Abstract
Background
This study compared the results of patients treated for ulnar impaction syndrome using an ulnar shortening osteotomy (USO) alone with those treated with combined arthroscopic debridement and USO.
Methods
The results of 27 wrists were reviewed retrospectively. They were divided into three groups: group A (USO alone, 10 cases), group B (combined arthroscopic debridement and USO, 9 cases), and group C (arthroscopic triangular fibrocartilage complex [TFCC] debridement alone, 8 cases). The wrist function was evaluated using the modified Mayo wrist score, disabilities of the arm, shoulder and hand (DASH) score and Chun and Palmer grading system.
Results
The modified Mayo wrist score in groups A, B, and C was 74.5 ± 8.9, 73.9 ± 11.6, and 61.3 ± 10.2, respectively (p < 0.05). The DASH score in groups A, B, and C was 15.6 ± 11.8, 19.3 ± 11.9, and 33.2 ± 8.5, respectively (p < 0.05). The average Chun and Palmer grading score in groups A and B was 85.7 ± 8.9 and 84.7 ± 6.7, respectively. The difference in the Mayo wrist score, DASH score and Chun and Palmer grading score between group A and B was not significant (p > 0.05).
Conclusions
Both USO alone and combined arthroscopic TFCC debridement with USO improved the wrist function and reduced the level of pain in the patients treated for ulnar impaction syndrome. USO alone may be the preferred method of treatment in patients if the torn flap of TFCC is not unstable.
Keywords: Ulnar impaction syndrome, Triangular fibrocartilage complex, Ulnar shortening osteotomy, Arthroscopic debridement
Ulnar impaction syndrome has a wide spectrum ranging from the simple wear of a triangular fibrocartilage complex (TFCC) to a large perforation. If a perforated TFCC unstable flap causes mechanical irritation between the ulnar head and carpal bones, an unstable flap should be debrided to stabilize the rim.1)
Until now, ulnar shortening remains the treatment of choice for ulna impaction syndrome. The indication of ulnar shortening has been extended to failed triangular fibrocartilage complex debridement, ulnar impaction syndrome with carpal instability and early posttraumatic distal radioulnar joint osteoarthritis.1)
Arthroscopy is widely used simultaneously if ulnar shortening osteotomy (USO) is planned but the role of arthroscopy in ulnar impaction syndrome is less clear.
In a biomechanical perspective, USO attempts to decompress the ulnocarpal articulation mechanically. Although USO is popular, the stabilizing effect of TFCC to the ulnocarpal and distal radioulnar joint by proximal migration of the ulnar head is not completely understood. Moreover, there are few reports comparing the results of USO alone with those of combined arthroscopic debridement and USO. This study hypothesized that USO alone has a similar effect on the clinical scores of combined arthroscopic TFCC debridement with USO for ulnar impaction syndrome. This study compared the efficacy of combined arthroscopic TFCC debridement with USO versus USO alone in the treatment of ulnar impaction syndrome.
METHODS
The results of 26 patients (27 wrists), who underwent surgical procedures to treat ulnar impaction syndrome and TFCC tears at our hospital between November 2003 and November 2008, were reviewed retrospectively. The 27 wrists were divided into group A (USO alone, 10 cases), group B (combined arthroscopic debridement with USO, 9 cases), and group C (arthroscopic TFCC debridement alone, 8 cases). Nine men and 18 women (mean age, 42 years [range, 25 to 69 years]) were followed up for a mean of 23 months (range, 13 to 53 months). The function of the wrists was evaluated using the modified Mayo wrist score2) and disabilities of the arm, shoulder and hand (DASH) score3) in all patients pre- and post-operatively. The function, bony union and ulnar variance were compared using the Chun and Palmer grading system.4)
The dominant hand was involved in 14 patients. All patients presented with ulnar wrist pain with a more than 3 months duration and a positive ulnar variance ranging from 0.5 to 15 mm (mean, 3.5 mm). The duration of symptoms from onset to surgery was 3 to 80 months (mean, 24.3 months). The symptoms were related to their occupation in 3 patients, all of whom were covered by workers' compensation. Surgery was performed on the patients who did not respond appropriately to nonsurgical treatments, such as medication and intermittent splinting for more than 3 months.
The inclusion criteria were as follows: 1) persistent ulnar-sided wrist pain provoked by pronation and ulnar deviation despite a minimum 3 months of conservative management; 2) neutral or positive ulnar variance, as measured by the method of perpendiculars from a standard posteroanterior radiograph of the wrist5); and 3) a positive ulnocarpal stress test. The exclusion criteria were as follows: 1) secondary USO due to a failed arthroscopically debrided TFCC tear; 2) repairable TFCC tear; 3) distal radioulnar joint (DRUJ) arthritis; 4) scapholunate (SL) ligament or lunatotriquetral (LT) ligament instability; and 5) distal radius malunion and shortening > 5 mm. Partial SL or LT ligament tears identified during an arthroscopic evaluation were not a cause for exclusion. The presence or absence of a TFCC perforation on the imaging studies is not a prerequisite for inclusion in this study. MRI was checked in 7 out of 10 cases in group A, 6 out of 9 cases in group B, and 3 out of 8 cases in group C. Computed tomography (CT) arthrography was checked in 3 out of 10 cases in group A, 3 out of 9 cases in group B, and 5 out of 8 cases in group C.
The decision as to which operation to perform depends on the patient's acceptance of USO and the tear condition of the cartilage. If patients just want an arthroscopic procedure, arthroscopic TFCC debridement alone was chosen. The arthroscopic wafer procedure was also performed in 1 case of group C with the ulnar head cartilage denuded. Informed consent was obtained from the patients before the secondary USO if the symptoms were not relieved after arthroscopic TFCC debridement alone. In the USO group, the tear condition of TFCC or LT ligament was considered for the selection of arthroscopic debridement. Only USO was performed if a torn flap of the TFCC or LT ligament was not so unstable using a probe (Fig. 1). On the other hand, if the torn flap of the TFCC or LT ligament was unstable, arthroscopic debridement was performed until the torn flap was stabilized. USO was then performed (Fig. 2).
Fig. 1.
(A) A 35-year-old female showing positive ulnar variance on a preoperative anteroposterior radiograph. (B) CT arthrography findings of a perforation of the triangular fibrocartilage complex and subchondral cyst in the ulnar border of the lunate in ulnar impaction syndrome. (C) Arthroscopic view of a central Palmer 2C lesion exposing the ulnar head through the defect in the articular disc. (D) An anteroposterior radiograph made after ulnar shortening osteotomy alone and fixation with a dynamic compression plate and screws. (E) A 30-month final follow-up anteroposterior radiograph.
Fig. 2.
(A) A 45-year-old female showing positive ulnar variance on a preoperative anteroposterior radiograph. (B) Computed tomography arthrography findings of a perforation of the triangular fibrocartilage complex (TFCC) and subchondral cyst in the lunate in ulnar impaction syndrome. (C) Wear in the central portion of the TFCC on arthroscopy. (D) Tear of membraneous portion of the lunatotriquetral ligament on arthroscopy. (E) Arthroscopic photo of Palmer 2D TFCC defect after debridement. (F) An anteroposterior radiograph made after arthroscopic debridement and ulnar shortening osteotomy and fixation with a dynamic compression plate and screws. (G) An 18-month final follow-up anteroposterior radiograph.
All procedures were performed by the same author. Arthroscopy was performed with the patients under general anesthesia with a tourniquet. The TFCC and articular surfaces of the lunate and triquetrum including the LT ligament were inspected for wear or tear. In group A, USO was performed after diagnostic arthroscopy for the TFCC condition in all cases. In groups B and C, debridement of the TFCC wear or a tear to a stable margin was performed using a small joint shaver or an electrothermal small joint probe. In group B, USO was performed after the arthroscopic procedures. The distal ulna was approached subperiosteally between the extensor carpi ulnaris and flexor carpi ulnaris, protecting the dorsal sensory branch of the ulnar nerve. A seven-hole small dynamic compression plate was placed on the volar surface of the ulna.6) The most distal and most proximal screw holes were then drilled along the midline of the ulnar shaft located a few millimeters eccentrically from each other depending on the amount of shortening, and the screws were inserted provisionally, which was helpful for controlling the rotational alignment and plate malposition. After the plate and screw were removed from the osteotomy site, oblique osteotomies were performed at the middle hole area of the plate in the proximal volar to distal dorsal direction.7) The length of the segment removed equaled the amount of positive ulnar variance measured on the preoperative radiograph. The plate was put back in place and the most proximal and distal screws were repositioned. The remaining screws were introduced in compression mode from the proximal screw hole adjacent osteotomy site and the distal screw hole adjacent osteotomy site. Finally, the most proximal and distal screws were tightened. Postoperatively, a below-elbow splint was applied for 2 weeks in all groups and a below-elbow cast was applied for an additional 2 weeks in groups A and B. Active motion of the wrist was started with a removable splint after postoperative 4 weeks in groups A and B. The perioperative ulnar variances were measured radiographically using a perpendicular line to the longitudinal axis of the radius at its distal ulnar volar rim and the line at the end of the ulna. A posteroanterior radiograph of the wrist was obtained with the shoulder in 90° abduction, elbow in 90° flexion, forearm in neutral rotation, and wrist in neutral alignment for accurate measuring. A Mann-Whitney test and Kruskal-Wallis test was carried out to analyze the differences in the clinical scores and radiographic measurements before and after surgery. All analyses were performed using a commercial SPSS (SPSS Inc., Chicago, IL, USA). The data obtained is expressed as the mean ± standard deviation. A p < 0.05 was considered significant.
RESULTS
TFCC perforation was detected by imaging studies in 7, 7, and 8 patients in group A, B and C, respectively. The arthroscopic findings were as follows. According to Palmer's classification of TFCC lesions, class IIB, IIC, and IID lesions were present in 4, 3, and 3 wrists, respectively, in group A, including a radial slit tear in 3 cases.8)
In group B, class IIC and IID lesions were present in 1 and 8 wrists, respectively, including a radial slit tear in 2 cases. The location of the perforation was central and radial in 6 and 2 cases, respectively. The mean diameter of the perforation was 4.3 mm (range, 1 to 7 mm). An unstable TFCC flap was excised until the torn margin had stabilized.
In group C, class IIC lesions were present in 8 wrists, including a radial slit tear in 2. The TFCC was not perforated in 4 cases in group A (Table 1). Chondromalacia of the lunate was observed in 21 patients. Grade I chondromalacia (softening) was noted in 6, 6, and 3 patients in group B, C, and A, respectively. Grade II (fibrillation) was observed in 4, 2, and 1 case in group B, C, and A, respectively. Grade III (extending down to the subchondral bone) was found in one case in group A. The LT ligament had a partial tear and minimal laxity in 2 cases in group A. In group B, 5 cases had a LT ligament tear, which included 4 cases of grade 1 laxity, and 1 case of grade II laxity. The proximal membranous portion of the LT ligament was almost detached from lunate in 1 case. Chondromalacia in the triquetrum was observed in 23 patients, with grade I in 13 patients (6 in group C, 5 in group B, and 2 in group A), and grade II in 10 (5 in group B, 3 in group A, and 2 in group C).
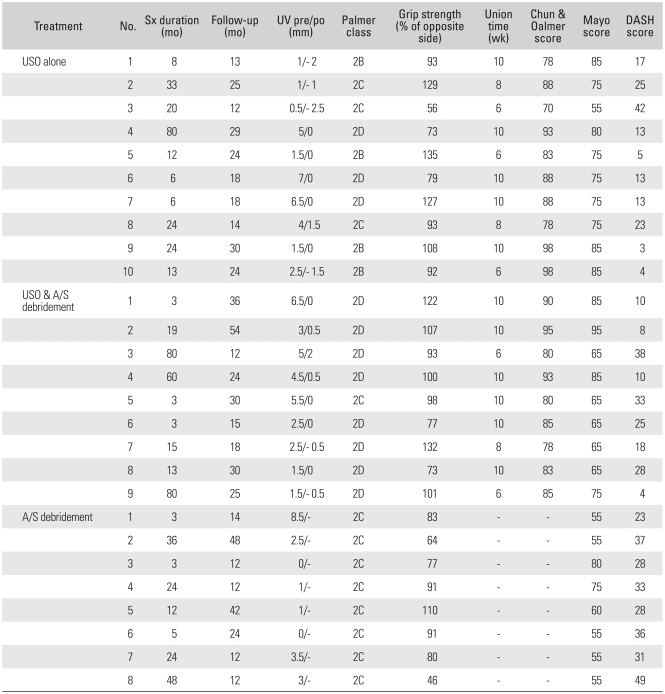
Table 1.
Summary of Results
Sx: symptoms, UV: ulnar variance, DASH: disabilities of the arm, shoulder and hand, USO: ulnar shortening osteotomy, A/S: arthroscopic.
Arthroscopic debridement of the triangular fibrocartilage complex, lunate, LT ligament, and/or triquetrum was performed in groups B and C. In group A, after diagnostic arthroscopy, USO was performed without arthroscopic debridement.
The modified Mayo wrist score improved from 55.5 ± 11.1 to 74.5 ± 8.9, 51.7 ± 14.1 to 73.9 ± 11.6 and 50.0 ± 12.5 to 61.3 ± 10.2, respectively (p < 0.05). The difference in the preoperative Mayo wrist score between groups A, B and C was not significant (p < 0.05). The postoperative Mayo wrist score of groups A and B was significantly higher than group C (p < 0.05). The DASH score improved from 34.4 ± 9.1 to 15.6 ± 11.8, 35.7 ± 16.8 to 19.3 ± 11.9 and 38.4 ± 9.6 to 33.2 ± 8.5 in group A, B, and C, respectively (p < 0.05). The difference in the preoperative DASH score between groups A, B, and C was not significant (p > 0.05). The postoperative DASH wrist score of groups A and B was significantly lower than group C (p < 0.05).
Three out of 8 patients in group C (arthroscopic debridement alone) had persistent symptoms. Two of them had an additional USO later but one patient refused further surgery. Finally, two patients who underwent secondary USO showed a resolution of their symptoms.
The grip power improved from 73.4 ± 22% to 89.0 ± 21% of the contralateral side. The Chun and Palmer score was used for a comparison between groups A and B. The Chun and Palmer subjective pain score improved from 12.1 ± 4.8 to 15.8 ± 3.0 (p < 0.05). The subjective function score improved from 12.9 ± 3.8 to 15.5 ± 2.8 (p < 0.05). The subjective range of motion improved from 7.6 ± 2.9 to 9.5 ± 2.3 (p < 0.05). The objective range of motion changed from 7.4 ± 1.0 to 7.9 ± 0.9 and the objective strength changed from 7.5 ± 2.2 to 9.1 ± 1.5 (p < 0.05). The mean Chun and Palmer grading score improved from 66.7 ± 7.8 to 85.2 ± 7.8 (p < 0.05) with 6 excellent, 8 good, and 5 fair results; from 68.7 ± 3.3 to 85.7 ± 8.9 (p < 0.05) with 3 excellent, 4 good, and 3 fair results in group A, and from 64.5 ± 10.6 to 84.7 ± 6.7 (p < 0.05) with 3 excellent, 4 good, and 2 fair results in group B. On the other hand, the difference in the preoperative and postoperative Chun and Palmer score between group A and B was not significant (p > 0.05). The ulnar variance decreased from 3.5 ± 3.3 mm preoperatively to -0.1 ± 1.1 mm postoperatively (p < 0.05). The mean preoperative radioulnar distance was 0.4 mm (range, -3.2 to 7.6 mm) on the true lateral radiograph, which decreased to -0.8 mm (range, -5.8 to 1.6 mm) after surgery (p < 0.05). A positive correlation was detected between the preoperative ulnar variance and radioulnar distance in groups A and B (r2 = 0.605, p = 0.006). All patients achieved bony union with an average union time of 8.4 ± 1.8 and 8.8 ± 1.7 weeks in groups A and B, respectively.
A fracture of the adjacent proximal screw hole occurred in one case at postoperative 6 months due to a slip down. Accordingly, open reduction and internal fixation were performed using a longer plate with an iliac bone graft, which achieved bony union after 8 weeks.
DISCUSSION
Overloading between the distal ulna and ulnar carpus occurs as a result of a positive ulnar variance. Patients usually report ulnar-sided pain and swelling with an insidious onset. USO is the treatment of choice for correcting positive ulnar variance, which relieves the pain by reestablishing a neutral or slightly negative ulnar variance.
Degenerative TFCC wears develop as a result of chronic repetitive conditions. In certain situations, they cannot be differentiated because of their uncertain history and physical findings. Imaging studies are also limited in identifying the precise pathology. Therefore, arthroscopy helps the surgeon to differentiate TFCC tears from ulnar impaction syndrome. TFCC tears may aggravate the symptoms if concomitant TFCC tears occur as a result of an acute injury in patients who already have an underlying ulnar impaction syndrome.9) Arthroscopy and USO might useful in this acute on chronic situation. Although combined arthroscopic TFCC debridement and a wafer distal ulna resection in patients with a TFCC tear and positive ulnar variance has been introduced,10) arthroscopy may have additional diagnostic and therapeutic value if USO is already planned preoperatively. On the other hand, the therapeutic effect of arthroscopy in ulnar impaction syndrome is less clear. This study showed that in terms of the therapeutic effect, USO alone is effective in relieving the symptoms of ulnar impaction syndrome. Minami et al.11) reported that simple TFCC debridement with positive ulnar variance was unsuccessful and concluded that osseous decompression of the ulnar side of the wrist should be performed. Fulcher and Poehling12) suggested that arthroscopy is not indicated in type IIA and IIB lesions. Nevertheless, many IIA and IIB lesions are being treated in the same manner as type IIC lesions. This study suggests that USO alone has a similar effect in types IIC and IID. If the symptoms persist after the osteotomy, they may be considered a mechanical irritation of TFCC or LT ligament attenuation or tears.
Osteotomy has a TFCC tightening effect if the bony attachment of TFCC is intact.13-15) A reduced load of the ulnar wrist column by ulnar shortening may not only improve the stability but also have favorable effects on a torn TFCC. These were observed in our cases as a decrease in the dorsal subluxation of the ulnar head due to ulnocarpal and distal radioulnar ligament tightening effect of the USO via the TFCC. The decrease in radioulnar distance was attributed to extrinsic ulnocarpal ligament tightening or a decrease in carpal supination because impaction with a very long ulna may stop after USO. This study also found a positive correlation between the ulnar variance and radioulnar distance, which suggests that a wrist with a larger ulnar variance has a higher likelihood of subluxation of the distal radioulnar joint.16)
The outcomes of combined arthroscopic TFCC debridement and USO for ulnar impaction syndrome were compared with those of USO alone. The data raises the question as to whether arthroscopic TFCC debridement is needed for symptom improvement. Recently, the TFCC was found to be repaired spontaneously during second-look arthroscopy in patients who underwent USO.17) Although combined arthroscopic TFCC debridement and USO improves the wrist function of patients with ulnar impaction syndrome,18) some authors16) suggest that USO alone provides satisfactory results for ulnar impaction syndrome.
The present study had some limitations. First, the analysis was based on data from a retrospective chart review. In addition, there may have been selection bias because the treatments depend on the tear condition of the cartilage. To confirm the effects of arthroscopic debridement, a randomized prospective controlled design will be needed to ensure the preoperative data is collected in a standard manner. Second, the small sample size could have limited the statistical power. Finally, whether or not tears of the disc had healed is unclear because second look arthroscopy was not performed in most patients.
This study also found a positive correlation between the Chun and Palmer's wrist score, modified Mayo wrist score and DASH. In this study, the workers compensation patients included 3 cases, (2 in group A and 1 in group B). The results of these cases were good in 2 cases and fair in 1.
Iwasaki et al.19) reported that the long duration of symptoms and worker's compensation predicted a poorer clinical score. In this study, the duration of symptoms was similar in groups A and B. In addition, the correlation between the duration of symptoms and the clinical score was not significant.
In summary, both USO alone and combined arthroscopic TFCC debridement with USO improved the wrist function and reduced the level of pain in the patients treated for ulnar impaction syndrome. The clinical outcomes do not differ between USO alone and combined arthroscopic TFCC debridement with USO. USO alone may be the preferred method of treatment in patients if the torn flap of the TFCC is not unstable.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Sachar K. Ulnar-sided wrist pain: evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg Am. 2008;33(9):1669–1679. doi: 10.1016/j.jhsa.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 2.Cooney WP, Linscheid RL, Dobyns JH. Triangular fibrocartilage tears. J Hand Surg Am. 1994;19(1):143–154. doi: 10.1016/0363-5023(94)90238-0. [DOI] [PubMed] [Google Scholar]
- 3.Hudak PL, Amadio PC, Bombardier C The Upper Extremity Collaborative Group (UECG) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected] Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 4.Chun S, Palmer AK. The ulnar impaction syndrome: follow-up of ulnar shortening osteotomy. J Hand Surg Am. 1993;18(1):46–53. doi: 10.1016/0363-5023(93)90243-V. [DOI] [PubMed] [Google Scholar]
- 5.Yeh GL, Beredjiklian PK, Katz MA, Steinberg DR, Bozentka DJ. Effects of forearm rotation on the clinical evaluation of ulnar variance. J Hand Surg Am. 2001;26(6):1042–1046. doi: 10.1053/jhsu.2001.26657. [DOI] [PubMed] [Google Scholar]
- 6.Lauder AJ, Luria S, Trumble TE. Oblique ulnar shortening osteotomy with a new plate and compression system. Tech Hand Up Extrem Surg. 2007;11(1):66–73. doi: 10.1097/bth.0b013e3180336cc7. [DOI] [PubMed] [Google Scholar]
- 7.Chen NC, Wolfe SW. Ulna shortening osteotomy using a compression device. J Hand Surg Am. 2003;28(1):88–93. doi: 10.1053/jhsu.2003.50003. [DOI] [PubMed] [Google Scholar]
- 8.Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14(4):594–606. doi: 10.1016/0363-5023(89)90174-3. [DOI] [PubMed] [Google Scholar]
- 9.Bickel KD. Arthroscopic treatment of ulnar impaction syndrome. J Hand Surg Am. 2008;33(8):1420–1423. doi: 10.1016/j.jhsa.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 10.Tomaino MM, Weiser RW. Combined arthroscopic TFCC debridement and wafer resection of the distal ulna in wrists with triangular fibrocartilage complex tears and positive ulnar variance. J Hand Surg Am. 2001;26(6):1047–1052. doi: 10.1053/jhsu.2001.28757. [DOI] [PubMed] [Google Scholar]
- 11.Minami A, Ishikawa J, Suenaga N, Kasashima T. Clinical results of treatment of triangular fibrocartilage complex tears by arthroscopic debridement. J Hand Surg Am. 1996;21(3):406–411. doi: 10.1016/s0363-5023(96)80353-4. [DOI] [PubMed] [Google Scholar]
- 12.Fulcher SM, Poehling GG. The role of operative arthroscopy for the diagnosis and treatment of lesions about the distal ulna. Hand Clin. 1998;14(2):285–296. [PubMed] [Google Scholar]
- 13.Moritomo H, Murase T, Arimitsu S, Oka K, Yoshikawa H, Sugamoto K. Change in the length of the ulnocarpal ligaments during radiocarpal motion: possible impact on triangular fibrocartilage complex foveal tears. J Hand Surg Am. 2008;33(8):1278–1286. doi: 10.1016/j.jhsa.2008.04.033. [DOI] [PubMed] [Google Scholar]
- 14.Nishiwaki M, Nakamura T, Nagura T, Toyama Y, Ikegami H. Ulnar-shortening effect on distal radioulnar joint pressure: a biomechanical study. J Hand Surg Am. 2008;33(2):198–205. doi: 10.1016/j.jhsa.2007.11.024. [DOI] [PubMed] [Google Scholar]
- 15.Nishiwaki M, Nakamura T, Nakao Y, Nagura T, Toyama Y. Ulnar shortening effect on distal radioulnar joint stability: a biomechanical study. J Hand Surg Am. 2005;30(4):719–726. doi: 10.1016/j.jhsa.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 16.Baek GH, Chung MS, Lee YH, Gong HS, Lee S, Kim HH. Ulnar shortening osteotomy in idiopathic ulnar impaction syndrome. J Bone Joint Surg Am. 2005;87(12):2649–2654. doi: 10.2106/JBJS.D.02983. [DOI] [PubMed] [Google Scholar]
- 17.Tatebe M, Horii E, Nakao E, et al. Repair of the triangular fibrocartilage complex after ulnar-shortening osteotomy: second-look arthroscopy. J Hand Surg Am. 2007;32(4):445–449. doi: 10.1016/j.jhsa.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 18.Bernstein MA, Nagle DJ, Martinez A, Stogin JM, Jr, Wiedrich TA. A comparison of combined arthroscopic triangular fibrocartilage complex debridement and arthroscopic wafer distal ulna resection versus arthroscopic triangular fibrocartilage complex debridement and ulnar shortening osteotomy for ulnocarpal abutment syndrome. Arthroscopy. 2004;20(4):392–401. doi: 10.1016/j.arthro.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 19.Iwasaki N, Ishikawa J, Kato H, Minami M, Minami A. Factors affecting results of ulnar shortening for ulnar impaction syndrome. Clin Orthop Relat Res. 2007;465:215–219. doi: 10.1097/BLO.0b013e31815a9e21. [DOI] [PubMed] [Google Scholar]