were randomly divided into either group A (paracetamol+placebo), group B (paracetamol+pregabalin+placebo), or group C (paracetamol+pregabalin+dexamethasone). The patients received paracetamol 1 g, pregabalin 300 mg, dexamethasone 8 mg, or placebo according to the group allocated 1 h before general anesthesia. Postoperative analgesia was provided with paracetamol 1 g in every 6 h and IV morphine-based PCA. The 24-h morphine consumption and pain score, both at rest and during mobilization, were not significantly different between treatment groups. The mean nausea score (P=0.002) was reduced in group C as compared to group A. The number of vomits was significantly reduced in both groups B (P=0.041) and C (P=0.001) as compared to group A. The consumption of ondansetron was reduced in group C as compared to groups A and B (P<0.001). Other side effects were not different between groups.[48]
Postlaparoscopic shoulder pain (PLSP) is not uncommon following laparoscopic surgery. In a placebo-controlled study, two doses of pregabalin 300 mg were administered 12 h apart. The frequency and severity of PLSP, need for postoperative rescue analgesia, and side effects were assessed for 48 h postoperatively. In both the groups, the overall incidence of PLSP, pain score for PLSP, time to first rescue analgesia, and cumulative ketorolac consumption did not differ significantly. However, the patients in the pregabalin group had increased sedation 2 h after surgery.[49]
Pregabalin and spinal anesthesia
One study compared the preemptive analgesic efficacy of gabapentin and pregabalin for postoperative pain after surgeries done under spinal anesthesia. Sixty patients were randomized to receive either gabapentin 1200 mg or pregabalin 300 mg 1 h prior to spinal anesthesia. Postoperative analgesia was provided with intramuscular diclofenac 1 mg/kg when the VAS score for pain was >3. Time to first analgesia was 8.98 h in the gabapentin group and 14.17 h in the pregabalin group (P<0.001).[50]
In a placebo-controlled, double-blind RCT, the efficacy of the perioperative treatment with pregabalin to reduce chronic pain following total knee arthroplasty (TKA) was studied. Pregabalin (300 mg) was administered before TKA and for 14 days after TKA (150 mg BD for 10 days, 75 mg BD on days 11–12 and 50 mg BD on days 13–14). Patients were screened for the presence of neuropathic pain at 3 and 6 months postoperatively. A combined spinal epidural technique was used for intraoperative anesthesia, and patient-controlled epidural analgesia (PCEA) with bupivacaine and fentanyl was used for postoperative analgesia. No patient in the pregabalin group had neuropathic pain whereas 8.7% and 5.2% patients had neuropathic pain in the placebo group, after 3 and 6 months, respectively (P=0.001 and P=0.014). During the hospital stay, patients in the pregabalin group consumed less epidural opioids (P=0.003) and less oral opioids (P=0.005), and had greater active flexion at postoperative day 30 (P=0.013). However, the increased incidence of sedation and confusion was noted in the pregabalin group in the first 24 h following surgery.[51]
In a RCT, premedication with pregabalin 300 mg or pregabalin 300 mg+dexamethasone 8 mg provided significant reduction in 24-h postoperative morphine consumption following total hip arthroplasty (THA) done under spinal anesthesia in 120 patients. The addition of dexamethasone did not provide any added advantage on pain control, but reduced the incidence of vomiting.[52]
Out of the three studies involving the use of pregabalin in spinal anesthesia, one[51] focused on chronic pain after surgery. Among the other two, only one study[52] was placebo controlled. This study reported a decrease in the postoperative narcotic use but not pain scores, and sedation was significantly increased as well.
Studies using pregabalin <300 mg/day
A single dose of pregabalin 150 mg administered 1 h before surgery was found to be effective in reducing pain scores and postoperative fentanyl consumption in the first 24 h following laparoscopic cholecystectomy in a randomized placebo-controlled trial conducted in 60 patients.[53]
Pregabalin in daycare surgery
The efficacy of pregabalin has been evaluated in ambulatory daycare surgeries. In a double-blind, parallel-group, placebo-controlled RCT, 90 women having minor gynecological surgery involving the uterus received either oral pregabalin 100 mg or placebo approximately 1 h before surgery. The primary outcome was the pain score in the recovery unit, and patients were followed for 24 h. There was no significant difference between groups for pain in the recovery room or thereafter, nor for the recovery room fentanyl requirement or the quality of recovery at 24 h postoperatively. The incidence of posthospital discharge light-headedness, visual disturbance, and difficulty with walking was significantly higher in the pregabalin group.[54]
In a randomized placebo-controlled trial, pregabalin 75 mg BD was used for 7 days along with hydrocodone 5 mg SOS following daycare augmentation mammoplasty in 80 patients. There was 70% reduction in the postoperative narcotic use, significantly less reported pain, and a 46% reduction in nausea in the pregabalin-treated group.[55]
The effect of low-dose pregabalin was evaluated in 162 patients undergoing laparoscopic cholecystectomy in a prospective randomized double-blind study. The patients received either pregabalin 50 mg or pregabalin 75 mg or placebo 1 h before surgery and then every 12 h for three doses. Compared to the placebo group, lower pain scores were observed till 90 min postoperatively in the pregabalin 75 mg group and for 45 min postoperatively in the pregabalin 50 mg group (P<0.05). However, postoperative analgesic consumption, recovery scores and side-effects were similar in all three groups.[56]
Six of the 14 RCTs reported a decrease in postoperative pain scores in the first 24 h, when compared to placebo, after the perioperative use of pregabalin, and 7 RCTs reported a significant decrease in opioid consumption in the first 24 h. However, in a recent meta-analysis it was found that the pain intensity is not significantly reduced by pregabalin in the first 24 h after surgery, though opioid consumption in the first 24 h was significantly reduced with an associated reduction in the incidence of postoperative vomiting.[57] However, pregabalin increased the incidence of visual disturbances in most of the studies along with increased sedation, dizziness, and headache suggesting that it should be used more cautiously in daycare surgeries. Most of the studies showing the benefit of pregabalin are laparoscopic surgeries, daycare surgeries, and minor gynaecological surgeries, which are not very painful. The efficacy of pregabalin in more painful surgeries is yet to be determined.
Pregabalin and perioperative anxiety and sedation
Pregabalin possesses an anxiolytic property and has been found effective in the treatment of generalized anxiety disorder (GAD) or social anxiety disorder (SAD).[58,59] A dose ranging study was conducted to find out the effect of pregabalin as premedication on acute state anxiety and sedation in 108 patients undergoing elective surgery. The patients were randomly divided to receive any of the following four drugs: placebo, pregabalin 75 mg, pregabalin 150 mg, and pregabalin 300 mg. The level of anxiety, sedation, and pain were assessed at baseline, 30 min, and 60 min after drug administration, before the induction of anesthesia and every 30 min in the postanaesthesia care unit (PACU) on an 11-point scale (0=no effect, 10=maximal effect). Postoperative fentanyl requirement, PACU and hospital discharge time, early recovery score, and late recovery outcome (e.g., recovery of the bowel function and resumption of the oral intake) were all assessed. Anxiety levels were not affected in the preoperative period and did not differ among the groups. However, in the pregabalin 300 mg group, sedation scores were higher compared to the control group during the preinduction period and at 90 and 120 min postoperatively. Postoperative fentanyl requirement, and PACU and hospital discharge time were not significantly different among the groups.[60]
Pregabalin and chronic pain
The approved uses of pregabalin for the treatment of chronic pain are shown in Table 2.
Table 2.
Approved usage of pregabalin

Tassone et al. reviewed the efficacy of pregabalin in neuropathic pain, partial seizures and GAD or SAD. Data of a total 1068 patients of diabetic peripheral neuropathy were reviewed from four clinical trials and pregabalin was found to be effective. Patients in the pregabalin group (300–600 mg/day) had significantly better pain relief than the placebo group (P ≤ 0.01). Pregabalin 450–600 mg/day showed a significant improvement in pain relief and pain-related sleep interference than placebo in patients with postherpetic neuralgia (P ≤ 0.002). In three studies which evaluated the efficacy of pregabalin in GAD and SAD, the use of pregabalin 200–600 mg/day showed a significant reduction in pain scores on the Hamilton Anxiety Scale compared to placebo groups (P ≤ 0.01). Most common adverse effects reported across all these clinical trials were somnolence (≤50%), dizziness (≤49%), and headache (≤29%) which resulted in withdrawal from the study in ≤32% patients.[61]
The Cochrane database reviewed the double-blind RCT reporting on the analgesic effect of pregabalin, with subjective pain assessment by the patient as either the primary or a secondary outcome. A total of 19 studies involving 7003 patients were reviewed. It was found that pregabalin doses ≥300 mg/day were effective analgesics in postherpetic neuralgia, diabetic neuropathy, central neuropathic pain, and fibromyalgia whereas doses ≤150 mg/day were generally ineffective. The lowest number needed to treat (NNT) for a substantial benefit (at least 50% pain relief over the baseline) for pregabalin 600 mg/day compared to placebo were 3.9 (95% confidence interval, 3.1–5.1) for postherpetic neuralgia, 5.0 (4.0–6.6) for diabetic peripheral neuropathy, 5.6 (3.5–14) for central neuropathic pain, and 11 (7.1–21) for fibromyalgia. Higher rates of the substantial benefit were found in postherpetic neuralgia and painful diabetic neuropathy, but not in central neuropathic pain or fibromyalgia. A high incidence of side effects was reported with pregabalin dose 600 mg/day with somnolence in 15–25% patients and dizziness in 27–46% patients, and discontinuation of treatment was observed in 18–28% of patients.[62] To have a substantial benefit (at least 50% pain relief over the baseline), NNTs for pregabalin 600 mg/day compared to placebo were 3.9 (95% confidence interval 3.1–5.1) for postherpetic neuralgia, 5.0 (4.0–6.6) for diabetic peripheral neuropathy, 5.6 (3.5–14) for central neuropathic pain, and 11 (7.1–21) for fibromyalgia.[62]
Roth et al. conducted a review of a double-blind, placebo-controlled RCT of pregabalin in painful diabetic neuropathy and postherpetic neuralgia. A total of nine RCTs which reported pain as well as sleep measures as end points were included in the review. It provided data of a total 2399 patients who were treated two to three times a day with pregabalin (dose 75–600 mg/day) or placebo on a fixed or flexible schedule. Pregabalin at doses 150–600 mg/day provided significant analgesic benefit as well as improved pain-related sleep interference.[63]
Conclusions
Based on available data (RCTs and meta-analysis), there is no clear evidence that the perioperative use of pregabalin reduces the post-operative pain intensity. However, pregabalin exhibits a significant opioid-sparing effect in the first 24 h and a significant reduction in opioid-related adverse effects (vomiting). The incidence of visual disturbance is significant with pregabalin; other side effects like sedation and dizziness are also increased. Due to heterogeneity of data, a conclusion on the optimal dose and duration of the therapy cannot be drawn. No studies have evaluated pregabalin in chronic nociceptive pain, like arthritis. However, pregabalin 150-600 mg/day has a proven efficacy under chronic neuropathic pain conditions (painful diabetic neuropathy, postherpetic neuralgia, central neuropathic pain) and fibromyalgia. Pregabalin is a valuable addition to the limited options for the treatment of neuropathic pain. It may be more cost-effective than high-dose gabapentin[64,65] and may be effective in patients who have previously failed to respond to gabapentin.[66]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Partridge B, Chaplan S, Sakamoto E, Yaksh T. Characterization of the effects of gabapentin and 3-isobutyl-g-aminobutyric acid on substance P-induced thermal hyperalgesia. Anesthesiology. 1998;88:196–205. doi: 10.1097/00000542-199801000-00028. [DOI] [PubMed] [Google Scholar]
- 2.Jun J, Yaksh T. The effect of intrathecal gabapentin and 3-isobutyl-g-aminobutyric acid on the hyperalgesia observed after thermal injury in the rat. Anesth Analg. 1998;86:348–54. doi: 10.1097/00000539-199802000-00025. [DOI] [PubMed] [Google Scholar]
- 3.Nozaki-Taguchi N, Chaplan SR, Higuera ES, Ajakwe RC, Yaksh TL. Vincristine-induced allodynia in the rat. Pain. 2001;93:69–76. doi: 10.1016/S0304-3959(01)00294-9. [DOI] [PubMed] [Google Scholar]
- 4.Field MJ, Holloman EF, McCleary S, Hughes J, Singh L. Evaluation of gabapentin and S-(+)-3-isobutylgaba in a rat model of postoperative pain. J Pharmacol Exp Ther. 1997;282:1242–6. [PubMed] [Google Scholar]
- 5.Field M, Oles R, Lewis A, McCleary S, Hughes J, Singh L. Gabapentin (neurontin) and S-(+)-3-isobutylgaba represent a novel class of selective antihyperalgesic agents. Br J Pharmacol. 1997;121:1513–22. doi: 10.1038/sj.bjp.0701320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Houghton AK, Lu Y, Westlund KN. S-(+)-3-Isobutylgaba and its stereoisomer reduces the amount of inflammation and hyperalgesia in an acute arthritis model in the rat. J Pharmacol Exp Ther. 1998;285:533–8. [PubMed] [Google Scholar]
- 7.Ho KY, Gan TJ, Habib AS. Gabapentin and postoperative pain—a systematic review of randomized controlled trials. Pain. 2006;126:91–101. doi: 10.1016/j.pain.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 8.Tiippana EM, Hamunen K, Kontinen VK, Kalso E. Do Surgical Patients Benefit from Perioperative Gabapentin/Pregabalin? A Systematic Review of Efficacy and Safety. Anesth Analg. 2007;104:1545–56. doi: 10.1213/01.ane.0000261517.27532.80. [DOI] [PubMed] [Google Scholar]
- 9.Ben-Menachem E. Pregabalin pharmacology and its relevance to clinical practice. Epilepsia. 2004;45:13–8. doi: 10.1111/j.0013-9580.2004.455003.x. [DOI] [PubMed] [Google Scholar]
- 10.Piyapolrungroj N, Li C, Bockbrader H, Liu G, Fleisher D. Mucosal uptake of gabapentin (neurontin) vs.pregabalin in the small intestine. Pharm Res. 2001;18:1126–30. doi: 10.1023/a:1010970809090. [DOI] [PubMed] [Google Scholar]
- 11.Busch J, Strand J, Posvar E, Bockbrader H, Radulovic L. Pregabalin (CI-1008) multiple-dose pharmacokinetics and safety/tolerence in healthy volunteers. Pharm Sci. 1999;1:2033. [Google Scholar]
- 12.Bockbrader H, Hunt T, Strand J, Posvar E, Sedman A. Pregabalin pharmacokinetics and safety in healthy volunteers: Results from two phase 1 studies. Neurology. 2000;54:A421. [Google Scholar]
- 13.Su TZ, Feng MR, Weber ML. Mediation of highly concentrative uptake of pregabalin by L-type amino acid transport in Chinese hamster ovary and Caco-2 cells. J Pharmacol Exp Ther. 2005;313:1406–15. doi: 10.1124/jpet.104.082255. [DOI] [PubMed] [Google Scholar]
- 14.Freynhagen R, Strojek K, Griesing T, Whalen E, Balkenohl M. Efficacy of pregabalin in neuropathic pain evaluated in a 12-week, randomised, double-blind, multicentre, placebo-controlled trial of fble- and fixed-dose regimens. Pain. 2005;115:254–63. doi: 10.1016/j.pain.2005.02.032. [DOI] [PubMed] [Google Scholar]
- 15.Bryans JS, Wustrow DJ. 3-Substituted GABA analogs with central nervous system activity: A review. Med Res Rev. 1999;19:149–77. doi: 10.1002/(sici)1098-1128(199903)19:2<149::aid-med3>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 16.Lauria-Horner BA, Pohl RB. Pregabalin: A new anxiolytic. Expert Opin Investig Drugs. 2003;12:663–72. doi: 10.1517/13543784.12.4.663. [DOI] [PubMed] [Google Scholar]
- 17.Arikkath J, Campbell KP. Auxiliary subunits: Essential components of the voltage-gated calcium channel complex. Curr Opin Neurobiol. 2003;13:298–307. doi: 10.1016/s0959-4388(03)00066-7. [DOI] [PubMed] [Google Scholar]
- 18.Bian F, Li Z, Offord J, Davis M, McCormick J, Taylor C. Calcium channel α(2)-δ type 1 subunit is the major binding protein for pregabalin in neocortex, hippocampus, amygdala, and spinal cord: An ex vivo autoradiographic study in α(2)-δ type 1 genetically modified mice. Brain Res. 2006;1:1–6. doi: 10.1016/j.brainres.2005.12.084. [DOI] [PubMed] [Google Scholar]
- 19.Belliotti T, Capiris T, Ekhato I, Kinsora J, Field M, Heffner T, et al. Structure-activity relationships of pregabalin and analogues that target the α(2)-δ protein. J Med Chem. 2005;48:2294–307. doi: 10.1021/jm049762l. [DOI] [PubMed] [Google Scholar]
- 20.Gazulla J, Tintore M. The P/Q-type voltage-dependent calcium channel as pharmacological target in spinocerebellar ataxia type 6: Gabapentin and pregabalin may be of therapeutic benefit. Med Hypotheses. 2007;68:131–6. doi: 10.1016/j.mehy.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 21.Jones D, Sorkin L. Systemic gabapentin and S(+)-3-isobutyl-γ- aminobutyric acid block secondary hyperalgesia. Brain Res. 1998;810:93–9. doi: 10.1016/s0006-8993(98)00890-7. [DOI] [PubMed] [Google Scholar]
- 22.Dooley D, Donovan C, Pugsley T. Stimulus-dependent modulation of [3H]norepinephrine release from rat neocortical slices by gabapentin and pregabalin. J Pharmacol Exp Ther. 2000;295:1086–93. [PubMed] [Google Scholar]
- 23.Dooley DJ, Mieske CA, Borosky SA. Inhibition of K+-evoked glutamate release from rat neocortical and hippocampal slices by gabapentin. Neurosci Lett. 2000;280:107–10. doi: 10.1016/s0304-3940(00)00769-2. [DOI] [PubMed] [Google Scholar]
- 24.Fink K, Dooley DJ, Meder WP, Suman-Chauhan N, Duffy S, Clusmann H, et al. Inhibition of neuronal Ca 2+ influx by gabapentin and pregabalin in the human neocortex. Neuropharmacology. 2002;42:229–36. doi: 10.1016/s0028-3908(01)00172-1. [DOI] [PubMed] [Google Scholar]
- 25.Errante L, Petroff OA. Acute effects of gabapentin and pregabalin on rat forebrain cellular GABA, glutamate, and glutamine concentrations. Seizure. 2003;12:300–6. doi: 10.1016/s1059-1311(02)00295-9. [DOI] [PubMed] [Google Scholar]
- 26.Cunningham M, Woodhall G, Thompson S, Dooley D, Jones R. Dual effects of gabapentin and pregabalin on glutamate release at rat entorhinal synapses in vitro. Eur J Neurosci. 2004;20:1566–76. doi: 10.1111/j.1460-9568.2004.03625.x. [DOI] [PubMed] [Google Scholar]
- 27.Micheva KD, Taylor CP, Smith SJ. Pregabalin reduces the release of synaptic vesicles from cultured hippocampal neurons. Mol Pharmacol. 2006;70:467–76. doi: 10.1124/mol.106.023309. [DOI] [PubMed] [Google Scholar]
- 28.Bialer M, Johannessen SI, Kupferberg HJ, Levy RH, Loiseau P, Perucca E. Progress report on new antiepileptic drugs: A summary of the fourth Eilat conference (EILAT IV) Epilepsy Res. 1999;34:1–41. doi: 10.1016/s0920-1211(98)00108-9. [DOI] [PubMed] [Google Scholar]
- 29.Welty D, Wang Y, Busch J, Taylor C, Vartanian M, Radulovic L. Pharmacokinetics and pharmacodynamics of CI-1008 (pregabalin) and gabapentin in rats with maximal electroshock. Epilepsia. 1977;388(suppl) Abstract 1.110. [Google Scholar]
- 30.Lanneau C, Green A, Hirst W, Wise A, Brown J, Donnier E, et al. Gabapentin is not a GABA receptor agonist. Neuropharmacology. 2001;41:965–75. doi: 10.1016/s0028-3908(01)00140-x. [DOI] [PubMed] [Google Scholar]
- 31.Randinitis EJ, Posvar EL, Alvey CW, Sedman AJ, Cook JA, Bockbrader HN. Pharmacokinetics of pregabalin in subjects with various degrees of renal function. J Clin Pharmacol. 2003;43:277–83. doi: 10.1177/0091270003251119. [DOI] [PubMed] [Google Scholar]
- 32.Hindmarch I, Trick L, Ridout F. A double-blind, placebo- and positive-internal-controlled (alprazolam) investigation of the cognitive and psychomotor profile of pregabalin in healthy volunteers. Psychopharmacology. 2005;183:133–43. doi: 10.1007/s00213-005-0172-7. [DOI] [PubMed] [Google Scholar]
- 33.Dolin SJ, Cashman JN. Tolerability of acute postoperative pain management: Nausea, vomiting, sedation, pruritis, and urinary retention.Evidence from published data. Br J Anaesth. 2005;95:584–91. doi: 10.1093/bja/aei227. [DOI] [PubMed] [Google Scholar]
- 34.Woolf C, Chong M. Preemptive analgesia-treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg. 1993;77:362–79. doi: 10.1213/00000539-199377020-00026. [DOI] [PubMed] [Google Scholar]
- 35.Lascelles BD, Waterman AE, Cripps PJ, Livingston A, Henderson G. Central sensitization as a result of surgical pain: Investigation of the pre-emptive value of pethidine for ovariohysterectomy in the rat. Pain. 1995;62:201–12. doi: 10.1016/0304-3959(94)00266-H. [DOI] [PubMed] [Google Scholar]
- 36.Perkins F, Kehlet H. Chronic pain as an outcome of surgery.A review of predictive factors. Anesthesiology. 2000;93:1123–33. doi: 10.1097/00000542-200010000-00038. [DOI] [PubMed] [Google Scholar]
- 37.Aasvang E, Kehlet H. Chronic postoperative pain: The case of inguinal herniorrhaphy. Br J Anaesth. 2005;95:69–76. doi: 10.1093/bja/aei019. [DOI] [PubMed] [Google Scholar]
- 38.Dahl JB, Mathiesen O, Moiniche S. ‘Protective premedication’: An option with gabapentin and related drugs? A review of gabapentin and pregabalin in the treatment of post-operative pain. Acta Anaesthesiol Scand. 2004;48:1130–6. doi: 10.1111/j.1399-6576.2004.00484.x. [DOI] [PubMed] [Google Scholar]
- 39.Rowbotham DJ. Gabapentin: A new drug for postoperative pain? Br J Anaesth. 2006;96:152–5. doi: 10.1093/bja/aei318. [DOI] [PubMed] [Google Scholar]
- 40.Turan A, Kaya G, Karamanlioglu B, Pamukcu Z, Apfel C. Effect of oral gabapentin on postoperative epidural analgesia. Br J Anaesth. 2006;96:242–6. doi: 10.1093/bja/aei294. [DOI] [PubMed] [Google Scholar]
- 41.Gilron I, Biederman J, Jhamandas K, Hong M. Gabapentin blocks and reverses antinociceptive morphine tolerance in the rat paw-pressure and tail-flick tests. Anesthesiology. 2003;98:1288–92. doi: 10.1097/00000542-200305000-00037. [DOI] [PubMed] [Google Scholar]
- 42.Hansen C, Gilron I, Hong M. The effects of intrathecal gabapentin on spinal morphine tolerance in the rat tail-flick and paw pressure tests. Anesth Analg. 2004;99:1180–4. doi: 10.1213/01.ANE.0000130383.87438.A9. [DOI] [PubMed] [Google Scholar]
- 43.Hill C, Balkenohl M, Thomas D, Walker R, Mathe H, Murray G. Pregabalin in patients with postoperative dental pain. Eur J Pain. 2001;5:119–24. doi: 10.1053/eujp.2001.0235. [DOI] [PubMed] [Google Scholar]
- 44.Reuben SS, Buvanendran A, Kroin JS, Raghunathan K. The analgesic efficacy of celecoxib, pregabalin, and their combination for spinal fusion surgery. Anesth Analg. 2006;103:1271–7. doi: 10.1213/01.ane.0000237279.08847.2d. [DOI] [PubMed] [Google Scholar]
- 45.Jokela R, Ahonen J, Tallgren M, Haanpaa M, Korttila K. A randomized controlled trial of perioperative administration of pregabalin for pain after laparoscopic hysterectomy. Pain. 2008;134:106–12. doi: 10.1016/j.pain.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 46.Ittichaikulthol W, Virankabutra T, Kunopart M, Khamhom W, Putarawuthichai P, Rungphet S. Effects of Pregabalin on Post operative Morphine Consumption and Pain after Abdominal Hysterectomy with/without Salphingo-oophorectomy: A Randomized, Double-Blind Trial. J Med Assoc Thai. 2009;92:1318–23. [PubMed] [Google Scholar]
- 47.Kim SY, Jeong JJ, Chung WY, Kim HJ, Nam KH, Shim YH. Perioperative administration of pregabalin for pain after robot-assisted endoscopic thyroidectomy: A randomized clinical trial. Surg Endosc. 2010;24:2776–81. doi: 10.1007/s00464-010-1045-7. [DOI] [PubMed] [Google Scholar]
- 48.Mathiesen O, Rasmussen ML, Dierking G, Lech K, Hilsted KL, Fomsgaard JS, et al. Pregabalin and dexamethasone in combination with paracetamol for postoperative pain control after abdominal hysterectomy.A randomized clinical trial. Acta Anaesthesiol Scand. 2009;53:227–35. doi: 10.1111/j.1399-6576.2008.01821.x. [DOI] [PubMed] [Google Scholar]
- 49.Chang SH, Lee HW, Kim HK, Kim SH, Kim DK. An evaluation of perioperative pregabalin for prevention and attenuation of postoperative shoulder pain after laparoscopic cholecystectomy. Anesth Analg. 2009;109:1284–6. doi: 10.1213/ane.0b013e3181b4874d. [DOI] [PubMed] [Google Scholar]
- 50.Saraswat V, Arora V. Preemptive gabapentin vs pregabalin for acute post-operative pain after surgery under spinal anaesthesia. Indian J Anaesth. 2008;52:829–34. [Google Scholar]
- 51.Buvanendran A, Kroin JS, Della-Valle CJ, Kari M, Moric M, Tuman KJ. Perioperative oral pregabalin reduces chronic pain after total knee arthroplasty: A prospective, randomized, controlled trial. Anesth Analg. 2010;110:199–207. doi: 10.1213/ANE.0b013e3181c4273a. [DOI] [PubMed] [Google Scholar]
- 52.Mathiesen O, Jacobsen LS, Holm HE, Randall S, Adamiec-Malmstroem L, Graungaad BK, et al. Pregabalin and dexamethasone for postoperative pain control: A randomized controlled study in hip arthroplasty. Br J Anaesth. 2008;101:535–41. doi: 10.1093/bja/aen215. [DOI] [PubMed] [Google Scholar]
- 53.Agarwal A, Gautam S, Gupta D, Agarwal S, Singh PK, Singh U. Evaluation of a single preoperative dose of pregabalin for attenuation of postoperative pain after laparoscopic cholecystectomy. Br J Anaesth. 2008;101:700–4. doi: 10.1093/bja/aen244. [DOI] [PubMed] [Google Scholar]
- 54.Paech MJ, Goy R, Chua S, Scott K, Christmas T, Doherty A. randomized, placebo-controlled trial of preoperative oral pregabalin for postoperative pain relief after minor gynecological surgery. Anesth Analg. 2007;105:1449–3. doi: 10.1213/01.ane.0000286227.13306.d7. [DOI] [PubMed] [Google Scholar]
- 55.Freedman BM, O’Hara E. Pregabalin has opioid-sparing effects following augmentation mammaplasty. Aesthetic Surg J. 2008;28:421–4. doi: 10.1016/j.asj.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 56.Peng PW, Li C, Farcas E, Haley A, Wong W, Bender J. Use of low-dose pregabalin in patients undergoing laparoscopic cholecystectomy. Br J Anaesth. 2010;105:155–61. doi: 10.1093/bja/aeq116. [DOI] [PubMed] [Google Scholar]
- 57.Zhang J, Ho KY, Wang Y. Efficacy of pregabalin in acute postoperative pain: A meta-analysis. Br J Anaesth. 2011;106:454–62. doi: 10.1093/bja/aer027. [DOI] [PubMed] [Google Scholar]
- 58.Pande AC, Feltner DE, Jefferson JW, Davidson JR, Pollack M, Stein MB, et al. Efficacy of the novel anxiolytic pregabalin in social anxiety disorder: A placebo-controlled, multicentre study. J Clin Psychopharmacol. 2004;24:141–9. doi: 10.1097/01.jcp.0000117423.05703.e7. [DOI] [PubMed] [Google Scholar]
- 59.Pande AC, Crockatt JG, Feltner DE, Janney CA, Smith WT, Weisler R, et al. Pregabalin in generalized anxiety disorder: A placebo-controlled trial. Am J Psychiatry. 2003;160:533–40. doi: 10.1176/appi.ajp.160.3.533. [DOI] [PubMed] [Google Scholar]
- 60.White PF, Tufanogullari B, Taylor J, Klein K. The Effect of Pregabalin on Preoperative Anxiety and Sedation Levels: A Dose-Ranging Study. Anesth Analg. 2009;108:1140–5. doi: 10.1213/ane.0b013e31818d40ce. [DOI] [PubMed] [Google Scholar]
- 61.Tassone DM, Boyce E, Guyer J, Nuzum D. Pregabalin: A novel gamma-aminobutyric acid analogue in the treatment of neuropathic pain, partial-onset seizures, and anxiety disorders. Clin Ther. 2007;29:26–48. doi: 10.1016/j.clinthera.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 62.Moore RA, Straube S, Wiffen PJ, Derry S, McQuay HJ. Pregabalin for acute and chronic pain in adults. Cochrane Database Syst Rev. 2009;8:CD007076. doi: 10.1002/14651858.CD007076.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Roth T, van Seventer R, Murphy TK. The effect of pregabalin on pain-related sleep interference in diabetic peripheral neuropathy or postherpetic neuralgia: A review of nine clinical trials. Curr Med Res Opin. 2010;26:2411–9. doi: 10.1185/03007995.2010.516142. [DOI] [PubMed] [Google Scholar]
- 64.Smith K, Roberts M. Sequential medication strategies for postherpetic neuralgia: A cost-effectiveness analysis. J Pain. 2007;8:396–404. doi: 10.1016/j.jpain.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 65.Tarride J, Gordon A, Vera-Llonch M, Dukes E, Rousseau C. Cost-effectiveness of pregabalin for the management of neuropathic pain associated with diabetic peripheral neuropathy and postherpetic neuralgia: A Canadian perspective. Clin Ther. 2006;28:1922–34. doi: 10.1016/j.clinthera.2006.11.017. [DOI] [PubMed] [Google Scholar]
- 66.D’Urso De Cruz E DR, Stacey B, Siffert J, Emir B. San Diego, California: American Diabetes Association 64th Scientific Sessions; 2005. Long-term treatment of painful DPH and PHN with pregabalin in treatmentrefractory patients. Poster presented at. [Google Scholar]


