Abstract
Objective
To assess the effectiveness of providing information by post about managing minor illnesses.
Design
Randomised controlled trial.
Setting
Six general practices.
Participants
Random sample of 4002 patients from the practice registers.
Intervention
Patients were randomised to receive one of three kinds of leaflet or booklet endorsed by their general practitioner: control (surgery access times), booklet, or summary card.
Main outcome measures
Attendance with the 42 minor illnesses listed in the booklet. Perceived usefulness of leaflets or booklets, confidence in managing illness, and willingness to wait before seeing the doctor.
Results
238 (6%) patients did not receive the intervention as allocated. Of the remaining 3764 patients, 2965 (79%) had notes available for review after one year. Compared with the control group, fewer patients attended commonly with the minor illnesses in the booklet group (⩾2 consultations a year: odds ratio 0.81, 95% confidence interval 0.67 to 0.99) and the summary card group (0.83; 0.72 to 0.96). Among patients who had attended with respiratory tract infections in the past year there was a reduction in those attending in the booklet group (0.81; 0.62 to 1.07) and summary card group (0.67; 0.51 to 0.89) compared with the control group. The incidence of contacts with minor illness fell slightly compared with the previous year in the booklet (incidence ratio 0.97; 0.84 to 1.13) and summary card groups (0.93; 0.80 to 1.07). More patients in the intervention groups felt greater confidence in managing illness (booklet 32%, card 34%, control 12%, P<0.001), but there was no difference in willingness to wait score (all groups mean=32, P=0.67).
Conclusion
Most patients find information about minor illness provided by post useful, and it helps their confidence in managing illness. Information may reduce the number attending commonly with minor illness, but the effect on overall contacts is likely to be modest. These data suggest that posting detailed information booklets about minor illness to the general population would have a limited effect.
What is already known on this topic
Increasing attendance for minor illness in primary care is a threat to consultation time and quality of care
Few recent studies have examined the effect of providing patients with information on self management of minor illness
What this study adds
Most patients find information about minor illness provided by post useful, and it helps their confidence in managing illness
Information booklets and leaflets reduced the number attending frequently with minor illness, but the effect on overall contacts was not significant
Information booklets on minor illness provided by post may have a limited role in the NHS
Introduction
Increasing attendance in primary care is an important problem for the health service.1 It increases stress on health professionals and has contributed to changing arrangements for out of hours care.2 It is also a potential threat to consultation time and the quality of care provided for patients.3 If changing patient expectations and a demand for advice have contributed to the rising rates of consultation, then providing written information could reduce consultation rates for minor or self limiting illness.
Little is known about the effect of general information leaflets in general practice. Although information leaflets about specific acute illness may enhance patients' ability to manage their own illness and can modify reattendance,4–6 these data cannot necessarily be extrapolated to the provision of general information leaflets. Previous research on providing general patient information in the United Kingdom predates the apparent rise in patient expectations and changes in out of hours arrangements that have occurred in the last 15 years. Nevertheless, the study showed a possible role for provision of information, particularly for younger people.7 A study targeting information at young families in Denmark in a single practice showed a significant reduction in attendance with minor illness,8 and a brochure aimed at new enrollees in a health maintenance organisation in the United States showed modest changes in consultation behaviour.9 However, neither study can be easily applied to patients in typical general practice settings.
We hypothesised that providing information by post about the self management of minor illness and when to contact the doctor could help patients' confidence in managing minor illness, help in their decision to consult the doctor, and hence reduce rates of consultation for minor illness. We report the main results of a randomised controlled trial of two kinds of general patient information about minor illness: an extensive booklet detailing the management of 42 conditions and a two page summary card dealing predominantly with the self management of respiratory illness.
Participants and methods
This study was approved by the Southampton and South West Hants, and Salisbury local research ethics committees. We chose six general practices within a 64 km radius of the administrative centre to give a range of sociodemographic and practice characteristics. We randomly selected 4002 households, sampling equal numbers from the age-sex register of each practice. We randomised at patient level rather than practice level because the evidence suggests that intrapractice contamination is likely to be small even with major practice initiatives10 and to avoid large practice cluster effects. Patients from nursing homes and those older than 80 were excluded as many of this group would have difficulty completing questionnaires. We selected one adult per household to avoid contamination of groups. When the random choice of participant was a child (aged under 16), an adult was asked to complete the questionnaire.
Patients were sent a letter from their doctors explaining that the project was investigating the value of patient information leaflets or booklets and would also involve examining their notes for attendance. Patients were asked not to share the leaflets or booklets with other households. The doctors endorsed the leaflet or booklet enclosed with the letter and encouraged patients to use them before consulting.
Interventions
Patients were randomised to receive one of three types of information.
Booklet group—Patients were sent What Should I Do?, a booklet summarising self management for 42 conditions and when to contact the doctor.11 This booklet is widely used in other areas of the United Kingdom and has been translated into several languages.
Summary card group—Patients were sent a two sided summary of self management. One page dealt with respiratory illnesses and the second page with other common illness. The content of this leaflet was based, when possible, on evidence from trials or systematic reviews. The content was initially drafted by four general practitioners (PL, IW, GW, MM) and then reviewed by the whole study team. The detailed contents of the leaflet were further discussed with patients randomly chosen from the practice lists to ensure that the type and detail of information was appropriate to patients' needs. We modified the leaflet and continued to interview patients until no major suggestions were made.
Control group—Patients received a one page leaflet giving the surgery times and how to contact the doctor in an emergency.
Baseline questionnaire
We enclosed a baseline questionnaire with the letter and the leaflet or booklet. This contained questions on demographic details, attitudes to doctors, the use of the pharmacy and surgery, lifestyle, medical problems, perception of somatic symptoms, health anxiety, and perceived health. Patients who had not returned a completed questionnaire were sent second and third mailings.
Review of notes
We reviewed patients' notes at one year to assess attendances for the minor illnesses listed in the booklet. Notes were assessed by one of two assessors, who were blind to randomisation group. To assess interrater reliability, a sample of 50 consecutive notes was reviewed blindly by both assessors. There was good agreement for the number of attendances with minor illness (rank correlation r=0.99).
We collected attendance data for patients who had not indicated willingness to participate by returning the baseline questionnaire. However, in accordance with General Medical Council guidance on confidentiality, their notes were anonymised within the practice before being released to the researchers. One of the practices was not happy to anonymise notes and applied two further conditions—that only patients who had returned the baseline questionnaire could be approached regarding consent to access their notes and that they could be contacted by post only once. This resulted in low rates of review in that practice (27% of the original sample).
Follow up questionnaire
A follow up questionnaire was sent at one year. All the practices requested that to avoid undue pressure on patients this questionnaire be sent only to those who had returned the original questionnaire. The follow up questionnaire asked whether the patient could remember receiving the booklet, if they had used it, whether they found the information useful, and whether they felt more confident in managing minor illness.
The questionnaire also contained questions about willingness to wait before seeing the doctor. Thirteen questions were included about the number of days people would wait before seeing the doctor for different clinical scenarios. In the sample that returned the baseline questionnaire, factor analysis of these questions with varimax rotation12 suggested a one factor solution that explained 88% of the variance. Seven “usually self-limiting” scenarios loaded strongly on to the factor: headache (factor loading 0.62), constipation (0.67), diarrhoea and vomiting (0.62), indigestion and heartburn (0.66), cold and runny nose (0.64), flu with fever (0.66), sore throat and fever (0.71). The scores for these seven questions (1=less than 1 day; 2=1-2 days; 3=3-7 days; 4=8-14 days; 5=over 14 days; 6=would not contact) were added to give a scale representing willingness to wait, with average interitem covariance of 0.78 and Cronbach's α=0.83 in the optimal range.12 Test-retest reliability after one month for this scale in 30 people was acceptable (r=0.48),13 and in the baseline sample the score was a strong predictor of attendance in both adults and children.
Sample size
To have 80% power and 95% confidence in detecting an average 5% reduction in attendance with the leaflets among those attending commonly for minor illness (twice or more), and assuming a larger effect size with the booklet (30% control, 26.5% summary card, 23.5% booklet), we needed 2673 patients, or a minimum of 3341 in total allowing for 20% loss to follow up. We considered effect sizes smaller than 5% unlikely to be important.
Analysis
We scanned the data using Formic 3 software and analysed them with SPSS and Stata software. We assessed more frequent attendance with minor illness (⩾2 consultations a year, representing 30% of the population) in the year after providing the leaflets or booklets using logistic regression and controlling for attendance in the previous year. Although randomisation at the patient level should balance practice related variables between groups, we also controlled for cluster effects at a practice level because of the potential importance of service factors in predicting attendance, the relatively large clusters from few practices, and the likely clustering of attendance patterns within practices. Because the summary card particularly dealt with respiratory illness, we also assessed whether attendance with minor illness was reduced among patients who had attended with respiratory illness in the past year as a secondary outcome. We also fitted a longitudinal Poisson regression model to estimate the effect of intervention on the change in incidence of consultations with minor illness over time (the incidence ratio); robust estimates of the standard errors were used since the distribution was overdispersed.
Results
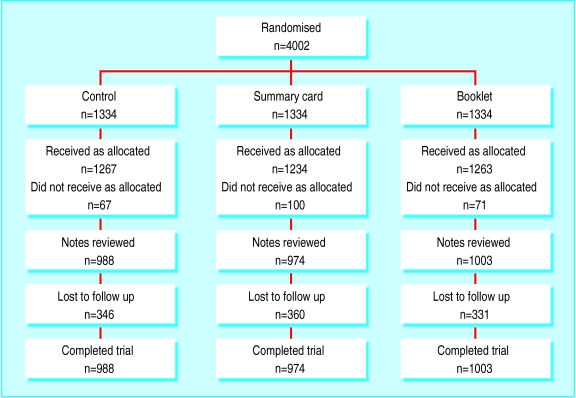
Only 238 (6%) patients were reported not living at that address and thus did not receive the intervention as allocated (figure). Of the remaining 3764 patients, 2719 (72%) returned the baseline questionnaire, and 2965 (79%) had notes available for follow up. Of the 2719 patients eligible to receive a follow up questionnaire, 1975 (73%) returned the follow up questionnaire at one year. The percentage loss to follow up was similar for the control, card, and booklet groups for both notes review (26%, 27%, 25% respectively) and follow up questionnaire (52% (695/1334), 50%, (669/1334), and 50% (663/1334) respectively).
We were able to generate demographic data from the enumeration district for 3476 out of the 3764 baseline sample. These data were used to assess the biases in loss to follow up for notes review and also non-response to the follow up questionnaire compared with the original randomised sample (table 1). Those not followed up for both notes review and questionnaire were younger than those who were followed up and more were in manual occupations. However, compared with the original sample, those who were followed up for both the notes review and questionnaire had similar characteristics to the original sample.
Table 1.
Baseline characteristics and characteristics of those followed up compared with original randomised sample
| Baseline characteristics | Booklet | Summary card | Control | Review of notes
|
Questionnaire at 1 year
|
|||
|---|---|---|---|---|---|---|---|---|
| Followed up | Not followed up | Followed up | Not followed up | |||||
| Mean (SD) age (years) | 37 (20) | 37 (20) | 38 (20) | 38 (20) | 31 (18) | 40 (21) | 34 (19) | |
| No (%) female | 487 (49) | 514 (53) | 493 (50) | 1494 (50) | 336 (52) | 1062 (54) | 768 (47) | |
| Occupational status (median (interquartile range)): | ||||||||
| Non-manual* | 0.50 (0.30 to 0.66) | 0.50 (0.29 to 0.66) | 0.52 (0.31 to 0.67) | 0.53 (0.35 to 0.68) | 0.37 (0.20 to 0.53) | 0.54 (0.36 to 0.70) | 0.45 (0.24 to 0.63) | |
| Retired* | 0.21 (0.10 to 0.35) | 0.21 (0.10 to 0.33) | 0.22 (0.11 to 0.34) | 0.22 (0.11 to 0.35) | 0.20 (0.07 to 0.32) | 0.21 (0.10 to 0.33) | 0.21 (0.11 to 0.35) | |
| Economically inactive* | 0.10 (0.03 to 0.21) | 0.10 (0.04 to 0.22) | 0.10 (0.04 to 0.21) | 0.10 (0.03 to 0.20) | 0.13 (0.07 to 0.27) | 0.09 (0.03 to 0.19) | 0.12 (0.05 to 0.25) | |
| No (%)† consulting in past year for: | ||||||||
| Acute respiratory conditions (⩾once) | 189 (19) | 224 (23) | 213 (22) | — | — | — | — | |
| Minor illness (⩾twice) | 255 (26) | 289 (30) | 272 (28) | — | — | — | — | |
| All consultations (⩾5 times) | 279 (28) | 279 (29) | 299 (30) | — | — | — | — | |
For each individual: from census data linked to postcodes we derived the proportions of individuals in non-manual work, retired, or economically inactive in their postal enumeration district. †Percentages of participants who had notes reviewed.
Compared with the control group, fewer patients in the booklet and summary card groups attended frequently with minor illnesses (table 2). Among patients who had attended with respiratory tract infections in the previous year, there was also a reduction in attendance in the booklet group (0.81; 95% confidence interval 0.62 to 1.07; z=1.5, P=0.14) and summary card group (0.67; 0.51 to 0.89; z=2.8, P=0.005) compared with the control group. Compared with the previous year there were small non-significant reductions in the incidence of contacts with minor illness for the booklet group (incidence ratio 0.97; 0.84 to 1.13) and summary card group (0.93; 0.80 to 1.07).
Table 2.
Impact of information booklets/leaflet on higher attendance for all conditions, minor illness, and acute respiratory tract infections
| High attendance No (%) | Not high attendance No (%) | Crude odds ratio (95% CI) | Adjusted odds ratio (95% CI)* | Wald test z (P value) | |
|---|---|---|---|---|---|
| All consultations (⩾5 times): | |||||
| Booklet | 268 (32) | 735 (35) | 0.89 (0.73;1.08) | 0.92 (0.72;1.16) | 0.71 (0.48) |
| Summary card | 276 (33) | 698 (33) | 0.96 (0.79;1.17) | 0.99 (0.80;1.23) | 0.04 (0.97) |
| Control | 288 (35) | 700 (33) | 1 | 1 | — |
| Total | 832 (100) | 2133 (100) | — | — | — |
| Minor illness (⩾twice): | |||||
| Booklet | 245 (31) | 758 (35) | 0.80 (0.66;0.98) | 0.81 (0.67;0.99) | 2.02 (0.043) |
| Summary card | 252 (32) | 722 (33) | 0.87 (0.71;1.06) | 0.83 (0.72;0.96) | 2.54 (0.011) |
| Control | 284 (36) | 704 (32) | 1 | 1 | — |
| Total | 781 (100) | 2184 (100) | — | — | — |
| Acute respiratory tract infection (⩾once): | |||||
| Booklet | 183 (32) | 820 (34) | 0.87 (0.70;1.09) | 0.91 (0.76;1.09) | 1.04 (0.30) |
| Summary | 186 (33) | 788 (33) | 0.92 (0.74;1.15) | 0.90 (0.67;1.20) | 0.73 (0.47) |
| Control | 201 (35) | 787 (33) | 1 | 1 | — |
| Total | 570 (100) | 2395 (100) | — | — | — |
Adjusted for baseline attendance, and controlling for clustering at a practice level using practice as a cluster term in the model.
Table 3 shows that most respondents could remember receiving a leaflet or booklet (booklet 85%, card 70%, control 52%, P<0.001) and found them useful (booklet 81%, card 78%, control 62%; χ2 =68, P<0.001). More patients in the intervention groups felt greater confidence in managing common illness than in the control group (booklet 32%, card 34%, control 12%, χ2 =151, P<0.001), but there was no difference in willingness to wait score.
Table 3.
Reponse to follow up questionnaire on access to, use, and utility of information. Values are numbers (percentages) of respondents unless stated otherwise
| Booklet (n=671)* | Summary card (n=665)* | Control (n=639 )* | χ2 (P value) | |
|---|---|---|---|---|
| Access: | ||||
| Remember receiving | 572 (85) | 467 (70) | 336 (52) | 169 (<0.001) |
| Have it still | 425 (67) | 305 (51) | 171 (31) | 151 (<0.001) |
| Use: | ||||
| Read it | 528 (84) | 454 (76) | 336 (63) | 70 (<0.001) |
| Self management of illness when would have contacted GP | 97 (21) | 74 (18) | 27 (3) | 30 (<0.001) |
| Contacted GP when would have self managed | 30 (7) | 18 (5) | 14 (4) | 4 (0.14) |
| Useful: | ||||
| Very | 148 (27) | 119 (25) | 43 (11) | 68 (<0.001) |
| Slightly or moderately | 304 (55) | 258 (53) | 202 (51) | |
| Not very | 105 (19) | 107 (22) | 152 (38) | |
| Easy to use: | ||||
| Very | 426 (77) | 365 (78) | 259 (71) | 15 (0.006) |
| Slightly or moderately | 111 (20) | 82 (17) | 74 (20) | |
| Not very | 20 (4) | 74 (20) | 33 (9) | |
| Illness information: | ||||
| Too much | 2 (0.4) | 2 (0.4) | 2 (0.6) | 97 (<0.001) |
| About right | 441 (82) | 346 (76) | 168 (52) | |
| Too simple | 98 (18) | 107 (24) | 156 (48) | |
| Confident in managing minor illness: | ||||
| More | 178 (32) | 156 (34) | 42 (12) | 56 (<0.001) |
| Same | 370 (67) | 306 (66) | 289 (86) | |
| Less | 3 (0.5) | 4 (0.9) | 7 (2) | |
| Mean willingness to wait score | 31.9 | 32.2 | 32.0 | F=0.40 (0.67)† |
Not all respondents answered all questions.
Analysis of variance.
Discussion
This study shows that information provided by post helped patients feel more confident in managing minor illness and can reduce subsequent attendance with minor illness. However, the impact of a detailed information booklet on overall consultations is likely to be modest for most patients. Before the results are discussed in detail the limitations of the study must be identified.
Sources of bias
There are no absolutely reliable measures of attendance; documented attendance may be preferable but is open to bias from omission, and reported attendance has inherent recall bias. However, we found good agreement between documented and reported attendance in the baseline sample (r=0.76, likelihood ratio for a positive test 9.4), which supports the internal reliability of the data. Furthermore, any biases in measurement of attendance within each practice would be expected to be similar in all groups and would reduce the chance of finding differences between groups. We have shown that the documentation of minor illness by the two people who reviewed the notes was very reliable.
The sample came from only six practices with varied structures and populations, and supply and sociodemographic factors may be important in use of health care.14,15 However, patients were randomised at the individual level within practices, so any practice effect should be evenly distributed between groups. We also controlled for potential cluster effects at the practice level. Although we sampled only one member from each household group, which means that smaller sized households have relatively higher representation (reducing the proportion of adults from younger families), the age distribution of respondents was similar to that in data from the Office for National Statistics. The main potential bias in the results is the loss to follow up, but we achieved over 70% follow up and the characteristics of patients who were followed up were similar to those of the original sample.
The intervention in this study was information provided by post. The impact of the intervention would probably be less than that of a leaflet or booklet given in the context of a specific consultation. Thus the study may underestimate the effect of providing information booklets or leaflets in surgery.
Interpretation of results
Fewer patients attended frequently with minor illness in the booklet group and in the summary card group, although the effect was modest. An odds ratio of 0.82 corresponds to about a 4% reduction in those attending frequently—that is, from 29% to 25%. Our data support previous evidence that both general information and specific information can modify patients' use of services.4–9 However, the absolute change in terms of consultations for minor illness was not significant for either the booklet or summary card. The estimate of the reduction in contacts with the summary card was 7%, but the confidence intervals greatly overlapped unity.
There is a potential danger that by providing leaflets or booklets about self management patients feel pressurised not to attend when they are unwell. However, the thrust of the booklet and the summary card was to help patients in their self management decisions—to provide information about self management and guidance about when it was important to see the doctor. Furthermore, most patients found the information useful and felt more confident in managing common illness, although we do not know whether the information improved patients' management of symptoms. Although patients thought the leaflet and booklet were useful, there was little change in their willingness to tolerate symptoms or in the number of consultations with health professionals. This raises important questions about whether such booklets provide sufficient benefit to justify the use of NHS funds.
Figure.
Study design and trial flow
Acknowledgments
We are grateful for the help of the doctors, staff, and patients at Aldermoor Health Centre, Lordshill Health Centre, Nightingale Surgery, Victor Street Surgery, Three Swans Surgery, and St Ann's Surgery. We thank RTFB Publishing for supplying the intervention leaflets and booklets and for printing the questionnaire and Southampton and South West Hants Health Commission for buying the booklets. We also thank Peter Smith for help and guidance in fitting the longitudinal Poisson models.
Footnotes
Funding: This work was funded by a NHS Regional Research and Development Grant. PL is funded by the Medical Research Council (except for his clinical practice at Nightingale surgery).
Competing interests: None declared.
References
- 1.Office of Population Censuses and Surveys. Morbidity statistics from general practice: fourth national study 1991. London: HMSO; 1994. [Google Scholar]
- 2.Lattimer V, George S. Nurse telephone triage in out of hours primary care. Primary Care Management. 1996;6:3–6. [Google Scholar]
- 3.Howie J, Heaney D, Maxwell M, Walker J, Freeman G, Rai H. Quality at general practice consultations: cross sectional survey. BMJ. 1999;319:738–743. doi: 10.1136/bmj.319.7212.738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roland M, Dixon M. Randomised controlled trial of an educational booklet for patients presenting with back pain in general practice. J R Coll Gen Pract. 1989;39:244–246. [PMC free article] [PubMed] [Google Scholar]
- 5.Macfarlane JT, Holmes WF, Macfarlane RM, Lewis S. Reducing reconsultation for acute lower respiratory tract illness with an information leaflet: a randomised controlled study of patients in primary care. Br J Gen Pract. 1997;47:719–722. [PMC free article] [PubMed] [Google Scholar]
- 6.Banks J, Howie J. Reducing consultations for symptoms of cystitis using a health education leaflet. Br J Gen Pract. 1998;48:1595–1596. [PMC free article] [PubMed] [Google Scholar]
- 7.Morrell DC, Avery AJ, Watkins CJ. Management of minor illness. BMJ. 1980;280:769–771. doi: 10.1136/bmj.280.6216.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hansen B. A randomised controlled trial of the effect of an information booklet for young families in Denmark. Patient Education and Counselling. 1990;16:147–150. doi: 10.1016/0738-3991(90)90089-4. [DOI] [PubMed] [Google Scholar]
- 9.Terry P, Pheley A. The effect of self-care brochures on use of medical services. J Occup Environ Med. 1993;35:422–426. [PubMed] [Google Scholar]
- 10.Family Heart Study Group. Randomised controlled trial evaluating cardiovascular screening and intervention in general practice: principal results of British family heart study. BMJ. 1994;308:313–320. [PMC free article] [PubMed] [Google Scholar]
- 11.Metz R, Van der Does E. What should I do? Southampton: RTFB Publishing; 1997. [Google Scholar]
- 12.Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. Oxford: Oxford Medical Publications; 1995. [Google Scholar]
- 13.Swinscoe T. Statistics at square one. London: BMJ; 1996. [Google Scholar]
- 14.Little PS, Gould C, Williamson I, Warner G, Gantley M, Kinmonth AL. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ. 1997;315:350–352. doi: 10.1136/bmj.315.7104.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carr-Hill R, Rice N, Roland M. Socio-economic determinants of rates of consultation in general practice based on the fourth national morbidity survey of general practice. BMJ. 1996;312:1008–1013. doi: 10.1136/bmj.312.7037.1008. [DOI] [PMC free article] [PubMed] [Google Scholar]