Abstract
Background
Children of substance abusers are at risk for behavioral/emotional problems. To improve outcomes for these children, we developed and tested an intervention that integrated a novel contingency management (CM) program designed to enhance compliance with an empirically-validated parent training curriculum. CM provided incentives for daily monitoring of parenting and child behavior, completion of home practice assignments, and session attendance.
Methods
Forty-seven mothers with substance abuse or dependence were randomly assigned to parent training + incentives (PTI) or parent training without incentives (PT). Children were 55% male, ages 2-7 years.
Results
Homework completion and session attendance did not differ between PTI and PT mothers, but PTI mothers had higher rates of daily monitoring. PTI children had larger reductions in child externalizing problems in all models. Complier Average Causal Effects (CACE) analyses showed additional significant effects of PTI on child internalizing problems, parent problems and parenting. These effects were not significant in standard Intent-to-Treat analyses.
Conclusion
Results suggest our incentive program may offer a method for boosting outcomes.
Keywords: contingency management, preschool, children of substance abusers, parent training, Complier Average Causal Effects
1. Introduction
Approximately 13.6% of all preschool children (ages 3-5) live with one or more parents with a past year diagnosis of substance abuse or dependence (SAMHSA, 2009). Parental substance abuse increases the risk for a variety of poor child outcomes, with the greatest risk for conduct problems across a wide developmental period (Clark et al., 2004; Hussong et al., 2007; Loukas et al., 2003; Tarter et al., 2004). Research on improving outcomes among children of parents who abuse substances is limited and has generally shown small effects. Several studies have targeted infants and toddlers ages 0-3 (Ernst et al., 1999; Huebner, 2002; Schuler et al., 2002). Others have focused on elementary and middle school-aged children (Brown et al., 2005; Kumpfer and DeMarsh, 1985; Lam et al., 2008; Luthar et al., 2007) .
However, it is particularly important to target the preschool period and the transition to elementary school because this period marks the onset of life-course-persistent conduct problems (Moffitt, 1993). To our knowledge, only one intervention study for substance abusing families has specifically targeted preschoolers (Nye et al., 1995). This study tested a 10-month parent training intervention plus therapy targeting marital conflict. Families in which the father had been convicted for drunk driving with a son aged 3-6 were randomly assigned to one of two treatment conditions (mother alone versus both parents) or to a no treatment control group. Both treatment groups showed significant effects on negative, prosocial and affectionate behavior, but only prosocial behavior remained improved at follow-up.
Contingency-management (CM) procedures can be applied to modify behavior of all kinds, including parenting practices, drug abuse, and other conduct problems. Clinical trials examining the efficacy of CM across multiple types of drug dependence and clinical populations provide compelling empirical support for the efficacy of this treatment approach (Higgins et al., 2008). In addition to directly reinforcing drug abstinence, CM procedures have also been used to reinforce compliance with participation in assigned pro-social, non-drug related activities outside of therapy sessions (Bickel et al., 1997; Iguchi et al., 1997; Petry et al., 2000). Participation in these activities was highly correlated with abstinence, suggesting that improving compliance with treatment can improve outcomes.
Parental involvement, compliance with treatment procedures, and therapeutic dose are important predictors of treatment outcome among parent management programs (Nye et al., 1995; Reid et al., 2004; Webster-Stratton et al., 2001). Recognizing the importance of attendance, studies of comprehensive preventive interventions targeting conduct problems have included monetary incentives to parents for attending sessions (Conduct Problems Prevention Research Group, 1999; Irvine et al., 1999). However, these studies did not test whether the incentives contributed to increased attendance or improved outcomes. Although Heinrichs (2006) found that providing incentives increased enrollment in parenting programs, providing monetary incentives for session attendance may not sufficiently increase parental involvement or compliance with treatment procedures (Heinrichs and Jensen-Doss, 2010).
Mothers who have a history of substance abuse or dependence tend to display parenting behaviors linked to the development of conduct problems with their preschool children (Kerwin, 2005; Luthar and Suchman, 2000; Luthar and Walsh, 1995). We selected Webster-Stratton's BASIC Parent Training Program for use with our target population because of its efficacy as a preventive intervention for at risk preschool age children (Reid et al., 2004; Webster-Stratton, 1998; Webster-Stratton et al., 2001). In several different Head Start samples, this parenting intervention has resulted in significantly improved parenting and reductions in child conduct problems. Of note, in a study that used the Incredible Years intervention across several treated preschool samples, approximately 24% of mothers reported lifetime histories of substance abuse, and mothers with a substance abuse history had higher pre-treatment inconsistent and ineffective parenting, but also higher supportive and positive parenting (Baydar et al., 2003). Maternal substance use history was also positively related to a program engagement construct (defined as attendance, compliance with assignments, and group leader rating of engagement), and engagement was related to positive parenting and child behavior outcomes in a dose-response fashion (Baydar et al., 2003). These results suggest that children of substance abusing mothers are at significant risk, but that both mothers and children can benefit from parenting interventions.
To boost outcomes for preschool aged children of substance abusing mothers, we augmented this evidence-based parent training (PT) program with a CM intervention that provided incentives contingent on attendance, homework completion, and daily report of parenting and child behavior. This 2-condition initial randomized study compared PT alone to PT plus contingent incentives (PTI). We hypothesized that PTI families would attend more sessions, complete more assignments, make more daily monitoring calls about parenting and child behavior, and show greater improvements in parenting and externalizing and internalizing problems compared to PT families. A second aim of the study was to examine these hypotheses as tested using traditional Intent-to-Treat (ITT) analyses versus Complier Average Causal Effect (CACE) analyses, a novel statistical technique that accounts for and identifies predictors of compliance with treatment in a randomized clinical trial.
2. Methods
2.1. Participants
Inclusion criteria were: (1) mother living with a child between the ages of 2 and 7 years1 ; and (2) meeting DSM-IV criteria for drug and/or alcohol abuse or dependence during the child's lifetime. If there was more than one child in the home between the ages of 2 and 7 years, mothers completed a Child Behavior Checklist (CBCL) (see below) for each child in this age range. Then, we selected the child with the highest score on CBCL Externalizing as the target child. All other child measures were completed about this target child. Target children were 55% male. Sixty-eight percent of families were Caucasian, 30% were African-American, and 2% identified as multiracial.
2.2. Procedures
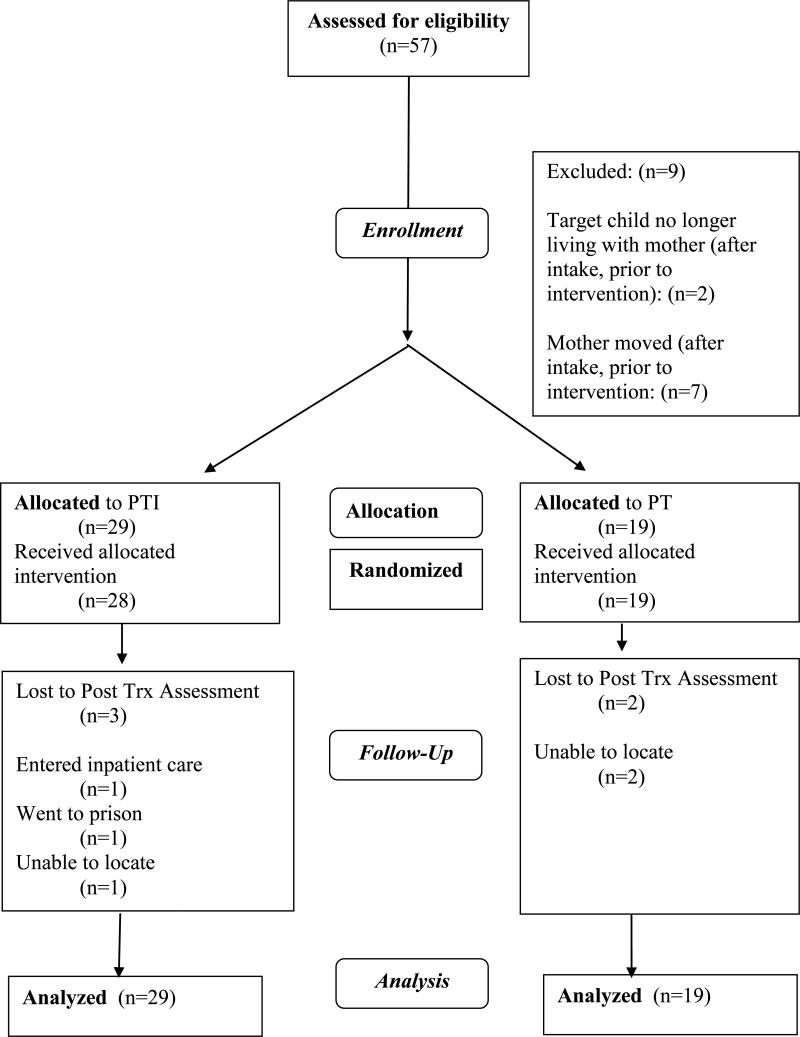
Families were referred by substance abuse treatment agencies, the courts, or were self-referred. Exclusion criteria included: (1) active psychosis, (2) medical or psychiatric illness severe enough to limit participation in the treatment; and (3) child mental retardation or severe developmental problems (e.g., autism). Most women (77%) were in residential treatment at the facility where the groups were held. A total of 57 mothers were assessed, all met inclusion criteria, and 47 mothers enrolled. Mothers were compensated $25 for completing questionnaires pre- and post-treatment. The study was conducted in compliance with the IRB of the University of Arkansas for Medical Sciences; and a Certificate of Confidentiality was obtained from the Department of Health and Human Services (DHHS). Figure 1 illustrates progress through the study phases (CONSORT diagram).
Figure 1.
CONSORT participant flow diagram.
All families participated in 12 2-hour weekly group parent training sessions. PTI mothers also received incentives contingent on treatment compliance. The prize-based incentive program involved earning opportunities to draw for prizes from a computerized bowl containing 250 virtual slips of paper that indicated whether mothers won a prize and its value (Petry et al., 2000). The bowl contained 169 small prize slips ($1 items), 17 medium prize slips ($20 gift card to local stores) and 1 large prize slip ($100 choice of gift cards). Mothers earned 2 draws each for attendance and completing homework. They earned 1 draw for each daily monitoring call about parenting and child behavior (see Daily Tracking below for more details), plus 5 bonus draws if they made one call more than the week before, up to the maximum of 7 calls per week.2
The overall goal of the CM reinforcement schedule was to use a total number of pulls and maximum compensation that was similar to prior research using the fishbowl CM procedure. Thus the fishbowl was designed so that each pull would earn on average $2.44, similar to Petry et al. (2000), and parents earning the maximum 16 pulls would be expected to earn at least one medium prize ($20) on average (each drawing provides an approximately 1/16 chance of winning a $20 prize). Using an incentive of 2 pulls (expected earnings of $5) for session attendance was similar to compensation we have used successfully in prior treatment studies to equalize attendance across groups receiving incentives for attendance only and attendance plus other behaviors (Stanger et al., 2009, Budney et al., 2006). We chose to match the compensation available for weekly homework completion and attendance. For the daily call, we chose to compensate parents for each call at the minimum number of pulls (1). We modeled this procedure on the Petry et al. (2000) fishbowl schedule, where subjects earned 1 draw per day for abstinence, with a bonus of 5 draws for 5 consecutive days (1 treatment week) of abstinence. We hypothesized that a shaping procedure would be more effective in generating a high rate of calling (e.g., Preston et al., 2001), thus we chose to use the bonus pulls to both reward gradual improvements in behavior over baseline levels and to sustain high levels of calling once achieved.
Small and medium prizes were redeemed immediately. Participants had the option of selecting 5 medium prizes as a large prize, or requesting a different $100 prize that would be purchased and available at the next session. Mothers earned an average of 91 draws, or an average of $252.19. PT mothers received monetary incentives for completing the assessments only.
2.2.1. Daily tracking
All mothers called a computerized Interactive Voice Response (IVR) system daily. Mothers without a telephone were provided with a prepaid cell phone (n=4) or with a prepaid phone card (n=1). The IVR system used TeleSage survey software. Calls lasted approximately 3-5 minutes and mothers rated their child's conduct problems and their parenting for the past 24 hours. All items were rated on a 3-step response scale (0=not true today, 1=somewhat or sometimes true today, 2=very or often true today). Included were externalizing items from the Child Behavior Checklist (CBCL) and items from the Parenting Scale (description of measures below). Items were divided into three forms administered on consecutive days to reduce daily call length. The percentage of calls made was used as the measure of daily tracking compliance in analyses. Item responses during calls were not used due to a high percentage of missing data and the association of call compliance with treatment condition (see Results).
2.3. Measures
2.3.1. Mother and child behavior
Current and lifetime diagnosis of maternal substance abuse or dependence, as well as maternal mental health diagnoses were assessed using the Vermont Structured Diagnostic Interview (Hudziak et al., 2004), which was administered by a master's level research assistant. We assessed substance abuse and dependence for each substance with reported lifetime use, and assessed Antisocial Personality Disorder (ASPD), Attention-Deficit/Hyperactivity Disorder (ADHD), Major Depression, and Generalized Anxiety Disorder (GAD). Reliability and validity have been established (Hudziak et al., 2004).
Maternal internalizing and externalizing problems were further assessed using the Adult Self-Report (ASR; Achenbach and Rescorla, 2003), a widely used self-report measure of adult behavioral and emotional problems. Mothers rated 126 items as 0 (not true), 1 (somewhat true), or 2 (very true) of themselves. Raw scores were converted into T scores, and the internalizing and externalizing T scores were used in analyses.
Child internalizing and externalizing problems were assessed using the age-appropriate Child Behavior Checklist (CBCL 1/2-5 and CBCL 6-18: Achenbach and Rescorla, 2000; 2001) completed by mothers. In both versions, mothers rated 100 or 113 (respectively) items as 0 (not true), 1 (somewhat true), or 2 (very true) of their child. Given that the number of items within the individual scales varies across these 2 versions of the CBCL, raw scores were converted to T scores in analyses of child internalizing and externalizing problems.
2.3.2. Parenting
Mothers completed the Parenting Scale (PS; Arnold et al., 1993), a 30-item, 7-point questionnaire for assessing parenting practices related to disruptive behavior problems in children ages 2-5. The PS includes three subscales: Lax, Over-reactive, and Hostile (Rhoades and O'Leary, 2007). Mean item scores were calculated for each scale. Higher scores indicate poorer parenting. This scale has established internal consistency and test-retest reliability (Arnold et al., 1993). This measure was not collected for 9 children ages 6-7, as a different parenting measure was used for children over 6.
2.3.3. Treatment integrity and parent satisfaction
Each group was co-lead by 2 female, master's level counselors who were certified by Incredible Years staff. All group sessions were videotaped to enhance the supervision process and ensure treatment integrity. Therapists attended weekly 2-hour supervision meetings throughout the project. Mothers completed the Parent Satisfaction Questionnaire (Webster-Stratton, 1998), rating the overall program and the difficulty and usefulness of the teaching format and the specific topics covered (e.g., praise, ignoring, time-out). Questions were rated on a 7-point Likert scale.
2.3.4. Research Design and Analyses
The first group was randomly assigned to PTI. Subsequent groups alternated between PT and PTI. This method was used for treatment assignment to ensure roughly equal assignment to both conditions. Groups were conducted consecutively. Five groups were conducted: 3 PTI (n=28 mothers) and 2 PT (n=19 mothers). All 47 families completed the CBCL and ASR at pre-treatment. At post-treatment, 5 families (3 PTI, 2 PT) did not participate.
T-tests were used to compare conditions on number of group sessions attended, number of homework assignments completed, and percent of daily calls made. Child internalizing and externalizing, maternal internalizing and externalizing, and over-reactive, lax, and hostile parenting were compared in Intent-to-Treat (ITT) analyses, controlling for pre-treatment scores. ITT analyses may underestimate active intervention components, due to biased estimates that result from combining individuals who do and do not comply with treatment in the experimental condition. Thus, in addition, we conducted a series of Complier Average Causal Effect (CACE) mixture models to test the effect of PTI among individuals who complied with treatment (Connell, 2009; Jo, 2002a).3 These analyses compare outcomes for individuals in the experimental condition (PTI) who complied with treatment to outcomes for individuals in the control condition who would have complied with the treatment given the opportunity to do so (Connell, 2009). Overall, power is similar in CACE and ITT models. Noncompliance and overall variance reduces power in both types of models, differences between outcome means in complier and noncomplier groups reduces power in ITT models, but increases power in CACE models, and including covariates that are associated with compliance increases power in CACE models (Jo, 2002b).
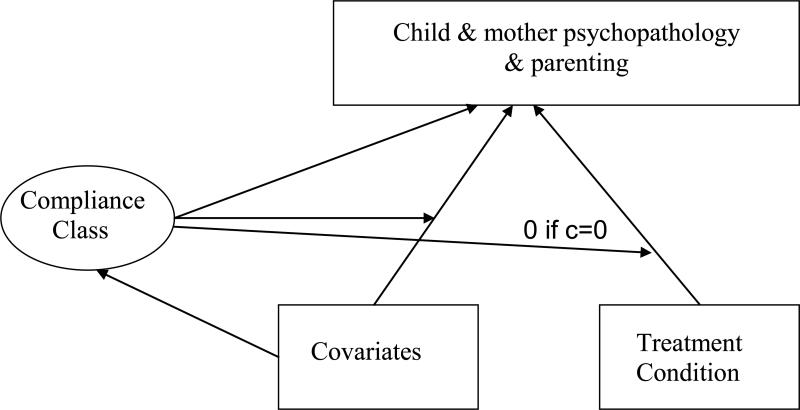
We tested models using 3 definitions of compliance, all based on session attendance (treatment exposure): attending >4 sessions (91% of PTI mothers), ≥8 sessions (85% of PTI mothers), and all 12 sessions (62% of PTI mothers). For CACE models, compliance is known in the intervention condition (i.e. the PTI condition), but is considered unknown/missing in the control condition (the PT condition), as PT participants did not have the opportunity to comply with PTI (see Connell, 2009 for more details). In each CACE model (see Figure 2), treatment was allowed to predict only the outcomes for the complier class, with the treatment effect set to 0 for the non-complier class. Initial CACE models also included treatment assignment and pre-treatment scores as predictors.
Figure 2.
Complier Average Causal Effects model.
Next, the CACE models were extended to include covariates (SES, child age, and gender) as predictors of treatment outcomes and compliance.4 Finally, we examined the tenability of the assumption of no effect of PTI among non-compliers. All analyses were conducted using Mplus 5.3 (Muthen and Muthen, 1998-2007), using full information maximum likelihood estimation and all available data.
3. Results
3.1. Participant Characteristics
Demographic, child mental health, and mother substance use and mental health characteristics were similar across conditions (see Table 1). There were no significant demographic differences between treatment conditions. Rates of current maternal mental health diagnoses were similar in both conditions. However, more PTI mothers had clinical range ASR internalizing scores.
Table 1.
Maternal and Child Pre-treatment Demographic Characteristics, Psychopathology, and Maternal Substance Use
| Treatment Condition | |||
|---|---|---|---|
| Pre-Treatment Variables | PT N=19 M (SD) or N (%) | PTI N=28 M (SD) or N (%) | F or X2a |
| Maternal Age | 30.1 (6.5) | 29.9 (6.0) | 0.01 |
| SES (9 step scale)b | 3.5 (1.5) | 3.4 (1.5) | 0.01 |
| Number of Children in Family | 1.8 (1.1) | 2.0 (0.8) | 0.19 |
| % Single/Separated/Divorced/Widowed | 14 (74%) | 23 (82%) | 0.49 |
| Child Age | 3.8 (1.5) | 3.6 (1.5) | 0.02 |
| Child Gender | |||
| Male | 11 (58%) | 15 (54%) | 0.77 |
| Child Ethnicity | |||
| Caucasian | 13 (68%) | 19 (68%) | 1.60 |
| African American | 5 (26%) | 9 (32%) | |
| Multi-ethnic | 1 (4%) | 0 (0%) | |
| CBCL Internalizing Clinical Range | 2 (11%) | 10 (36%) | 3.78 |
| CBCL Externalizing Clinical Range | 6 (32%) | 10 (36%) | 0.09 |
| Current Maternal Substance Use Diagnoses | |||
| Alcohol Abuse or Dependence | 2 (11%) | 10 (36%) | 3.78 |
| Marijuana Abuse or Dependence | 2 (11%) | 5 (18%) | 0.48 |
| Methamphetamine Abuse or Dependence | 6 (32%) | 5 (18%) | 1.19 |
| Cocaine Abuse or Dependence | 3 (16%) | 6 (21%) | 0.23 |
| Opiate Abuse or Dependence | 4 (21%) | 4 (14%) | 0.37 |
| Sedative Abuse or Dependence | 2 (11%) | 3 (11%) | 0.001 |
| Used Drugs or Alcohol in Past 30 days | 6 (31.6%) | 12 (44.4%) | 0.78 |
| Past or Current Substance Abuse Treatment | |||
| None | 3 (16%) | 1 (3.5%) | 4.8 |
| Current Residential | 12 (63%) | 24 (86%) | |
| Current Outpatient | 2 (10.5%) | 2 (7%) | |
| Past Inpatient/Residential | 2 (10.5%) | 1 (3.5%) | |
| ASR Internalizing Clinical Range | 4 (21%) | 16 (57%) | 6.03* |
| ASR Externalizing Clinical Range | 9 (47%) | 18 (64%) | 1.33 |
| Maternal Mental Health Diagnoses | |||
| ASPD | 5 (26%) | 8 (29%) | 0.03 |
| ADHD | 6 (32%) | 7 (25%) | 0.24 |
| Major Depression | 4 (21%) | 7 (25%) | 0.10 |
| GAD | 1 (5%) | 6 (21%) | 2.33 |
| Sessions Attended | 10.2 (3.2) | 9.4 (3.2) | 0.69 |
| Assignments Completed | 5.4 (2.9) | 5.0 (3.1) | 0.2 |
| Percent Calls Made | 21% (23%) | 41% (28%) | 6.9* |
| Satisfaction Scores | 6.1 (7.4) | 6.2 (0.5) | 0.32 |
Notes :
p < 0.05.
** p < 0.01.
*** p < 0.001.
F ratios for continuous variables/X2 for categorical variables
Score of 3 on the (Hollingshead, 1975) scale represents the following types of occupations: hairdressers, child care workers, cosmetologists; PT=Parent Training only; PTI=Parent Training + Incentives; ASPD=Antisocial Personality Disorder; ADHD = Attention Deficit Hyperactivity Disorder; GAD = Generalized Anxiety Disorder; CBCL=Child Behavior Checklist -CBCL 1/2-5 & CBCL 6-18; ASR=Adult Self Report; Clinical Range=T scores ≥60; SES=socioeconomic status; M= mean; SD = standard deviation.
3.2 Attendance, Homework, Calls, and Satisfaction: Impact of Incentives
Rates of attendance and homework completion did not differ significantly between the PTI and PT conditions (see Table 1). The number of daily tracking calls made was significantly different across conditions, with PTI mothers making on average 41% of the possible calls versus 21% for PT mothers. Overall, satisfaction with treatment was high and similar in both conditions, with average scores of 6 on a 7-step scale.
3.3 Treatment Condition Effects on Child and Mother Problems and Parenting
3.3.1 Intent-to-Treat Analyses
Table 2 shows the pre- and post-treatment means for each outcome measure. In ITT analyses controlling for pre-treatment scores of each outcome, PTI families showed significantly lower child externalizing scores, but did not show significant post-treatment differences in child internalizing, maternal psychopathology or parenting (see Table 3).
Table 2.
Pre- and Post-Treatment Child and Maternal Problems and Parenting
| PT | PTI | |||
|---|---|---|---|---|
| Pre M (SD) | Post M (SD) | Pre M (SD) | Post M (SD) | |
| Child Behavior | N=19 | N=16 | N=28 | N=25 |
| Internalizing | 46.8 (9.2) | 49.3(9.5) | 54.7(12.1) | 49.0(10.9) |
| Externalizing | 51.2 (14.7) | 55.7(13.3) | 55.9(15.3) | 51.0(10.9) |
| Adult Self-Report | N=19 | N=12 | N=28 | N=25 |
| Internalizing | 54.6 (9.9) | 56.9(10.9) | 62.4(11.7) | 55.7(12.8) |
| Externalizing | 58.9(11.0) | 56.2(10.1) | 62.7(11.7) | 57.5(12.2) |
| Parenting Scale | N=17 | N=15 | N=21 | N=18 |
| Over-reactive Parenting | 3.3(1.1) | 2.5(1.3) | 3.3 (0.9) | 2.6(1.1) |
| Lax Parenting | 3.4(1.3) | 2.5(1.0) | 3.5(1.4) | 2.5(1.1) |
| Hostile Parenting | 2.3(0.9) | 1.8(0.8) | 1.9(0.9) | 1.7(0.8) |
Notes : aNs are lower for the Pre-treatment Parenting Scale, which is missing by design for 9 children ages 6 and older, PT=Parent Training only; PTI=Parent Training + Incentives; M= mean; SD = standard deviation.
Table 3.
Intent-to-Treat (ITT) and Complier Average Causal Effects (CACE) Models
| Treatment Effects: ITT versus CACE Models |
||||||||
|---|---|---|---|---|---|---|---|---|
| ITT | Compliance = Attend >4 sessions | Compliance = Attend ≥8 sessions | Compliance = Attend 12 sessions | |||||
| Outcome Variables | β | SE | β | SE | β | SE | β | SE |
| CBCL Internalizing | -0.24 | 0.13 | -0.28 | 0.15 | -0.32* | 0.16 | -0.57 | 0.30 |
| CBCL Externalizing | -0.33** | 0.11 | -0.37* | 0.14 | -0.42* | 0.18 | -0.84*** | 0.13 |
| ASR Internalizing | -0.22 | 0.15 | -0.25 | 0.16 | -0.26 | 0.16 | -0.42* | 0.17 |
| ASR Externalizing | -0.04 | 0.13 | -0.08 | 0.11 | -0.05 | 0.16 | -0.08 | 0.30 |
| PS Over-reactive Parenting | 0.04 | 0.17 | 0.06 | 0.19 | 0.06 | 0.19 | -0.73*** | 0.17 |
| PS Lax Parenting | -0.03 | 0.16 | -0.03 | 0.16 | -0.03 | 0.16 | -0.09 | 0.40 |
| PS Hostile Parenting | -0.04 | 0.16 | 0.03 | 0.18 | 0.03 | 0.18 | -0.42 | 0.26 |
Notes :
p < 0.05.
p < 0.01.
p < 0.001.
PTI=Parent Training + Incentives; β=standardized parameter estimate; SE=Standard Error. N=41 for child internalizing and externalizing outcomes; N=37 for mother internalizing and externalizing outcomes; N=33 for parenting outcomes. Pre-treatment score was controlled in all 4 models. CBCL=Child Behavior Checklist - CBCL 1/2-5 & CBCL 6-18; ASR=Adult Self Report; PS=Parenting Scale; Estimates are identical for the three PS scales in the Compliance ≥4 and ≥8 models because all participants with an end of treatment Parenting Scale attended at least 8 sessions.
3.3.2. CACE Analyses
The CACE models indicated significant effects of PTI on child internalizing and externalizing and maternal internalizing and over-reactive parenting (see Table 3). As the criterion for compliance in each model increased from more than 4 to 8 to 12 sessions, the PTI effects consistently increased and were significant in each model for child externalizing symptoms. A similar pattern was observed for child internalizing, and the estimate was significant for the 8 session compliance model. For maternal internalizing symptoms, the estimate was significant for the full complier class who completed 12 sessions of treatment. In addition, the effect of PTI on over-reactive parenting was significant for the 12 sessions compliance model.
3.3.3 CACE Analyses with Inclusion of Covariates
Because it showed the largest effects of PTI, the 12-session compliance CACE model was expanded to test the effects of treatment plus additional demographic predictors of both treatment outcome and compliance. Controlling for the covariates, the effects of PTI were large and significant on child internalizing and externalizing, maternal internalizing, as well as over-reactive parenting. 5 Pre-treatment scores were significantly related to child internalizing and child externalizing outcomes, as well as maternal internalizing and externalizing outcomes, but not parenting outcomes. There were few significant relations between the demographic predictors and outcomes. Higher SES predicted less lax parenting, having a younger target child predicted higher maternal internalizing scores, but lower child internalizing scores, and male children had higher internalizing and externalizing scores. Predictors of less than full compliance included higher pre-treatment maternal externalizing scores and higher over-reactive parenting, but there were no significant effects of SES, child age, or child gender on compliance.6
3.3.4 CACE Analyses Testing Treatment Effects for Noncompliers
In the presence of covariates, we also tested whether it is tenable to assume random assignment to treatment does not affect the outcomes of individuals who did not attend all 12 sessions by allowing treatment condition to predict outcomes for mothers who did not attend all sessions (the non-compliance class). In these models, relaxing the exclusion restriction did not affect the magnitude of the PTI effect on child externalizing (β = -0.82, Standard Error(SE)=.12; p < 0.001), child internalizing (β = -0.47, SE=.18; p < 0.01), mother's internalizing (β = -0.42, SE=.15; p < 0.01), and maternal over-reactive parenting (β = -0.69, SE=.25; p < 0.01) for mothers completing 12 sessions of treatment. Results also showed that relaxing the exclusion restriction revealed an effect of PTI on maternal hostile parenting (β = .71, SE=.19; p < 0.001), but not for maternal lax parenting (β = 0.17, SE=.37; p = ns) or externalizing symptoms (β = -0.19, SE=.16; p = ns). The effect of PTI was significant, but much smaller on child externalizing symptoms (β = -0.17, SE=.06; p < 0.01) for mothers who did not complete 12 sessions of treatment. Further, effects of PTI were not significant on child internalizing symptoms, maternal internalizing and externalizing symptoms, or parenting for mothers who did not complete 12 sessions. These results support the exclusion restriction and indicate that the effects of PTI are much smaller among mothers who do not attend all sessions.
4. Discussion
Overall, children of mothers who received parent training plus the CM program targeting treatment compliance (PTI) showed a greater reduction in externalizing behavior problems over the course of treatment than children of mothers who received parent training alone. These results were consistent in the ITT and CACE analyses, with larger effects in the CACE models. In the ITT analyses, PTI mothers did not show greater improvements in psychopathology or parenting practices. However, CACE analyses indicated greater reductions in child internalizing and in maternal internalizing symptoms and over-reactive parenting when mothers received PTI. A recent prevention research study comparing ITT to CACE analyses also found stronger treatment effects in CACE analyses compared to ITT analyses (Connell, 2009).
Two features of CACE analyses highlight the possible reasons for these divergent results (Little et al., 2009). First, ITT analyses provide estimates of the effect of treatment assignment, whereas, CACE analyses provide estimates of receiving treatment. Thus, these results suggest that some improvements in child behavior can result from less than the full parent training curriculum. However, improvements are larger and more pervasive among families completing the entire curriculum. Second, ITT analyses do not accurately estimate treatment effects in the presence of less than full compliance on the part of all participants. CACE analyses provide a correction for these biased estimates.
When the PTI treatment effect was examined among 3 complier classes in CACE models (i.e., treatment attendance > 4, ≥8 , and 12 sessions), a “dose” response was observed for child internalizing and externalizing symptoms and maternal internalizing symptoms, revealing a clear pattern of increasing treatment effect as the number of sessions attended increased. This is consistent with Webster-Stratton et al. (2001) which showed that outcomes were significantly better for at-risk preschool children of mothers who attended 6 or more of 12 Incredible Years sessions. It is important to note, however, that full 12-session compliance was impacted by pre-treatment levels of maternal externalizing symptoms and maternal over-reactive parenting. These results suggest that mothers who use substances and have co-occurring externalizing symptoms or an over-reactive parenting style may be an important subgroup to identify at treatment intake so additional services might be offered to boost treatment compliance.
Of note, across several outcome measures (child internalizing and externalizing, and parent internalizing), mean scores for the PT only condition worsened from pre to post treatment. However, none of these changes were statistically significant in t-tests conducted separately for the PT condition. Without a no-treatment control, the meaning of this pattern of increasing problems over time is susceptible to alternative explanations. Despite the lack of significance, this pattern is unexpected, and is important to test in future studies.
Our hypothesis that PT plus incentives would improve compliance relative to PT alone received partial, preliminary support. Specifically, compliance with daily tracking of child behavior and parenting was significantly greater among the PTI families, but no effects were observed on attendance or homework completion. PTI mothers used the daily monitoring system on close to 40% of days, twice as often as PT mothers. Because the effect of the incentives was isolated to daily monitoring, it is likely that this daily intervention, combined with weekly in-group feedback graphs, contributed significantly to the better outcomes observed in PTI families. These findings are consistent with studies showing a positive impact of providing both clients and therapists with weekly feedback reports (Harmon et al., 2005; Slade et al., 2008). However, in our study, mothers in both conditions received weekly graphs showing mean child behavior and parenting scores for each week of treatment, but mothers who received incentives for making the calls on which the graphs were based (and consequently made more calls), showed the largest improvements.
Completion of home practice assignments and attendance were similar in the PTI and PT condition. Overall, rates of attendance for mothers were quite high in both conditions, likely due to our assertive outreach and the nature of the sample (most women were in residential substance abuse treatment with their children during the intervention). Mean attendance of 9 to 10 sessions across the two conditions in this study compares favorably to an average attendance of 7 sessions across several studies testing Incredible Years in Head Start settings (Baydar et al., 2003). However, given the results suggesting that full attendance has significant effect on outcomes, future research might test alternative schedules to boost rates of full attendance, such as an escalating schedule of reinforcement, with a reset contingency (Petry, 2000; Roll et al., 1996).
Rates of assignment completion showed room for improvement across conditions. It is not possible to compare the rates of assignment completion directly to other preschool samples because we are not aware of studies reporting that information specifically. However, as assignment completion is an important component of engagement that has been shown to predict outcomes (Baydar et al., 2003), it is important to explore ways to increase it. Our results suggest that an alternative schedule of reinforcement should be tested. Options include using an escalating schedule of reinforcement and/or larger magnitude incentives. Multiple studies testing CM interventions for adult substance abusers have reinforced the completion of activities related to treatment goals (e.g., Petry et al., 2006; Petry et al., 2000). However, in all these studies activities are only assigned to and tracked in those participants receiving incentives for completing them. Thus, it is not possible to isolate the impact of these procedures on completion of such activities in prior studies.
Limitations
The current study had several limitations that warrant comment. The primary limitation is the small sample size. Studies using structural equation modeling with small sample sizes have some drawbacks. Most notably, the fit function may fail to converge or generate an improper solution (e.g., out-of-range parameter estimates) and accuracy of parameter estimates and related sampling variability issues are of concern. However, Marsh and Hau (1999) suggest that problems associated with small sample sizes in SEM analyses are largely negated by increasing the number of observed variables (for example, model covariates). Consistent with this suggestion, all CACE models reported in our study converged properly and the parameter estimates were within the parameter space (i.e., solutions were proper). However, the standard errors of all estimates are relatively large, due to the sample size, and our results need to be replicated with a larger sample in future studies. Second, outcomes were assessed only at the end of treatment in this initial trial. Longer term follow ups will be necessary in future research to assess the durability of these effects. Third, given that treatment took place at a residential facility, the present findings may have limited generalizability. Fourth, the present study relied on maternal report for all outcomes. Fifth, both ITT and CACE analyses assume that potential outcomes for each participant are independent of the outcomes for other participants. In this study, group members could have influenced one another. However, the sample size was too small to test or control within-group associations.
4.2. Conclusion
This study is important because there are few controlled trials testing the impact of interventions designed to reduce identifiable risks for young children in families who abuse substances. We provide preliminary support for augmenting an evidence-based parent training treatment with our novel incentive program as a possible prevention strategy for children at risk for developing externalizing and internalizing problems. Incentive-based CM programs that have demonstrated much success in improving outcomes among adults with drug dependence disorders, may offer an effective method for preventing and reducing children's externalizing and internalizing problems in these high-risk families. Our analyses revealed significant decreases in CBCL internalizing and externalizing symptoms, demonstrating a possible preventive effect of treatment. To our knowledge, this is the first study to examine the impact of systematically monitoring child behavior and parenting between sessions and to implement a strategy for increasing this behavior.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Fifty-one percent (n=24) of mothers reported that there was a co-parenting adult living in the home. Of the 24 reporting a co-parent, 19 gave permission to contact the co-parent to request their participation in the parenting group. Of those co-parents contacted, 9 (6 male partners and 3 grandmothers) participated in the parenting groups (6 in PTI and 3 in PT). Overall, 19% of families had 2-adult participation, 21% in PTI and 16% in PT (see Table 1). Because co-parent participation was low, current analyses focus on mothers only.
PTI mothers could earn a maximum of 177 draws over the course of treatment: (12 sessions × 2 draws=24) + (11 homework assignments × 2 draws=22) + (6 daily calls in week 1 × 1 draw per call=6) + (7 daily calls per week in weeks 2-11 × 1 draw per call=70) + (11 weekly call bonuses × 5 draws=55).
There are 5 assumptions that underlie CACE analyses (Connell, 2009): (1) potential outcomes for each participant are independent of the outcomes for other participants, (2) a monotonic relationship exists between treatment assignment and treatment receipt, (3) offering treatment to participants in the intervention condition induces at least some participants to receive treatment, so the compliance is not zero, (4) assignment to the intervention condition is random, and (5) random assignment to treatment does not affect the outcomes of individuals who do not comply with treatment.
Mother ethnicity and residential status were included in preliminary analyses, but were excluded from the final analyses due to lack of variability in their distribution, as well as showing minimal effects in predicting the mother and child psychopathology and parenting outcomes.
Effects of PTI and covariates on child and maternal internalizing and externalizing symptoms and parenting in CACE models for 12 session compliance models are available in Supplementary Materials.
Effects of pre-treatment scores, SES, child gender and age on compliance (12 sessions vs. <12 sessions) are available in Supplementary Materials.
References
- Achenbach TM, Rescorla L. Manual for the ASEBA Preschool Forms and Profiles. University of Vermont Department of Psychiatry; Burlington, VT: 2000. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for ASEBA School-Age Forms and Profiles. University of Vermont, Research Center for Children, Youth, and Families; Burlington, VT: 2001. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA Adult Forms and Profiles. University of Vermont, Research Center for Children, Youth and Families; Burlington, VT: 2003. [Google Scholar]
- Arnold DS, O'Leary SG, Wolff LS, Acker MM. The parenting scale: a measure of dysfunctional parenting in discipline situations. Psychol. Assess. 1993;5:137–144. [Google Scholar]
- Baydar N, Reid MJ, Webster-Stratton C. The role of mental health factors and program engagement in the effectiveness of a preventive parenting program for Head Start mothers. Child Dev. 2003;74:1433–1453. doi: 10.1111/1467-8624.00616. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Amass L, Higgins ST, Badger GJ, Esch RA. Effects of adding a behavioral treatment to opioid detoxification with buprenorphine. J. Consult. Clin. Psychol. 1997;65:803–810. doi: 10.1037//0022-006x.65.5.803. [DOI] [PubMed] [Google Scholar]
- Brown EC, Catalano RF, Fleming CB, Haggerty KP, Abbott RD. Adolescent substance use outcomes in the Raising Healthy Children project: a two-part latent growth curve analysis. J. Consult. Clin. Psychol. 2005;73:699–710. doi: 10.1037/0022-006X.73.4.699. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Moore BA, Rocha HL, Higgins ST. Clinical trial of abstinence-based vouchers and cognitive-behavioral therapy for cannabis dependence. J Consult Clin Psychol. 2006;74:307–316. doi: 10.1037/0022-006X.4.2.307. [DOI] [PubMed] [Google Scholar]
- Clark DB, Cornelius JR, Wood DS, Vanyukov M. Psychopathology risk transmission in children of parents with substance use disorders. Am. J. Psychiatry. 2004;161:685–691. doi: 10.1176/appi.ajp.161.4.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conduct Problems Prevention Research Group Initial impact of the Fast Track Prevention Trial for conduct problems: I. The high-risk sample. J. Consult. Clin. Psychol. 1999;67:631–647. [PMC free article] [PubMed] [Google Scholar]
- Connell AM. Employing complier average causal effect analytic methods to examine effects of randomized encouragement trials. Am. J. Drug Alcohol Abuse. 2009;35:253–259. doi: 10.1080/00952990903005882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst CC, Grant TM, Streissguth AP, Sampson PD. Intervention with high risk alcohol and drug-abusing mothers: II. Three-year findings from the Seattle Model of Paraprofessional Advocacy. J. Community Psychol. 1999;27:19–38. [Google Scholar]
- Harmon C, Hawkins EJ, Lambert MJ, Slade K, Whipple JL. Improving outcomes for poorly responding clients: the use of clinical support tools and feedback to clients. J. Clin. Psychol. 2005;61:175–185. doi: 10.1002/jclp.20109. [DOI] [PubMed] [Google Scholar]
- Heinrichs N. The effects of two different incentives on recruitment rates of families into a prevention program. J. Prim. Prev. 2006;27:345–365. doi: 10.1007/s10935-006-0038-8. [DOI] [PubMed] [Google Scholar]
- Heinrichs N, Jensen-Doss A. The effects of incentives on families’ long-term outcomes in a parenting program. J. Clin. Child Adolesc. Psychol. 2010;39:705–712. doi: 10.1080/15374416.2010.501290. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Silverman K, Heil SH. Contingency Management in Substance Abuse Treatment. The Guilford Press; New York, NY: 2008. [Google Scholar]
- Hollingshead AB. Department of Sociology. Yale University; New Haven, CT: 1975. Four Factor Index of Social Status. [Google Scholar]
- Hudziak JJ, Copeland W, Stanger C, Wadsworth M. Screening for DSM-IV externalizing disorders with the Child Behavior Checklist: a receiver-operating characteristic analysis. J. Child Psychol. Psychiatry. 2004;45:1299–1307. doi: 10.1111/j.1469-7610.2004.00314.x. [DOI] [PubMed] [Google Scholar]
- Huebner CE. Evaluation of a clinic-based parent education program to reduce the risk of infant and toddler maltreatment. Public Health Nurs. 2002;19:377–389. doi: 10.1046/j.1525-1446.2002.19507.x. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Wirth RJ, Edwards MC, Curran PJ, Chassin LA, Zucker RA. Externalizing symptoms among children of alcoholic parents: entry points for an antisocial pathway to alcoholism. J. Abnorm. Psychol. 2007;116:529–542. doi: 10.1037/0021-843X.116.3.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iguchi MY, Belding MA, Morral AR, Lamb RJ, Husband SD. Reinforcing operants other than abstinence in drug abuse treatment: an effective alternative for reducing drug use. J. Consult. Clin. Psychol. 1997;65:421–428. doi: 10.1037//0022-006x.65.3.421. [DOI] [PubMed] [Google Scholar]
- Irvine AB, Biglan A, Smolkowski K, Metzler CW, Ary DV. The effectiveness of a parenting skills program for parents of middle school students in small communities. J. Consult. Clin. Psychol. 1999;67:811–825. doi: 10.1037//0022-006x.67.6.811. [DOI] [PubMed] [Google Scholar]
- Jo B. Estimation of intervention effects with noncompliance: alternative model specifications. J. Ed. Behav. Stats. 2002a;27:385–409. [Google Scholar]
- Jo B. Statistical power in randomized intervention studies with noncompliance. Psychol. Methods. 2002b;7:178–193. doi: 10.1037/1082-989x.7.2.178. [DOI] [PubMed] [Google Scholar]
- Kerwin ME. Collaboration between child welfare and substance-abuse fields: combined treatment programs for mothers. J. Pediatr. Psychol. 2005;30:581–597. doi: 10.1093/jpepsy/jsi045. [DOI] [PubMed] [Google Scholar]
- Kumpfer KL, DeMarsh J. Family environmental and genetic influences on children's future chemical dependency. J. Children Contemp. Society. 1985;18:49–91. [Google Scholar]
- Lam WK, Fals-Stewart W, Kelley ML. Effects of Parent Skills Training with Behavioral Couples Therapy for alcoholism on children: a randomized clinical pilot trial. Addict. Behav. 2008;33:1076–1080. doi: 10.1016/j.addbeh.2008.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJ, Long Q, Lin X. A comparison of methods for estimating the causal effects of a treatment in randomized clinical trials subject to noncompliance. Biometrics. 2009;65:640–649. doi: 10.1111/j.1541-0420.2008.01066.x. [DOI] [PubMed] [Google Scholar]
- Loukas A, Zucker RA, Fitzgerald HE, Krull JL. Developmental trajectories of disruptive behavior problems among sons of alcoholics: effects of parent psychopathology, family conflict, and child undercontrol. J. Abnorm. Psychol. 2003;112:119–131. [PubMed] [Google Scholar]
- Luthar SS, Suchman NE. Relational Psychotherapy Mothers’ Group: a developmentally informed intervention for at-risk mothers. Dev. Psychopathol. 2000;12:235–253. doi: 10.1017/s0954579400002078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Suchman NE, Altomare M. Relational Psychotherapy Mothers’ Group: a randomized clinical trial for substance abusing mothers. Dev. Psychopathol. 2007;19:243–261. doi: 10.1017/S0954579407070137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Walsh KG. Treatment needs of drug-addicted mothers: integrated parenting psychotherapy interventions. J. Subst. Abuse Treat. 1995;12:341–348. doi: 10.1016/0740-5472(95)02010-1. [DOI] [PubMed] [Google Scholar]
- Marsh HW, Hau KT. Confirmatory factor analysis: strategies for small sample sizes. In: Hoyle RH, editor. Strategies for Small Sample Research. Sage; Thousand Oaks, CA: 1999. [Google Scholar]
- Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychol. Rev. 1993;100:1–28. [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus User's Guide. Fifth Edition Muthen and Muthen; Los Angeles, CA: 1998-2007. [Google Scholar]
- Nye CL, Zucker RA, Fitzgerald HE. Early intervention in the path to alcohol problems through conduct problems: treatment involvement and child behavior change. J. Consult. Clin. Psychol. 1995;63:831–840. doi: 10.1037//0022-006x.63.5.831. [DOI] [PubMed] [Google Scholar]
- Petry NM. A comprehensive guide to the application of contingency management procedures in clinical settings. Drug Alcohol Depend. 2000;58:9–25. doi: 10.1016/s0376-8716(99)00071-x. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Carroll KM, Hanson T, MacKinnon S, Rounsaville B, Sierra S. Contingency management treatments: reinforcing abstinence versus adherence with goal-related activities. J. Consult. Clin. Psychol. 2006;74:592–601. doi: 10.1037/0022-006X.74.3.592. [DOI] [PubMed] [Google Scholar]
- Petry NM, Martin B, Cooney JL, Kranzler HR. Give them prizes, and they will come: contingency management for treatment of alcohol dependence. J. Consult. Clin. Psychol. 2000;68:250–257. doi: 10.1037//0022-006x.68.2.250. [DOI] [PubMed] [Google Scholar]
- Preston KL, Umbricht A, Wong CJ, Epstein DH. Shaping cocaine abstinence by successive approximation. J. Consult. Clin. Psychol. 2001;69:643–654. doi: 10.1037//0022-006x.69.4.643. [DOI] [PubMed] [Google Scholar]
- Reid MJ, Webster-Stratton C, Baydar N. Halting the development of conduct problems in head start children: the effects of parent training. J. Clin. Child Adolesc. Psychol. 2004;33:279–291. doi: 10.1207/s15374424jccp3302_10. [DOI] [PubMed] [Google Scholar]
- Rhoades KA, O'Leary SG. Factor structure and validity of the parenting scale. J. Clin. Child Adolesc. Psychol. 2007;36:137–146. doi: 10.1080/15374410701274157. [DOI] [PubMed] [Google Scholar]
- Roll JM, Higgins ST, Badger GJ. An experimental comparison of three different schedules of reinforcement of drug abstinence using cigarette smoking as an exemplar. J. Appl. Behav. Anal. 1996;29:495–505. doi: 10.1901/jaba.1996.29-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA . The NSDUH Report: Children Living With Substance-Dependent or Substance-Abusing Parents: 2002 to 2007. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2009. [Google Scholar]
- Schuler ME, Nair P, Black M. Ongoing maternal drug use, parenting attitudes, and a home intervention: effects on mother-child interaction at 18 months. J. Dev. Behav. Pediatr. 2002;23:87–94. doi: 10.1097/00004703-200204000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade K, Lambert MJ, Harmon SC, Smart DW, Bailey R. Improving psychotherapy outcome: the use of immediate electronic feedback and revised clinical support tools. Clin. Psychol. Psychother. 2008;15:287–303. doi: 10.1002/cpp.594. [DOI] [PubMed] [Google Scholar]
- Stanger C, Budney AJ, Kamon JL, Thostensen J. A randomized trial of contingency management for adolescent marijuana abuse and dependence. Drug Alcohol Depend. 2009;105:240–247. doi: 10.1016/j.drugalcdep.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarter RE, Kirisci L, Habeych M, Reynolds M, Vanyukov M. Neurobehavior disinhibition in childhood predisposes boys to substance use disorder by young adulthood: direct and mediated etiologic pathways. Drug Alcohol Depend. 2004;73:121–132. doi: 10.1016/j.drugalcdep.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C. Preventing conduct problems in Head Start children: strengthening parenting competencies. J. Consult. Clin. Psychol. 1998;66:715–730. doi: 10.1037//0022-006x.66.5.715. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Reid JM, Hammond M. Preventing conduct problems, promoting social competence: a parent and teacher training partnership in Head Start. J. Clin. Child Psychol. 2001;30:283–302. doi: 10.1207/S15374424JCCP3003_2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.